Abstract
Background
Home-based palliative care (HPC) is considered to moderate the problem of rising healthcare utilization of cancer patients at end-of-life. Reports however suggest a proportion of HPC patients continue to experience high care intensity. Little is known about differential trajectories of healthcare utilization in patients on HPC. Thus, we aimed to uncover the heterogeneity of healthcare utilization trajectories in HPC patients and identify predictors of each utilization pattern.
Methods
This is a cohort study of adult cancer patients referred by Singapore Health Services to HCA Hospice Service who died between 1st January 2018 and 31st March 2020. We used patient-level data to capture predisposing, enabling, and need factors for healthcare utilization. Group-based multi-trajectory modelling was applied to identify trajectories for healthcare utilization based on the composite outcome of emergency department (ED) visits, hospitalization, and outpatient visits.
Results
A total of 1572 cancer patients received HPC (median age, 71 years; interquartile range, 62–80 years; 51.1% female). We found three distinct trajectory groups: group 1 (31.9% of cohort) with persistently low frequencies of healthcare utilization, group 2 (44.1%) with persistently high frequencies, and group 3 (24.0%) that begin with moderate frequencies, which dropped over the next 9 months before increasing in the last 3 months. Predisposing (age, advance care plan completion, and care preferences), enabling (no medical subsidy, primary decision maker), and need factors (cancer type, comorbidity burden and performance status) were significantly associated with group membership. High symptom needs increased ED visits and hospitalizations in all three groups (ED visits, group 1–3: incidence rate ratio [IRR] 1.74–6.85; hospitalizations, group 1–3: IRR 1.69–6.60). High home visit intensity reduced outpatient visits in all three groups (group 1–3 IRR 0.54–0.84), while it contributed to reduction of ED visits (IRR 0.40; 95% CI 0.25–0.62) and hospitalizations (IRR 0.37; 95% CI 0.24–0.58) in group 2.
Conclusions
This study on HPC patients highlights three healthcare utilization trajectories with implications for targeted interventions. Future efforts could include improving advance care plan completion, supporting care preferences in the community, proactive interventions among symptomatic high-risk patients, and stratification of home visit intensity.
Similar content being viewed by others
Background
Healthcare utilization in patients with cancer escalates at the end of life. This is primarily driven by hospital visits that drive up healthcare-related costs [1,2,3,4,5,6]. Beyond economic repercussions, the experience of repeated hospital visits at EOL can result in care fragmentation and non-beneficial interventions [7,8,9]. There is compelling evidence that providing home-based palliative care (HPC) services can moderate the problem of rising healthcare utilization by reducing symptom burden, decreasing the number and length of hospital visits and increasing the chances of dying at home [10, 11]. Broadly, HPC services offer holistic care to patients at home or community-based care facilities through in-person visits up to several times a week, provision of supplies and equipment, and round-the-clock telephone support. Specific referral criteria may differ across services and countries, but referred patients are generally stable, with poor performance status and limited lifespan [12, 13]. Despite HPC support, research on HPC enrolees suggests that a proportion continues to have repeated ED visits and hospitalizations [14, 15]. To optimize HPC outcomes through reducing unnecessary hospital visits, it is imperative to first understand the heterogeneity in healthcare utilization among HPC patients and the reasons driving the differences.
Within literature, predictive factors for higher utilization among HPC patients included younger age [14,15,16], male gender [14, 15, 17], more comorbidities [14, 16], better function [17], and reduced hospice capacity [14, 15, 18]. Preference to die at home, having an involved decision-maker, and an advanced care plan (ACP) protect against hospitalizations [17, 19, 20]. These studies typically measured healthcare utilization as an aggregated single composite index over a cross-sectional period (e.g. ≥ 2 hospitalizations in the last month of life). Such approaches oversimplify the complex intra- and inter-individual variability of the real-life clinical context [8, 21]. To our knowledge, differential patterns of healthcare utilization over the HPC journey and the factors influencing the differences have not been elucidated.
Considering the limitations in literature, we adopted group-based multi-trajectory modelling (GBMTM) to uncover groups of HPC patients with different healthcare utilization over time. GBMTM is a specialized finite mixture modelling that allows groups of distinct trajectories to emerge from data as opposed to a conventional method that estimates patient-level averages [22, 23]. Moreover, GBMTM has an advantage of adding time-varying covariates to estimate whether events that occur during the course of a trajectory could alter the trajectory shape itself [24]. Identifying and characterizing groups of HPC patients with meaningfully different healthcare use patterns over time presents unique opportunities for targeted interventions designed to address their varying needs [25].
Therefore, this study aimed to uncover groups with distinct patterns of healthcare utilization, identify factors associated with group membership, and examine the influence of symptom burden and home visit frequency on healthcare utilization within each group.
Methods
Setting
The current study was conducted in Singapore where the EOL population segment (80% with cancer) contributes to approximately 50% of healthcare cost per capita of $60,000 (US$44,200) [26]. Ranked 12th in the 2015 Economist Intelligence Unit’s Quality of Death Index, Singapore’s palliative care services are conceptually and operationally similar to many first-world countries elsewhere [27]. Specifically, our HPC model offers patients with a life expectancy of less than 12 months to receive concurrent inter-disciplinary palliative care at home and disease-modifying therapies at tertiary hospitals [28, 29]. This model bears similarities to the Medicare Care Choices Model in the United States and some Hospice at Home services in England [13, 30, 31].
Our HPC services are run by voluntary welfare organizations, funded by government subsidies and philanthropic donations. Most offer care packages comprising home visits, equipment loans and round-the-clock support as core elements. Around 60% of Singapore’s HPC caseload is managed by HCA Hospice (HCA). HCA serves more than 3000 patients a year, of which 80% have cancer diagnoses. The free service includes an after-hours helpline for medical crisis. Enrolled patients are managed by multidisciplinary teams comprising of palliative care doctors, nurses, medical social workers, counsellors, and volunteers. Bereavement support is also provided in selected cases [32].
Study design and participants
This is a cohort study of cancer patients in HCA who died between 1st January 2018 and 31st March 2020. We included Singapore citizens or permanent residents referred to HCA by Singapore Health Services Regional Health System (SingHealth RHS). Out of the three healthcare clusters, SingHealth RHS is the largest in Singapore serving 70% of public sector cancer patients within inpatient and outpatient settings.
Electronic health records (EHR) from both HCA [32] and SingHealth [33] databases were extracted and linked using the patient’s unique National Registration Identity Card number. Linked datasets were de-identified before statistical analysis.
Outcome measures and covariates
Outcome sought a priori was healthcare utilization trajectories 1 year after HPC enrolment. We assumed stratification of trajectories to split along differential patterns of health service use. Emergency department (ED) visits, hospitalizations, and outpatient visits were chosen as the three healthcare utilization indicators of interest as they have been shown to rise substantially at EOL among cancer patients [34].
We identified covariates for testing association with outcomes by referencing Andersen’s model for health service use [35] (Additional file 1: Table S1). Andersen’s landmark model suggests health service use as a function of (1) predisposition to use services, (2) enabling or impeding factors, and (3) need for care. This model is widely used to investigate factors associated with healthcare utilization [36, 37].
Predisposing factors included age, gender, ethnicity, religion, marital status, residential status, and health beliefs. Andersen defines health beliefs as attitudes, values, and knowledge a patient has about health and health services [35]. For this, we included the patient’s awareness of diagnosis and prognosis, family’s awareness of diagnosis and prognosis, and ACP components. ACP components included the preferred place of care, preferred place of death and preferred plan of care (Additional file 1: Tables S1 and S2).
Enabling or impeding factors included socioeconomic (SES) surrogates of the Housing value Index (HI) and medical subsidy testing categories. HI utilizes housing type as a surrogate of past SES, where eligibility for public housing type is based on income ceilings [38,39,40] (Additional file 1: Table S3). Medical subsidy testing calculates government healthcare subsidies, taking into consideration current per capita household income [41]. Subsidies were categorized into 0% (highest SES), 1–25%, 25–50%, and 51–80% (lowest SES). Additional factors included social structure variables pertaining to primary caregiver, primary decision maker, and prevailing living arrangements.
Need-related factors included cancer type, comorbid burden, and Eastern Cooperative Oncology Group (ECOG) performance status. Cancer types were grouped by two-digit International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes [42]. Comorbidity burden was computed using Charlson Comorbidity Index (CCI) [43]. Additional factors included time-varying symptoms and psychosocial needs. HCA assesses the patient’s symptoms and/or psychosocial severity at every home visit. Details on symptoms and psychosocial assessment are in Additional file 1: Table S4a and S4b. We predefined high symptom needs by an assessment of “U1” and high psychosocial needs as an assessment of “P3” or “P4”. We measured home visit intensity using visit counts, with visits after-hours weighted twice as much, i.e. two points assigned. We predefined high intensity as ≥ 4 points over 2 weeks, as minimal standards are pegged at one home visit within 1 to 2 weeks.
STROBE guidelines were referenced in reporting this study [44].
Statistical analysis
First, we determined trajectories for the number of ED visits, hospitalizations, and outpatient visits separately using group-based trajectory modelling (GBTM), with extensions to account for non-random patient attrition due to death [22, 45]. GBTM uses maximum likelihood to identify latent subgroups of individuals with similar trajectories for a variable and has been used to describe healthcare trajectories in other populations [46,47,48]. Details of the trajectory analyses are in the additional file. Briefly, we used Poisson distribution to model each measure with time expressed in terms of weekly, bi-weekly, thrice-weekly, and monthly. For each time-unit analysis, we excluded patients who died within the first time-unit interval. The best-fit model for each time-unit was selected based on the Bayesian Information Criterion (BIC). To determine the optimum model for each measure, we compared cohort size and BIC between the best-fit model of the 4 time-units and identified the time-unit that provided a balance between information loss and goodness of model fit.
Second, we applied group-based multi-trajectory modelling (GBMTM) to identify distinct trajectories for healthcare utilization based on the composite outcome of ED, hospitalization, and outpatient visits [23]. GBMTM is a generalization of GBTM allowing multiple variables measuring an outcome to be jointly analysed. The optimum GBMTM model is again determined based on the BIC. We classified patients into one of the trajectory groups of the optimum GBMTM model based on maximum posterior probability assignment rule. We assessed model performance using these criteria: (1) close correspondence between the model’s estimated group size and the actual percentage of patients classified into each group, (2) high (>0.7) average posterior probabilities of group membership, (3) sufficient patients (>5% in proportion) classified in each group, and (4) narrow confidence band for each group [24].
Third, we identified predictors for trajectory group membership in the optimum GBMTM model using multinomial logit regression. We also assessed whether time-varying symptom burden, psychosocial needs and home visit intensity were associated with a within-group change in healthcare utilization trajectory. These associations were tested by expanding the Poisson regression model specification of each group-specific trajectory to include indicator variables measuring each patient’s presence of high symptom needs, high psychosocial needs, and high intensity of home visits at each time-unit of analysis. For these analyses, all statistically significant covariates on univariate analysis were considered for inclusion in the multivariable model. To avoid model overfitting and multi-collinearity, pairwise Spearman’s correlations (ρ) between covariates were generated and clinical judgement was used to decide which highly correlated covariates (ρ >0.65) to drop from the final multivariable model.
There was a low percentage of patients with missing data for the covariates. Patients with missing values for a covariate were retained in the multinomial logit regression analyses and analysed as a category for that covariate in these analyses. No imputation was performed. The total number of predictors tested was below the maximum number of predictors that could be fitted given the total sample size and number of patients in each trajectory group [49]. Analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC), with GBTM and GBMTM conducted using PROC TRAJ macros. All statistical tests were 2-sided with a 5% significance level.
Results
Group-based trajectory analysis of hospitalization, ED, and outpatient visits separately
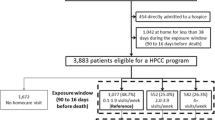
A total of 1931 patients were in the analysis cohort (Fig. 1). Of these patients, 1771, 1572, 1410, and 1257 were included based on weekly, bi-weekly, thrice-weekly, and monthly time-unit intervals, respectively (Additional file 1: Figs. S1–S3) The optimum model of each outcome was comprised of three groups with bi-weekly time-unit intervals.
Group-based multi-trajectory analysis of healthcare utilization as a composite measure
We included 1572 patients in the GBMTM analysis (Table 1). Figure 2 illustrates the optimum model for our composite measure. Group 1 (31.9% of patients) was characterized by low frequencies of ED visits, outpatient visits, and hospitalizations. Trajectory shape of ED visits and hospitalizations increased slightly over the first 9 months before decreasing in the last 3 months, while the outpatient visits saw a steady decline over the 12-month period. Group 2 (44.1%) was characterized by high frequencies of ED visits and hospitalizations, and moderate frequencies for outpatient visits, which remained constant over time. Group 3 (24.0%) was characterized by moderate frequencies of ED visits and hospitalizations and high frequencies of outpatient visits. The trajectory shape of each visitation type dipped over the first 9 months before increasing in the last 3 months.
The performance of the optimum model was good, with average posterior probabilities of patients classified in each group greater than 0.8 (Additional file 1: Table S5). Table 1 provides patient characteristics breakdown by trajectory group.
Factors associated with healthcare utilization trajectories
We used group 1 as the reference group in the multinomial logit model. Patients who were younger (relative risk ratio [RRR] 1.02; 95% CI 1.01–1.04 per year decrease), had higher CCI (RRR 1.16; 95% CI 1.10–1.21 per score increase), had no ACP (RRR 3.35; 95% CI 2.29–4.91), or had preferred care plans for a full treatment or limited interventions (RRR 2.32; 95% CI 1.45–3.69) were at increased risk of group 2 membership. Patients with breast (RRR 0.35; 95% CI 0.18–0.70) or urinary tract cancers (RRR 0.39; 95% CI 0.17–0.90) or received 1–50% medical subsidy (RRR 0.65; 95% CI 0.43–0.97) were less likely to be in group 2 (Table 2).
The following had increased risk of group 3 membership: being younger (RRR 1.05; 95% CI 1.04–1.06 per year decrease), higher CCI (RRR 1.03; 95% CI 1.01–1.06 per score increase), better ECOG (RRR 2.33; 95% CI 1.79–3.04), received 0% medical subsidy (RRR 1.57; 95% CI 1.08–2.28), had haematological malignancy (RRR 4.86; 95% CI 2.20–10.74), had non-blood relations or self as the primary decision maker (RRR 3.78; 95% CI 1.04–13.73), had no ACP (RRR 2.74; 95% CI 1.91–3.93), or had preferred care plans for a full treatment or limited interventions (RRR 2.08; 95% CI 1.31–3.30) (Table 2).
Association of time-varying needs and visit intensity on healthcare utilization trajectory within groups
Patients assessed with U1 symptoms had a significantly higher incidence of ED visits and hospitalizations in all three groups (ED visits, group 1–3: incidence rate ratio [IRR] 1.74–6.85; hospitalizations, group 1–3: IRR 1.69–6.60). High home visit intensity was significantly associated with a reduced incidence of outpatient visits in all three groups (group 1–3: IRR 0.54–0.84). In addition, high home visit intensity was significantly associated with decreased incidence of ED visits (IRR 0.40; 95% CI 0.25–0.62) and hospitalizations (IRR 0.37; 95% CI 0.24–0.58) in group 2 (Table 3).
Discussion
We found wide heterogeneity in healthcare utilization within a cohort of cancer patients enrolled in HPC. There appears a place for targeted interventions based on individual trajectories instead of a one-size fits all approach. We identified three distinct patient subgroups: group 1 with constantly low intensity of healthcare utilization; group 2 with persistently high healthcare utilization; and group 3 with early reductions in healthcare utilization that rose gradually over time. Broadly, several predisposing (age, ACP completion, and care preferences), enabling (no medical subsidy, primary decision maker), and need factors (cancer type, comorbidity burden and performance status) were significantly associated with group membership. Severe symptoms resulted in higher incidence rates of ED visits and hospitalizations across all three groups. Higher home visit intensity was associated with reduced outpatient visits across all groups, and reduced rates of ED visits and hospitalizations for group 2. Finer points pertaining to individual groups and their practice and policy implications are discussed next.
Within our cohort, only 53.6% of patients completed ACP, echoing findings from the Kaiser Permanente HomePal program in the USA where only 55% of patients had advance directive documentation. Like HCA, the HomePal program provides interdisciplinary HPC to patients with an estimated prognosis of 12 months or less and allows receipt of concurrent disease-directed therapy [50]. ACP is a process that supports patients in understanding their medical conditions and sharing their personal values, life goals and healthcare preferences with family and healthcare providers [51]. Without documented clarity on patient’s care preferences, it may be difficult for the HPC team to intervene and reduce unnecessary hospital visits [52, 53]. We postulate this as an underlying reason for patients without completed ACP having a higher risk of membership in group 2 or 3. Barriers to ACP may include patient factors (cognitive and emotional barriers), clinician factors (lack of training and prognostication challenges), and system factors (cumbersome documentation process) [54, 55]. More needs to be done to increase ACP completion within HPC services.
Patients with ACP preferences for “active” or “limited” interventions were also at higher risk of being in group 2 or 3 compared with those with ACP preferences for “comfort care only”. However, Singapore’s HPC services do not routinely provide medical interventions such as blood investigations, parenteral hydration or intravenous drug administration [56]. This is unlike some HPC services elsewhere which provide home-based clinical interventions [57, 58]. It is thus unsurprising that documented preferences for medical interventions predispose hospital visits when the need arises. If we desire to provide appropriate goal-concordant care without increasing the burden on hospital resources, a system change may be required. For example, the capacity to provide episodes of hospital-level care within the home could be explored for the treatment of reversible conditions [59]. Indeed, systematic reviews suggest that episodic Hospital-at-Home models were associated with lower costs per care episode without detriment to readmission and mortality rates for various disease groups [60, 61]. Data is however lacking for terminal cancer patients, highlighting areas for future research.
To reduce unplanned ED visits and hospitalizations, another approach would be to pre-emptively intervene for high-risk patients [62]. This may become increasingly possible as risk prediction models improve, following the rise of machine learning for big data analytics [25]. In this study, we found the presence of severe symptoms over 2 weeks to be a significant predictor for increased incidence of ED visits and hospitalizations across all three groups. Time-series symptom data could be explored using predictive modelling for risk-stratified early interventions to manage healthcare utilization.
Lastly, group 2 patients experienced frequent transitions between hospital and home despite having the shortest contact time with HPC before death. For this group, we observed encouraging signals that frequent home visits (≥4 visits per 2 weeks) lowered rates of all healthcare utilization. However, this association was not found for groups 1 and 3 with respect to ED visits and hospitalizations. A previous study demonstrated higher intensity of PC associated with reduced ED visits and hospitalizations in the last 30 days of life [63]. We expanded those early findings by showing the differential impact of HPC on healthcare utilization in three patient groups. Funding model per patient for HPC here is based on monthly block or package rates, similar to non-activity-based funding models in other countries [56, 64]. With the potential of HPC intensity to reduce hospital admissions in persistently high utilizers, considerations could be given to calibrate community funding models based on patient complexity and expected impact on hospital cost reduction.
Limitations
This study has several limitations. As a retrospective cohort study using readily available EHR data, inherent selection and information biases can occur, implicating the internal validity of results. Our study was conducted within Singapore, which may limit generalizability to HPC elsewhere. However, similarities do exist between Singapore’s HPC model and models of other developed countries, with multidisciplinary home visits, symptom assessment, psychosocial care, and round-the-clock support being common elements [13, 32]. Our sample only included patients referred by SingHealth to HCA, with an underlying assumption that patients previously cared for by SingHealth would continue to seek future care with the same provider. This may limit the generalizability of our findings. We did not capture drug prescription data and primary care utilization, which are additional components of healthcare utilization. Despite this, we believe that the omission of these data did not significantly skew study findings as we have included ED visits, hospitalizations, and outpatient visits that constitute three major components of healthcare costs [3, 4]. Our findings on healthcare utilization trajectories may not extrapolate to non-cancer patients, as compared to cancer counterparts, they may have higher rates of ED use but lower rates of hospitalisations and outpatient visits [65]. While aiming to study trajectories of healthcare utilization from HPC enrolment to death, we did not include patients discharged from HPC. Reasons for discharge included refusal of service, outliving prognosis, and discharge to inpatient hospice. Findings should be interpreted in that light. The optimum GBMTM model was derived based on bi-weekly time-unit intervals, resulting in the exclusion of patients who died within 14 days of HCA enrolment. Thus, our findings are not representative of imminently dying patients referred to HPC. Lastly, further work to externally validate our findings is required.
Conclusions
This study demonstrated the heterogeneity of healthcare utilization trajectories in HPC patients and identified factors associated with individual trajectories. Our findings suggest the applicability of targeted interventions such as increasing completion of ACP, supporting preferences for medical treatments at home, and proactive symptom interventions. Additionally, home visit intensity could be stratified to accommodate the needs of persistently high healthcare utilizers.
Availability of data and materials
The anonymized datasets used and/or analysed during the current study are available from the corresponding author on reasonable request
Abbreviations
- EOL:
-
End-of-life
- HPC:
-
Home-based palliative care
- HCA:
-
HCA Hospice
- ACP:
-
Advance care plan
- SingHealth RHS:
-
Singapore Health Services Regional Health System
- ED:
-
Emergency department
- GBTM:
-
Group-based trajectory modelling
- GBMTM:
-
Group-based multi-trajectory modelling
References
Luengo-Fernandez R, Leal J, Gray A, Sullivan R. Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol. 2013;14:1165–74.
Laudicella M, Walsh B, Burns E, Smith PC. Cost of care for cancer patients in England: evidence from population-based patient-level data. Br J Cancer. 2016;114:1286–92.
Goldsbury DE, Yap S, Weber MF, Veerman L, Rankin N, Banks E, et al. Health services costs for cancer care in Australia: Estimates from the 45 and Up Study. PLoS One. 2018;13:e0201552.
Mariotto AB, Enewold L, Zhao J, Zeruto CA, Yabroff KR. Medical Care Costs Associated with Cancer Survivorship in the United States. Cancer Epidemiol Biomark Prev. 2020;29:1304–12.
Park M, Song I. Medical care costs of cancer in the last year of life using national health insurance data in Korea. PLoS One. 2018;13:e0197891.
Leng A, Jing J, Nicholas S, Wang J. Geographical disparities in treatment and health care costs for end-of-life cancer patients in China: a retrospective study. BMC Cancer. 2019;19:39.
Committee on Approaching Death: Addressing Key End of Life Issues, Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Washington (DC): National Academies Press (US); 2015.
Aldridge MD, Bradley EH. Epidemiology And Patterns Of Care At The End Of Life: Rising Complexity, Shifts In Care Patterns And Sites Of Death. Health Aff. 2017;36:1175–83.
Teno JM, Gozalo P, Trivedi AN, Bunker J, Lima J, Ogarek J, et al. Site of Death, Place of Care, and Health Care Transitions Among US Medicare Beneficiaries, 2000-2015. JAMA. 2018;320:264–71.
Gomes B, Calanzani N, Curiale V, McCrone P, Higginson IJ. Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Cochrane Database Syst Rev. 2013;2013(6):CD007760.
Gonzalez-Jaramillo V, Fuhrer V, Gonzalez-Jaramillo N, Kopp-Heim D, Eychmüller S, Maessen M. Impact of home-based palliative care on health care costs and hospital use: A systematic review. Palliat Support Care. 2021;19:474–87.
Hui D, Bruera E. Models of Palliative Care Delivery for Patients With Cancer. J Clin Oncol. 2020;38:852–65.
Rees-Roberts M, Williams P, Hashem F, Brigden C, Greene K, Gage H, et al. Hospice at Home services in England: a national survey. BMJ Support Palliat Care. 2021;11:454–60.
Wang S-Y, Aldridge MD, Gross CP, Canavan M, Cherlin E, Johnson-Hurzeler R, et al. Transitions Between Healthcare Settings Among Hospice Enrollees at the End of Life. J Am Geriatr Soc. 2016;64:314–22.
Abraham S, Menec V. Transitions Between Care Settings at the End of Life Among Older Homecare Recipients. Gerontol Geriatr Med. 2016;2:2333721416684400.
Phongtankuel V, Johnson P, Reid MC, Adelman RD, Grinspan Z, Unruh MA, et al. Risk Factors for Hospitalization of Home Hospice Enrollees Development and Validation of a Predictive Tool. Am J Hosp Palliat Care. 2017;34:806–13.
Tay RY, Choo RWK, Ong WY, Hum AYM. Predictors of the final place of care of patients with advanced cancer receiving integrated home-based palliative care: a retrospective cohort study. BMC Palliative Care. 2021;20:164.
Sundararajan V, Bohensky MA, Moore G, Brand CA, Lethborg C, Gold M, et al. Mapping the patterns of care, the receipt of palliative care and the site of death for patients with malignant glioma. J Neuro-Oncol. 2014;116:119–26.
Salam-White L, Hirdes JP, Poss JW, Blums J. Predictors of emergency room visits or acute hospital admissions prior to death among hospice palliative care clients in Ontario: a retrospective cohort study. BMC Palliat Care. 2014;13:35.
Goldenheim A, Oates D, Parker V, Russell M, Winter M, Silliman RA. Rehospitalization of Older Adults Discharged to Home Hospice Care. J Palliat Med. 2014;17:841–4.
Nguefack HLN, Pagé MG, Katz J, Choinière M, Vanasse A, Dorais M, et al. <p>Trajectory Modelling Techniques Useful to Epidemiological Research: A Comparative Narrative Review of Approaches</p>. CLEP. 2020;12:1205–22.
Nagin DS. Group-Based Modeling of Development. Cambridge: Harvard University Press; 2005.
Nagin DS, Jones BL, Passos VL, Tremblay RE. Group-based multi-trajectory modeling. Stat Methods Med Res. 2018;27:2015–23.
Nagin D, Odgers C. Group-Based Trajectory Modeling in Clinical Research. Annu Rev Clin Psychol. 2010;6:109–38.
Bates DW, Saria S, Ohno-Machado L, Shah A, Escobar G. Big data in health care: using analytics to identify and manage high-risk and high-cost patients. Health Aff (Millwood). 2014;33:1123–31.
Yan S, Kwan YH, Thumboo J, Low LL. Characteristics and Health Care Utilization of Different Segments of a Multiethnic Asian Population in Singapore. JAMA Netw Open. 2019;2:e1910878.
The Economist Intelligence Unit. The 2015 Quality of Death Index Ranking palliative care across the world. 2015.
Luckett T, Phillips J, Agar M, Virdun C, Green A, Davidson PM. Elements of effective palliative care models: a rapid review. BMC Health Serv Res. 2014;14:136.
Palliative Care Services – Singapore Hospice Council. https://singaporehospice.org.sg/services/. Accessed 25 Jan 2022.
Parikh RB, Wright AA. The Affordable Care Act and End-of-Life Care for Patients with Cancer. Cancer J. 2017;23:190–3.
U S Centers for Medicare & Medicaid Services. Medicare Care Choices Model Enables Concurrent Palliative and Curative Care. J Pain Palliat Care Pharmacother. 2015;29:401–3.
Ho BJ, Akhileswaran R, Pang GSY, Koh GCH. An 11-Year Study of Home Hospice Service Trends in Singapore from 2000 to 2010. J Palliat Med. 2017;20:461–72.
Electronic Health Intelligence System. https://www.ihis.com.sg/Project_Showcase/Healthcare_Systems/Pages/eHINTS.aspx. Accessed 12 Jul 2020.
Langton JM, Blanch B, Drew AK, Haas M, Ingham JM, Pearson S-A. Retrospective studies of end-of-life resource utilization and costs in cancer care using health administrative data: a systematic review. Palliat Med. 2014;28:1167–96.
Andersen RM. Revisiting the Behavioral Model and Access to Medical Care: Does it Matter? J Health Soc Behav. 1995;36:1–10.
Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen’s Behavioral Model of Health Services Use: a systematic review of studies from 1998–2011. Psychosoc Med. 2012;9:Doc11.
Hajek A, Kretzler B, König H-H. Determinants of Healthcare Use Based on the Andersen Model: A Systematic Review of Longitudinal Studies. Healthcare (Basel). 2021;9:1354.
Zhuang Q, Lau ZY, Ong WS, Yang GM, Tan KB, Ong MEH, et al. Sociodemographic and clinical factors for non-hospital deaths among cancer patients: A nationwide population-based cohort study. PLoS One. 2020;15:e0232219.
Wong FY, Wong RX, Zhou S, Ong WS, Pek PP, Yap Y-S, et al. Effects of housing value and medical subsidy on treatment and outcomes of breast cancer patients in Singapore: A retrospective cohort study. Lancet Reg Health West Pac. 2021;6:100065.
Wong TH, Skanthakumar T, Nadkarni N, Nguyen HV, Iyer NG. Survival of patients with head and neck squamous cell carcinoma by housing subsidy in a tiered public housing system. Cancer. 2017;123:1998–2005.
Introduction fo Means-Testing. https://www.aic.sg/resources/means-testing. Accessed 9 Jan 2022.
Topography Codes from ICD-O-2 and ICD-O-3 | SEER Training. https://training.seer.cancer.gov/arc_neoplasms/codes.html. Accessed 24 Jun 2019.
NCI Comorbidity Index Overview. https://healthcaredelivery.cancer.gov/seermedicare/considerations/comorbidity.html. Accessed 27 Jan 2022.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–8.
Haviland AM, Jones BL, Nagin DS. Group-based Trajectory Modeling Extended to Account for Nonrandom Participant Attrition. Sociol Methods Res. 2011;40:367–90.
Chien T-Y, Lee M-L, Wu W-L, Ting H-W. Exploration of Medical Trajectories of Stroke Patients Based on Group-Based Trajectory Modeling. Int J Environ Res Public Health. 2019;16:E3472.
Lauffenburger JC, Mahesri M, Choudhry NK. Use of Data-Driven Methods to Predict Long-term Patterns of Health Care Spending for Medicare Patients. JAMA Netw Open. 2020;3:e2020291.
Tyagi S, Koh GC-H, Nan L, Tan KB, Hoenig H, Matchar DB, et al. Healthcare utilization and cost trajectories post-stroke: role of caregiver and stroke factors. BMC Health Serv Res. 2018;18:881.
Harrell F. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis. New York: Springer-Verlag; 2001.
Wang SE, Liu I-LA, Lee JS, Khang P, Rosen R, Reinke LF, et al. End-of-Life Care in Patients Exposed to Home-Based Palliative Care vs Hospice Only. J Am Geriatr Soc. 2019;67:1226–33.
Sudore RL, Lum HD, You JJ, Hanson LC, Meier DE, Pantilat SZ, et al. Defining Advance Care Planning for Adults: A Consensus Definition From a Multidisciplinary Delphi Panel. J Pain Symptom Manag. 2017;53:821–832.e1.
Brinkman-Stoppelenburg A, Rietjens JAC, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med. 2014;28:1000–25.
Dixon J, Matosevic T, Knapp M. The economic evidence for advance care planning: Systematic review of evidence. Palliat Med. 2015;29:869–84.
Cheung JTK, Au D, Ip AHF, Chan J, Ng K, Cheung L, et al. Barriers to advance care planning: a qualitative study of seriously ill Chinese patients and their families. BMC Palliative Care. 2020;19:80.
Menon S, Kars MC, Malhotra C, Campbell AV, van Delden JJM. Advance Care Planning in a Multicultural Family Centric Community: A Qualitative Study of Health Care Professionals’, Patients’, and Caregivers’ Perspectives. J Pain Symptom Manag. 2018;56:213–221.e4.
2021 SHC FAQs on Palliative Care – SHC e-Library. https://library.singaporehospice.org.sg/faqs-on-palliative-care/2021-shc-faqs-on-palliative-care-2/. Accessed 4 Feb 2022.
Johnston B, Patterson A, Bird L, Wilson E, Almack K, Mathews G, et al. Impact of the Macmillan specialist Care at Home service: a mixed methods evaluation across six sites. BMC Palliat Care. 2018;17:36.
Home-Based Palliative Care | Serious Illness | Get Palliaitve Care. https://getpalliativecare.org/how-home-based-palliative-care-can-help-you-or-a-loved-one/. Accessed 27 Jun 2022.
Evans WG, Cutson TM, Steinhauser KE, Tulsky JA. Is there no place like home? Caregivers recall reasons for and experience upon transfer from home hospice to inpatient facilities. J Palliat Med. 2006;9:100–10.
Leong MQ, Lim CW, Lai YF. Comparison of Hospital-at-Home models: a systematic review of reviews. BMJ Open. 2021;11:e043285.
Shepperd S, Iliffe S, Doll HA, Clarke MJ, Kalra L, Wilson AD, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9:CD007491.
Wallace E, Stuart E, Vaughan N, Bennett K, Fahey T, Smith SM. Risk Prediction Models to Predict Emergency Hospital Admission in Community-dwelling Adults: A Systematic Review. Med Care. 2014;52:751–65.
Pellizzari M, Hui D, Pinato E, Lisiero M, Serpentini S, Gubian L, et al. Impact of intensity and timing of integrated home palliative cancer care on end-of-life hospitalization in Northern Italy. Support Care Cancer. 2017;25:1201–7.
Groeneveld EI, Cassel JB, Bausewein C, Csikós Á, Krajnik M, Ryan K, et al. Funding models in palliative care: Lessons from international experience. Palliat Med. 2017;31:296–305.
Langton JM, Reeve R, Srasuebkul P, Haas M, Viney R, Currow D, et al. Health service use and costs in the last 6 months of life in elderly decedents with a history of cancer: a comprehensive analysis from a health payer perspective. Br J Cancer. 2016;114:1293–302.
Acknowledgements
Not applicable
Funding
This work was supported by the SingHealth Duke-NUS Academic Medicine Research Grant FY2020: Special Category (HSR-HEARTS) [Grant Number: AM/HRT003/2020]. The funders had no role in the study design, collection, analysis, interpretation, and manuscript writing.
Author information
Authors and Affiliations
Contributions
QZ, PC, SY, and GMY conceptualized and designed the study. QZ, WSO, ZZY, and CQZF acquired and analysed the data. QZ, PC, GMY, SYY, GL, and ZZY were involved in the interpretation of the data. QZ, PC, WSO, and SY drafted the work. All authors read and approved the final manuscript.
Authors’ information
QZ is a palliative care consultant with a keen interest in health services research using electronic health record data. He holds relevant portfolios as the lead of institutional and national palliative care registries.
PC is HCA Hospice’s medical director and Vice Chairman of the Singapore Hospice Council. He has been heavily involved in home-based palliative care services from 2008 to current.
SY is an assistant professor at the Programme in Health Services and Systems Research in Duke-NUS. She is a public health researcher and behavioural scientist. Her main research interest lies in understanding individual and population health behaviour which may have public health significance.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by SingHealth Central Institutional Review Board (CIRB Ref No: 2020/2448). Waiver of requirement for informed consent was granted for research involving de-identified data.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table 1.
Candidate list of variables based on the Andersen’s framework for health service use. Table 2. Preferred plan of care categories and definitions. Table 3. Comparison of size, income ceiling for eligibility to purchase average price after subsidy of public housing and derived categories of Housing value Index (HI). Table 4a. Patient symptom categories. Table 4b. Patient psychosocial categories and definitions. Table 5. Performance of the optimum model for the trajectories of the composite healthcare utilization measure. Figure 1. Trajectories of emergency department (ED) visits using group-based trajectory modelling. Best-fit model based on (A) monthly time-unit, (B) thrice-weekly time-unit, (C) bi-weekly time-unit and (D) weekly time-unit, and (E) the optimum model is the model with bi-weekly time-unit based on trade-off comparison between cohort size and Bayesian Information Criterion (BIC). Figure 2. Trajectories of outpatient visits using group-based trajectory modelling. Best-fit model based on (A) monthly time-unit, (B) thrice-weekly time-unit, (C) bi-weekly time-unit and (D) weekly time-unit, and (E) the optimum model is the model with bi-weekly time-unit based on trade-off comparison between cohort size and Bayesian Information Criterion (BIC). Figure 3. Trajectories of hospitalizations using group-based trajectory modelling. Best-fit model based on (A) monthly time-unit, (B) thrice-weekly time-unit, (C) bi-weekly time-unit and (D) weekly time-unit, and (E) the optimum model is the model with bi-weekly time-unit based on trade-off comparison between cohort size and Bayesian Information Criterion (BIC). Supplementary Information on Group-based trajectory modelling (GBTM) and Group-based multi-trajectory modelling (GBMTM) Analyses.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhuang, Q., Chong, PH., Ong, W.S. et al. Longitudinal patterns and predictors of healthcare utilization among cancer patients on home-based palliative care in Singapore: a group-based multi-trajectory analysis. BMC Med 20, 313 (2022). https://doi.org/10.1186/s12916-022-02513-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-022-02513-y