Abstract
Background
Hospitals are the biggest users of the health system budgets. Policymakers are interested in improving hospital efficiency while maintaining their performance during the economic crisis. This study aims at analysing the hospitals’ policy solutions during the economic crisis using the resilience system capacities framework.
Method
This study is a systematic review. The search strategy was implemented on the Web of Science, PubMed, Embase, Scopus databases, and Econbiz search portal. Data were extracted and analysed through the comparative table of resilience system capacities framework and the World Health Organization (WHO) health system’s six building blocks (i.e., leadership and governance, service delivery, health workforce, health systems financing, health information systems, and medicines and equipment).
Findings
After the screening, 78 studies across 36 countries were reviewed. The economic crisis and adopted policies had a destructive effect on hospital contribution in achieving Universal Health Coverage (UHC). The short-term absorptive capacity policies were the most frequent policies against the economic crisis. Moreover, the least frequent and most effective policies were adaptive policies. Transformative policies mainly focused on moving from hospital-based to integrated and community-based services. The strength of primary care and community-based services, types and combination of hospital financing systems, hospital performance before the crisis, hospital managers’ competencies, and regional, specialties, and ownership differences between hospitals can affect the nature and success of adopted policies.
Conclusion
The focus of countries on short-term policies and undermining necessary contextual factors, prioritizing efficiency over quality, and ignoring the interrelation of policies compromised hospital contribution in UHC.
Similar content being viewed by others
Introduction
Various factors can lead to an economic crisis. One of the most prominent of those was the financial crisis of 2007–2008 that affected a large number of developed countries [1]. This crisis began in the US due to excessive leverage and risky investments and spread worldwide [2]. Moreover, the economic crisis can result from wars, sanctions, climate change, or natural disasters. Similarly, the Corona Virus Disease of 2019 (COVID-19) has devastated the global economy [3]. The World Bank forecasts an almost 8% decrease in global growth and an enormous impact on low- and middle-income countries due to this pandemic [4]. Thus, more than ever, policymakers need to use the experience of previous economic crises.
The financial crisis affected the hospitals seriously [5, 6]. Also, hospitals that constitute one-third of health care expenditures are at the forefront of reforms for cost reduction [7]. Hence, the question is how to maintain hospital performance during the economic crisis and enhance hospital resilience against it. The term ‘resilience’ has gained popularity in recent years [8]. The concept of resilience generally refers to “the ability of an individual, household, community or an entire system to withstand the negative impact of shocks” (e.g., an economic crisis) [9].
There is no comprehensive, systematic study that analyzes hospital policies and their outcomes in countries that face an economic crisis within the resilience analysis framework. In this regard, Clemens et al. used document analysis to study hospital reforms in the EU member states during the financial crisis [10]. Thomas et al. examined the resilience of the Irish health system against economic crisis [11], and Alameddine et al. applied the Blanchet et al. resilience capacities framework [12] and Organization for Economic Co-operation and Development (OECD’s) resilience systems’ analysis guideline [13] to evaluate the resilience of health systems in Lebanon and Jordan in accommodating Syrian refugees [14].
The present research aims at identifying and analyzing various hospitals' policy solutions in each of the three resilience system capacities, the effects of these policies on hospital contribution to UHC, and the influential contextual factors in their implementation. Given that detailed information on the impact of interventions in the face of the economic crisis was not reported, we tried to reach a general conclusion based on the available qualitative information.
Theoretical framework
There are several frameworks for system resilience analysis. Some of them focused on resilient system capacities [12, 15]. Based on the definition by Organization for Economic Co-operation and Development (OECD), a resilient system is a system that can absorb and recover from shocks in the short term while positively adapting and transforming its structure in the long term to cope with changes and maintain its optimal performance [13, 16]. Therefore, the policies adopted in the face of crises divide into one of the following three categories:
-
(i)
Absorptive capacity: Policies seek continuity and maintenance of the health services level in terms of quality, quantity, and equity using available resources and keeping the current system’s structure and sustainability.
-
(ii)
Adoptive capacity: Policies that imply the system flexibility and make gradual changes in characteristics and activities to provide health services with fewer and different resources.
-
(iii)
Transformative capacity: Policies make principal reforms in functions and structure of the health system in response to change [12, 13, 16].
Methods
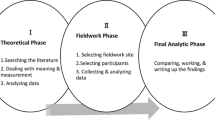
This study is a systematic review conducted based on Preferred Reporting Standards for Systematic Reviews 2020 (PRISMA 2020) [17]. It has three main sections. First, the study identifies the effects of the economic crisis on hospital contribution to UHC. Second, it analyzes the policies to deal with these effects. Finally, the study recognizes contextual factors that affect achieving hospital resilience against the economic crisis.
Eligibility criteria
We included studies published in English until March 1, 2022, with any research design (i.e., quantitative, qualitative, and mixed methods) as well as the grey literature such as research reports and dissertations.
Only publications focused on hospitals were included. In addition, studies included that investigated the effects of the economic crisis on hospitals, how hospitals dealt with the crisis and their policies, and the implications.
Studies published in languages other than English, studies that have examined the health system or one of its levels other than the hospital level, and studies that have examined clinical interventions in times of economic crisis were excluded. The reason for excluding studies that examine the entire health system from the screening was the large number of these studies and the time constraints of researchers. However, this limitation was overcome by reviewing comparative studies.
Information sources
The search strategy was conducted in Web of Science, PubMed, Embase, Scopus databases, and Econbiz search portal. Econbize is the search portal of economic and business literature that is provided by the German National Library of Economics, Leibniz Information Centre for Economics) to detect relevant studies. Moreover, Google Scholar and ProQuest were searched for grey literature, including reports and dissertations. Also, hand searching in related journals and reference checking of relevant studies were conducted.
Search strategy
Similar studies were used to detect relevant economic crisis keywords. The most specific and sensitive search strategies were selected by applying different search strategies with various combinations of terms in databases. Table 1 provides the PubMed search strategy as an example.
Selection process
Among retrieved studies, duplicates were removed using the Endnote software. Two researchers performed screenings. In the first stage, titles and abstracts of studies were examined based on their relevance. Then the studies’ full text is explored based on the eligibility criteria. The screening was conducted by two researchers separately, and controversies were discussed.
Data collection and synthesis methods
Hospital interventions in the face of the economic crisis were identified and analyzed through the comparative table of the resilience system capacities framework plus WHO’s health system building blocks. In this study, leadership and governance policies refer to rule-based policies (i.e., setting hospital policies, strategies, ownership arrangements, decentralization, stakeholder participation, and contextual factors) [18].
The outcome of program actions, influential contextual factors and studies recommendations were reached by content analysis of related data using MAXQDA 10 software.
Quality appraisal
Quality of studies assessed based on Mixed Methods Appraisal Tool (MMAT), VERSION2018, which is applicable for quality assessment of various methodologies (i.e., studies with qualitative, quantitative, and mixed-method designs) [19, 20]. Two researchers rated studies on a five-point scale: 0, 25, 50, 75, and 100 (highest level of quality). They resolved the disagreements through discussion and the use of a third researcher. Given that the present systematic review was qualitative, we didn’t exclude any study for having a low rating. However, studies with a higher-quality rating received a higher weight in analysis (i.e., any contradicted results of low-quality studies did not consider).
Results
The extraction table of study is presented in Additional file 1.
Study selection and characteristics
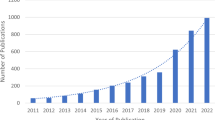
From a total of 5169 initially detected studies, after screening based on title and abstract,195 studies were examined based on eligibility criteria, of which 78 studies from 36 countries were selected for data extraction (Fig. 1). Among these countries, the highest number of studies belonged to the United States (28%), Greece (17%), Spain (15%) (Table 2).
Most of the studies (58%) were non-randomized or descriptive quantitative studies. Moreover, 24% of the studies were non-empirical, and one study was from grey literature.
Quality appraisal results
Additional file 1 present The quality appraisal results. Almost 58% of the studies had a high rate (100 or 75), and 9% had a medium rate, while only 4% of studies were in a low rating.
Impacts of economic crisis and adopted policies on achieving universal health coverage at hospital level
As the final goal of a resilient health system is to achieve UHC [97, 98], the impact of economic crisis and adopted policies were reviewed based on their contribution to UHC objectives, including equity in service use, quality, and financial protection [99].
Equity in service use
Economic crisis, decrease in household income, and insurance loss reduced hospital services utilization in several countries (Spain, Germany, Iran) [46, 47, 53,54,55,56,57]. Also, in the United States, preventable hospitalization decreased in vulnerable groups [24, 82]. Variously, it caused an increase in emergency, complicated and acute care utilization, especially in vulnerable groups (e.g., Spain and Finland) [34, 67]. Consequently, the inequity in access to hospital services increased (Spain, Germany) [24, 46, 47, 82], which highlights the impact of the crisis on the underserved population’s access to quality primary care [86].
Quality
During the economic crisis, hospitals focused on cost reduction and related structural reforms and neglected quality-related issues [30]. For example, the shortage of resources has led to a decline in evidence-based practice in hospitals [38, 75]. In addition, understaffing has led to poor quality and safety of care, patient dissatisfaction [38, 43, 48, 52], and a higher mortality rate [90], which is related to increasing staff workload and decreasing adequate skilled staff [23, 73].
Furthermore, the patient’s waiting time has increased and led to fatal delays and poor quality of care due to the lack of infrastructure, equipment, and medical supplies [28, 37, 59, 61, 75, 90]. For instance, the long waiting lists for surgeries increased patient dissatisfaction threefold in Southern Spain [67].
Financial protection
The economic crisis has reduced the available hospitals’ funds, including reimbursement rates, donations, and income (Greece and the US) [35, 79, 80]. Moreover, hospitals’ patient care losses increased due to the reduction in ambulatory care and elective surgeries [29, 60, 79, 85]. Furthermore income from non-patient care activities decreased after the economic crisis [79, 84]. All these factors increased out-of-pocket and informal payments. Policies and measures such as hospitals closure, admission of fewer patients with acute conditions by hospitals, limiting drug prescription, and patients being forced to supply consumables and drugs from outside the hospital have led to an indirect increase in patients’ financial burden [25, 26, 81].
The frequency of adopted policies based on health system building blocks and resilience capacities
As shown in Fig. 2, absorptive capacity policies are the most frequent policies. Most absorptive capacity policies involve service delivery (57% of countries have implemented such policies). Adaptive capacity policies are the least frequent ones that focus on financing policies (18%). Also, transformative capacity policies are used in service delivery reforms (45%).
Hospital policies against the economic crisis
The following section refers to various policies of countries in a comparative table of the resilience system capacities framework and the WHO health system’s six building blocks.
Absorptive capacity policies
Policies adopted to mitigate the impact of the economic crisis on the essential activities and critical hospital functions (absorptive capacity policies) have aimed to reduce inputs and investment in the health workforce, service delivery, financial resources, and drugs and medical equipment.
Generally, examining the impact and outcomes of these policies indicates a decline in quality, access, equity in service delivery, and greater reliance on informal and Out-Of-Pocket Payments (OOP) [37, 42, 63, 80].
Forty-five percent of countries adopted absorptive financing policies. Most of these countries adopted policies to decrease hospital budgets and payment rates. These policies contributed to an increase in OOP [34]. Only 21% of countries focused on reducing hospital expenditures and investments to save hospital funds (Table 3).
In this area, the researchers recommended adopting cost reduction policies in line with utilization [70]. In this regard, about hospital financing policies, some countries have made conscious cost reduction decisions. For example, the UK, Portugal, and Bulgaria adopted policies to reduce main cost groups such as consumables and administrative expenses [24, 30, 35, 39]. Similarly, a Greek study reports an increase in operating expenses following the economic crisis (i.e., overheads, consumables, and security costs [35]. In addition, in Spain, the main reason for increasing costs during the economic crisis was attributed to increased utilization, including hospitalization, surgical admissions, outpatient day-case surgeries, and less to the increase in quasi-prices, including average length of stay, staff-to-bed ratio, and hospital teaching capacity [23, 68, 69].
Concerning the health workforce, absorptive policies included:
-
a.
Reducing personnel payments (United States, UK, Slovenia, Denmark, Cyprus, Greece, Ireland, Romania, Spain, and Portugal) [5, 6, 10, 35, 77, 94],
-
b.
Reducing the number of staff through hiring freezes, layoffs, reduction in staffing positions, reduction in the rate of replacement, and redeploying human resources (United States, Greece, Spain, Denmark, France, Portugal) [5, 6, 10, 27, 39, 71, 78, 79, 85].
-
c.
Employing less skilled or unskilled personnel (Netherlands, UK, Slovakia, United States) [5, 6, 10, 35].
These policies have led to a decline in the quantity and quality of hospital staff [37, 42, 63, 80]. In this regard, to mitigate the impact of austerity policies, studies recommended an increase in the human resources quality, improvement of working conditions, and employee motivation [26, 28, 35, 43, 68, 69, 80]. For example, in Spain, reducing the staff wages and salaries and increasing taxes and working hours have reported no negative impact on clinical personnel because of autonomy in the workplace and other working conditions [68, 69]. Also, the results of a US study indicated that highly distressed organizations could serve to motivate employees through group dynamics [91].
Most countries adopted explicit and implicit rationing in service delivery policies. For example, increasing waiting time, introducing or increasing co-payments, reducing patient access, and increasing out-of-pocket payments [34, 35, 41, 75]. However, the results of some studies showed the effectiveness of these policies in countries that strengthened other service delivery methods, including primary care and community-based facilities. For instance, introducing co-payments for emergency department visits in Cyprus reduced avoidable admissions but did not affect unavoidable emergency admissions. Strengthening primary care and community-based facilities in this country was the main reason [50]. Table 4 provides the other absorptive service delivery policies.
Absorptive drugs and medical equipment policies are in two category of supply-side and demand-side policies. About the supply-side policies, some countries adopted policies to reduce drugs price.
Austria, Spain, and the Ireland reduced the price through negotiations and long-term contracts [10]. Also, Belgium introduced a new reimbursement mechanism [10]. Additionally, Malta and Slovakia determine reference price systems for the price reduction [10]. Also, Belgium introduced a new reimbursement mechanism [10]. Additionally, Malta and Slovakia determine reference price systems for the price reduction [10]. Further, countries reduced the use of brand-name drugs and increased the use of generic drugs (Greece, France, Hungary, and the Czech Republic) [10, 39, 44, 80]. Moreover, Greece applied international E-auction [39], and the Czech Republic introduced the auction for drugs and equipment procurement [10].
Demand-side policies concentrated on Reduction in prescription prices (Portugal, Slovenia, Catalonia, Greece, Spain, and Poland) [26, 39, 45], reducing the use of drugs (United States) [80], and Postpone & Reduction of investments for new technologies (United States, Spain) [71, 80].
A limited number of countries implemented absorptive governance and leadership policies. These countries focused on changing the behavior of service providers and patients by applying incentives and regulations (Cuba, United States) [28, 77]. Also, the stakeholders’ support is gained by involving them in decision-making (United States, Norway, Portugal) [30, 88].
Adaptive capacity policies
In general, adaptive capacity policies included strengthening and adjusting infrastructure through medium-term changes and contributed to the maintenance and improvement of hospital performance in different building blocks. Meanwhile, a Greek study showed that almost all productivity gains were due to technology changes, including applying new methodologies, procedures, and techniques. Thus, studies recommended the utilization and promotion of organizational and managerial reforms [44].
Regarding Governance and Leadership, Cuba, Greece, and Denmark have revised and promoted the clinical processes, guidelines, and hospital policies [10, 28, 35, 44].
Indeed, developing and promoting appropriate policies, guidelines, and regulations are necessary for the prevention of corruption and to manage the diagnostic and treatment choices of physicians [26, 41, 85, 89]. A study in Greece showed that the economic crisis could shift the selection of the surgical technique toward less costly protocols [40]. On the other hand, a US study showed that doctors who had a closer tie to the hospital (e.g., employment) increased their treatment intensity, especially for patients with private insurance [92].
Besides, in governance and leadership, studies highlighted the importance of developing mechanisms for controlling and monitoring performance [22, 26, 88, 89], which is highlighted in the policies of Cuba and Tanzania by promoting financial control and departmental and personnel evaluation systems [28, 75].
Regarding service delivery, only two countries had strategies for enhancing the efficiency of service delivery. These policies have been adopted as solutions that led to using less expensive services (Denmark, Cuba) [10, 28].
Adaptive financing policies were introduced in a limited number of countries, focusing on aligning payments to patient outcomes (Table 5). In this domain, only the United States applied revenue-generating policies [82, 83].
Only Greece, Cuba, and Tanzania applied policies in the area of Information systems [28, 45, 75]. These policies were creating and improving the quality of monitoring and controlling hospital financial systems.
Human resource policies are limited to Cuba and Costa Rica [27, 28]. These countries improve personnel efficiency through conducting training programs and evaluation systems.
Transformative capacity policies
In terms of transformative capacity, countries have used various mechanisms in governance and leadership, health systems financing, and service delivery domains with a specific focus on transforming service delivery.
On this subject, some of the studies’ recommendations were strengthening the primary care system, restructuring emergency units and creating autonomous emergency departments, and integrating care [5, 10, 28, 29, 39, 41, 67].
In this regard, some countries created new governance and leadership structures to coordinate and manage primary care and hospital services (Greece, US) [41, 44, 45, 86]. Also, several countries conducted hospital integration or closure to reduce hospital care utilization (United States, Canada, Greece, Denmark, Spain) [6, 10, 25, 32, 35, 39, 44, 71, 76, 80, 81, 87].
In addition, there is a necessity to rationalize the payment mechanisms to reflect the exact costs of services [10, 26, 41]. For this purpose, Greece, Portugal, Bulgaria, the Czech Republic, and Cyprus have noted reforms in their payment systems and the shifting from retrospective to prospective payment systems and from cost-based to case-based payment systems [10, 39, 44, 45, 65].
However, the policymakers must consider the effects of cost reduction policies on the patients’ psychosocial wellbeing and access. For example, hospital closure can lead to unemployment, loss of physicians, transportation costs, fear of being hospitalized in other cities, and reduced access to services [25, 44, 81, 88].
Contextual factors that affect on achieving hospital resilience
Underlying factors that affect on hospital resilience to economic crisis can be examined in six categories, including:
-
A.
Strong primary care and community-based services
A study in Cuba showed that a powerful first line and a family physician system could prevent excessive load on hospitals, making them a place only for the service provided to patients with acute diseases at the second line [28]. Also, appropriate primary care facilities in rural regions of Greece led to lower vulnerability in these regions comparing the urban and suburban areas [5, 36]. In the UK, the transfer of outpatient and ambulatory care into community settings slowed down the increase rate in emergency hospital admissions [32]. However, it didn’t show a significant relationship between social care provision and emergency hospital admissions, which was attributed to ineffective community care [33]. Similarly, a US study showed that the establishment of urgent care centers outside of the hospitals reduced the patients access to Medicare and Medicaid, increased geographical inequalities, and led to the growth of the for-profit health sector due to the lack of proper regulations [81].
-
B.
Hospital financing system
Access to different payment plans [76, 81, 82], lower dependence on non-patient care income, lower need for charity and community-based care, membership of for-profit hospitals in hospital systems, and having a supportive network [76, 95] can make hospitals more resistant against the economic shocks. Contrary, relying on weak insurance funds and the inflexibility of service tariffs has increased the vulnerability of hospitals to the economic crisis [58].
-
C.
Hospital performance before the crisis
Hospitals with lower levels of efficiency before the economic crisis [21] and larger hospitals [39] have achieved more in terms of efficiency and productivity by applying relevant policies. On the other hand, patient-related outcomes (patient safety indicators) in hospitals with better financial performance before the economic crisis have improved post-crisis due to the financial constraints effects [92].
-
D.
Hospital’s ownership and region
After the economic crisis, public and private hospitals have not responded differently to budget constraints [21]. Also, in Greece, the effects of economic crisis were more significant on urban and suburban hospitals comparing rural hospitals [5, 36]. In the same vein, a study in the US showed that being private or public, is located in urban or rural areas, and profitability and financial performance affect a hospital’s quality of care during an economic crisis [80]. In Iran, public hospitals were less vulnerable to the economic crisis [58]. In addition, a study in Spain revealed that public-private partnerships are more resilient against the economic crisis than public and private hospitals [74].
-
E.
Hospital management competencies
Hospital management’s competence in addressing internal and external demands and the information and communication network within hospitals affect their response to the economic crisis [75]. Studies referred to the capacity to manage actors and network interconnectedness as the main factor for improving resilience [23].
-
F.
Hospital specialties
Differences among hospital departments and specialties also moderate the impact of the economic crisis. For example, evidence shows that the economic crisis increased cardiovascular and psychosomatic diseases and suicide attempts while reducing pregnancy and fetal health [36, 39, 67]. In addition, personnel in different departments have shown different levels of vulnerability. For example, a study in Italy found that surgery ward personnel are more at risk of exhibiting symptoms of depression and burnout compared to laboratory personnel [64].
Discussion
Hospitals are consumers of the majority of health system resources. Therefore, policymakers are interested to know how to deal with hospital policies during an economic crisis. The economic crisis can be a window of opportunity to improve hospitals’ performance in different countries by making resilience. The resilience term raises in the face of various crises and shocks. It is the system viability at the same or a higher level as before the shock. Strategies used in response to a shock can be absorptive (buffering the system from shocks with little or no change in structure), adaptive (limited adjustments in the system structure or processes), or transformative (significant functional or structural change) [100].
The present study sought to identify different countries’ solutions in the face of economic crisis and analyze them within the resilience system capacities framework. For this purpose, the impacts of the economic crisis and adopted policies were examined to identify measures for enhancing hospital resilience against the economic crisis and provide insights and directions for health policymakers. Figure 3 summarizes the study findings and recommendations to improve hospital resilience in the economic crisis.
Studies indicated the focus of hospitals on short-term, absorptive measures. As such, failure to identify the root cause of increased hospital costs and failure to make evidence-based cost reduction decisions compromised service quality, access, and fair financial contribution. Moreover, the least frequent policies were adaptive policies, which could play the most significant role in improving hospital performance.
A few countries began reforms in service delivery by moving toward the provision of integrated care and reducing the delivery of hospital services while developing primary care and community-based outpatient care.
Considering the interrelations and the mutual effect of different policies on each other as well as relevant contextual factors is necessary when analyzing the results of this study.
Regarding policies’ interrelations, it is noteworthy that the effects of cost reduction policies on other goals and policies must be considered [101]. A functional cost-containment policy can lead to a decline in the quality of care [26]. For example, hospital restructuring and downsizing policies can create poor working conditions and generate mistrust in the personnel. Personnel dissatisfaction will lead to the provision of low-quality care [37, 42, 64, 68, 77, 78].
Concerning the effect of contextual factors, in the present study, 28% of the reviewed studies are related to the US, which is a federal system where a significant part of the health system follows federal rules and is administered by the private sector with very little public sector participation [102]. Moreover, 17% of the articles are related to Greece, with a highly centralized health system comprising both the public (the National Health System) and the private sector [103]. For instance, a decrease in elective and preventable emergency care services has been observed in countries with a national health system and social insurance such as (e.g., the UK) [10, 27, 29, 32]. On the contrary, various states across the US declined non-profit services and emergency care with low reimbursement [80, 93, 94]. In response to the economic crisis, some countries such as the US resort to public-private partnerships (PPPs) [87], while others such as the UK choose to terminate PPPs contracts.
In addition, the economic crisis and the policies adopted to counter it have had different impacts on different countries. For example, US studies have noted a reduction in efficiency [79, 82], while Greek studies have reported increasing efficiency [35, 39, 44]. This may be due to differences in their financial resource and revenue generation mechanisms since US hospitals are more dependent on non-patient care revenues.
The present study also showed that most countries adopted short-term absorptive policies. These results are in accordance with the study of Clemens et al. that indicates the tendency of countries to make short-term and quick changes to reduce costs, a small number of studies have mentioned structural reforms and integration of care in response to the economic crisis [104]. This may be because most of them are developed countries with appropriate health service infrastructures and less need for structural reforms. For example, implementing the policy of ambulatory and avoidable emergency service reductions requires a powerful and effective primary health care system and community-based services; otherwise, it will lead to increased inequity and reduce patients’ access.
Generally, countries have strived to reduce costs and increase efficiency in each of the three resilience capacities, i.e., absorptive, adaptive, and transformative capacities. However, it has endangered their universal health coverage. Notably, addressing the needs of the covered society and quality care provision takes precedence over financial and cost-saving issues, and improvement of the quality and safety of essential care must continue throughout the economic crisis [26, 38, 39, 65, 95].
In terms of the health system building blocks, the greatest focus was on service delivery and health system financing policies. Also, the governance and leadership and the health information system have the lowest frequency of policies. However, all the health system building blocks are interrelated and should not be considered in isolation [105]. The results of a comparative analysis of hospital reforms in 11 Central and Eastern European Countries between 2008 and 2019 showed that most of these countries had engaged in governance reforms to reduce hospital capacities, purchasing and payment reforms to limit hospital expenditures and to shift service provision to ambulatory care, and all of the countries pursued the objective of reducing the number of hospital beds [104].
The present study has two limitations. The first is in method and inclusion criteria. Studies only were included if they were related to the hospital area. The large number of studies on health systems against the economic crisis and the time constraint of researchers prevented the inclusion of these studies. This could lead to the loss of several hospital-related information in these studies. To overcome this limitation, we included existing comparative studies in this area.
The second limitation concerns the interpretation of the results. Studies didn’t have enough accurate information about the effects of hospital interventions against the economic crisis. Hence, it is not possible to conclude certainly about the impact of the adopted policies. However, we extracted any related data on the effects of policies and concluded based on the frequency of mentioned effects.
Future quantitative and qualitative studies should examine the long-term impacts of any adopted policies on the health system building blocks separately. In this case, a reasonable number of studies can be included in the study. Also, the impacts of each policy will be determined with more confidence.
Conclusion
The present study was designed to analyze hospital resilience in economic crisis using the resilience system capacities framework. It is hoped that this study could provide a holistic view for policymakers in different countries to choose appropriate policies recognizing different policy options (including absorptive, adaptive, and transformative policies) in each health system six building blocks, and probable consequences on hospital resilience considering contextual factors.
The analysis indicated the importance of considering contextual factors as well as the health system maturity in choosing appropriate policies to improve hospital resilience against the economic crisis. Also, it is necessary to consider the interrelation of the health system’s six building blocks and the effects of policies on each other.
In other words, the focus of countries on short-term absorptive measures without considering related influential contextual factors leads to jeopardizing the UHC. This study highlighted the effects of the strength of primary care and community-based services, hospital managers’ competencies, types and combinations of hospital financing, hospital performance before the crisis, and regional, specialties, and ownership differences between hospitals can affect the effectiveness of adopted policies.
Overall, the study showed that a resilient hospital against the economic crisis is a hospital that has policies to reduce costs and increase efficiency whiteout disturbing the hospital performance in three main building blocks (service delivery, financing, and human resources).
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
- COVID-19:
-
Corona Virus Disease of 2019
- OECD:
-
Organization for Economic Co-operation and Development
- WHO:
-
World Health Organization
- UHC:
-
Universal Health Coverage
- OOP:
-
Out of Pocket payment
References
International Monetary Fund. World Economic Outlook, April 2009: crisis and recovery: International Monetary Fund; 2009.
O'Riordan M, Fitzpatrick F. The impact of economic recession on infection prevention and control. J Hosp Infect. 2015;89(4):340–5.
Goodell JW. COVID-19 and finance: agendas for future research. Financ Res Lett. 2020;35:101512.
Kaye AD, Okeagu CN, Pham AD, Silva RA, Hurley JJ, Arron BL, et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: International perspectives. Best Pract Res Clin Anaesthesiol. 2021;35(3):293-306.
Koutserimpas C, Agouridakis P, Velimezis G, Papagiannakis G, Keramidis I, Ioannidis A, et al. The burden on public emergency departments during the economic crisis years in Greece: a two-center comparative study. Public Health. 2019;167:16–20.
Kalafati M. How Greek healthcare services are affected by the euro crisis. Emergency Nurse. 2012;20(3):26.
Blank JL, Eggink E. The impact of policy on hospital productivity: a time series analysis of Dutch hospitals. Health Care Manag Sci. 2014;17(2):139–49.
Sturmberg JP. Resilience for health—an emergent property of the “health systems as a whole”. J Eval Clin Pract. 2018;24(6):1323–9.
Gordeev VS, Goryakin Y, McKee M, Stuckler D, Roberts B. Economic shocks and health resilience: lessons from the Russian Federation. J Public Health. 2016;38(4):e409–e18.
Clemens T, Michelsen K, Commers M, Garel P, Dowdeswell B, Brand H. European hospital reforms in times of crisis: aligning cost containment needs with plans for structural redesign? Health Policy. 2014;117(1):6–14.
Thomas S, Keegan C, Barry S, Layte R, Jowett M, Normand C. A framework for assessing health system resilience in an economic crisis: Ireland as a test case. BMC Health Serv Res. 2013;13:450.
Blanchet K, Nam SL, Ramalingam B, Pozo-Martin F. Governance and capacity to manage resilience of health systems: towards a new conceptual framework. Int J Health Policy Manag. 2017;6(8):431.
OECD. Guidelines for resilience system analysis: OECD Publishing; 2014.
Alameddine M, Fouad FM, Diaconu K, Jamal Z, Lough G, Witter S, et al. Resilience capacities of health systems: accommodating the needs of Palestinian refugees from Syria. Soc Sci Med. 2019;220:22–30.
Gilson L, Barasa E, Nxumalo N, Cleary S, Goudge J, Molyneux S, et al. Everyday resilience in district health systems: emerging insights from the front lines in Kenya and South Africa. BMJ Glob Health. 2017;2(2):e000224.
Mitchell A. Risk and Resilience; 2013.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
World Health Organization. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies: World Health Organization; 2010.
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34(4):285–91.
Pace R, Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, et al. Testing the reliability and efficiency of the pilot mixed methods appraisal tool (MMAT) for systematic mixed studies review. Int J Nurs Stud. 2012;49(1):47–53.
Berger M, Sommersguter-Reichmann M, Czypionka T. Determinants of soft budget constraints: how public debt affects hospital performance in Austria. Soc Sci Med. 2020;249:112855.
Martins M, Lima SML, Andrade CLT, Portela MC. Access and effectiveness inpatient care indicators and economic crisis: analysis based on the Brazilian Unified Health System data, Brazil and Southern Brazil states, 2009–2018. Cien Saude Colet. 2019;24:4541–54.
Fana T, Goudge J. Austerity, resilience and the management of actors in public hospitals: a qualitative study from South Africa. BMJ Glob Health. 2021;6(2):e004157.
Vaseva V, Voynov L, Donchev T, Popov R, Mutafchiyski V, Aleksiev L, et al. Outcomes analysis of hospital management model in restricted budget conditions. Biotechnol Biotechnol Equip. 2016;30(2):411–7.
James AM. Closing rural hospitals in Saskatchewan: on the road to wellness? Soc Sci Med. 1999;49(8):1021–34.
Yan J, Lin H-H, Zhao D, Hu Y, Shao R. China’s new policy for healthcare cost-control based on global budget: a survey of 110 clinicians in hospitals. BMC Health Serv Res. 2019;19(1):84.
Boddiger D. Costa Rica restructures health system to curb financial crisis. Lancet. 2012;379(9819):883.
De Vos P, Orduñez-García P, Santos-Peña M, Van der Stuyft P. Public hospital management in times of crisis: lessons learned from Cienfuegos, Cuba (1996–2008). Health Policy. 2010;96(1):64–71.
Petrou P, Ingleby D. Co-payments for emergency department visits: a quasi-experimental study. Public Health. 2019;169:50–8.
Burnett S, Mendel P, Nunes F, Wiig S, van den Bovenkamp H, Karltun A, et al. Using institutional theory to analyse hospital responses to external demands for finance and quality in five European countries. J Health Serv Res Policy. 2016;21(2):109–17.
Hellowell M, Stafford A, Stapleton P. Austerity and hospitals in deficit: is PPP termination the answer? Abacus. 2019;55(3):535–56.
Lewis RQ. More reform of the English National Health Service: from competition back to planning? Int J Health Serv. 2019;49(1):5–16.
Seamer P, Brake S, Moore P, Mohammed MA, Wyatt S. Did government spending cuts to social care for older people lead to an increase in emergency hospital admissions? An ecological study, England 2005–2016. BMJ Open. 2019;9(4):e024577.
Keskimäki I. How did Finland's economic recession in the early 1990s affect socio-economic equity in the use of hospital care? Soc Sci Med. 2003;56(7):1517–30.
Kaitelidou D, Katharaki M, Kalogeropoulou M, Economou C, Siskou O, Souliotis K, et al. The impact of economic crisis to hospital sector and the efficiency of Greek public hospitals. EJBSS. 2016;4:111–25.
Gkentzi D, Katsoula V, Fouzas S, Mentis M, Karatza A, Dimitriou G. Economic recession and attendances in the pediatric emergency department. Biomed Res Int. 2019;2019:4186486.
Karamanoli E. 5 years of austerity takes its toll on Greek health care. Lancet. 2015;386(10010):2239–40.
Keramidou I, Triantafyllopoulos L. The impact of the financial crisis and austerity policies on the service quality of public hospitals in Greece. Health Policy. 2018;122(4):352–8.
Mitropoulos P, Mitropoulos I, Karanikas H, Polyzos N. The impact of economic crisis on the Greek hospitals' productivity. Int J Health Plann Manag. 2018;33(1):171–84.
Schizas D, Michalinos A, Kanavidis P, Karaolanis G, Lidoriki I, Sioulas AD, et al. The profile of patients receiving public and private surgical services in Greece during the economic crisis: a comparative study. Ann Transl Med. 2019;7(1):5.
Souliotis K, Golna C, Tountas Y, Siskou O, Kaitelidou D, Liaropoulos L. Informal payments in the Greek health sector amid the financial crisis: old habits die last. Eur J Health Econ. 2016;17(2):159–70.
Spiridakis K, Gionis I, Sfakianakis E, Flamourakis M, Rahmanis E, Vrenzos N, et al. Impact of financial crisis on the workload, training, personal and social life of the residents in surgical specialties in Greece (first results). Chirurgia. 2015;28:1–2.
Stavrianou A, Kafkia T, Mantoudi A, Minasidou E, Konstantinidou A, Sapountzi-Krepia D, et al. Informal caregivers in Greek hospitals: a unique phenomenon of a health system in financial crisis. Mater Sociomed. 2018;30(2):147.
Xenos P, Yfantopoulos J, Nektarios M, Polyzos N, Tinios P, Constantopoulos A. Efficiency and productivity assessment of public hospitals in Greece during the crisis period 2009–2012. Cost Eff Resour Alloc. 2017;15(1):6.
Polyzos N, Karanikas H, Thireos E, Kastanioti C, Kontodimopoulos N. Reforming reimbursement of public hospitals in Greece during the economic crisis: implementation of a DRG system. Health Policy. 2013;109(1):14–22.
Moreno A, Lostao L, Beller J, Sperlich S, Ronda E, Geyer S, et al. Trends and equity in the use of health services in Spain and Germany around austerity in Europe. Int J Equity Health. 2021;20(1):1–10.
Lostao L, Geyer S, Albaladejo R, Moreno-Lostao A, Santos JM, Regidor E. Socioeconomic position and health services use in Germany and Spain during the great recession. PLoS One. 2017;12(8):e0183325.
Gorji A. Sanctions against Iran: the impact on health services; 2014.
Murphy A, Abdi Z, Harirchi I, McKee M, Ahmadnezhad E. Economic sanctions and Iran’s capacity to respond to COVID-19. Lancet Public Health. 2020;5(5):e254.
Shahabi S, Teymourlouy AA, Shabaninejad H, Kamali M, Lankarani KB, Mojgani P. Physical rehabilitation in Iran after international sanctions: explored findings from a qualitative study. Glob Health. 2020;16:86.
Tabrizi A. Impact of economic sanctions on orthopedic residency program (education & training). Stud Med Sci. 2019;30(6):513–4.
Abdoli A. Iran, sanctions, and the COVID-19 crisis. J Med Econ. 2020;23(12):1461–5.
Rad EH, Delavari S, Aeenparast A, Afkar A, Farzadi F, Maftoon F. Does economic instability affect healthcare provision? Evidence based on the urban family physician program in Iran. Korean J Fam Med. 2017;38(5):296.
Danaei G, Harirchi I, Sajadi HS, Yahyaei F, Majdzadeh R. The harsh effects of sanctions on Iranian health. Lancet. 2019;394(10197):468–9.
Yazdi-Feyzabadi V, Amini-Rarani M, Delavari S. The health consequences of economic sanctions: call for health diplomacy and international collaboration. Arch Iran Med. 2020;23(4Suppl1):S51.
Aloosh M, Salavati A, Aloosh A. Economic sanctions threaten population health: the case of Iran. Public Health. 2019;169:10–3.
Kokabisaghi F, Miller AC, Bashar FR, Salesi M, Zarchi AA, Keramatfar A, et al. Impact of United States political sanctions on international collaborations and research in Iran. BMJ Glob Health. 2019;4(5):e001692.
Nasiri T, Shams L, Hosseini-Shokouh SM. The economic effects of COVID-19 on the hospital industry in Iran and the world. Ann Ig. 2021;33(1):103–4.
Taslimi MS, Azimi A, Nazari M. Resilience to economic sanctions; case study: hospital equipment cluster of Tehran (HECT). Int J Disast Resil Built Environ. 2020;12:13–28.
Rawaf S. The health crisis in Iraq. Crit Public Health. 2005;15(2):181–8.
Garfield R, Dresden E, Boyle JS. Health care in Iraq. Nurs Outlook. 2003;51(4):171–7.
Kiernan F. Public policy failure in healthcare: the effect of salary reduction for new entrant consultants on recruitment in public hospitals. Administration. 2019;67(2):95–112.
Carr M, Beck MP. Clinician responses to management control: Case evidence from a university hospital during the fiscal crisis. Financ Account Manage. 2020;36(3):319-37.
Carta M, Preti A, Portoghese I, Pisanu E, Moro D, Pintus M, et al. Risk for depression, burnout and low quality of life among personnel of a university hospital in Italy is a consequence of the impact one economic crisis in the welfare system? Clin Pract Epidemiol Ment Health. 2017;13:156.
Perelman J, Felix S, Santana R. The great recession in Portugal: impact on hospital care use. Health Policy. 2015;119(3):307–15.
Abásolo I, Saez M, López-Casasnovas G. Financial crisis and income-related inequalities in the universal provision of a public service: the case of healthcare in Spain. Int J Equity Health. 2017;16(1):134.
Córdoba-Doña JA, Escolar-Pujolar A, San Sebastián M, Gustafsson PE. Withstanding austerity: equity in health services utilisation in the first stage of the economic recession in southern Spain. PLoS One. 2018;13(3):e0195293.
Esteban-Sepúlveda S, Moreno-Casbas MT, Fuentelsaz-Gallego C, Ruzafa-Martinez M. The nurse work environment in Spanish nurses following an economic recession: from 2009 to 2014. J Nurs Manag. 2019;27(6):1294–303.
Fontova-Almató A, Suñer-Soler R, Salleras-Duran L, Bertran-Noguer C, Congost-Devesa L, Ferrer-Padrosa M, et al. Evolution of job satisfaction and burnout levels of emergency department professionals during a period of economic recession. Int J Environ Res Public Health. 2020;17(3):921.
Bernal-Delgado E, Comendeiro-Maaløe M, Ridao-López M, Rosselló AS. Factors underlying the growth of hospital expenditure in Spain in a period of unexpected economic shocks: a dynamic analysis on administrative data. Health Policy. 2020;124:389–96.
Borra C, Pons-Pons J, Vilar-Rodriguez M. Austerity, healthcare provision, and health outcomes in Spain. Eur J Health Econ. 2020;21(3):409-23.
Sánchez‐Recio R, Alonso JP, Gil‐Lacruz A, Aguilar‐Palacio I. Inequities in hospitalisation in a South European country: Lessons learned from the last European recession. Health Soc Care Community. 2022;30(4):e1170-82.
Manzano García G, Montañés Muro MP, López MJ. Does the economic crisis contribute to the burnout and engagement of Spanish nurses? Curr Psychol. 2021:1–8.
Ortega-Díaz M, Ocaña-Riola R, Pérez-Romero C, Martín-Martín JJ. Multilevel analysis of the relationship between ownership structure and technical efficiency frontier in the Spanish National Health System Hospitals. Int J Environ Res Public Health. 2020;17(16):5905.
Strong AE. Working in scarcity: effects on social interactions and biomedical care in a Tanzanian hospital. Soc Sci Med. 2017;187:217–24.
Bazzoli GJ, Fareed N, Waters TM. Hospital financial performance in the recent recession and implications for institutions that remain financially weak. Health Aff. 2014;33(5):739–45.
Burke RJ, Ng ES, Wolpin J. Economic austerity and healthcare restructuring: correlates and consequences of nursing job insecurity. Int J Hum Resour Manag. 2015;26(5):640–56.
Burke RJ, Ng EW, Wolpin J. Hospital restructuring and downsizing: effects on nursing staff well-being and perceived hospital functioning. Eur J Psychol. 2011;7(1):81–98.
Chen Y, Wang J, Zhu J, Sherman HD, Chou S-Y. How the great recession affects performance: a case of Pennsylvania hospitals using DEA. Ann Oper Res. 2019;278(1–2):77–99.
Dong GN. Performing well in financial management and quality of care: evidence from hospital process measures for treatment of cardiovascular disease. BMC Health Serv Res. 2015;15(1):45.
Henry C. Hospital closures: the sociospatial restructuring of labor and health care. Ann Assoc Am Geogr. 2015;105(5):1094–110.
Izon GM, Pardini CA. A Stochastic Frontier Analysis of California Safety-Net Hospital Cost Inefficiency through the Great Recession. J Health Care Finance. 2015;42(2):2-21.
Izón GM, Pardini CA. Cost inefficiency under financial strain: a stochastic frontier analysis of hospitals in Washington state through the great recession. Health Care Manag Sci. 2017;20(2):232–45.
Schuhmann TM. Can net income from non-patient-care activities continue to save hospitals? The times when hospitals could rely on non-patient-care activities to offset losses on patient care may be over. Healthcare reform and economic conditions may soon force hospitals to look for ways to deliver high-quality care profitably, despite constrained reimbursement. Healthc Financ Manage. 2010;64(5):74–83.
Shortt J. A historical perspective of the effect of the great recession on hospitals. AORN J. 2014;100(2):177–87.
White B, Ellis C, Jones W, Moran W, Simpson K. The effect of the global financial crisis on preventable hospitalizations among the homeless in New York state. J Health Serv Res Policy. 2018;23(2):80–6.
Berliner HS. The crisis of the Los Angeles County public hospital system: a harbinger for the nation. Int J Health Serv. 2004;34(2):313–22.
Bledsoe DN, Sullivan D, Mathias D. Human capital and process improvement. Nurs Manag. 2012;43(1):46–53.
Stewart LJ, Smith PC. An examination of contemporary financing practices and the global financial crisis on nonprofit multi-hospital health systems. J Health Care Finance. 2011;37(3):1.
Lee J. The impact of financial crisis on the financial asset in California hospitals. Korea World Econ. 2015;16(1):151–65.
Boakye KG, Apenteng BA, Hanna MD, Kimsey L, Mase WA, Opoku ST, Owens C, Peden A. The impact of interpersonal support, supervisory support, and employee engagement on employee turnover intentions: Differences between financially distressed and highly financially distressed hospitals. Health Care Manage Rev. 2021;46(2):135-44.
Adelino M, Lewellen K, McCartney WB. Hospital financial health and clinical choices: evidence from the financial crisis. 2019. Available at SSRN 3224667.
Choi S. Hospital capital investment during the great recession. Inquiry. 2017;54:0046958017708399.
Sussman JB, Halasyamani LK, Davis MM. Hospitals during recession and recovery: vulnerable institutions and quality at risk. J Hosp Med. 2010;5(5):302–5.
Fingar KR, Coffey RM, Mulcahy AW, Andrews RM, Stocks C. Shifts in Medicaid and uninsured payer mix at safety-net and non-safety-net hospitals during the great recession. J Healthc Manag. 2018;63(3):156–72.
Craig J, Koleda M. The urban fiscal crisis in the United States, National Health Insurance, and municipal hospitals. Int J Health Serv. 1978;8(2):329–49.
Abiiro GA, De Allegri M. Universal health coverage from multiple perspectives: a synthesis of conceptual literature and global debates. BMC Int Health Hum Rights. 2015;15(1):1–7.
Tumusiime P, Nabyonga-Orem J, Karamagi H, Lehmann U, Elongo T, Nikiema J-B, et al. Resilient health systems for attaining universal health coverage. BMJ Glob Health. 2019;4:e002006.
Kutzin J, Sparkes SP. Health systems strengthening, universal health coverage, health security and resilience. Bull World Health Organ. 2016;94(1):2.
Kagwanja N, Waithaka D, Nzinga J, Tsofa B, Boga M, Leli H, et al. Shocks, stress and everyday health system resilience: experiences from the Kenyan coast. Health Policy Plan. 2020;35(5):522–35.
Stadhouders N, Kruse F, Tanke M, Koolman X, Jeurissen P. Effective healthcare cost-containment policies: a systematic review. Health Policy. 2019;123(1):71–9.
Rice T, Rosenau P, Unruh L, Barnes A, Saltman R, Van Ginneken E. United state of America: health system review; 2013.
Economou C. Greece: Health system review 2010.
Dubas-Jakóbczyk K, Albreht T, Behmane D, Bryndova L, Dimova A, Džakula A, et al. Hospital reforms in 11 central and eastern European countries between 2008 and 2019: a comparative analysis. Health Policy. 2020;124:368–79.
Biddle L, Wahedi K, Bozorgmehr K. Health system resilience: a literature review of empirical research. Health Policy Plan. 2020;35(8):1084-1109. https://doi.org/10.1093/heapol/czaa032.
Acknowledgements
The authors would like to acknowledge the support of Iran university of medical sciences.
Funding
This study was part of a PhD thesis supported by the School of Health Management and Information Sciences, Iran University of Medical Sciences, Iran (IUMS/SHMIS_1397-3-37-12709).
Author information
Authors and Affiliations
Contributions
ZF: Conceptualization, Methodology, Writing - Original Draft PE: Project administration, Supervision, Validation AA: Writing - Review & Editing MM: Writing - Review & Editing ShY: Conceptualization, Methodology. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Financial competing interests: non
Non-financial competing interest: non
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Foroughi, Z., Ebrahimi, P., Aryankhesal, A. et al. Hospitals during economic crisis: a systematic review based on resilience system capacities framework. BMC Health Serv Res 22, 977 (2022). https://doi.org/10.1186/s12913-022-08316-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-08316-4