Abstract
Background
The COVID-19 pandemic led to new and unfamiliar changes in healthcare services globally. Most COVID-19 patients were cared for in primary healthcare services, demanding major adjustments and adaptations in care delivery. Research addressing how rural primary healthcare services coped during the COVID-19 pandemic, and the possible learning potential originating from the pandemic is limited. The aim of this study was to assess how primary healthcare personnel (PHCP) working in rural areas experienced the work situation during the COVID-19 outbreak, and how adaptations to changes induced by the pandemic were handled in nursing homes and home care services.
Method
This study was conducted as an explorative qualitative study. Four municipalities with affiliated nursing homes and homecare services were included in the study. We conducted focus group interviews with primary healthcare personnel working in rural nursing homes and homecare services in western Norway. The included PHCP were 16 nurses, 7 assistant nurses and 2 assistants. Interviews were audio recorded, transcribed and analyzed using thematic analysis.
Results
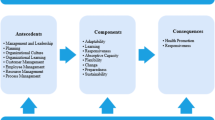
The analysis resulted in three main themes and 16 subthemes describing PHCP experience of the work situation during the COVID-19 pandemic, and how they adapted to the changes and challenges induced by the pandemic. The main themes were: “PHCP demonstrated high adaptive capacity while being put to the test”, “Adapting to organizational measures, with varying degree of success” and “Safeguarding the patient’s safety and quality of care, but at certain costs”.
Conclusion
This study demonstrated PHCPs major adaptive capacity in response to the challenges and changes induced by the covid-19 pandemic, while working under varying organizational conditions. Many adaptations where long-term solutions improving healthcare delivery, others where short-term solutions forced by inadequate management, governance, or a lack of leadership. Overall, the findings demonstrated the need for all parts of the system to engage in building resilient healthcare services. More research investigating this learning potential, particularly in primary healthcare services, is needed.
Similar content being viewed by others
Background
Immediately after the World Health Organization (WHO) announced that the Coronavirus disease (COVID-19) was a pandemic on March 12, 2020, healthcare services globally faced new and unfamiliar challenges [1, 2]. In addition to a major increase in patients needing acute care in the specialist healthcare services [3], primary healthcare services were forced to alter infection control and to prepare for infection outbreaks in nursing homes and among patients receiving home care services [4, 5].
Although the primary healthcare services are considered to represent the backbone of the healthcare service globally in almost all nations, it has often been “the poor stepchild” in terms of allocation of resources, competence, availability, and attention [6,7,8]. This was also seen in the beginning of the pandemic, as both infection control measures and distribution of personal protective equipment (PPE) were mainly focused on hospitals’ needs [7, 9]. However, only a small proportion of COVID-19 patients were hospitalized. Primary healthcare services managed the bulk of these patients, in addition to their important role in caring for, and protecting elderly and chronically ill patients from infection [8, 10]. Primary healthcare personnel had to make major adjustments to handle the ongoing pandemic, often despite deficient guidelines [5] and inadequate personnel [11].
Health personnel’s ability to adjust and adapt their work to expected or unexpected changes and maintain adequate performance is main pillars of resilience in healthcare (RiH) [12]. Taking a resilience perspective, health personnel need to make continuous adaptations to everyday changes or variations in the healthcare system [13]. While COVID represented an extreme example, these adaptations are critical. In this instance it included management of both performance variability, and management of complexity in terms of unexpected situations and variability in demands. This ability is, according to RiH, crucial to ensure adequate performance.
Although there is a growing body of research on how the primary healthcare services coped during COVID-19 [14,15,16,17,18,19], many issues remain unaddressed. Research has, for example, mostly focused on healthcare services situated in urban areas, leaving rural primary healthcare services under-investigated. There is also a specific need for evaluation in the Norwegian context, and for research aiming to learn from the COVID-19 pandemic [20].
Aim and research question
In this study, we aimed to assess how primary care health personnel (PHCP) working in rural areas experienced the work situation during the COVID-19 outbreak. More specifically, the study aimed to explore how adaptations to changes induced by the COVID-19 pandemic were handled in nursing homes and home care services from the perspectives of PHCP. The study was guided by the following research question: How did health personnel in rural primary care contextual settings experience the work situations during the COVID-19 outbreak and how did they adapt to the rapid onset changes induced by the COVID-19 outbreak?
Methods
Design
This study was an explorative qualitative study. The qualitative design allowed for exploration of how changes induced by the COVID-19 pandemic were handled in the rural Norwegian primary healthcare services by obtaining an understanding of the meaning health personnel ascribed to the situation they found themselves in during the pandemic [21, 22].
Setting
In Norway, municipalities are responsible for providing primary care to its inhabitants (e.g., nursing homes, homecare, care homes). A Norwegian municipality is a geographic delimited area that constitutes a separate political and administrative unit. Norway is divided into 356 municipalities with population rates ranging from 188 to 699,827 inhabitants [23]. The three smallest municipality types (which were the focus of this study) are characterized as small-town municipalities, small center municipalities and least central municipalities. They have an average population span from 1940 to 9601 inhabitants (Table 1.). The Norwegian municipalities are not fully autonomous but exercise autonomy within limits set by the parliament, this includes the operation of primary healthcare services. The municipalities and their affiliated primary healthcare services are organized and run differently, due to demographic, social and geographic conditions, which also causes differences in operating costs [24]. However, all municipalities are obligated to provide certain services (e.g., primary healthcare services) within a minimum standard [24].
Recruitment
Small town, - small center, - and less central municipalities (Table 1) across the Norwegian west coast were invited to participate in the study. Health- and care managers of 11 municipalities were contacted via e-mail and invited to participate in the study. Four of these agreed to participate in the study and provided contact information to managers of nursing homes and homecare services within their municipality. The nursing home and homecare services managers were contacted by MKG and recruited to participate in the study. The same managers organized recruitment of health personnel within their services through distributing information letters and invitation to participate to their employees. The leaders also organized interview time and place in cooperation with MKG.
Participants
Four municipalities and their nursing homes and homecare services were included in the study (Table 2). Half of the included municipalities had combined nursing homes and homecare services (the same health personnel covered both roles) due to their small size. The other half had one or several nursing homes and one homecare services covering the whole municipality.
The included PHCP were 16 nurses, 7 assistant nurses and 2 assistants with differing experience and (continued) education, all of whom worked during the COVID-19 pandemic (Table 2).
Data collection
Data collection was conducted from September 2021 to November 2022. All interviews were conducted face to face with necessary infection precautions and measures. PHCP were interviewed in focus groups of 3–6 participants using a semi-structured interview guide based on previous research on health personnel and COVID-19 and RiH theory. The interviews were conducted by two researchers (MKG: moderator and TK: note taker). Both researchers had healthcare background in primary and secondary healthcare, and experience with qualitative interviewing (focus groups and individual interviewing). The interviews lasted for approximately 60 min, were audio recorded and transcribed verbatim.
Data analysis
The data were analyzed using Braun and Clarkes thematic analysis [25], and was conducted by MKG. The transcribed data were read actively, and in several rounds to search for meanings or patterns. Text with meaning where then moved into a Word table and labeled with initial codes. When all text had been coded, 85 individual codes remained. The codes were read through carefully, and some were merged, separated into new codes or removed due to lack of relevance to the research question [25]. This resulted in 71 codes. In the next step, codes were analyzed to identify potential overreaching themes or subthemes. A new Word table was developed to help sort and find relationships between the different codes. When initial themes and subthemes were identified, a review was conducted to see if any themes needed to be “combined, refined and separated or discarded” [25]. (Table 3). Themes and subthemes were reviewed and approved by the author team.
Results
Three main themes describing how health personnel in primary healthcare experience the work situations during the COVID-19 outbreak and how they adapted to the rapid onset changes induced by the pandemic, were identified in the focus group interviews.
The findings showed that despite the uncertainty and unfamiliar challenges characterizing the COVID-19 pandemic, PHCP saw it as their duty to do what was needed of them, to keep the healthcare service running, including safeguarding healthcare quality and patient safety. The main challenges they encountered were reduced staffing, increased work tasks, facilities not built for infection control and an information overload. PHCP oversaw these challenges by, working extra hours, taking on extra work tasks, engaging in new roles, rearranging wards to ease infection control, developing tools to ease patients care, and find novel solutions to handle infection control in the facilities they had available.
PHCP demonstrated high adaptive capacity whilst being put to the test
At the beginning of the pandemic, PHCP described being terrified of the new and unknown virus. They described how they distanced themselves from their spouses, children, and grandchildren, and worried about infecting their families or getting infected by their families, bringing COVID-19 into their workplaces. One nurse said that she feared she would inflict an illness on someone from which they could potentially die. Despite this fear, the PHCP embraced their responsibilities and went to work:
I remember thinking that I had to go to work… many people could stay safe at home, but we couldn’t, we had to go to work. And I remember thinking, it is what it is, I must go to work, if I get it [COVID-19], if I die, then I’ll just have to be grateful for the life I’ve had so far….
(Nursing home, Municipality A)
As the world became more familiar with the virus and PPE, effective infection control routines and the vaccine came into place, health personnel described mainly feeling safe at work during the COVID-19 pandemic, although they felt more vulnerable to infection than others.
Although PPE was the main infection control measure providing security to the PHCPs, it was described as challenging to work with. They encountered problems like unbearable heat, foggy visors, and constant sweating. Despite wearing PPE, several of the PHCPs got infected with COVID-19 while at work. In one nursing home, almost every employee got infected, and experienced symptoms. Some of them were still struggling with the after-effects.
Due to the high infection rates and/or high amounts of quarantined PHCPs, the workload was, in several of the facilities, reported to be high. Some were forced to work 11-hour shifts and take on extra nigh-shifts with limited rest between them. They were required to take on extra workload to make up for the lack of personnel. Some were even called back from vacations or had planned vacations postponed. That said, some PHCP reported having almost no changes in their work schedules, demonstrating great variation between the included primary healthcare services.
Although fear, work schedules and PPE took a toll on the PHCPs, many also experienced positives from going through these challenges. Not only did they report that the pandemic had been a great learning experience (e.g., in infection control measures, PPE use, and managing critically ill patients) they also experienced an increased trust in their professional assessment by, for example attending physicians. Moreover, in addition to receiving support from the local community, many PHCPs reported that they experienced a good working environment where people supported, cared for, and helped each other as best they could:
I have to say that we became wielded together handling something like this… we tried to make each other good, helped each other with things, helped each other getting dressed… it was really nice to see how we could be a team, and have fun together although going through something this tough.
(Nursing home, Municipality C)
There were, however, also reports of loneliness, where the lack of joint lunch breaks, personnel meetings and generally being separated from colleagues – particularly in the homecare service, left PHCPs feeling alone. They missed being able to discuss things and solve professional problems with colleagues, and most of all they missed social interactions. There were also reports of PHCPs who had a hard time dealing with the high work pressure and made the decision to leave their positions during the COVID-19 period.
That said, PHCPs in all included primary healthcare services demonstrated how they adapted to the long-and short-term challenges they encountered in everyday work, despite the unpredictability (e.g., changing guidelines and routines) characterizing their workdays. They became creative in terms of findings ways to rearrange the wards to ease infection control, they designed their own tools (e.g., a patient record sheet for quick overview of patients) and became creative in how to make caring for infected patients easier and safer (e.g., use lockable cash boxes to able to keep the patients’ medications in their rooms). Homecare nurses changed their PPE in raw cellars, garages and on patients’ stairs and the nursing homes that did not experience any infected patients had provisional infection rooms and equipment ready, in case of infection outbreaks.
Despite the numerous pandemic related guidelines and rules PHCP had to deal with, they adapted guidelines to their professional discretion in many situations, particularly in situations where they cared for dying patients. They did for example make sure that patients had their family around them during their last hours (with necessary precautions and infection measures) despite visit restrictions, which did not occur in some other countries.
Moreover, PHCPs became much more accustomed to using electronic tools. Homecare nurses talked about an increase in use of medication dispensers for the patients’ homes. iPads and tablets were used for communication, both between patients and their families, and for having doctors’ visits and PHCP meetings. Most of the nursing homes had access to iPads or tablets before the pandemic but it pushed them to start to use them.
PHCPs from several of the included sites described that they stood up for the tasks ahead of them, and that they worked extra hours when needed. Terms like “going the extra mile”, “rolling up their sleeves” and “not backing out” were used.
Adapting to organizational measures, with varying degree of success
Most PHCPs described that their task scope had increased. New tasks included disinfecting, arranging patient visits (with pre and post disinfections, registration, and assessment of risk of infection), care for extra patients, taking phone calls from worried next of kin and “guarding” patient rooms when patients suffering from dementia did not understand the isolation rules. In many of the primary healthcare services these extra work tasks were laid upon them without adding extra personnel. This felt chaotic and demanding for some.
It was quite early in the evening [the start of a night shift], and you had to be involved in the evening care of the patients [getting them ready for bed, a task dedicated for the evening shift]. And you might have to care for all the patients in the ward, because they [the evening shift], hadn’t had the time to do it. And then you work all night, without a break, because there’s not enough staff to take a break.
(Nursing home, Municipality A)
In the attempt to relieve work pressures, some adapted by dropping the least necessary tasks. For example, in homecare services they reduced supervision of patients that could do without it and tried to involve next of kin more in these tasks. Later, however, these measures were found to lead to a deterioration of some of the affected patients’ health.
A range of organizational adaptations to prevent spread of infection was described. Some primary healthcare services separated PHCPs into fixed groups and tried to keep these groups separated, although it was challenging to do so. They introduced pre-made meals for the patients, longer shifts (11 h), separated the break rooms, and gave courses in PPE use and infection control. Although primary healthcare services found that some of these measures worked, not all were appreciated or understood. Particularly in the beginning of the pandemic, measures were perceived to be unclear and confusing, such as when to use facemasks and which types were required. As the rules were unclear, some wore facemasks when caring for patients while others did not. There was also a limited access to PPE in the beginning of the pandemic and primary healthcare services’ conserved the PPE they had available to prepare for a potential COVID-19 outbreak. Moreover, there were reports of inadequate communication between cooperating healthcare services (e.g., home care service and ambulance personnel) in terms of infection risk among patients. In one case, ambulance personnel had been informed about a patient being an infection risk and showed up in full PPE when picking up the patient. The home care health personnel, however, had not been informed about this risk, and provided care to the patient without PPE. This caused insecurity, fear of contagion and a feeling of being undervalued.
Another reported problem was that there were different rules within different primary healthcare services, even within the same municipality. Moreover, there were differences in how distribution of information was managed in the different healthcare services. Although everyone agreed that there was a lot of information to comprehend, some participants were happy with the amount of information-, and how they got their information (often via e-mail or an information binder kept in the office) and managed to adapt accordingly. Others experienced an information overload which was difficult to oversee and struggled with interpreting the information as well as keeping track of the latest news.
There was also varying access to leaders during the pandemic period. Many described that they had leaders supporting their needs as best they could, who kept track of the information flow, and secured enough personnel. Others described that they had limited access to a leader.
We lost a leader in this period… so we were… my ward was without a leader. We felt that everything was… complete chaos… Things were hanging midair… (Municipality A).
Safeguarding the patient’s safety and quality of care, but at certain costs
Overall, PHCPs in all included primary healthcare services perceived that the patient safety and quality of care was safeguarded during the COVID-19 pandemic. The aspect of safety and quality was said to be one of their highest priorities when adapting to challenges and changes induced by the pandemic.
The one main thing PHCPs believed to threaten quality of care, was the lack of psychosocial care the patients received. As a measure to avoid infection outbreaks in nursing homes, there were prolonged periods with firm visiting restrictions. This was perceived to severely affect patients’ quality of life. In addition, the PPE created a distance between the patient and the PHCP, limiting the interpersonal aspect of the care. Some nursing homes had the capacity to introduce measures to care for psychosocial aspects (and even employed personnel for this purpose), while others struggled to simply get their basic PHCP tasks done. In facilities where they had the resources to do so, PHCP took over the roles of next of kin and volunteers, coming up with creative measures to care for the patients’ psychosocial needs (e.g., arranging tea-parties, bingo, sing-alongs, making and showing videos from the patients’ families, work-out sessions and arranging “window visits”).
Discussion
We evaluated the response of PCHPs to the COVID-19 pandemic in rural areas and found that it demanded an extreme level of adaption at a rapid clip. Moreover, we found that PHCPs had to make these adaptations under varying organizational conditions, and that the primary healthcare service often did not adapt as fast as PHCPs, for example, in terms of provision of rules and guidelines. The working environment, leadership, and health system organization profoundly affected PHCPs’ experience of working during the COVID-19 pandemic.
Previous research conducted on COVID-19 and primary healthcare services, supports our findings concerning the different challenges encountered by PHCPs—such as insecurity, the urge to self-isolate, staffing issues, changing guidelines, PPE shortage and information overload [11, 14, 26,27,28]. Staffing issues have been reported as a particular problem in smaller, more rural municipalities [29]. Although few studies in this context uses RiH theory as backdrop [2], several studies demonstrated PHCPs adaptive behavior in response to challenges and changes induced by the pandemic (e.g., increased use of electronic tools, workarounds, engaging in new responsibilities and roles) [27, 28, 30, 31]. Aspects identified in this study, which has been less illuminated in previous research included the role of professional discretion in the face of multitudes of new guidelines, challenges concerning varying guidelines in neighboring municipalities and healthcare services, and the challenging communication between collaborating healthcare services [32, 33] .
How organizations affect PHCP adaptive capacity
Professional discretion is intricately linked to healthcare personnels adaptive capacity, which is one of the main pillars of RiH [12]. The span between professional discretion, adaptations and established rules and regulations, and how the different aspects are, or should be weighted in a resilient healthcare services remains underinvestigated [34]. RiH theory, usually describes resilient healthcare services as having the ability to adapt, improvise and being flexible - aspects highlighting the value of a decentralized authority allowing professional judgement and professional discretion, particularly when encountering high levels of variability, uncertainty and change [34]. This description of a resilient healthcare services nearly undermines rules and regulations, or at least, indicates a difficulty in reconciling them [34].
Although healthcare personnel are familiar with delivering healthcare in a context of constant social and political change [35], during the pandemic, the pace of healthcare delivery change was dramatic with major changes occurring often, along with rapid changes in rules and procedures. In many cases new regulations did not keep pace with the development of the pandemic, leaving a great responsibility on healthcare personnel and their professional discretion. In the current study, unclear regulation created frustration and insecurity among PHCPs, which in turn limited their adaptive capacity. This insecurity was particularly seen in the primary healthcare services which did not have a resolute leader. Later in the pandemic, however, when rules and guidelines became clearer, PHCP became more secure in making decisions based on professional discretion, and adapting guidelines to their professional assessment, for example “bending” the visiting rules for patients on their death beds.
On the other hand, previous studies have argued that too many rules and regulations and high external control restrain healthcare personnels’ adaptive capacity [36, 37]. According to Grote [38] there is a need to balance flexibility and stability to support RiH. The leaders play a key role in this context. On one side, healthcare personnel need the stability and security associated with established routines and rules, on the other side, they need their flexibility to adapt to the context they are working in, and to apply their professional discretion when providing healthcare to patients. In other words, a RiH promoting leadership needs to foster both cohesiveness and independence, thereby representing the dual, and often opposing challenge, of balancing flexibility and stability [38,39,40]. Moreover, leaders need to provide guidelines, structures and mechanisms that support resilience [34]. Providing such mechanisms and structures are, however, closely related to governance, particularly during crises [41, 42].
Governance “enables the financing, resource generation and service delivery functions to operate as intended and in coordination with the rest of the system to achieve maximum overall system performance, and by extension, resilience” [42]. Inadequate governance function results in confusing information flow, unclear guidelines, lack of equipment and staff, and lack of coordination between healthcare services [42]. This is supported by this and other studies [43, 44]. In the current study, there were examples of both well-functioning and less well-functioning governance. This variation was evident both across and within municipalities, however, the background for the variation remains unclear. One explanation may be related to the stringent division between municipal governance in Norway, where each municipality have the autonomy to organize and run their healthcare services at their own discretion, additionally, with different economic starting points. This will naturally lead to differences in healthcare organization in general, and COVID-19 management specifically, particularly if the cooperation and communication between the municipalities are limited. A recent literature review on resilience in healthcare during COVID-19 [2], found that the pandemic led to better and increased collaboration among healthcare services, and was found to be a contributing factor in maintaining resilient healthcare services, a finding supported by other literature [42, 45]. A report on the COVID-19 pandemic in Norwegian municipalities, however, found that intermunicipal collaboration was difficult due to differences in location (e.g., rural versus urban locations) and needs [43]. This indicates a need for more research investigating how the structure of primary healthcare services influence resilience in healthcare.
Rural healthcare services often face more challenges than urban areas (e.g., economic limitations, an elderly population, access to competence and large distances) [46, 47]. This can in turn limit their resilience in the face of healthcare crises, for example, in terms of a lacking supply chain, limited staffing during regular operation and the need to depend on more rural healthcare services for patients with critical conditions [48]. Although many of the aforementioned challenges were stated in the current study, there are large differences in how overreaching these challenges are in different municipalities, often regardless of size and rurality [47]. Overall, there are large variation in rural healthcare services both nationally and internationally, their sizes, location, their inhabitants, and their economy. This indicate inequality in terms of preconditions to handle crises, and may also be an explanation of the differences in COVID-19 management in Norwegian primary healthcare services [43]. Either way, it signifies the importance of a context disclosure when planning RiH enhancing work in primary healthcare services [49,50,51].
Maintaining adaptive capacity over time
Despite both governance and leadership, healthcare personnel often adapt to their working conditions to provide quality care and safeguard patient safety, if they are provided with the flexibility to do so [14, 52]. This is reflected in this study through descriptions of adaptive capacity in all the included primary healthcare services, regardless of variation in both governance and leadership. As discussed earlier, PHCPs responsibility increased during the pandemic. They had to make more decisions on their own, in for example, how to organize wards, organize patient care and interpret guidelines and information from state level. These finding are supported by other studies [44]. Moreover, it can be argued that there was a higher need for PHCP adaptations as organization of hospitals got first priority in beginning of the pandemic [8, 53].
Anderson et al. [54] say that “adapting safely to pressure is what keeps the health system functioning.” However, there are different types of adaptations, varying from long term adaptations and innovations to unsustainable adaptations required in poorly functioning systems [52]. In this study we identified long-term adaptations such as development of new tools for quick patient overview and better organization of patient rooms to decrease infection risk. However, the varying conditions in the primary healthcare service during the pandemic also induced short-term adaptations, which of many, lead to unsustainable short-term solutions (e.g., taking on extra shifts to cover for the lack of staff and taking on tasks outside their work scope). Such adaptations are often caused by system unpreparedness, forcing healthcare personnel to find quick fix solutions to maintain healthcare quality [52]. At the pandemic peak, these measures were necessary to be able to keep the healthcare service running. However, over time, short-term adaptations are masking system failures and may lead to worn out PHCP, intention to leave, lower staffing and consequently decreased patient safety and care quality [37, 55].
The lengthiness of a crisis will often have an impact on healthcare resilience in terms of anticipating, coping, recovering and learning from the crisis [56]. Bardoel & Drago [57] proposes two types of resilience related to crisis’ over time: acceptance resilience (resource preserving) and strategic resilience (resource enhancing). Acceptance resilience involves continuing work as before, aiming at the same goals as before, but with greater costs of resources required to do so [57], for example PHCPs aiming to provide the same high-quality care to patients as before the pandemic, but with more tasks and less personnel. In contrast, strategic resilience invests in new environments, relationships and goals aiming to gain more resources when facing adversity, including planning new pathways appropriate for the new state of the system [57].
Although both strategies can be successful coping mechanisms, it is argued that strategic resilience is the most productive strategy when confronting a long-term crisis such as the COVID-19 pandemic [56, 57]. Förster et al. [56] claims that the healthcare services more often encounter short and intensive crisis’ (e.g., acute illness or injury) and therefore uses the “acceptance resilience” strategy more often when responding to unforeseen events. This is supported by Barasa et al. [41] who found that healthcare systems often focused on resilience in acute or catastrophic shocks to the system, and more seldom on chronic, everyday challenges. COVID-19 has forced health personnel and healthcare systems to focus more on long-term solutions. Long-term solutions may involve changes in health system operation and development of alternative routes to reach the desired goal (patient safety and quality of care) [18, 19, 41]. This stresses the importance of learning from the things that worked when handling the COVID-19 pandemic (e.g., fixed working groups, readymade meals for patients and dedicated personnel taking caring for patients sociopsychological needs), learning from the things that did not work (e.g., increase work scope without increasing staff, removing tasks involving direct patient care to reduce workload and rationing PPE) and take health personnel suggestions for improvement into consideration (e.g., keeping a PPE storage, build premises suited for infection control (also in primary care), more involvement of PHCP in decisions regarding reorganization, and better planning ahead of reorganization). According to RiH, learning from previous crises are critical for handling future ones more effectively [58]. Although predictions of future pandemics like COVID-19 vary, there seem to be an agreement among experts that the world is at high risk for pandemics in near future [59,60,61]. In this context, more research aiming to learn from the COVID-19 pandemic, both from what went well, and what did not, is needed for healthcare systems become more resilient and thus stay resilient during long-time burdens or crisis’ [62,63,64]. The COVID-19 pandemic offers a unique potential for this task.
This paper adds to the COVID-19 literature by demonstrating the major learning potential COVID-19 has in terms of building more resilient primary healthcare services. Considering the World Health Organizations’ aim of building more resilient primary healthcare services [62], more research untapping this potential is needed.
Limitations
This study has certain limitations which should be considered. More municipalities from a wider area could have provided a broader perspective on PHCPs management of COVID-19 in rural healthcare services. There where however, relatively large variation in size, organization and rurality in the municipalities included, providing some variation in perspectives. Furthermore, due to COVID-19 restrictions, data were collected over time, implying that participants were at different stages of the COVID-19 development while being interviewed. This means that some PHCP had fresh experiences with the COVID-19 pandemic, while others had more retrospective experiences. What is more, there is a need to bear in mind the possible danger of diverting healthcare staff from patient care during the initial period of a crisis. However, the healthcare services set limits for this themselves by denying interview access until they had gained more control over the COVID-19 situation.
It is also important to consider that the PHCP were selected through their leaders. This strategy was implemented to enable the merging of interview time and work task at the respective wards yet, can generate issues such as undesirable pressure to participate or leaders selecting PHCP they think would provide “good” answers concerning the COVID-19 management. To limit this potential bias, the PHCP gave their final consent before the interview started and were given the opportunity to redraw from the study. The results indicate that recruited PHCP had varying experiences with the handling of the pandemic. Lastly, although the Norwegian perspective on PHCPs experiences of the COVID-19 pandemic in rural areas is lacking, adding additional countries would have strengthen the study.
Conclusion
Primary healthcare personnel in this study demonstrated major adaptive capacity despite working under varying and trying organizational conditions. Many of the adaptions they described improved function, and delivered long-term adaptations, though some were work-arounds needed to cope with poor management, governance, or lack of leadership. We found that although PHCPs are a critical piece in the complex resilience puzzle, they cannot create a resilient primary healthcare service on their own. All parts of the system, including policymakers, regulators, leaders, healthcare personnel, and patients and their families need to contribute to this task. Moreover, rural healthcare services have varied context, this needs to be taken into consideration when building resilient primary healthcare services. Lastly, the study is an indicator of the learning potential inherent in a pandemic experience, which stands for one of the most extreme challenges a system can face and offers lessons regarding how to build future resilient primary healthcare services. More research investigating the learning potential of the pandemic is needed, as well as research exploring the importance of the interplay between all parts of the system in the development of resilient healthcare systems.
Availability of data and materials
Data are available from the corresponding author upon reasonable request.
Change history
16 February 2024
A typo in the title was corrected.
Abbreviations
- PHCP:
-
Primary healthcare personnel
- RiH:
-
Resilience in healthcare
- PPE:
-
Personal protective equipment
References
Damian AJ, Gonzalez M, Oo M, Anderson D. A National study of community health centers’ readiness to address COVID-19. J Am Board Fam Med. 2021;34(Suppl):S85-s94.
Malin Knutsen G, Kristiana L, Siri W, David Westfall B, Elizabeth EA. Resilience perspective on healthcare professionals’ adaptations to changes and challenges resulting from the COVID-19 pandemic: a meta-synthesis. BMJ Open. 2023;13(9):e071828.
Khalid A, Ali S. COVID-19 and its challenges for the healthcare system in Pakistan. Asian Bioeth Rev. 2020;12:551.
Kearon J, Risdon C. The role of primary care in a pandemic: reflections during the COVID-19 pandemic in Canada. J Prim Care Community Health. 2020;11:2150132720962871.
Haldane V, Zhang Z, Abbas RF, Dodd W, Lau LL, Kidd MR, Haldane V, Zhang Z, Abbas RF, Dodd W, Lau LL, Kidd MR, Rouleau K, Zou G, Chao Z, Upshur REG, Walley J, Wei X. National primary care responses to COVID-19: a rapid review of the literature. BMJ Open. 2020;10(12): e041622. https://doi.org/10.1136/bmjopen-2020-041622.
World Health Organization and the United Nations Children’s Fund (UNICEF). A vision for primary healthcare in 21st century towards universal health coverage and the sustainable development goals. 2018. Contract No.: WHO/HIS/SDS/2018.X.
Hermansen M. COVID-19 underveis rapport (COVID-19 progress report). 2021.
OECD. Strengthening the frontline: how primary health care helpshealth systems adapt during the COVID-19 pandemic. 2021.
Plagg B, Piccoliori G, Oschmann J, Engl A, Eisendle K. Primary health care and hospital management during COVID-19: lessons from Lombardy. Risk Manag Healthc Policy. 2021;14:3987–92.
World Health Organization. Regional Office for the Western Pacific. Role of primary care in the COVID-19 response. Manila: WHO Regional Office for the Western Pacific; 2020. (Contract No.: WPR/DSE/2020/004).
Zhao S, Yin P, Xiao LD, Wu S, Li M, Yang X, Zhao Si, Yin P, Xiao LD, Wu S, Li M, Yang X, Zhang D, Liao L, Feng H. Nursing home staff perceptions of challenges and coping strategies during COVID-19 pandemic in China. Geriatr Nurs. 2021;42(4):887–93. https://doi.org/10.1016/j.gerinurse.2021.04.024.
Aase I, Ree E, Johannessen T, Strømme T, Ullebust B, Holen-Rabbersvik E, Aase I, Ree E, Johannessen T, Strømme T, Ullebust B, Holen-Rabbersvik E, Thomsen LH, Schibevaag L, van de Bovenkamp H, Wiig S. Talking about quality: how ‘quality’ is conceptualized in nursing homes and homecare. BMC Health Serv Res. 2021;21(1):104. https://doi.org/10.1186/s12913-021-06104-0.
Wiig S, Fahlbruch B. Exploring resilience - an introduction. In: Wiig S, Fahlbruch B, editors. Exploring resilience: a scientific journey from practice to theory. Springer briefs in applied sciences and technology: safety management. Cham: Springer Open; 2019. p. 1–3.
Stengel S, Roth C, Breckner A, Cordes L, Weber S, Ullrich C, Stengel S, Roth C, Breckner A, Cordes L, Weber S, Ullrich C, Peters-Klimm F, Wensing M. Resilience of the primary health care system - German primary care practitioners’ perspectives during the early COVID-19 pandemic. BMC Prim care. 2022;23(1):203. https://doi.org/10.1186/s12875-022-01786-9.
Albert SL, Paul MM, Nguyen AM, Shelley DR, Berry CA. A qualitative study of high-performing primary care practices during the COVID-19 pandemic. BMC Fam Pract. 2021;22(1):237. https://doi.org/10.1186/s12875-021-01589-4.
Litke N, Weis A, Koetsenruijter J, Fehrer V, Koeppen M, Kuemmel S, Litke N, Weis A, Koetsenruijter J, Fehrer V, Koeppen M, Kuemmel S, Szecsenyi J, Wensing M. Building resilience in German primary care practices: a qualitative study. BMC Prim care. 2022;23(1):221. https://doi.org/10.1186/s12875-022-01834-4.
Leslie M, Fadaak R, Pinto N, Davies J, Green L, Seidel J, et al. Achieving resilience in primary care during the COVID-19 pandemic: competing visions and lessons from Alberta. Healthc Policy = Politiques de sante. 2021;17(2):54–71.
Ree E, Wiig S, Seljemo C, Wibe T, Lyng, HB. Managers' strategies in handling the COVID-19 pandemic in Norwegian nursing homes and homecare services. Leadersh Health Serv (Bradf Engl). 2023;200–18. https://doi.org/10.1108/LHS-05-2022-0052. Ahead of print.
Lyng HB, Ree E, Wibe T, Wiig S. Healthcare leaders’ use of innovative solutions to ensure resilience in healthcare during the Covid-19 pandemic: a qualitative study in Norwegian nursing homes and home care services. BMC Health Serv Res. 2021;21(1):878. https://doi.org/10.1186/s12913-021-06923-1.
Fossberg B. Vi må lære av koronapandemien (english title: we need to learn from the COVID-19 pandemic) Tidskriftet. 2022;10:1-3
Creswell JW. Research design: qualitative, quantitative, and mixed methods approaches. 5th ed. Los Angeles: SAGE; 2018.
Holloway I, Galvin K. Qualitative research in nursing and healthcare. 4th ed. Chichester: Wiley Blackwell; 2017.
Statistic Norway. Areal og befolkning, etter region, statistikkvariabel og år (Area and population, by region, statistical variable and year). 2022. Available from: https://www.ssb.no/statbank/table/11342/tableViewLayout1/. Cited 2022 17.11.
Langørgen A, Løkken SA, Aaberge R. Gruppering av kommuner etter folkemengde og økonomiske rammebetingelser 2013 (Grouping of municipalities by population and economic framework conditions 2013). Oslo-Kongsvinger: Statistics Norway; 2015. Report No.: 2015/19.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3:77–101.
Golechha M, Bohra T, Patel M, Khetrapal S. Healthcare worker resilience during the COVID-19 pandemic: a qualitative study of primary care providers in India. World Med Health Policy. 2022;14(1):6–18.
Alboksmaty A, Kumar S, Parekh R, Aylin P. Management and patient safety of complex elderly patients in primary care during the COVID-19 pandemic in the UK-Qualitative assessment. PLoS ONE. 2021;16(3): e0248387. https://doi.org/10.1371/journal.pone.0248387.
Ruíz-Fernández MD, Fernández-Medina IM, Gálvez Ramírez F, Granero-Molina J, Fernández-Sola C, Hernández-Padilla JM. Experiences of home care nurses during the COVID-19 pandemic. Nurs Res. 2022;71(2):111–8. https://doi.org/10.1097/NNR.0000000000000566.
Andreassen T, Coward SK, Falk M, Forland F, Heradstveit P, Hveding Ø, et al. Erfaringar etter handteringa av smitte og utbrot av covid-19 i Noreg hausten 2021 og vinteren 2022 i utvalde kommunar (Experiences of handling infection and outbreak of covid-19 in Norway during autumn 2021 and winter 2022 in selection of municipalities). The Norwegian Institute of Public Health; 2022.
Juvet TM, Corbaz-Kurth S, Roos P, Benzakour L, Cereghetti S, Moullec G, Juvet TM, Corbaz-Kurth S, Roos P, Benzakour L, Cereghetti S, Moullec G, Suard J-C, Vieux L, Wozniak H, Pralong JA, Weissbrodt R. Adapting to the unexpected: problematic work situations and resilience strategies in healthcare institutions during the COVID-19 pandemic’s first wave. Saf Sci. 2021;139: 105277. https://doi.org/10.1016/j.ssci.2021.105277.
Marshall F, Gordon A, Gladman JRF, Bishop S. Care homes, their communities, and resilience in the face of the COVID-19 pandemic: interim findings from a qualitative study. BMC Geriatr. 2021;21(1):102. https://doi.org/10.1186/s12877-021-02053-9.
Hou Y, Zhou Q, Li D, Guo Y, Fan J, Wang J. Preparedness of our emergency department during the coronavirus disease outbreak from the nurses’ perspectives: a qualitative research study. J Emerg Nurs. 2020;46(6):848.
Franchini L, Varani S, Ostan R, Bocchi I, Pannuti R, Biasco G, Franchini L, Varani S, Ostan R, Bocchi I, Pannuti R, Biasco G, Bruera E. Home palliative care professionals perception of challenges during the Covid-19 outbreak: a qualitative study. Palliat Med. 2021;35(5):862–74. https://doi.org/10.1177/02692163211008732.
Macrae C. Reconciling regulation and resilience in Health Care. In: Hollnagel E, Braithwaite J, Wears RL, editors. Resilient health care. Ashgate studies in resilience engineering. Farnham: Ashgate; 2013. p. 111–21.
Hoyle L. I mean, obviously you’re using your discretion’: nurses use of discretion in policy implementation. Soc Policy Soc. 2014;13(2):189–202.
Wiig S, Aase K, Bal R. Reflexive Spaces: Leveraging resilience Into healthcare regulation and management. J Patient Saf. 2020.
Lyng HB, Macrae C, Guise V, Haraldseid-Driftland C, Fagerdal B, Schibevaag L, Lyng HB, Macrae C, Guise V, Haraldseid-Driftland C, Fagerdal B, Schibevaag L, Alsvik JG, Wiig S. Balancing adaptation and innovation for resilience in healthcare – a metasynthesis of narratives. BMC Health Serv Res. 2021;21(1):759. https://doi.org/10.1186/s12913-021-06592-0.
Grote G. Leadership in resilient organizations. In: Wiig S, Fahlbruch B, editors. Exploring resilience: a scientific journey from practice to theory. Volume 1. Cham: Springer Open; 2019. pp. 59–67.
Southwick FS, Martini BL, Charney DS, Southwick SM. Leadership and Resilience. In: Marques J, Dhiman S, editors. Leadership Today: practices for Personal and Professional Performance. Cham: Springer International Publishing; 2017. p. 315–33.
Mannion R, Exworthy M, Wiig S, Braithwaite J. The power of autonomy and resilience in healthcare delivery. BMJ Clinical Res Ed. 2023;382:e073331. https://doi.org/10.1136/bmj-2022-073331.
Barasa E, Mbau R, Gilson L. What is resilience and how can it be nurtured? A systematic review of empirical literature on organizational resilience. Int J Health Policy Manag. 2018;7(6):491–503. https://doi.org/10.15171/ijhpm.2018.06.
Sagan A, Webb E, Rajan D, Karanikolos M, Scott LG. Health system resilience during the pandemic: it’s mostly about governance. Eurohealth. 2021;27(1):10–5.
The Norwegian municipal sector organisation (KS). Kommunens erfaring fra Koronapandemien så langt Sluttrapport fra FoU-prosjekt for KS (Englis title: The municipality’s experience from the Corona pandemic so far final report from R&D project for KS). Oslo: KS/Deloitte; 2021. p. 148. Cited 2023 Oct 29. Available from: https://www.ks.no/sok/?query=+++++++plattformen+frivillighet+norge+ks+++++++&filter=dokumenter¤tPageNumber=36.
Glette MK, Ludlow K, Wiig S, Bates DW, Austin EE. Resilience perspective on healthcare professionals’ adaptations to changes and challenges resulting from the COVID-19 pandemic: a meta-synthesis. BMJ Open. 2023;13(9):e071828. https://doi.org/10.1136/bmjopen-2023-071828.
Haraldseid-Driftland C, Billett S, Guise V, Schibevaag L, Alsvik JG, Fagerdal B, Haraldseid-Driftland C, Billett S, Guise V, Schibevaag L, Alsvik JG, Fagerdal B, Lyng HB, Wiig S. The role of collaborative learning in resilience in healthcare—a thematic qualitative meta-synthesis of resilience narratives. BMC Health Serv Res. 2022;22(1):1091. https://doi.org/10.1186/s12913-022-08451-y.
Ford DM, editor. Editor four persistent rural healthcare challenges. Healthcare management forum. Los Angeles: SAGE Publications Sage CA; 2016.
Brandtzæg BA, Lunder TE, Aastvedt A, Thorstensen A, Groven S, Møller G. Utredning om små kommuner (Investigation of small municipalities). Ministry of Local Government and Modernization; 2019;473.
Barnard M, Mark S, Greer SL, Trump BD, Linkov I, Jarman H. Defining and analyzing health system resilience in rural jurisdictions. Environ Syst Decis. 2022;42(3):362–71. https://doi.org/10.1007/s10669-022-09876-w.
Ree E, Johannessen T, Wiig S. How do contextual factors influence quality and safety work in the Norwegian home care and nursing home settings? A qualitative study about managers’ experiences. BMJ Open. 2019;9(7): e025197. https://doi.org/10.1136/bmjopen-2018-025197.
Seljemo C, Viksveen P, Ree E. The role of transformational leadership, job demands and job resources for patient safety culture in Norwegian nursing homes: a cross-sectional study. BMC Health Serv Res. 2020;20(1):799. https://doi.org/10.1186/s12913-020-05671-y.
van de Bovenkamp H, van Pijkeren N, Ree E, Aase I, Johannessen T, Vollaard H, van de Bovenkamp H, van Pijkeren N, Ree E, Aase I, Johannessen T, Vollaard H, Wallenburg I, Bal R, Wiig S. Creativity at the margins: a cross-country case study on how Dutch and Norwegian peripheries address challenges to quality work in care for older persons. Health Policy. 2023;127:66–73. https://doi.org/10.1016/j.healthpol.2022.12.008.
Lyng HB, Macrae C, Guise V, Haraldseid-Driftland C, Fagerdal B, Schibevaag L, Lyng HB, Macrae C, Guise V, Haraldseid-Driftland C, Fagerdal B, Schibevaag L, Alsvik JG, Wiig S. Exploring the nature of adaptive capacity for resilience in healthcare across different healthcare contexts; a metasynthesis of narratives. Appl Ergon. 2022;104: 103810. https://doi.org/10.1016/j.apergo.2022.103810.
Halcomb E, Williams A, Ashley C, McInnes S, Stephen C, Calma K, et al. The support needs of Australian primary health care nurses during the COVID-19 pandemic. J Nurs Adm Manag. 2020;28(7):1553–60.
Anderson JE, Ross AJ, Macrae C, Wiig S. Defining adaptive capacity in healthcare: a new framework for researching resilient performance. Appl Ergon. 2020;87:103111.
Wears RL, Hettinger AZ. The tragedy of adaptability. Ann Emerg Med. 2014;63(3):338–9. https://doi.org/10.1016/j.annemergmed.2013.10.035.
Förster C, Füreder N, Hertelendy A. Why time matters when it comes to resilience: how the duration of crisis affects resilience of healthcare and public health leaders. Public Health. 2023;215:39–41. https://doi.org/10.1016/j.puhe.2022.11.024.
Bardoel EA, Drago R. Acceptance and Strategic resilience: an application of conservation of resources Theory. Group Org Manag. 2021;46(4):657–91. https://doi.org/10.1177/10596011211022488.
Hollnagel E. Safety-II in Practice: developing the resilience potentials. 1st ed. London: Routledge; 2018.
Haileamlak A. Pandemics will be more frequent. Ethiop J Health Sci. 2022;32(2):228.
Smith J. Q&A: Future pandemics are inevitable, but we can reduce the risk European comission: European Comission. 2021. Available from: https://ec.europa.eu/research-and-innovation/en/horizon-magazine/qa-future-pandemics-are-inevitable-we-can-reduce-risk.
Smitham E, Glassman A. The Next Pandemic Could Come Soon and Be Deadlier Center for Global development: Center for Global development. 2021. Available from: https://www.cgdev.org/blog/the-next-pandemic-could-come-soon-and-be-deadlier.
World Health Organization. Building health systems resilience for universal health coverage and health security during the COVID-19 pandemic and beyond: WHO position paper. 2021. Contract No.: WHO/UHL/PHCSP/2021.01.
World Health Organization. Fostering resilience through integrated health system strengthening: technical meeting report. Geneva: World Health Organization; 2021. (Contract No.: CC BY-NC-SA 3.0 IGO).
World Health Organization. Building health systems resilience for universal health coverage and health security during the COVID-19 pandemic and beyond: a brief on the WHO position. Geneva: World Health Organization; 2021. (Contract No.: CC BY-NC-SA 3.0 IGO).
Acknowledgements
Not applicable.
Funding
The publication processing charge was covered by the University of Stavanger.
Author information
Authors and Affiliations
Contributions
MKG, SW, DWB and TK participated in discussions involving the development of the project. MKG and TK conducted the focus group interviews and MKG conducted the analysis of the data material. MKG, SW, DWB, TK and PD contributed in writing the manuscript. All Authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki, and all methods were carried out in accordance with relevant guidelines and regulations. The ethical approval was conducted by the Norwegian center for research data (NSD) (registration number: 655437). NSD was renamed Sikt (Norwegian Agency for Shared Services in Education and Research) in 2022 and provides the ethical approval, information security and privacy services as a part of the HK-dir (Norwegian Directorate for Higher Education and Skills). Approval by Sikt (former NSD) is considered sufficient ethical approval for Norwegian studies without involvement of patients, as Sikt serves as an ethics committee for research in Norwegian universities, assessing ethics, information security and privacy. All participants signed an informed consent form prior to the interviews, and information about the aim of the study and their right to redraw was repeated immediately before the interviews started.
Consent for publication
Not applicable.
Competing interests
Dr. Bates reports grants and personal fees from EarlySense, personal fees from CDI Negev, equity from ValeraHealth, equity from Clew, equity from MDClone, personal fees and equity from AESOP, personal fees and equity from Feelbetter, equity from Guided Clinical Solutions, and grants from IBM Watson Health, outside the submitted work. Dr. Bates has a patent pending (PHC-028564 US PCT), on intraoperative clinical decision support. The other authors report no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Glette, M.K., Bates, D.W., Dykes, P.C. et al. A resilience perspective on healthcare personnels’ experiences of managing the COVID-19 pandemic: a qualitative study in Norwegian nursing homes and home care services. BMC Health Serv Res 23, 1177 (2023). https://doi.org/10.1186/s12913-023-10187-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-10187-2