Abstract
Background
While involving users in healthcare decision-making has become increasingly common and important, there is a lack of knowledge about how to best design community-based health screening programs. Reviews of methods that incorporate discrete choice experiments (DCEs) are scarce, particularly for non-cancer illnesses like cardiovascular disease, diabetes and liver disease. We provide an overview of currently available applications and methods available by using DCEs in health screening programs, for chronic conditions.
Methods
A scoping review was undertaken, where four electronic databases were searched for key terms to identify eligible DCE studies related to community health screening. We included studies that met a pre-determined criteria, including being published between 2011 and 2021, in English and reported findings on human participants. Data were systematically extracted, tabulated, and summarised in a narrative review.
Results
A total of 27 studies that used a DCE to elicit preferences for cancer (n = 26) and cardiovascular disease screening (n = 1) programmes were included in the final analysis. All studies were assessed for quality, against a list of 13 criteria, with the median score being 9/13 (range 5–12). Across the 27 studies, the majority (80%) had the same overall scores. Two-thirds of included studies reported a sample size calculation, approximately half (13/27) administered the survey completely online and over 75% used the general public as the participating population.
Conclusion
Our review has led to highlighting several areas of current practice that can be improved, particularly greater use of sample size calculations, increased use of qualitative methods, better explanation of the chosen experimental design including how choice sets are generated, and methods for analysis.
Similar content being viewed by others
Background
In recent years, there have been increased calls for user’s involvement in healthcare decision-making [1, 2]. User involvement can support decision-making at the planning and rolling out stages and these views can be elicited quantitatively, qualitatively or using a mixed-methods approach [3, 4]. Discrete choice experiments (DCEs) are a quantitative technique for appraising user choices, and are increasingly used to inform decisions on healthcare treatments, diagnostics and screening programs [5].
Since 1990, there has been a marked increase in years lived with disability from non-communicable diseases including cancer, cardiovascular and liver disease [6]. Over the next 15 years, the human and economic costs of these diseases are estimated to total more than US$7 trillion in developing countries alone [7]. To address this, preventive interventions and early detection of disease is a key area of research. A comprehensive approach, which includes health screening programs, are often being recommended [7, 8]. Professional societies recommend health screening programs, because patients with screen detected chronic disease are more likely to have early-stage disease and better prognosis [9, 10]. For example, patients at higher risk for cancer or fibrosis due to chronic hepatitis B, cirrhosis, and non-alcoholic fatty live disease are recommended to have surveillance examinations such as imaging and histology tests [11, 12]. Despite the many available screening programs and current recommendations, health screening uptake remains low in many countries [13, 14]. To increase uptake there is a need to quantify users’ preferences for health screening programs, using the robust method of discrete choice experiments [3].
Studies reporting DCE methods and results can provide decision-makers and researchers with valuable insights how health screening programs could be delivered more effectively and more efficiently [15]. In a DCE, participants state their preferred option from a set of alternative services, described by the same attributes but perhaps differing in their amount, known as levels [3].
The use of DCEs in the healthcare setting is increasing but reviews of methods that incorporate DCEs are scarce. Systematic reviews of health related DCEs have increased from seven studies in 1999 [16], to 30 studies in 2008 [17] and 98 studies in 2015 [18]. These reviews included and analysed 129, 114 and 301 DCEs respectively, but did not categorise by treatment, screening, or prevention options. The reviews identified a substantial variation [17] as well as inadequate reporting of the methods [18], inhibiting quality assessment. Therefore, there is need to summarize the methods used in previous DCE studies. There have been some reviews of the DCEs regarding health screening programs, including cancer screening [19], colorectal cancer screening [20, 21], and newborn screening [22]. Generally, these reviews concluded that the specific methodological issues raised when conducting DCEs in health screening programs, indicating the methodology needs to be evolved. To our knowledge, no review has summarised studies that have elicited preferences for chronic disease screening programmes such as cancer screening programs as well as cardiovascular or liver disease screening programs besides increased number of screening programmes for chronic conditions [13, 14].
This study was designed to conduct a scoping review of DCEs of health screening programs for chronic conditions including cancer, cardiovascular and liver disease screening programs. The objectives were to: (1) identify published studies using DCEs in chronic condition screening programs and synthesize current methodology used in previous DCE studies; (2) assess the quality of included DCE studies, and (3) provide recommendations for future design of DCEs in relation to community-based health screening programs as well as an item list for developing attributes of DCEs in community screening.
Methods
A scoping review was considered the most appropriate study design [23] to identify the methodologies used in DCEs in health screening programs, describe the key characteristics of DCEs used, and identify key gaps in this research field. This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) statement for processing and reporting scoping reviews [24, 25] (Appendix 1). A review protocol was developed with search methods and inclusion criteria specified in advance (Appendix 2). As this is a scoping review, registration in PROSPERO was not applicable.
Inclusion and exclusion criteria
This scoping review included studies meeting the following criteria: (1) applied a discrete choice experiment method; (2) was used to elicit consumer/provider/stakeholders’ preferences towards a chronic disease screening program; and (3) published in English since January 2011. The target population of this review is consumers, healthcare providers and stakeholders who were involved in a chronic disease screening program. Studies were excluded if the DCE:
-
was a non-community-based screening program (intended to focus on population/community-based screening programs only).
-
was associated with prenatal screening, newborn screening, communicable disease screening, or genetic testing (as the review of the DCEs regarding newborn screening [22] was conducted recently and the current review intended to focus on non-communicable disease screening programs such as cancer screening as well as liver and cardiovascular disease screening programs).
-
was a scholarly review, letter to the editor, commentary, news article or conference abstract.
Final decisions regarding the inclusion or exclusion of studies were made by consensus among all reviewers (SK, DB and AJ). Full inclusion and exclusion criteria for selection of studies are shown in the protocol in Appendix 2.
Search strategy
Four electronic databases (EMBASE, MEDLINE, PubMed, National Health Service Economic Evaluation Databases from 01 Jan 2011 up to 04 Mar 2021) were searched with the assistance of a librarian to identify the studies that applied a DCE method to elicit consumers’, providers’ or stakeholders’ preferences towards a health screening program. The following search terms were used: “discrete choice*” or “stated preference*” or “conjoint analysis*” and “consumer*” or “patient*” or “health care personnel*” or “stakeholder*” and “preference*” or “value*” and “screening” or “surveillance” or “health assessment”. The search was restricted to the English language and by publication since 2011. The reference lists of included studies were manually searched for other relevant studies.
Data extraction and quality assessment
After removal of duplicates using EndNote software, studies were imported into a web-based review program – Rayyan [26]. The titles and abstracts were screened for relevance and adherence to eligibility criteria by three reviewers, independently, and data were extracted using a predesigned extraction form. In preparation for data extraction, a predesigned data extraction spreadsheet was piloted and iteratively revised by the research team. The author (AJ) extracted data using the final version of this spreadsheet in Microsoft Excel. The data extraction sheet was pilot tested on five studies and was revised to include:
-
background information - data source, period of publication, location, sample size, age group;
-
development of choice set - methods for attributes and levels selection, number of attributes, levels, alternatives with or without opt-out option;
-
attribute development - design type, plan, software;
-
econometric analyses - econometric analysis model, software;
-
presented outcome measures (Appendix 3).
We followed a five-step development process for data extraction and analysis of choice sets [27]. This is a rigorous and systematic approach to DCE development which is useful to establish methods for reducing and prioritising attributes. Additionally, more general attribute domains: process attributes, outcome attributes, cost attributes, and others - proposed by existing systematic reviews [28] were used to extract and analyse data as the current scoping review aimed to summarise the methods used in DCEs in community health screening programs.
The quality of each study was assessed using a list of 13 criteria, which covers all four key stages of a discrete choice experiment, using a previously published and validated approach [29]. Each item in the checklist was scored as having ‘met the criteria in full’ (‘1’) and ‘partially met or did not meet the criteria’ (‘0’). Overall compliance with the checklist was calculated as the proportion of the checklist criteria addressed by the study. The quality assessment for each study is presented in Appendix 4.
Results
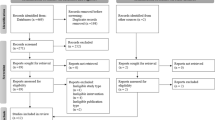
Search strategy
Figure 1 details the flow of studies through the review process. A total of 3197 articles were identified in the electronic database search, of which 1483 were duplicates. Titles and abstracts for 1226 unduplicated abstracts were reviewed by three authors (SK, DB, and AJ) using Rayyan [26], with a further 1184 articles excluded. Disagreements (n = 12) were resolved by consensus among authors. One study was not able to be retrieved. Of the 44 studies assessed for eligibility, 27 fully satisfied the pre-determined inclusion criteria.
Quality assessment
All studies were scored against a list of 13 criteria [29], with median count of 9/13, and a range between 5 [30] and 12 [31]. Across the 27 studies, majority of studies (80%) had the same overall score and response to individual criteria except a few studies that scored between 5 and 6.
Background information of included studies
Table 1 provides an overview of descriptive information for the 27 included studies. Only one of 27 studies examined preferences for a cardiovascular disease screening program [32], while the remaining studies investigated preferences for cancer screening programs. The most common objective was to explore the general population’s preferences for a health screening program, which was examined in 21 studies. A median of 685 participants were approached with considerable variation among the studies (range 46 to 4000). When a general population was used, the median remained the same. There was no discernible increase in the number of participants approached when choice sets with higher number of attributes and levels were used. Of 27 DCEs, three had sample sizes less than 100 respondents, whereas eleven of the 27 DCEs had a sample size greater than 1,000 respondents. Only 18 studies reported sample size considerations such as parametric approach [33], Orme’s rule-of-thumb [31, 34,35,36,37,38,39], and referring studies [40, 41].
The methods of data collection varied between studies but were mostly either self-completed online choice sets or self-completed paper-based choice sets. Participants in 13 of 16 online administered surveys were recruited via an online survey panel. Response rates varied from 5 to 6% [38, 42] to 100% [34, 43, 44]. High response rates were reported in studies where participants were directly invited and data were collected via face-to-face interview [34, 45]. Low response rates were reported in studies where participants were invited via email or traditional mail [36, 38]. In studies where data were collected through an online survey panel, there was a large variation in response rates (6-100%) [42, 44]. Several studies offered a reimbursement to participants.
Developing choice sets
The first step in developing choice sets is to generate a list of attributes using information from literature reviews and qualitative work. Twenty-two of 27 studies conducted literature and/or systematic reviews, and the remainder used: a small qualitative study [42], semi-structured interviews with the target population and healthcare providers [35], or existing research [36, 40, 43]. Ten studies identified attributes and levels through a combination of literature reviews and qualitative work with either a specified target population or identified experts. Interviews were conducted in nine studies, with the majority conducting interviews with both experts and a specified target population, with variable number of participants. For example, De Bekker-Grob, Rose [46] completed interviews with both experts in the field of prostate cancer screening (n = 8) and men aged 55–75 years (n = 8) while Li, Liu [45] interviewed rural women aged 30–65 (n = 15) and clinical experts in the field of cervical cancer screening, to get feedback on the list of attributes created from a literature review. Six studies used focus group: two groups with four participants each [31], eight focus groups with eight women each [34], three focus groups with seven participants each [47], and one focus group with eight individuals [41]. Two of these six did not state how many participants were involved in the focus group [42, 48].
In the second step, a ‘long list’ of attributes was screened by experts to determine whether they would be feasible or meaningful to include in a DCE study. Nine studies involved experts’ opinion in selecting attributes and levels of attributes. Where attributes and levels were created from literature review only (n = 3), literature review combined with qualitative work (n = 3), or literature review combined with existing research or data (n = 3) were validated with expert opinion, according to the area of research.
In the third step, a structured prioritisation or ranking exercise was used. Ten studies reported that interviewers or focus group participants were asked to rank the attributes from most important to least important, with respect to their preferences for screening [33, 40,41,42, 44, 46, 47, 49,50,51] to identify the relative importance of various attributes. Following this ranking exercise, with or without subsequent panel discussion, a set of exclusion and inclusion criteria was agreed with reference to a study objective.
In the fourth step, qualitative and/or quantitative pilot tests were undertaken to validate the scenarios and content, face validity, usability, robustness, and likely response rate to DCE questionnaires. Two-thirds of studies reported piloting their surveys before full rollout. There was great variation in piloting, ranging from a qualitative face-to-face interview with only nine individuals from the target population [40], to a two-step procedure including face-to-face interview and online questionnaire completed by 116 participants [50]. Two studies used “think aloud” techniques to check for any problems in interpretation of the attributes, levels, and face validity [47, 51]. In one study [41] the participants were asked to verbalize their thought process during decision-making. There are two types of think aloud: (1) concurrent think aloud is where people are asked to verbalise what they are thinking as they complete a certain task, and (2) retrospective think aloud asks people to describe what they were thinking after the task has been completed. The study [41] applied a mixed approach: the respondents were asked to think-aloud for two or three choices, and then to reflect after this. If the respondent was silent for a period of time, they were reminded to keep thinking aloud. In the final stage, issues raised from pilot testing were considered and the final attributes and levels were agreed via expert panel discussions. Seven studies stated that no alterations were made after pilot testing [36, 39, 42, 46, 47, 50, 52].
In summary, only a single study applied this five-stage development process and established twelve unlabelled choices of two alternatives, with 5 attributes and 4 levels for each attribute [41]. In this single study, instead of using the “think aloud” technique, researchers conducted two face-to-face pilot studies to ascertain if respondents could manage the length of the questionnaire and to examine its intelligibility, acceptability, and validity [41].
The number of attributes per alternative in the included DCEs ranged from three to ten, with an average of six (Table 2). The most frequently used attributes in these DCEs were details for screening procedure, such as travel time, location, interval, false positive/negative test, sensitivity, and specificity (n = 26), regarding costs - out of pocket costs, cost to health service, and cost of follow-up care (n = 18). Less frequently used outcome attributes were related to health outcomes, such as reduction in mortality, risk of overtreatment, and surgical outcomes (n = 14), and others such as scientific evidence, target population, and stakeholder’s action (n = 8).
The average number of levels for each attribute was three, with a maximum of six and a minimum of two. Ten studies included 5 attributes, followed by six studies reporting 6 and other six reporting 7 or more attributes. Sixteen studies used generic or unlabelled scenarios; six studies used labelled scenarios while four did not report their approach clearly enough to tell. A single study used both labelled and generic scenarios [53]. The majority of included studies included two alternatives (n = 14), not including an opt-out option, with four studies including three alternatives. Almost half of the reviewed studies (n = 12) did not include an opt-out option.
Generating experimental design
Table 3 shows the current trends with respect to experimental design and construction of choice sets. Twenty-five studies used a fractional factorial design; the remaining two studies used a full factorial design. Of the 25 studies that used a fractional factorial design, majority (n = 16) did not state the type, others used orthogonal (n = 6) or balanced (n = 2) or both (n = 1) types. The most common measure to select the design type was D-efficient (n = 16). Only one study used C-efficient, and the rest ten studies did not state this. Seventeen studies used only a main effects design, while five studies used a main effect plus two-way interaction design [33, 36, 47, 49]. Five studies did not report this aspect of the design plan.
Eleven studies reported using blocks when generating the experimental design (Table 3). On average, studies with blocked design had 650 participants, each of whom completed 10 choice sets, whereas studies without blocking had an average of 230 participants, completing 20 choice sets. Norman, Moorin [43] created an unblocked design with 100 unique choice sets and included those participants in the analysis who completed at least one choice set.
Conducting econometric analyses
There was considerable variation in methods of econometric analyses between the reviewed studies (Table 4). Ten studies analysed their preference data using modelling techniques such as mixed logit (n = 6) and Hierarchical Bayes mixed logit (HB-MXL) model (n = 4). Multinominal logit (MNL) and Latent Class logit were used each in three studies while Mixed Multinominal logit (MMNL) and logit were used in two studies. Few studies employed two or more models [42, 43, 47, 48].
Several authors explained why they chose a certain model. For example, de Bekker-Grob, Donkers [47] explained that given their interest in accounting for systematic preference heterogeneity and also taking scale effects into account (i.e. how consistent individuals make their choices), a Heteroscedastic model within a four step approach was employed to determine optimal utility function. Others used Latent class logit model with explanation of appropriateness for identifying different utility functions across different or unobserved subgroups [46, 51]. Another study did not clearly report which model or method was used to analyse weights relating to the utility importance [44].
Software used
In designing, the most common software packages used to generate experimental designs were Ngene (8 studies) and SAS (6 studies) followed by Sawtooth (5 studies) and SPSS (2 studies). The remaining 6 studies did not clearly indicate the software.
In analysis, six of 27 studies used STATA and five studies used NLOGIT (Econometric Software). Sawtooth and SPSS were each used by three studies while R and SAS each by two studies. Five studies did not report what software they used for analysis.
Outcomes
Twenty-two studies presented their outcomes as utility scores (Table 5). Willingness to pay (WTP) as well as willingness to accept (WTA) were estimated in eleven studies. Only three studies used relative importance and ranking as a primary outcome [35, 44, 54], while another three studies calculated changes to uptake rate according to change in attributes/levels [34, 41, 45]. The remaining three studies presented their results as “other” outcomes, including relative risk [30], choice shares [55], and maximum acceptable risk [38].
There are several function measures that can describe a model’s power, and how well a statistical model fits a set of observations. Thirteen studies reported that they employed likelihood function measures with or without Pseudo R2, Bayesian information criterion (BIC), and Akaike information (AIC) criterion to show the model fit. Several studies reported that selection of model was based on goodness of fit measures [42, 43, 47, 54]. Rest of the studies did not report this information.
Discussion
This scoping review gives an overview of available DCE studies evaluating preferences and identified current available applications and key methods used in DCEs to elicit preferences for community health screening programs. Of the 27 included studies, none were related to liver disease which indicates that there is a lack of reporting DCE methods in relation to community screening programmes unless they are related to cancer disease.
Methods in developing choice sets.
Advice regarding methods to develop the attributes and levels of attributes for DCE choice sets are scarce. De Brún, Flynn [27] has given a five-stage development strategy consisting of exploratory work, expert panel discussion, prioritisation, pilot testing and a second expert panel discussion [27]. Moreover, Trapero-Bertran, Rodríguez-Martín [56] recommended to use more in-depth methods such as interviews, sub-group analysis, and expert opinion. These qualitative methods enable sensitive subjects to be discussed and attributes captured, reducing the potential for misspecification of attributes through over-reliance on the views of limited number of experts or researchers. Hence, our review followed a five-step development process proposed by De Brún, Flynn [27] that allows to check whether attributes were developed through qualitative methods. We found that less than 50% of reviewed studies used qualitative methods in selecting attributes and levels of attributes, revealing an area for significant improvement. It is advisable to use qualitative methods to develop and select attributes for DCEs of community screening programs, with clear reporting criteria. Also, we recommend a revised, shortened version of De Brún, Flynn [27] methods for developing attributes for community screening programmes, to facilitate efficiency by excluding the pilot testing stage. This four-stage method could include (1) literature review to develop an initial attribute list, (2) a focus group discussion including patients, clinicians, primary health workers and other stakeholders to revise, to add and remove from the list provided by the review, (3) prioritisation exercise using a sample of clinicians and patients, and (4) expert panel discussion to finalise the attributes and the levels of attributes. After finalising the attributes and the levels of attributes, pilot testing survey will be conducted to ascertain comprehension and understanding of the DCE choice tasks, attributes, and their levels via conducting one-on-one interviews and/or an online survey. The current review allows us to develop a list of items that could be useful in developing attributes of any community screening programme (Table 1, Appendix 5).
Experimental design
An experimental design is a sample from all possible combinations of the developed attributes and levels. Since a complete combination of all attributes and levels (a full factorial design) is too large to be used in practice, a fractional factorial is frequently used. Lancsar and Louviere [3] recommended to use optimal designs in DCEs in healthcare service because it makes the DCE more robust. Our review found that fractional factorial design is the most popular method to create choice sets using D-efficient as a measure to select designs. Ngene is the most popular software tool for generating experimental designs in DCEs for community-based health screening programmes. Main effects are dominant in the reviewed DCE studies but researchers recommended avoiding small fractional designs that only allows estimation of main effects [3]. Moreover, at a minimum, designs that allow independent estimation of all main effects and two-way interactions ensure that even if two-way interactions are significant, they are independent of main effects, minimising bias if interactions are omitted [57]. In summary, we would recommend fractional factorial design using a D-efficient measure that allows estimation of main effects with limited interactions considering theory, intuition, feasibility in terms of sample size and survey design [58].
Designing choice sets
In the context of screening, an opt out is likely to be important because the reality is that many people do opt out of screening resulting in health screening uptake remains low in many countries [13, 14]. The inclusion of an opt out option in a DCE or choose neither option may have an effect on choice behaviour [3, 59]. Thus, it is recommended to allow respondents to opt out or choose neither option that can reveal the reality of health screening uptake. More than half of reviewed studies offered an opt-out option. Since offering opt-out options, a dual response design is strongly recommended to increase data quality [59]. In a dual response design, participants first make a forced choice and then participants are asked if they would like to opt-out if given the choice [60]. This might reduce the risk that a direct introduction of an opt-out results in large numbers of respondents avoiding to seriously weigh the different levels of attributes [59].
Analysis methods
The current review found considerable variation in methods of econometric analyses which raises concern about the validity of the results. The ISPOR guidelines and more importantly theoretical underpinning suggests conditional logit as one of the most common analysis methods [61]. Other models such as scale multinomial logit, generalised multinomial logit and mixed logit have also been recommended. The conditional logit model was first suggested by McFadden [62] proposing random utility model which describes the choice among alternatives due to the characteristics of attribute levels defining those alternatives [61]. Multinomial logit is similar to conditional logit but the choices with multinomial logit are more reflective of the characteristics of the respondents [61, 63]. Of the 27 reviewed studies only ten had used one of the recommended analysis methods and three had used conditional logit. Others had not justified the use of different analysis models. Our recommendation is to follow the ISPOR guidelines on best practices [61, 64]. For evaluating the goodness-of-fit of the model, pseudo R2 measures and AIC or BIC are ideal techniques. However, both have strengths and limitations. AIC and BIC focus on minimizing underestimation rather than checking the adequacy of the model to explain responses in the data as done in the pseudo R2 measures. Our review findings were consistent with these guidelines and we would recommend using goodness of fit measures such as likelihood function measures with Pseudo R2, BIC, and AIC to compare and/or select a model.
Sample size
The sample size for DCE study depends on the chosen statistical model, significance level, statistical power level, the experimental design, and likely parameter estimates [65, 66]. Consequently, the reviewed studies used a wide range of sample sizes as well as a variety of sample size calculation methods. Initially, in the healthcare sector, the number of eligible public informants and healthcare providers is generally limited. Consequently, minimum and adequate sample size is needed to have statistical power to detect a difference in preferences when this difference is sufficiently large [65]. Studies that were published in the last 2 years [47, 51, 54] applied the minimum sample size for health care related DCE studies proposed by de Bekker-Grob, Donkers [65]. Compared to other methods such as parametric approach, rule of thumb, and referring studies, this approach was better suited to determine the minimum required sample size for hypothesis testing for coefficients based on DCEs, and can be extended to functions of parameters [65]. The parametric approach can only be used if prior parameter estimates are available and are not equal to zero [66]. The rule of thumb methods are not intended to be strictly accurate or reliable [65]. The number of participants approached varied from very small (n = 46) to large (n = 4000). However, the average size was approximately 1000 when the general population or clinicians were surveyed.
Survey method
Compared with face-to-face interview and paper-based methods, online surveys are cheaper and save time [67]. This review found that response rates were high when studies used face-to-face interview methods to collect data, while response rates varied in studies where DCEs were administered to an online survey panel. We recommend using face to face data collection methods to improve validity and failing that, a known contact list to collect data from clinicians and patients. When DCE data collection involve general population, the convenient method is to use a valid online panel.
Strengths and limitations
This study focuses on the technical aspects of DCE studies in relation to their use in community health screening programs. The number of DCE studies is increasing over time, and our work can serve both as a guide to the details of conducting a DCE and as a practical aid to future research. We have highlighted several areas of current practice that can be improved, particularly greater use of sample size calculations, increased use of qualitative methods, better reporting of how choice sets are generated, and explanation of chosen experimental design and analysis method.
A limitation of this scoping review was the reliance on what was reported in the studies published in English language between Jan 2011 and Mar 2021. Additionally, abstracts based on a conference presentation were excluded.
Conclusion
Discrete Choice Experiments of community health screening programmes vary substantially with respect to developing choice sets and generating experimental design. These variations limit the overall conclusions and generalisability of the results in policy contexts. Nevertheless, based on information obtained from the studies included in this review, our findings provide a series of recommendations for future DCE studies related to community-based health screening programmes.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
References
Epstein RMMD, Street RLP. The Values and Value of Patient-Centered Care. Ann Fam Med. 2011;9(2):100–3.
Ho MM, Saha ABSE, McCleary KKBA, Levitan BMDP, Christopher SMA, Zandlo KMBA, et al. A Framework for Incorporating Patient Preferences Regarding Benefits and Risks into Regulatory Assessment of Medical Technologies. Value Health. 2016;19(6):746–50.
Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making. Pharmacoeconomics. 2008;26(8):661–77.
Soekhai V, Whichello C, Levitan B, Veldwijk J, Hammad T, Kihlbom U, et al. Compendium of methods for measuring patient preferences in medical treatment. Value Health. 2017;20(9):A684-A5.
York Health Economics Consortium. Discrete Choice Experiment (DCE) 2016 [Available from: https://yhec.co.uk/glossary/discrete-choice-experiment-dce/.
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
United Nations General Assembly. Political declaration of the third high-level meeting of the General Assembly on the prevention and control of non-communicable diseases. New York: United Nations 2018 [
Jameson JL, Longo DL. Precision medicine—personalized, problematic, and promising. Obstetrical Gynecol Survey. 2015;70(10):612–4.
Omata M, Lesmana LA, Tateishi R, Chen P-J, Lin S-M, Yoshida H, et al. Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int. 2010;4(2):439–74.
Kansagara D, Papak J, Pasha AS, O’Neil M, Freeman M, Relevo R, et al. Screening for Hepatocellular Carcinoma in Chronic Liver Disease. Ann Internal Med. 2014;161(4):261–9.
European Association For The Study Of The Liver. EASL–EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56(4):908–43.
Leoni S, Tovoli F, Napoli L, Serio I, Ferri S, Bolondi L. Current guidelines for the management of non-alcoholic fatty liver disease: A systematic review with comparative analysis. World J Gastroenterol. 2018;24(30):3361–73.
AIHW. Cancer screening program: quarterly data: Australian Institute of Health and Welfare; 2021 [Available from: https://www.aihw.gov.au/reports/cancer-screening/national-cancer-screening-programs-participation/contents/national-bowel-cancer-screening-program/participation.
tot Babberich MPdN, Vermeer NC, Wouters MW, van Grevenstein WM, Peeters KC, Dekker E, et al. Postoperative Outcomes of Screen-Detected vs Non–Screen-Detected Colorectal Cancer in the Netherlands. JAMA Surg. 2018;153(12):e183567-e.
Neumann PJ, Goldie SJ, Weinstein MC. Preference-based measures in economic evaluation in health care. Ann Review Public Health. 2000;21(1):587–611.
Ryan M, Gerard K. Using discrete choice experiments to value health care programmes: current practice and future research reflections. Appl Health Econ Health Policy. 2003;2(1):55–64.
de Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Economics. 2012;21(2):145–72.
Soekhai V, de Bekker-Grob EW, Ellis AR, Vass CM. Discrete Choice Experiments in Health Economics: Past, Present and Future. PharmacoEconomics. 2019;37(2):201–26.
Mansfield C, Tangka FK, Ekwueme DU, Smith JL, Guy GP, Jr., Li C, et al. Stated Preference for Cancer Screening: A Systematic Review of the Literature, 1990–2013. Prev Chronic Dis. 2016;13:E27.
Ghanouni A, Smith SG, Halligan S, Plumb A, Boone D, Yao GL, et al. Public preferences for colorectal cancer screening tests: a review of conjoint analysis studies. Expert Rev Med Devices. 2013;10(4):489–99.
Wortley S, Wong G, Kieu A, Howard K. Assessing stated preferences for colorectal cancer screening: a critical systematic review of discrete choice experiments. Patient. 2014;7(3):271–82.
Vass CM, Georgsson S, Ulph F, Payne K. Preferences for aspects of antenatal and newborn screening: a systematic review. BMC Pregnancy Childbirth. 2019;19(1):131-.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143-.
Peters MD, Godfrey CM, McInerney P, Munn Z, Tricco AC, Khalil H, et al. Scoping reviews. 2020. In: JBI Manual for Evidence Synthesis. [2119-26]. Available from: https://doi.org/10.46658/JBIMES-20-12.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Internal Med. 2018;169(7):467–73.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
De Brún A, Flynn D, Ternent L, Price CI, Rodgers H, Ford GA, et al. A novel design process for selection of attributes for inclusion in discrete choice experiments: case study exploring variation in clinical decision-making about thrombolysis in the treatment of acute ischaemic stroke. BMC Health Serv Res. 2018;18(1):483.
Gutknecht M, Schaarschmidt ML, Herrlein O, Augustin M. A systematic review on methods used to evaluate patient preferences in psoriasis treatments. J Eur Acad Dermatol Venereol. 2016;30(9):1454–64.
Mandeville KL, Lagarde M, Hanson K. The use of discrete choice experiments to inform health workforce policy: a systematic review. BMC Health Serv Res. 2014;14(1):367.
Walters SJ, Winslow M, Collins K, Robinson T, Green T, Madan J, et al. Health care professionals’ preferences for extending mammographic breast screening to the over 70s. J Geriatr Oncol. 2011;2(1):1–10.
Sicsic J, Pelletier-Fleury N, Moumjid N. Women’s Benefits and Harms Trade-Offs in Breast Cancer Screening: Results from a Discrete-Choice Experiment. Value Health. 2018;21(1):78–88.
Hansen TB, Lindholt JS, Diederichsen A, Søgaard R. Do Non-participants at Screening have a Different Threshold for an Acceptable Benefit-Harm Ratio than Participants? Results of a Discrete Choice Experiment. Patient. 2019;12(5):491–501.
Sicsic J, Krucien N, Franc C. What are GPs’ preferences for financial and non-financial incentives in cancer screening? Evidence for breast, cervical, and colorectal cancers. Soc Sci Med. 2016;167:116–27.
Bilger M, Özdemir S, Finkelstein EA. Demand for Cancer Screening Services: Results From Randomized Controlled Discrete Choice Experiments. Value Health. 2020;23(9):1246–55.
Byrne MM, Thurer RJ, Studts JL. Individual decision making about lung cancer screening: A conjoint analysis of perspectives among a high-risk national sample. Cancer Med. 2019;8(12):5779–86.
Papin-Lefebvre F, Guillaume E, Moutel G, Launoy G, Berchi C. General practitioners’ preferences with regard to colorectal cancer screening organisation Colon cancer screening medico-legal aspects. Health Policy. 2017;121(10):1079–84.
Pignone MP, Crutchfield TM, Brown PM, Hawley ST, Laping JL, Lewis CL, et al. Using a discrete choice experiment to inform the design of programs to promote colon cancer screening for vulnerable populations in North Carolina. BMC Health Serv Res. 2014;14:611.
Raginel T, Grandazzi G, Launoy G, Trocmé M, Christophe V, Berchi C, et al. Social inequalities in cervical cancer screening: a discrete choice experiment among French general practitioners and gynaecologists. BMC Health Serv Res. 2020;20(1):693.
Snoswell CL, Whitty JA, Caffery LJ, Loescher LJ, Gillespie N, Janda M. Direct-to-consumer mobile teledermoscopy for skin cancer screening: Preliminary results demonstrating willingness-to-pay in Australia. J Telemed Telecare. 2018;24(10):683–9.
Mansfield C, Ekwueme DU, Tangka FKL, Brown DS, Smith JL, Guy GP, et al. Colorectal Cancer Screening: Preferences, Past Behavior, and Future Intentions. Patient. 2018;11(6):599–611.
Peters Y, van Grinsven E, van de Haterd M, van Lankveld D, Verbakel J, Siersema PD. Individuals’ Preferences for Esophageal Cancer Screening: A Discrete Choice Experiment. Value Health. 2020;23(8):1087–95.
Kitchener HC, Gittins M, Rivero-Arias O, Tsiachristas A, Cruickshank M, Gray A, et al. A cluster randomised trial of strategies to increase cervical screening uptake at first invitation (STRATEGIC). Health Technol Assess. 2016;20(68):1–138.
Norman R, Moorin R, Maxwell S, Robinson S, Brims F. Public Attitudes on Lung Cancer Screening and Radiation Risk: A Best-Worst Experiment. Value Health. 2020;23(4):495–505.
Priaulx J, Csanádi M, de Koning HJ, McKee M. A choice experiment to identify the most important elements of a successful cancer screening program according to those who research and manage such programs. Int J Health Plan Manag. 2019;34(1):e34-e45.
Li S, Liu S, Ratcliffe J, Gray A, Chen G. Preferences for cervical cancer screening service attributes in rural China: A discrete choice experiment. Patient Preference Adherence. 2019;13:881–9.
De Bekker-Grob EW, Rose JM, Donkers B, Essink-Bot ML, Bangma CH, Steyerberg EW. Men’s preferences for prostate cancer screening: A discrete choice experiment. Brit J Cancer. 2013;108(3):533–41.
de Bekker-Grob EW, Donkers B, Veldwijk J, Jonker MF, Buis S, Huisman J, et al. What Factors Influence Non-Participation Most in Colorectal Cancer Screening? A Discrete Choice Experiment. Patient - Patient-Centered Outcomes Res. 2021;14(2):269–81.
Peters Y, Siersema PD. Public Preferences and Predicted Uptake for Esophageal Cancer Screening Strategies: A Labeled Discrete Choice Experiment. Clin Transl Gastroenterol. 2020;11(11):e00260.
Charvin M, Launoy G, Berchi C. The effect of information on prostate cancer screening decision process: a discrete choice experiment. BMC Health Serv Res. 2020;20(1):467.
Howard K, Salkeld GP, Patel MI, Mann GJ, Pignone MP. Men’s preferences and trade-offs for prostate cancer screening: a discrete choice experiment. Health Expectations. 2015;18(6):3123–35.
Mandrik O, Yaumenenka A, Herrero R, Jonker MF. Population preferences for breast cancer screening policies: Discrete choice experiment in Belarus. PLoS ONE. 2019;14(11):e0224667.
Martens CE, Crutchfield TM, Laping JL, Perreras L, Reuland DS, Cubillos L, et al. Why Wait Until Our Community Gets Cancer?: Exploring CRC Screening Barriers and Facilitators in the Spanish-Speaking Community in North Carolina. J Cancer Educ. 2016;31(4):652–9.
Spinks J, Janda M, Soyer HP, Whitty JA. Consumer preferences for teledermoscopy screening to detect melanoma early. J Telemed Telecare. 2016;22(1):39–46.
Hendrix N, Hauber B, Lee CI, Bansal A, Veenstra DL. Artificial intelligence in breast cancer screening: primary care provider preferences. J Am Med Informatics Assoc. 2020;28(6):1117–24.
Benning TM, Dellaert BG, Severens JL, Dirksen CD. The effect of presenting information about invasive follow-up testing on individuals’ noninvasive colorectal cancer screening participation decision: results from a discrete choice experiment. Value Health. 2014;17(5):578–87.
Trapero-Bertran M, Rodríguez-Martín B, López-Bastida J. What attributes should be included in a discrete choice experiment related to health technologies? A systematic literature review. PloS one. 2019;14(7):e0219905.
Louviere JJ, Lancsar E. Choice experiments in health: the good, the bad, the ugly and toward a brighter future. Health Econ Policy Law. 2009;4(Pt 4):527–46.
Johnson FR, Hauber AB, Özdemir S, Lynd L. Quantifying women’s stated benefit-risk trade-off preferences for IBS treatment outcomes. Value Health. 2010;13(4):418–23.
Veldwijk J, Lambooij MS, De Bekker-Grob EW, Smit HA, De Wit GA. The effect of including an opt-out option in discrete choice experiments. PLoS ONE. 2014;9(11).
Marshall DA, Johnson FR, Kulin NA, Ozdemir S, Walsh JM, Marshall JK, et al. How do physician assessments of patient preferences for colorectal cancer screening tests differ from actual preferences? A comparison in Canada and the United States using a stated-choice survey. Health Econ. 2009;18(12):1420–39.
Hauber AB, González JM, Groothuis-Oudshoorn CG, Prior T, Marshall DA, Cunningham C, et al. Statistical methods for the analysis of discrete choice experiments: a report of the ISPOR conjoint analysis good research practices task force. Value Health. 2016;19(4):300–15.
McFadden D. Conditional logit analysis of qualitative choice behavior. 1973.
Fiebig DG, Keane MP, Louviere J, Wasi N. The generalized multinomial logit model: accounting for scale and coefficient heterogeneity. Market Sci. 2010;29(3):393–421.
Bridges JFP, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, et al. Conjoint Analysis Applications in Health—a Checklist: A Report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14(4):403–13.
de Bekker-Grob EW, Donkers B, Jonker MF, Stolk EA. Sample size requirements for discrete-choice experiments in healthcare: a practical guide. Patient-Patient-Centered Outcomes Res. 2015;8(5):373–84.
Rose JM, Bliemer MC. Sample size requirements for stated choice experiments. Transportation. 2013;40(5):1021–41.
Determann D, Lambooij MS, Steyerberg EW, de Bekker-Grob EW, De Wit GA. Impact of survey administration mode on the results of a health-related discrete choice experiment: online and paper comparison. Value Health. 2017;20(7):953–60.
Acknowledgements
Not applicable.
Funding
This study is part of a wider program of research which is funded by a competitive grant via the National Health and Medical Research Council’s Medical Research Future Fund, GNT1175567. The funder had no role in the design of the study and data collection, analysis and interpretation of results and in writing the manuscript or submitting for publication.
Author information
Authors and Affiliations
Contributions
Conception and design of work (DB, AJ, SK). Data collection (AJ, DB). Data analyses add interpretation (AJ, DB, SK). Drafting article (AJ, DB). Critical revision of the article (DB, SK, AJ). Final approval for publication (DB, AJ, SK).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Brain, D., Jadambaa, A. & Kularatna, S. Methodology to derive preference for health screening programmes using discrete choice experiments: a scoping review. BMC Health Serv Res 22, 1079 (2022). https://doi.org/10.1186/s12913-022-08464-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-08464-7