Abstract
Sickle cell disease and β thalassemia are common severe diseases with little effective pathophysiologically-based treatment. Their phenotypic heterogeneity prompted genomic approaches to identify modifiers that ultimately might be exploited therapeutically. Fetal hemoglobin (HbF) is the major modulator of the phenotype of the β hemoglobinopathies. HbF inhibits deoxyHbS polymerization and in β thalassemia compensates for the reduction of HbA. The major success of genomics has been a better understanding the genetic regulation of HbF by identifying the major quantitative trait loci for this trait. If the targets identified can lead to means of increasing HbF to therapeutic levels in sufficient numbers of sickle or β-thalassemia erythrocytes, the pathophysiology of these diseases would be reversed. The availability of new target loci, high-throughput drug screening, and recent advances in genome editing provide the opportunity for new approaches to therapeutically increasing HbF production.
Similar content being viewed by others
Introduction
Hemoglobin contains 2 α-like and 2 β-like globin subunits. The genes encoding the subunits and their hemoglobin products are shown in Fig. 1 along with a brief classification of hemoglobinopathies and thalassemia. Globin, the protein moiety of hemoglobin, is affected by more than 1500 unique mutations that alter its structure, function and expression [1]. The number of children born each year with clinically significant hemoglobinopathies is estimated to be 300,000 to 500,000; 70 % have sickle cell disease [2–4]. Eighty percent of affected patients are born in developing countries where these diseases are a major health burden [5]. This high concentration is the sequelae of endemic malaria and the protection afforded carriers of globin gene mutations, however, the burden of disease from hemoglobinopathies is now global.
a Arrangement of the β- and α-globin gene clusters and their regulatory regions, The LCR (locus control region) and HS-40 are the major enhancers of expression within the HBB and HBA gene clusters, respectively. HbA is a tetramer of normal α- and β-globin chains. b. The expression of the globin genes changes throughout development. Embryonic ε globin is produced in the embryo, fetal γ-globin during most of gestation and the major adult β globin from mid-gestation onwards. Not shown are the α-globin-like ζ globin genes and the α-globin genes whose expression starts early in embryogenesis. c. Classification of hemoglobinopathies and thalassemia. Hemoglobinopathies result from mutations that change the primary structure of globin. The most common examples are HbS (HBB glu6val), HbC (HBB glu6lys), and HbE (HBB glu26lys). Rare structural variants affect the oxygen delivery functions of the molecule, its stability and its resistance to oxidation. Thalassemia is caused by mutations that affect transcription and translation of any globin gene by nearly all possible mechanisms. They lead to decreased or absent production of a globin subunit; α and β thalassemia are most common. In all thalassemias the phenotype is a consequence of imbalanced synthesis of globin subunits allowing globin unincorporated into a tetramer to precipitate and otherwise damage the erythrocyte. About 1600 structural variants and thalassemia mutations have been cataloged in The Hemoglobin Variant Database [1]. All thalassemias and hemoglobinopathies can interact in various ways and many different compound heterozygous conditions occur. (Adapted from [51])
Hemoglobinopathies are single gene Mendelian disorders. Nevertheless there is substantial phenotypic heterogeneity within a single genotype of disease. Genetics have a major role in determining phenotypic heterogeneity. Association studies using candidate genes and genome-wide approaches have provided clues to loci that might mediate phenotypic variation but with 2 notable exceptions a detailed understanding of the relationship between putative modifying genes and the phenotypes of sickle cell disease and β thalassemia has not been achieved. The greatest progress has been made in defining genomic regions and specific sequence variants that modulate expression of the HbF genes, HBG2 and HBG1. HbF is the major known modulator of the phenotype of the β hemoglobinopathies so the application of these discoveries has the potential to improve care and guide development of new and better therapeutics.
Sickle cell disease
A point mutation in the β-globin gene (HBB) specifies the production of HbS, which polymerizes when deoxygenated. The damaged sickle erythrocyte is the proximate cause of vascular occlusion and anemia. The sickle erythrocyte has a lifespan about 1/10th that of a normal erythrocyte. Abnormal sickle erythrocytes are inflexible and obstruct blood flow leading to tissue damage and pain and membrane damage leads to hemolytic anemia. Clinical complications start early and include episodic painful vasoocclusive episodes that can lead to widespread tissue damage. Intracellular HbS concentration is a major determinant of disease severity and this can be reduced by increasing the concentration of HbF, or reducing mean cell HbS concentration by other means.
Thalassemia
Thalassemia is typified by imbalanced α- and β-globin chain synthesis and anemia. More than 400 mutations are associated with thalassemia [1]. The 2 most common thalassemia syndromes affect expression of β- and α-globin. In β thalassemia, unpaired α globin chains precipitate, impairing the maturation of erythroid precursors causing ineffective erythropoiesis. Anemia and expansion of erythroid precursors with expanded hematopoiesis in bones and other organs occurs. In α thalassemia, underproduction of α globin leads to β4 and γ4 homotetramers that have high oxygen affinity, are ineffective oxygen transporters, precipitate when oxidized, and cause membrane dysfunction, erythrocyte damage and shortened cell survival [6]. The clinical course of both α and β thalassemia is heterogeneous and depends in part on the impairment of globin synthesis and the ratio of α and non-α chains.
Current therapies
Treatment is imperfect. The management of sickle cell anemia and β thalassemia begins with carrier detection and parenteral counseling followed by screening for selected complications, supportive care, judicious use of blood transfusions, and hydroxyurea in sickle cell anemia, a medication that can stimulate HbF production. Transfusion therapy causes excess iron deposition and organ dysfunction, and also alloimmunization. It requires safe and effective blood banking which is a challenge in developing economies. Hydroxyurea is not effective in most patients with severe β thalassemia.
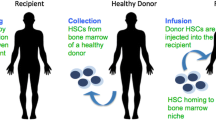
Stem cell transplant can “cure” both disorders. The best results are with identical sibling matched donors. Haploidentical and unrelated stem cell donors have widened the availability of transplants but with poorer results. In sickle cell anemia, the underrepresentation of donors with a similar genetic population structure as recipients reduces the donor pool.
Using genomics to find therapeutic targets
Phenotypic heterogeneity of the β hemoglobinopathies
In sickle cell anemia, every patient has the identical HbS mutation; in thalassemia, many different mutations can cause the disease. Nevertheless, even amongst patients with the same thalassemia mutation, the clinical course can vary, sometimes markedly. This heterogeneity complicates prognostication, management and clinical trials.
The most potent genetic modifiers of the course of β hemoglobinopathies lie within the globin gene complexes. For example, concomitant α thalassemia modifies the phenotype of sickle cell anemia and β thalassemia. In sickle cell anemia, it reduces mean cell HbS concentration and in β thalassemia it decreases globin chain imbalance. The phenotype of sickle cell anemia-α thalassemia has been well described [7, 8]. HbS concentration in sickle cell anemia-α thalassemia is less than in sickle cell anemia reducing polymer-induced damage, anemia, and the complications of disease closely associated with the rate of hemolysis. However, complications associated with blood viscosity are increased, perhaps because total hemoglobin level increases [9, 10]. The complexity of the relationship between hemoglobin concentration, cell density and disease complications was further demonstrated in a clinical trial of a Gardos ion channel inhibitor that reduces cation transport and cell density [11]. In a phase III trial (NCT00102791), the drug had the expected effects of reducing cell density and hemolysis, and increasing hemoglobin levels. Yet, there was no clinical improvement and vasoocclusive episodes increased in the treatment arm, and the trial was stopped [12].
Genetic association studies
The clinical heterogeneity of β hemoglobinopathies prompted the application of genetic association studies to find genes that influenced their phenotypes Most of the work was focused on sickle cell anemia.
Candidate gene association studies
Initial attempts to define genotype-phenotype relationships relied on candidate gene analysis, which examined polymorphisms in genes chosen by an “educated guess” that the gene might modify some disease feature. The frequencies of genetic variants in the candidate genes are then compared between groups with and without the phenotype of interest. If the variant is significantly more frequent in people with the phenotype than an association—not causality—can be inferred. The scarcity of β hemoglobinopathies limits the sample size. When a limited number of polymorphisms are being tested the statistical analysis is straightforward. Nevertheless, many caveats that include heritability of the phenotype of interest, sample selection, phenotypic definition, population stratification and linkage disequilibrium (LD) between the polymorphisms genotyped and the causal variant—rarely one in the same—exist [13]. The candidate gene approach has been applied to search for polymorphisms that correlate with subphenotypes of sickle cell anemia independent of HbF and α thalassemia.
Candidate gene association studies have been criticized for their lack of robustness and replicability [14]. A summary of the candidate gene associations with common sub-phenotypes of sickle cell anemia is shown in Table 1. With some exceptions, validation of much of this work is weak [8, 14]. A further disappointment of candidate gene studies is that functional and mechanistic studies of loci associated with a phenotype have rarely been reported so that most associations have not met the ultimate test of validation as a potential therapeutic target.
The TGF-β/BMP pathway has been identified as a possible modulator of different subphenotypes of sickle cell anemia. This is a super-family of genes modulating cell growth, angiogenesis, endothelial function, cell, and inflammation that are integral to the pathophysiology of the vasculopathy seen in the hemoglobinopathies [15–17]. Inflammation causes endothelial cell expression of adhesion molecules such as selectins [18, 19]. Adherence to the vascular endothelium by sickle erythrocytes, leukocytes, and platelets initiates the process of vasoocclusion leading to downstream effects of ischemia and reperfusion injury.
Drugs targeting TGF-β signaling have undergone clinical studies [15] for fibrosis and vasculopathy of the lung, kidneys, and heart. The underlying pathophysiology of these conditions might overlap with mechanisms that lead to sickle vasculopathy like pulmonary hypertension, kidney disease, and stroke, and with further research proving safety and efficacy might warrant investigation as therapy for sickle cell anemia. Studies of a modified activin type IIb receptor-Fc fusion protein that inhibits Smad2/3 signaling decreased iron overload, splenomegaly, and bone pathology in murine β thalassemia, and in preliminary studies of sickle transgenic mice (ASH 2014, abstract 113, Modified ActRIIB-mFc Fusion Protein (murine ortholog of Luspatercept) Mitigates Sickling and Red Cell Pathology in a Murine Model of Sickle Cell Disease), reduced some markers of hemolysis, irreversibly sickled cells, membrane exposure of phosphatidylserine and splenomegaly [20].
Genome-wide association studies
One drawback of the candidate gene approach is that of selection bias. Genome-wide association studies (GWAS) offered an unbiased approach by scanning thousands to millions of single nucleotide polymorphisms (SNPs) to find association with a disease trait. Obstacles of applying GWAS to sickle cell anemia and other hemoglobinopathies include: the limited sample sizes, the issue of LD, interpreting associations with SNPs when a biological connection is unclear, and dealing with gene-gene and gene-environment interactions [21].
GWAS have been used in sickle cell anemia to study the genetic associations of bilirubin [22–24], cholelithiasis [24], hemolysis [25], HbA2 level [26], tricuspid regurgitation velocity—a surrogate for pulmonary hypertension [27]—stroke [28] and systemic blood pressure—a surrogate for silent ischemic infarct [29]. The results for bilirubin and cholelithiasis were robust but expected, and identified the well know UGT1A gene family as the major regulator of bilirubin metabolism in African Americans with sickle cell anemia, as it is in other ethnicities [24]. Another well validated result was the association of a SNP in NPRL3 with hemolysis in sickle cell anemia [25]. In a first discovery cohort, a SNP in this gene was associated with hemolysis at a p value of 10−7. The association was replicated by GWAS in 2 additional independent cohorts and by targeted genotyping in a fourth independent cohort. The HBA1/HBA2 regulatory elements, hypersensitive sites (HS)-33, HS-40 and HS-48 are located in introns of NPRL3. The associated SNP was in high LD with SNPs in HS-33 and HS-40 and next to a transcriptional repressor CTCF binding site. The association with hemolysis remained after adjustment for HbF and gene deletion α thalassemia. Perhaps by independently down-regulating expression of the HBA1/HBA2 genes, variants tagged by this NPRL3 SNP reduce hemolysis in sickle cell anemia. Two studies, one in a normal population and the other in sickle cell anemia, showed that BCL11A, the HBS1l-MYB interval and variants in HBB were associated with HbA2 level. However, except for one SNP 3’ to HBB that was downstream of 3’ HS-1 and the 3D enhancer that had an independent effect on HbA2 in sickle cell anemia, the association was mediated through the effect of these loci on HbF level [26, 30].
GWAS have not validated any of the associations found in candidate gene association studies. This might be due to the stringency needed to accept an association by GWAS as “significant” that is generally accepted as 10-8, a level difficult to obtain without a sample size of many thousands or where the associated SNP has a large effect size.
NextGen sequencing
Massive parallel genomic sequencing approaches allow variant detection that is not captured by gene array methods. NexGen sequencing can be applied to the 3 billion bases of the whole genome, the 30 million bases of the exome or to the transcriptome (RNA-seq).
Whole exome sequencing was used to look for variants associated with stroke in sickle cell anemia [28]. There were 294 SNPs and 6 insertion-deletion variants that included 11 variants within 250 kb of at least 1 SNP identified by GWAS as correlating with stroke risk. A SNP in PON1 was previously associated with increased risk of strokes in adults [31, 32]. SNPs in GOLGB1 ENPP1 were validated but further confirmation and functional assessments of these genetic polymorphisms are needed to elucidate pathways involved in stroke pathogenesis and potentially direct targets for drug discovery.
Whole exome sequencing targets only 1 % of the genome, and most SNPs fall outside of exomes. For many traits like HbF, variation in regulatory regions—the regulome— have proven critical. Not all exons are covered in exome arrays or whole exome scans, so variants residing in the excluded exons will be missed. As the cost for whole genome sequencing falls below $1000 US the application of this technology will expand.
One study compared high-density exon arrays with RNA-seq to assess the peripheral blood transcriptome in sickle cell anemia [33]. There was 64 % concordance between exon array and RNA-seq technology for assessing differentially expressed transcripts. RNA-seq detected a higher magnitude of differential expression than exon arrays and was capable of detecting novel transcript variants in previously unannotated genomic regions.
The singular success of GWAS in β hemoglobinopathies was the totally unexpected discovery of the association of SNPs in BCL11A with HbF. This observation was first made in a very small number of carefully selected normal samples [34] and has since been widely replicated, studied functionally and mechanistically, and is now the subject of studies applying this basic observation to treatment.
The genomics of HbF regulation and its application to therapeutics
HbF is the major modulator of β hemoglobinopathies. Infants with sickle cell disease and β thalassemia are asymptomatic until HbF expression wanes as HBB expression begins to predominate [35].
HbF is the dominant hemoglobin of the fetus. Following birth, HbF is nearly totally replaced by HbA and the stable “adult” levels of HbF are normally achieved by age 6 months. In the β hemoglobinopathies, stable adult levels of HbF are not achieved until age 5 years in patients with sickle cell anemia of African origin while 10 years is needed before stable levels are seen in carriers of the Arab-Indian (AI) HBB haplotype [36]. The switch from HbF to HbA involves repression of HBG2 and HBG1 followed by up-regulation of HBB expression. It is never totally complete and some clones of erythroid precursors continue to produce progeny capable of expression of the HbF genes. Trace amounts of HbF, usually <1 %, are found in normal adults. Perhaps many clones are capable of expressing HbF but the amounts are below the current limits of detection of about 4 pg./cell. This could have important therapeutic applications as loci still able to express HbF might be more amenable to therapeutic up-regulation than loci where expression is nil.
HbF can persist at higher levels in adults. as part of a group of conditions known as hereditary persistence of HbF (HPFH) [37]. Perhaps the best example of the critical role HbF plays in the modulation of sickle cell anemia comes from the interaction of gene deletion HPFH with the HbS gene. Patients with the gene-deletion form of HPFH, who are also heterozygous for the HbS, have about 30 % HbF (10 pg./cell) distributed uniformly among all their erythrocytes [38]. They are clinically asymptomatic with nearly normal hematologic parameters [38]. Compound heterozygote for β thalassemia and HPFH are also mildly affected [39]. Non-gene deletion forms of HPFH are usually associated with a more modest increase in HbF and their HbF is usually distributed unevenly amongst erythrocytes. This is known as heterocellular HPFH [40]. Any degree of increase in HbF is likely to have clinically and therapeutically meaningful impact in sickle cell anemia [41–43]. Nevertheless, the distribution of HbF amongst the erythrocyte population of F-cells— erythrocytes containing measurable HbF— using flow cytometry is highly individualized and in patients with sickle cell anemia, individuals with the same total concentration of HbF can have very different erythrocyte distributions of HbF, perhaps explaining the heterogeneity of phenotypes found in patients with similar total HF level [44]. The therapeutic ideal for treatments directed at inducing high levels of HbF gene expression should therefor mimic the level and distribution of HbF seen in HbS-gene deletion HPFH where each erythrocyte has sufficient HbF to thwart deoxyHbS polymerization under physiological circumstances [38].
The genetics regulating the switch from HbF to HbA production involve multiple transcription factors interacting with each other and the promoters and enhancers of the β-like globin genes, and the epigenetic milieu of the chromatin involved [40, 45–51]. Modulation of HbF gene expression involves interaction of many different proteins including the transcription factors KLF1 and BCL11A, and the hematopoietic regulatory factor MYB with each other and with other genetic elements, like the master regulator of erythroid development GATA 1, and other co-repressor complexes that involve chromatin-modeling and epigenetic modifiers. Expanded and stress erythropoiesis is also needed for maximal expression of HbF [52, 53]. The complexity of these interactions and the transcription factors involved are shown in Fig. 2. The emerging network of HbF regulation has provided new insights and leads for therapeutic HbF reactivation. A 3.5 kb interval 5’ to HBD is an area with BCL11A-binding motifs suspected of having an important role in hemoglobin switching and whose deletion has been associated with increased HbF [54–56].
HbF Gene Expression is controlled by Cis- and Trans-acting elements. Shown, not to scale is the LCR, the γ-globin genes and the β-globin gene. γ-Globin and α globin (not shown) form HbF while β-globin and α globin form adult HbA. The major known transcription factors that have been implicated in hemoglobin switching are shown along with some of their interactions. One model holds that BCL11A participates as part of complexes of transcription factors like those shown to regulate the HbF to HbA switch. KLF1 binds the BCL11A promoter activating its expression and as shown has a dual effect switching by directly on activating HBB while repressing HBG2 and HBG1 indirectly by activating BCL11A. The cartoon does not illustrate the 3 dimensional interactions and the chromosome dynamics that include histone modification and methylation of critical regions of the HBB gene cluster.that are integral components of the transcription process. (Figure provided by and adapted from Orkin, SH, From GWAS-identified locus to reversing the fetal hemoglobin switch: Functional and genetic validation, in, Genomics: Gene discovery and clinical applications for cardiovascular, lung, and blood diseases. Sept. 2011, NIH, Bethesda, MD)
One of the first important discoveries linking genetic polymorphism to the variable clinical phenotype of β hemoglobinopathies was the finding that the sickle and β thalassemia globin mutations were present on different haplotypes of HBB [21, 57–59]. These haplotypes identified centers of origin of the HbS gene in Africa, the Middle East, and India. Some of the regional and ethnic differences in the severity of sickle cell anemia were associated with the HBB haplotype and this was explained by the HbF levels characteristic of each haplotype. The highest HbF levels in patients with sickle cell anemia are found in Eastern Saudi Arabia and Western India and in the West African region of Senegal. The AI and Senegal haplotypes extant in these regions have a C-T polymorphism 158 bp 5’ to HBG2 and known as the Xmn1 polymorphism (rs7482144) [60–62]. The Xmn1 polymorphism explains 2-10 % of the HbF variation and is associated with increased expression of HBG2 only [34, 63, 64]. Further analysis of the association of this polymorphism and HbF in African Americans with sickle cell anemia showed that rs10128556 downstream of HBG1 was more strongly associated with HbF than the Xmn1 site itself, and that conditioning the analysis on rs10128556 rendered the effect of Xmn1 on HbF insignificant. This suggested that the Xmn1 site is not the functional variant but that rs10128556 or a variant in LD with it might be the functional variant [65].
Although the AI and Senegal haplotypes share the Xmn1 restriction site polymorphism they differ in other polymorphisms linked to the HBB gene cluster. HbF in carriers of the AI haplotype is about twice as high as that in the African-origin Senegal haplotype. This is responsible for the less severe disease observed in children with the AI haplotype where HbF levels are about 30 % [62, 66–68]. When HbF falls as these patients become adults to levels about 20 %, their disease begins to resemble that seen in typical African-origin patients.
The molecular basis of high HbF concentrations in the AI compared with other HBB haplotypes of sickle cell disease is unknown. Compound heterozygotes with HbS-β0 thalassemia where the HbS gene is on the AI haplotype have similarly increased HbF levels suggesting that only a single AI haplotype is needed [69]. In sickle cell trait and the AI haplotype, HbF is normal, although BFU-e make more HbF than BFU-e from controls [70]. The high HbF associated with the AI haplotype requires hemolytic anemia in addition to the proper genetic background [49, 71]. Based on the known association of the HBB haplotype with HbF and the effects of polymorphisms of BCL11A and MYB on HbF gene expression, it is likely that the novel regulatory loci governing HbF in the AI haplotype are both cis and trans to the HBB gene cluster. The autochthonous nature of the HbS gene associated with the AI haplotypes implies that among the genetic differences distinguishing Saudi Arabs from other populations with sickle cell disease, a determinant that allows increased expression of the HbF genes is linked to the haplotype of the HBB gene cluster and differs from the functional variant in the Senegal haplotype [36, 72, 73]. Variation in the know trans-acting QTL, BCL11A and MYB did not distinguish high from low HbF AI haplotype patients and accounted for less than 10 % of their HbF variance. Variants in KLF1 did not explain HbF differences in the AI haplotype [36]. The nature of unique Arab or Indian trans- or cis-acting loci has yet to be defined.
Trans-acting HbF QTL
BCL11A:Genetic association studies using HbF as a phenotype have been propitious because of the high heritability of HbF and F-cells, the stability and quantitative nature of the phenotype and because—as luck would have it—a few quantitative trait loci explained between 10 to 50 % of HbF variability in a population [74, 75].
The GWAS that first found the association between BCL11A and HbF overcame the obstacle of having a small sample size by taking subjects from the extremes of HbF distribution scale [34]. Blood samples from 179 normal unrelated subjects from a United Kingdom twin’s registry, who were in the upper and lower 5th percentile at the extremes of F-cells were studied and a novel and totally unexpected QTL associated with increased F-cells mapped to a region on chromosome 2p containing the BCL11A gene. Two other regions on chr 6q23 and 11p15, the former containing the HBS1L-MYB region and the latter, the Xmn1 polymorphism, were known from prior linkage studies to influence HbF [60, 62, 63]. These findings were rapidly replicated by a larger GWAS studies looking for polymorphic associations with HbF from subjects with β thalassemia from Sardinia, in African Americans and in Chinese and Thai carriers of β thalassemia, and in HbE-β thalassemia [64, 76–81]. Functional studies showed that BCL11A protein is a repressor of γ-globin gene expression, acting at a distance and cooperating with the transcription factors GATA-1, FOG-1, and SOX6 [82, 83]. Discovery of BCL11A as a HbF QTL was proof of principle that GWAS could be used as an unbiased tool to define genotype-phenotype relationships.
It is now known that BCL11A expression is regulated by erythroid-specific enhancers in its 2nd intron. The enhancer elements contain 3 hypersensitive sites (HS) located +62, +58 and +55 kb from the transcription initiation site [84]. Two SNP haplotypes of the enhancer elements were associated with HbF levels in African American patients with sickle cell anemia. The strongest association with HbF levels in African Americans with sickle cell anemia was with rs1427407 in HS +62. Six BCL112A enhancer SNPs and their haplotypes were studied in Saudi Arabs from the Eastern Province and Indian patients with AI haplotype, African Americans, and Saudi Arabs from the Southwestern Province. Four enhancer SNPs (rs1427407, rs6706648, rs6738440, and rs7606173) and their haplotypes were consistently associated with HbF levels. The distributions of haplotypes differ in the 3 cohorts but not their genetic effects: the haplotype TCAG was associated with the lowest HbF level and the haplotype GTAC was associated with the highest HbF level. Differences in HbF levels between carriers of these haplotypes in all cohorts were approximately 6 %. Common HbF BCL11A enhancer haplotypes in patients with African origin and AI sickle cell anemia appeared to have similar effects on HbF but did not explain the differences in HbF among the HBB haplotypes [85].
HBS1L-MYB: The 3rd well established QTL modulating HF expression is the HBS1L-MYB intergenic region (HMIP) on chr6q23. This QTL was localized to a group of variants in tight LD in a 24-kb block referred to as HMIP-2 [63]. MYB has pleiotropic effects on erythroid traits like erythrocyte count, mean corpuscular volume, mean corpuscular hemoglobin, HbA2 levels, and also with platelet and monocyte counts. The causal polymorphisms reside in 2 clusters upstream of MYB [80, 86]. Functional studies in transgenic mice and primary human erythroid cells provide evidence that the SNPs at these two regions disrupt binding of key erythroid enhancers affecting long-range interactions with MYB and MYB expression and provide a functional explanation for the effects of this enhancer on HbF. A three-base pair (3 bp) deletion in HMIP-2 is one functional element in the MYB enhancers accounting for increased HbF expression in individuals who have the sentinel SNP rs9399137 common in Europeans and Asians but less frequent in African-origin populations. The DNA fragment encompassing the 3 bp deletion had enhancer-like activity that was augmented by the introduction of the 3 bp deletion [80]. Rare missense mutations of MYB were associated with increased HbF in African Americans with sickle cell anemia [65].
MYB is regulates hematopoiesis [87] and modulates HbF expression indirectly through alteration of the kinetics of erythroid differentiation and directly via activation of KLF1 and other repressors [88, 89]. When MYB levels are reduced erythroid differentiation is accelerated leading to release of early erythroid progenitor cells that are still synthesizing predominantly HbF. The wider role of MYB in hematopoiesis and the lack of a known erythroid-specific isoform limit the attractiveness of this gene as a target for modulating HbF expression.
KLF1: The association of KLF1 with HbF levels was first noted in a Maltese family with β thalassemia and an HPFH phenotype [90]. A locus on chromosome 19p13 containing KLF1 was identified and gene expression profiling confirmed KLF1 as the HbF modifier. Individuals with HPFH were heterozygous for a nonsense mutation in KLF1 that disrupted its DNA-binding domain. Many reports followed of different mutations in KLF1 associated with increases in HbF [91]. HbF increases secondary to KLF1 mutations are mediated through the effects of KLF1 on globin gene expression and also through its effects on erythropoiesis, the membrane or on cell metabolism [92–94]. KLF1 variants did not appear to be associated with HbF in β hemoglobinopathies based on the results of GWAS but with the small number of cases studied, rare variants are easily missed. In contrast to studies in Africa and Arab patients, KLF1 mutations were overrepresented in a southern Chinese population with β thalassemia [95]. Two mutations were also associated with a β thalassemia intermedia phenotype in β-thalassemia homozygotes.
KLF1 is a direct activator of BCL11A and is also essential for HBB expression [96–98]. Collectively, studies suggest that KLF1 is key in the switch from HbF to HbA expression; activating HBB directly and silencing HBG1 and HBG indirectly via activation of BCL11 [99]. The protean effects of KLF1 make it a less attractive therapeutic target than the erythroid-specific enhancers of BCL11A.
One application of genomics is to use the results in predictive or prognostic models. SNPs in candidate genes predicted the risk of stroke in sickle cell anemia using Bayesian network analysis [100]. Based on focused genotyping of HbF- associated QTL and on GWAS, genetic scores were developed for predicting the likelihood of acute painful episodes in sickle cell anemia, hematologic severity β thalassemia, the severity of HbE-β0 thalassemia, and for predicting HbF levels in sickle cell anemia [64, 76, 101–103].
Genomic approaches to HbF induction
Some possible approaches to therapeutically increasing HbF levels are shown in Table 2. Disruption of bcl11a in sickle mice abrogates the phenotype of sickle cell disease; about 30 % HbF is present in each sickle erythrocyte [47]. Biallelic excision of the bcl11a erythroid enhancers using TALENs reduced the level of bcl11a transcript and protein and increased the ratio of embryonic murine globin—a surrogate for human γ globin— to adult globin by 364-fold [84]. Similar approaches are being used to develop this technology as a means of increasing HbF in hemoglobinopathies.
The LCR enhancers have an important role controlling the expression of the β-like globin genes (Fig. 1). Its interaction with promoters of these genes modulate globin gene switching. This interaction is mediated by long-range protein interactions and among the key proteins mediating these interactions and a key element in the assembly of transcriptional activators is the LIM domain-binding protein of Ldb1 [104]. This protein does not bind DNA and has an amino acid N-terminal domain needed for multimerization. In erythroid cells, LDB1 interacts with LIM domain only 2 (LMO2) and the DNA-binding partners GATA1 and TAL1. Tethering the self-association domain of Ldb1 to artificial zinc-finger proteins that were targeted to β-globin promoter allowed activation of this gene and showed the importance of chromatin looping in transcription [105]. Furthermore, targeting the HbF gene promoters using forced looping strategies allowed their reactivation to the degree that γ globin accounted for about 85 % of total globin synthesis, while adult globin expression was reciprocally reduced [106]. This technology has the potential for reactivating HbF gene to therapeutically useful levels.
Other pathophysiology-based therapeutic approaches
The phenotype of sickle cell anemia is due to insufficient blood flow. Disrupting the interaction of sickle cells with endothelium should improve flow. In a phase II study (NCT00773890), an oral P-selectin blocker used chronically lowered plasma sVCAM and showed a trend toward improving microvascular flow [107]. A phase II trial of a pan-selectin blocker (NCT01119833) used at the time of an acute event to reduce the length of sickle vasoocclusive events has yet to report the full results, but a phase III study is planned. A block-copolymer was used acutely to improve flow and decrease sickle vasoocclusion (NCT00004408). The first pilot study lead to a phase III trial that showed some efficacy in younger patients and another phase III trial (NCT017378140) is underway [108, 109]. Finally, a phase II study of an anti-P-selectin antibody is ongoing (NCT01895361). These studies, even if successful, are years away from clinical application. Logic suggests that agents that sustain flow and prevent the initiation of vasoocclusion would be more successful than agents given after an acute vasoocclusive event has started, nevertheless animal studies have shown that this latter approach might be useful [110]. Logic also has it that preventing HbS polymerization would abrogate the need for any treatment that targets events downstream of this causative event.
Other early phase trials are based on improving the inflammation that is a result of sickle vasoocclusion and vasculopathy by reducing the activation of invariant natural killer T-cells (NCT01788631) and using a statin as an anti-inflammatory (NCT01702246).
Novel approaches to treating β thalassemia based on pathophysiology have recently been summarized [111]. In distinction to sickle cell anemia, ineffective erythropoiesis is a major feature of severe β thalassemia and contributes to the anemia that is the cardinal feature of this disorder. So, as expected, one focus of drug development has been on repairing anemia. Most of the studies of novel therapeutic have been done in murine β thalassemia and work in man is lags behind studies in sickle cell disease. Among the potential treatment are JAK2 inhibitors, which decrease erythropoiesis, at least in thalassemic mice, and is the subject of a phase IIa trial (NCT02049450). In man, the enlarged spleen is a major site of extramedullary erythropoiesis and red cell destruction. As discussed above, a receptor-II trap ligand inhibits Smad2/3 by targeting gdf11 and improves anemia in thalassemic mice by decreasing stress erythropoiesis. This agent is also in a phase IIa trial (NCT01571635) [20].
Another general approach is to target iron overload that contributes to ineffective erythropoiesis by using hepcidin agonists [112], reducing hepcidin expression by targeting tmprss6 a protease that attenuates its expression [113], and using apo-transferrin to decrease labile plasma iron [114].
Review and conclusions
Genomic research and bioinformatics have evolved rapidly. The technological advancements in genetics have increased our understanding of hemoglobin gene regulation and the influences of genetic variation on disease phenotypes but have proven less valuable for identifying new therapeutic targets other than those focused on HbF regulation. The greatest successes of genomics have been those surrounding HbF gene regulation where the initial discoveries have been amply validated and causal variants identified by in vitro and in vivo mechanistic studies. Although molecular-based techniques such as gene replacement therapy, somatic cell reprogramming, and stem cell transplant are advancing, the application of these strategies require substantial financial and technological resources. This poses serious challenges for countries where most patients with severe hemoglobin disorders reside. For these reasons, pharmacologic approaches to optimize HbF switching may be the most attractive strategy for controlling these diseases.
Abbreviations
- HbA:
-
Adult hemoglobin
- AI:
-
Arab-Indian haplotype
- HS:
-
DNase hypersensitive sites
- HbF:
-
Fetal hemoglobin
- GWAS:
-
Genome-wide association studies
- HMIP:
-
HBS1L-MYB intergenic region
- JAK2:
-
Janus kinase 2
- LD:
-
Linkage disequilibrium
- LCR:
-
Locus control region
- QTL:
-
Quantitative trait locus
- RNA-seq:
-
RNA sequencing
- HbS:
-
Sickle hemoglobin
- sVCAM:
-
Soluble vascular cell adhesion molecule
- 3 bp:
-
Three-base pair
References
Giardine B, Borg J, Viennas E, Pavlidis C, Moradkhani K, Joly P, et al. Updates of the HbVar database of human hemoglobin variants and thalassemia mutations. Nucl Acids Res. 2014;42:D1063–1069.
Piel FB, Weatherall DJ. The alpha-thalassemias. N Engl J Med. 2014;371:1908–16.
Piel FB, Hay SI, Gupta S, Weatherall DJ, Williams TN. Global burden of sickle cell anaemia in children under five, 2010–2050: modelling based on demographics, excess mortality, and interventions. PLoS Med. 2013;10:e1001484.
Colah R, Gorakshakar A, Nadkarni A. Global burden, distribution and prevention of beta-thalassemias and hemoglobin E disorders. Expert Rev Hematol. 2010;3:103–17.
Organization WH. Management of Haemoglobin Disorders, Report of Joint WHO/TIF Meeting. Nicosia: Cyprus; 2007.
Yuan J, Bunyaratvej A, Fucharoen S, Fung C, Shinar E, Schrier SL. The instability of the membrane skeleton in thalassemic red blood cells. Blood. 1995;86:3945–50.
Steinberg MH, Embury SH. Alpha-thalassemia in blacks: genetic and clinical aspects and interactions with the sickle hemoglobin gene. Blood. 1986;68:985–90.
Steinberg MH, Sebastiani P. Genetic modifiers of sickle cell disease. Am J Hematol. 2012;87:824–6.
Taylor JG, Nolan VG, Mendelsohn L, Kato GJ, Gladwin MT, Steinberg MH. Chronic hyper-hemolysis in sickle cell anemia: association of vascular complications and mortality with less frequent vasoocclusive pain. PLoS One. 2008;3:e2095.
Kato GJ, Gladwin MT, Steinberg MH. Deconstructing sickle cell disease: reappraisal of the role of hemolysis in the development of clinical subphenotypes. Blood Rev. 2007;21:37–47.
Gallagher PG. Disorders of red cell volume regulation. Curr Opin Hematol. 2013;20:201–7.
Ataga KI, Reid M, Ballas SK, Yasin Z, Bigelow C, James LS, et al. Improvements in haemolysis and indicators of erythrocyte survival do not correlate with acute vaso-occlusive crises in patients with sickle cell disease: a phase III randomized, placebo-controlled, double-blind study of the Gardos channel blocker senicapoc (ICA-17043). Br J Haematol. 2011;153:92–104.
Cardon LR, Bell JI. Association study designs for complex diseases. Nat Rev Genet. 2001;2:91–9.
Lettre G. The search for genetic modifiers of disease severity in the beta-hemoglobinopathies. Cold Spring Harb Perspect Med. 2012; 2(10). doi10.1101/cshperspect.a015032.
Akhurst RJ, Hata A. Targeting the TGFbeta signalling pathway in disease. Nat Rev Drug Discov. 2012;11:790–811.
Derynck R, Zhang YE. Smad-dependent and Smad-independent pathways in TGF-beta family signalling. Nature. 2003;425:577–84.
Bertolino P, Deckers M, Lebrin F, ten Dijke P. Transforming growth factor-beta signal transduction in angiogenesis and vascular disorders. Chest. 2005;128:585S–90S.
Pober JS, Cotran RS. The role of endothelial cells in inflammation. Transplantation. 1990;50:537–44.
Solovey A, Lin Y, Browne P, Choong S, Wayner E, Hebbel RP. Circulating activated endothelial cells in sickle cell anemia. N Engl J Med. 1997;337:1584–90.
Suragani RN, Cawley SM, Li R, Wallner S, Alexander MJ, Mulivor AW, et al. Modified activin receptor IIB ligand trap mitigates ineffective erythropoiesis and disease complications in murine beta-thalassemia. Blood. 2014;123:3864–72.
Steinberg MH, Nagel RL. Genetic modulation of sickle cell disease and thalassemia. In: Steinberg MH, Forget BG, Higgs DR, Weatherall D, editors. Disorders of Hemoglobin: Genetics, Pathophysiology, and Clinical Management. 2nd ed. New York, NY: Cambridge University Press; 2009. p. 638–57.
Passon RG, Howard TA, Zimmerman SA, Schultz WH, Ware RE. Influence of bilirubin uridine diphosphate-glucuronosyltransferase 1A promoter polymorphisms on serum bilirubin levels and cholelithiasis in children with sickle cell anemia. J Pediatr Hematol Oncol. 2001;23:448–51.
Fertrin KY, Melo MB, Assis AM, Saad ST, Costa FF. UDP-glucuronosyltransferase 1 gene promoter polymorphism is associated with increased serum bilirubin levels and cholecystectomy in patients with sickle cell anemia. Clin Genet. 2003;64:160–2.
Milton JN, Sebastiani P, Solovieff N, Hartley SW, Bhatnagar P, Arking DE, et al. A genome-wide association study of total bilirubin and cholelithiasis risk in sickle cell anemia. PLoS One. 2012;7:e34741.
Milton JN, Rooks H, Drasar E, McCabe EL, Baldwin CT, Melista E, et al. Genetic determinants of haemolysis in sickle cell anaemia. Br J Haematol. 2013;161:270–8.
Griffin PJ, Sebastiani P, Edward H, Baldwin CT, Gladwin MT, Gordeuk VR, et al. The genetics of hemoglobin A2 regulation in sickle cell anemia. Am J Hematol. 2014;89:1019–23.
Desai AA, Zhou T, Ahmad H, Zhang W, Mu W, Trevino S, et al. A novel molecular signature for elevated tricuspid regurgitation velocity in sickle cell disease. Am J Respir Crit Care Med. 2012;186:359–68.
Flanagan JM, Sheehan V, Linder H, Howard TA, Wang YD, Hoppe CC, et al. Genetic mapping and exome sequencing identify 2 mutations associated with stroke protection in pediatric patients with sickle cell anemia. Blood. 2013;121:3237–45.
Bhatnagar P, Barron-Casella E, Bean CJ, Milton JN, Baldwin CT, Steinberg MH, et al. Genome-wide meta-analysis of systolic blood pressure in children with sickle cell disease. PLoS One. 2013;8:e74193.
Menzel S, Garner C, Rooks H, Spector TD, Thein SL. HbA2 levels in normal adults are influenced by two distinct genetic mechanisms. Br J Haematol. 2013;160:101–5.
Bhattacharyya T, Nicholls SJ, Topol EJ, Zhang R, Yang X, Schmitt D, et al. Relationship of paraoxonase 1 (PON1) gene polymorphisms and functional activity with systemic oxidative stress and cardiovascular risk. JAMA. 2008;299:1265–76.
Luu HN, Kingah PL, North K, Boerwinkle E, Volcik KA. Interaction of folate intake and the paraoxonase Q192R polymorphism with risk of incident coronary heart disease and ischemic stroke: the atherosclerosis risk in communities study. Ann Epidemiol. 2011;21:815–23.
Raghavachari N, Barb J, Yang Y, Liu P, Woodhouse K, Levy D, et al. A systematic comparison and evaluation of high density exon arrays and RNA-seq technology used to unravel the peripheral blood transcriptome of sickle cell disease. BMC Med Genomics. 2012;5:28.
Menzel S, Garner C, Gut I, Matsuda F, Yamaguchi M, Heath S, et al. A QTL influencing F cell production maps to a gene encoding a zinc-finger protein on chromosome 2p15. Nat Genet. 2007;39:1197–9.
Watson J. The significance of the paucity of sickle cells in newborn Negro infants. Am J Med Sci. 1948;215:419–23.
Ngo D, Bae H, Steinberg MH, Sebastiani P, Solovieff N, Baldwin CT, et al. Fetal hemoglobin in sickle cell anemia: genetic studies of the Arab-Indian haplotype. Blood Cells, Mol & Dis. 2013;51:22–6.
Forget BG. Molecular basis of hereditary persistence of fetal hemoglobin. Ann N Y Acad Sci. 1998;850:38–44.
Ngo DA, Aygun B, Akinsheye I, Hankins JS, Bhan I, Luo HY, et al. Fetal haemoglobin levels and haematological characteristics of compound heterozygotes for haemoglobin S and deletional hereditary persistence of fetal haemoglobin. Br J Haematol. 2012;156:259–64.
Weatherall DJ, Clegg JB. The Thalassaemia Syndromes. Oxford: Blackwell Science; 2001.
Thein SL, Menzel S, Lathrop M, Garner C. Control of fetal hemoglobin: new insights emerging from genomics and clinical implications. Hum Mol Genet. 2009;18:R216–23.
Platt OS, Thorington BD, Brambilla DJ, Milner PF, Rosse WF, Vichinsky E, et al. Pain in sickle cell disease. Rates and risk factors. N Engl J Med. 1991;325:11–6.
Platt OS. Easing the suffering caused by sickle cell disease. N Engl J Med. 1994;330:783–4.
Steinberg MH, Barton F, Castro O, Pegelow CH, Ballas SK, Kutlar A, et al. Effect of hydroxyurea on mortality and morbidity in adult sickle cell anemia: risks and benefits up to 9 years of treatment. JAMA. 2003;289:1645–51.
Steinberg MH, Chui DH, Dover GJ, Sebastiani P, Alsultan A. Fetal hemoglobin in sickle cell anemia: a glass half full? Blood. 2014;123:481–5.
Wilber A, Nienhuis AW, Persons DA. Transcriptional regulation of fetal to adult hemoglobin switching: new therapeutic opportunities. Blood. 2011;117:3945–53.
Sankaran VG, Xu J, Orkin SH. Advances in the understanding of haemoglobin switching. Br J Haematol. 2010;149:181–94.
Xu J, Peng C, Sankaran VG, Shao Z, Esrick EB, Chong BG, et al. Correction of sickle cell disease in adult mice by interference with fetal hemoglobin silencing. Science. 2011;334:993–6.
Bauer DE, Orkin SH. Update on fetal hemoglobin gene regulation in hemoglobinopathies. Curr Opin Pediatr. 2011;23:1–8.
Stamatoyannopoulos G. Control of globin gene expression during development and erythroid differentiation. Exp Hematol. 2005;33:259–71.
Bauer DE, Kamran SC, Orkin SH. Reawakening fetal hemoglobin: prospects for new therapies for the beta-globin disorders. Blood. 2012;120:2945–53.
Sankaran VG, Orkin SH. The switch from fetal to adult hemoglobin. Cold Spring Harb Perspect Med. 2013;3:a011643.
Stamatoyannopoulos G, Veith R, Galanello R, Papayannopoulou T. Hb F production in stressed erythropoiesis: observations and kinetic models. Ann NY Acad Sci. 1985;445:188–97.
Xiang J, Wu DC, Chen Y, Paulson RF. In vitro culture of stress erythroid progenitors identifies distinct progenitor populations and analogous human progenitors. Blood. 2015;125:1803–12.
Sankaran VG, Xu J, Byron R, Greisman HA, Fisher C, Weatherall DJ, et al. A functional element necessary for fetal hemoglobin silencing. N Engl J Med. 2011;365:807–14.
Kulozik AE, Yarwood N, Jones RW. The Corfu delta beta zero thalassemia: a small deletion acts at a distance to selectively abolish beta globin gene expression. Blood. 1988;71:457–62.
Prakobkaew N, Fucharoen S, Fuchareon G, Siriratmanawong N. Phenotypic expression of Hb F in common high Hb F determinants in Thailand: roles of alpha-thalassemia, 5' delta-globin BCL11A binding region and 3' beta-globin enhancer. Eur J Haematol. 2014;92:73–9.
Orkin SH, Antonarakis SE, Kazazian Jr HH. Polymorphism and molecular pathology of the human beta-globin gene. Prog Hematol. 1983;13:49–73.
Antonarakis SE, Kazazian Jr HH, Orkin SH. DNA polymorphism and molecular pathology of the human globin gene clusters. Hum Genet. 1985;69:1–14.
Pagnier J, Mears JG, Dunda-Belkhodja O, Schaefer-Rego KE, Beldjord C, Nagel RL, et al. Evidence for the multicentric origin of the sickle cell hemoglobin gene in Africa. Proc Natl Acad Sci USA. 1984;81:1771–3.
Labie D, Dunda-Belkhodja O, Rouabhi F, Pagnier J, Ragusa A, Nagel RL. The −158 site 5' to the G gamma gene and G gamma expression. Blood. 1985;66:1463–5.
Labie D, Pagnier J, Lapoumeroulie C, Rouabhi F, Dunda-Belkhodja O, Chardin P, et al. Common haplotype dependency of high G gamma-globin gene expression and high Hb F levels in beta-thalassemia and sickle cell anemia patients. Proc Natl Acad Sci USA. 1985;82:2111–4.
Miller BA, Olivieri N, Salameh M, Ahmed M, Antognetti G, Huisman TH, et al. Molecular analysis of the high-hemoglobin-F phenotype in Saudi Arabian sickle cell anemia. N Engl J Med. 1987;316:244–50.
Thein SL, Menzel S, Peng X, Best S, Jiang J, Close J, et al. Intergenic variants of HBS1L-MYB are responsible for a major quantitative trait locus on chromosome 6q23 influencing fetal hemoglobin levels in adults. Proc Natl Acad Sci USA. 2007;104:11346–51.
Lettre G, Sankaran VG, Bezerra MA, Araujo AS, Uda M, Sanna S, et al. DNA polymorphisms at the BCL11A, HBS1L-MYB, and beta-globin loci associate with fetal hemoglobin levels and pain crises in sickle cell disease. Proc Natl Acad Sci USA. 2008;105:11869–74.
Galarneau G, Palmer CD, Sankaran VG, Orkin SH, Hirschhorn JN, Lettre G. Fine-mapping at three loci known to affect fetal hemoglobin levels explains additional genetic variation. Nat Genet. 2010;42:1049–51.
Perrine RP, Brown MJ, Clegg JB, Weatherall DJ, May A. Benign sickle-cell anaemia. Lancet. 1972;2:1163–7.
Pembrey ME, Wood WG, Weatherall DJ, Perrine RP. Fetal haemoglobin production and the sickle gene in the oases of Eastern Saudi Arabia. Br J Haematol. 1978;40:415–29.
Alsultan A, Alabdulaali MK, Griffin PJ, Alsuliman AM, Ghabbour HA, Sebastiani P, et al. Sickle cell disease in Saudi Arabia: the phenotype in adults with the Arab-Indian haplotype is not benign. Br J Haematol. 2014;164:597–604.
Alsultan A, Ngo D, Bae H, Sebastiani P, Baldwin CT, Melista E, et al. Genetic studies of fetal hemoglobin in the Arab-Indian haplotype sickle cell-beta(0) thalassemia. Am J Hematol. 2013;88:531–2.
Miller BA, Salameh M, Ahmed M, Wainscoat J, Antognetti G, Orkin S, et al. High fetal hemoglobin production in sickle cell anemia in the eastern province of Saudi Arabia is genetically determined. Blood. 1986;67:1404–10.
Mabaera R, West RJ, Conine SJ, Macari ER, Boyd CD, Engman CA, et al. A cell stress signaling model of fetal hemoglobin induction: what doesn't kill red blood cells may make them stronger. Exp Hematol. 2008;36:1057–72.
Alsultan A, Solovieff N, Aleem A, AlGahtani FH, Al-Shehri A, Osman ME, et al. Fetal hemoglobin in sickle cell anemia: Saudi patients from the Southwestern province have similar HBB haplotypes but higher HbF levels than African Americans. Am J Hematol. 2011;86:612–4.
Akinsheye I, Alsultan A, Solovieff N, Ngo D, Baldwin CT, Sebastiani P, et al. Fetal hemoglobin in sickle cell anemia. Blood. 2011;118:19–27.
Garner C, Tatu T, Reittie JE, Littlewood T, Darley J, Cervino S, et al. Genetic influences on F cells and other hematologic variables: a twin heritability study. Blood. 2000;95:342–6.
Gibney GT, Panhuysen CI, So JC, Ma ES, Ha SY, Li CK, et al. Variation and heritability of Hb F and F-cells among beta-thalassemia heterozygotes in Hong Kong. Am J Hematol. 2008;83:458–64.
Nuinoon M, Makarasara W, Mushiroda T, Setianingsih I, Wahidiyat PA, Sripichai O, et al. A genome-wide association identified the common genetic variants influence disease severity in beta0-thalassemia/hemoglobin E. Hum Genet. 2010;127:303–14.
Uda M, Galanello R, Sanna S, Lettre G, Sankaran VG, Chen W, et al. Genome-wide association study shows BCL11A associated with persistent fetal hemoglobin and amelioration of the phenotype of beta-thalassemia. Proc Natl Acad Sci USA. 2008;105:1620–5.
Sedgewick A, Timofeev N, Sebastiani P, So JCC, Ma ESK, Chan LC, et al. BCL11A (2p16) is a major HbF quantitative trait locus in three different populations. Blood Cells Mol & Dis. 2008;41:255–8.
Solovieff N, Milton JN, Hartley SW, Sherva R, Sebastiani P, Dworkis DA, et al. Fetal hemoglobin in sickle cell anemia: genome-wide association studies suggest a regulatory region in the 5' olfactory receptor gene cluster. Blood. 2010;115:1815–22.
Farrell JJ, Sherva RM, Chen ZY, Luo HY, Chu BF, Ha SY, et al. A 3-bp deletion in the HBS1L-MYB intergenic region on chromosome 6q23 is associated with HbF expression. Blood. 2011;117:4935–45.
Galanello R, Sanna S, Perseu L, Sollaino MC, Satta S, Lai ME, et al. Amelioration of Sardinian beta0 thalassemia by genetic modifiers. Blood. 2009;114:3935–7.
Sankaran VG, Menne TF, Xu J, Akie TE, Lettre G, Van Handel B, et al. Human fetal hemoglobin expression is regulated by the developmental stage-specific repressor BCL11A. Science. 2008;322:1839–42.
Xu J, Sankaran VG, Ni M, Menne TF, Puram RV, Kim W, et al. Transcriptional silencing of {gamma}-globin by BCL11A involves long-range interactions and cooperation with SOX6. Genes Dev. 2010;24:783–98.
Bauer DE, Kamran SC, Lessard S, Xu J, Fujiwara Y, Lin C, et al. An erythroid enhancer of BCL11A subject to genetic variation determines fetal hemoglobin level. Science. 2013;342:253–7.
Sebastiani P, Farrell JJ, Alsultan A, Wang S, Edward HL, Shapell H, Bae H, Milton JN, Baldwin CT, Al-Rubaish AM, et al. BCL11A enhancer haplotypes and fetal hemoglobin in sickle cell anemia Blood Cells Mol Dis 2015;54:224–230.
Stadhouders R, Aktuna S, Thongjuea S, Aghajanirefah A, Pourfarzad F, van Ijcken W, et al. HBS1L-MYB intergenic variants modulate fetal hemoglobin via long-range MYB enhancers. J Clin Iinvest. 2014;124:1699–710.
Vegiopoulos A, Garcia P, Emambokus N, Frampton J. Coordination of erythropoiesis by the transcription factor c-Myb. Blood. 2006;107:4703–10.
Bianchi E, Zini R, Salati S, Tenedini E, Norfo R, Tagliafico E, et al. c-myb supports erythropoiesis through the transactivation of KLF1 and LMO2 expression. Blood. 2010;116:e99–110.
Tallack MR, Perkins AC. Three fingers on the switch: Kruppel-like factor 1 regulation of gamma-globin to beta-globin gene switching. Curr Opin Hematol. 2013;20:193–200.
Borg J, Papadopoulos P, Georgitsi M, Gutierrez L, Grech G, Fanis P, et al. Haploinsufficiency for the erythroid transcription factor KLF1 causes hereditary persistence of fetal hemoglobin. Nat Genet. 2010;42:801–5.
Borg J, Patrinos GP, Felice AE, Philipsen S. Erythroid phenotypes associated with KLF1 mutations. Haematologica. 2011;96:635–8.
Arnaud L, Saison C, Helias V, Lucien N, Steschenko D, Giarratana MC, et al. A dominant mutation in the gene encoding the erythroid transcription factor KLF1 causes a congenital dyserythropoietic anemia. Am J Hum Genet. 2010;87:721–7.
Jaffray JA, Mitchell WB, Gnanapragasam MN, Seshan SV, Guo X, Westhoff CM, et al. Erythroid transcription factor EKLF/KLF1 mutation causing congenital dyserythropoietic anemia type IV in a patient of Taiwanese origin: review of all reported cases and development of a clinical diagnostic paradigm. Blood Cells, Mol Dis. 2013;51:71–5.
Viprakasit V, Ekwattanakit S, Riolueang S, Chalaow N, Fisher C, Lower K, et al. Mutations in Kruppel-like factor 1 cause transfusion-dependent hemolytic anemia and persistence of embryonic globin gene expression. Blood. 2014;123:1586–95.
Liu D, Zhang X, Yu L, Cai R, Ma X, Zheng C, et al. KLF1 mutations are relatively more common in a thalassemia endemic region and ameliorate the severity of beta-thalassemia. Blood. 2014;124:803–11.
Esteghamat F, Gillemans N, Bilic I, van den Akker E, Cantu I, van Gent T, et al. Erythropoiesis and globin switching in compound Klf1::Bcl11a mutant mice. Blood. 2013;121:2553–62.
Zhou D, Liu K, Sun CW, Pawlik KM, Townes TM. KLF1 regulates BCL11A expression and gamma- to beta-globin gene switching. Nat Genet. 2010;42:742–4.
Siatecka M, Bieker JJ. The multifunctional role of EKLF/KLF1 during erythropoiesis. Blood. 2011;118:2044–54.
Yien YY, Bieker JJ. EKLF/KLF1, a tissue-restricted integrator of transcriptional control, chromatin remodeling, and lineage determination. Mol Cell Biol. 2013;33:4–13.
Sebastiani P, Ramoni MF, Nolan V, Baldwin CT, Steinberg MH. Genetic dissection and prognostic modeling of overt stroke in sickle cell anemia. Nat Genet. 2005;37:435–40.
Danjou F, Francavilla M, Anni F, Satta S, Demartis FR, Perseu L, et al. A genetic score for the prediction of beta-thalassemia severity. Haematologica. 2014;100:452–7.
Milton JN, Gordeuk VR, Taylor JG, Gladwin MT, Steinberg MH, Sebastiani P. Prediction of fetal hemoglobin in sickle cell anemia using an ensemble of genetic risk prediction models. Circulation Cardiovascular Genet. 2014;7:110–5.
Ma Q, Abel K, Sripichai O, Whitacre J, Angkachatchai V, Makarasara W, et al. Beta-globin gene cluster polymorphisms are strongly associated with severity of HbE/beta(0)-thalassemia. Clin Genet. 2007;72:497–505.
Love PE, Warzecha C, Li L. Ldb1 complexes: the new master regulators of erythroid gene transcription. Trends in Genet : TIG. 2014;30:1–9.
Deng W, Lee J, Wang H, Miller J, Reik A, Gregory PD, et al. Controlling long-range genomic interactions at a native locus by targeted tethering of a looping factor. Cell. 2012;149:1233–44.
Deng W, Rupon JW, Krivega I, Breda L, Motta I, Jahn KS, et al. Reactivation of developmentally silenced globin genes by forced chromatin looping. Cell. 2014;158:849–60.
Kutlar A, Ataga KI, McMahon L, Howard J, Galacteros F, Hagar W, et al. A potent oral P-selectin blocking agent improves microcirculatory blood flow and a marker of endothelial cell injury in patients with sickle cell disease. Am J Hematol. 2012;87:536–9.
Adams-Graves P, Kedar A, Koshy M, Steinberg M, Veith R, Ward D, et al. RheothRx (poloxamer 188) injection for the acute painful episode of sickle cell disease: A pilot study. Blood. 1997;90:2041–6.
Orringer EP, Casella JF, Ataga KI, Koshy M, Adams-Graves P, Luchtman-Jones L, et al. Purified poloxamer 188 for treatment of acute vaso-occlusive crisis of sickle cell disease: A randomized controlled trial. JAMA. 2001;286:2099–106.
Chang J, Patton JT, Sarkar A, Ernst B, Magnani JL, Frenette PS. GMI-1070, a novel pan-selectin antagonist, reverses acute vascular occlusions in sickle cell mice. Blood. 2010;116:1779–86.
Rivella S. β-thalassemias: paradigmatic diseases for scientific discoveries and development of innovative therapies. Haematologica. 2015;100:418–30.
Ramos E, Ruchala P, Goodnough JB, Kautz L, Preza GC, Nemeth E, et al. Minihepcidins prevent iron overload in a hepcidin-deficient mouse model of severe hemochromatosis. Blood. 2012;120:3829–36.
Nai A, Pagani A, Mandelli G, Lidonnici MR, Silvestri L, Ferrari G, et al. Deletion of TMPRSS6 attenuates the phenotype in a mouse model of beta-thalassemia. Blood. 2012;119:5021–9.
Li H, Rybicki AC, Suzuka SM, von Bonsdorff L, Breuer W, Hall CB, et al. Transferrin therapy ameliorates disease in beta-thalassemic mice. Nat Med. 2010;16:177–82.
Flanagan JM, Frohlich DM, Howard TA, Schultz WH, Driscoll C, Nagasubramanian R, et al. Genetic predictors for stroke in children with sickle cell anemia. Blood. 2011;117:6681–4.
Taylor JG, Tang DC, Savage SA, Leitman SF, Heller SI, Serjeant GR, et al. Variants in the VCAM1 gene and risk for symptomatic stroke in sickle cell disease. Blood. 2002;100:4303–9.
Hoppe C, Klitz W, Cheng S, Apple R, Steiner L, Robles L, et al. Gene interactions and stroke risk in children with sickle cell anemia. Blood. 2004;103:2391–6.
Mendonca TF, Oliveira MC, Vasconcelos LR, Pereira LM, Moura P, Bezerra MA, et al. Association of variant alleles of MBL2 gene with vasoocclusive crisis in children with sickle cell anemia. Blood Cells Mol Dis. 2010;44:224–8.
Oliveira MC, Mendonca TF, Vasconcelos LR, Moura P, Bezerra MA, Santos MN, et al. Association of the MBL2 gene EXON1 polymorphism and vasoocclusive crisis in patients with sickle cell anemia. Acta Haematol. 2009;121:212–5.
Galarneau G, Coady S, Garrett ME, Jeffries N, Puggal M, Paltoo D, et al. Gene-centric association study of acute chest syndrome and painful crisis in sickle cell disease patients. Blood. 2013;122:434–42.
Martinez-Castaldi C, Nolan VG, Baldwin CT, Farrer LA, Steinberg MH, Klings ES. Association of genetic polymorphisms in the TGF-β pathway with the acute chest syndrome of sickle cell anemia. ASH Annual Meeting Abstracts. 2007;110:2247.
Bean CJ, Boulet SL, Ellingsen D, Pyle ME, Barron-Casella EA, Casella JF, et al. Heme oxygenase-1 gene promoter polymorphism is associated with reduced incidence of acute chest syndrome among children with sickle cell disease. Blood. 2012;120:3822–8.
Sharan K, Surrey S, Ballas S, Borowski M, Devoto M, Wang KF, et al. Association of T-786C eNOS gene polymorphism with increased susceptibility to acute chest syndrome in females with sickle cell disease. Br J Haematol. 2004;124:240–3.
de Oliveira Filho RA, Silva GJ, de Farias Domingos I, Hatzlhofer BL, da Silva Araujo A, de Lima Filho JL, et al. Association between the genetic polymorphisms of glutathione S-transferase (GSTM1 and GSTT1) and the clinical manifestations in sickle cell anemia. Blood Cells Mol Dis. 2013;51:76–9.
Neonato MG, Lu CY, Guilloud-Bataille M, Lapoumeroulie C, Nabeel-Jassim H, Dabit D, et al. Genetic polymorphism of the mannose-binding protein gene in children with sickle cell disease: identification of three new variant alleles and relationship to infections. Eur J Hum Genet. 1999;7:679–86.
Adewoye AH, Nolan VG, Ma Q, Baldwin C, Wyszynski DF, Farrell JJ, et al. Association of polymorphisms of IGF1R and genes in the transforming growth factor- beta /bone morphogenetic protein pathway with bacteremia in sickle cell anemia. Clin Infect Dis. 2006;43:593–8.
Dossou-Yovo OP, Zaccaria I, Benkerrou M, Hauchecorne M, Alberti C, Rahimy MC, et al. Effects of RANTES and MBL2 gene polymorphisms in sickle cell disease clinical outcomes: association of the g.In1.1T > C RANTES variant with protection against infections. Am J Hematol. 2009;84:378–80.
Tamouza R, Neonato MG, Busson M, Marzais F, Girot R, Labie D, et al. Infectious complications in sickle cell disease are influenced by HLA class II alleles. Hum Immunol. 2002;63:194–9.
Tamouza R, Busson M, Fortier C, Diagne I, Diallo D, Sloma I, et al. HLA-E*0101 allele in homozygous state favors severe bacterial infections in sickle cell anemia. Hum Immunol. 2007;68:849–53.
Baldwin C, Nolan VG, Wyszynski DF, Ma QL, Sebastiani P, Embury SH, et al. Association of klotho, bone morphogenic protein 6, and annexin A2 polymorphisms with sickle cell osteonecrosis. Blood. 2005;106:372–5.
Ulug P, Vasavda N, Awogbade M, Cunningham J, Menzel S, Thein SL. Association of sickle avascular necrosis with bone morphogenic protein 6. Ann Hematol. 2009;88:803–5.
Nolan VG, Baldwin C, Ma Q, Wyszynski DF, Amirault Y, Farrell JJ, et al. Association of single nucleotide polymorphisms in klotho with priapism in sickle cell anaemia. Br J Haematol. 2005;128:266–72.
Elliott L, Ashley-Koch AE, De Castro L, Jonassaint J, Price J, Ataga KI, et al. Genetic polymorphisms associated with priapism in sickle cell disease. Br J Haematol. 2007;137:262–7.
Nolan VG, Adewoye A, Baldwin C, Wang L, Ma Q, Wyszynski DF, et al. Sickle cell leg ulcers: associations with haemolysis and SNPs in Klotho, TEK and genes of the TGF-beta/BMP pathway. Br J Haematol. 2006;133:570–8.
Ofosu MD, Castro O, Alarif L. Sickle cell leg ulcers are associated with HLA-B35 and Cw4. Arch Dermatol. 1987;123:482–4.
Ashley-Koch AE, Okocha EC, Garrett ME, Soldano K, De Castro LM, Jonassaint JC, et al. MYH9 and APOL1 are both associated with sickle cell disease nephropathy. Br J Haematol. 2011;155:386–94.
Nolan VG, Ma Q, Cohen HT, Adewoye A, Rybicki AC, Baldwin C, et al. Estimated glomerular filtration rate in sickle cell anemia is associated with polymorphisms of bone morphogenetic protein receptor 1B. Am J Hematol. 2007;82:179–84.
Carpenter SL, Lieff S, Howard TA, Eggleston B, Ware RE. UGT1A1 promoter polymorphisms and the development of hyperbilirubinemia and gallbladder disease in children with sickle cell anemia. Am J Hematol. 2008;83:800–3.
Ashley-Koch AE, Elliott L, Kail ME, De Castro LM, Jonassaint J, Jackson TL, et al. Identification of genetic polymorphisms associated with risk for pulmonary hypertension in sickle cell disease. Blood. 2008;111:5721–6.
Zhang X, Zhang W, Ma SF, Desai AA, Saraf S, Miasniakova G, et al. Hypoxic response contributes to altered gene expression and precapillary pulmonary hypertension in patients with sickle cell disease. Circulation. 2014;129:1650–8.
Wong TE, Brandow AM, Lim W, Lottenberg R. Update on the use of hydroxyurea therapy in sickle cell disease. Blood. 2014;124:3850–7.
Patthamalai P, Fuchareon S, Chaneiam N, Ghalie RG, Chui DH, Boosalis MS, et al. A phase 2 trial of HQK-1001 in HbE-beta thalassemia demonstrates HbF induction and reduced anemia. Blood. 2014;123:1956–7.
Lavelle D, Vaitkus K, Ling Y, Ruiz MA, Mahfouz R, Ng KP, et al. Effects of tetrahydrouridine on pharmacokinetics and pharmacodynamics of oral decitabine. Blood. 2012;119:1240–7.
Meiler SE, Wade M, Kutlar F, Yerigenahally SD, Xue Y, Moutouh-de Parseval LA, et al. Pomalidomide augments fetal hemoglobin production without the myelosuppressive effects of hydroxyurea in transgenic sickle cell mice. Blood. 2011;118:1109–12.
Johnson J, Hunter R, McElveen R, Qian XH, Baliga BS, Pace BS. Fetal hemoglobin induction by the histone deacetylase inhibitor, scriptaid. Cell Mol Biol. 2005;51:229–38.
Hebbel RP, Vercellotti GM, Pace BS, Solovey AN, Kollander R, Abanonu CF, et al. The HDAC inhibitors trichostatin A and suberoylanilide hydroxamic acid exhibit multiple modalities of benefit for the vascular pathobiology of sickle transgenic mice. Blood. 2010;115:2483–90.
Campbell AD, Cui S, Shi L, Urbonya R, Mathias A, Bradley K, et al. Forced TR2/TR4 expression in sickle cell disease mice confers enhanced fetal hemoglobin synthesis and alleviated disease phenotypes. Proc Natl Acad Sci US A. 2011;108:18808–13.
Suzuki M, Yamamoto M, Engel JD. Fetal globin gene repressors as drug targets for molecular therapies to treat the beta-globinopathies. Mol Cell Biol. 2014;34:3560–9.
Acknowledgements
This work was supported in part by 5KL2 RR025770-04 (D.N.) and R01 HL068970, RC2 L101212, 5 T32 HL007501 (M.H.S.) from the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contribution
DAN and MHS wrote the manuscript. Both read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ngo, D.A., Steinberg, M.H. Genomic approaches to identifying targets for treating β hemoglobinopathies. BMC Med Genomics 8, 44 (2015). https://doi.org/10.1186/s12920-015-0120-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12920-015-0120-2