Abstract
Background
As of November 25th 2021, four SARS-CoV − 2 variants of concern (VOC: Alpha (B.1.1.7), Beta (B.1.351), Gamma (P.1), and Delta (B.1.617.2)) have been detected. Variable degrees of increased transmissibility of the VOC have been documented, with potential implications for hospital and health system capacity and control measures. This rapid review aimed to provide a synthesis of evidence related to health system responses to the emergence of VOC worldwide.
Methods
Seven databases were searched up to September 27, 2021, for terms related to VOC. Titles, abstracts, and full-text documents were screened independently by two reviewers. Data were extracted independently by two reviewers using a standardized form. Studies were included if they reported on at least one of the VOC and health system outcomes.
Results
Of the 4877 articles retrieved, 59 studies were included, which used a wide range of designs and methods. Most of the studies reported on Alpha, and all except two reported on impacts for capacity planning related to hospitalization, intensive care admissions, and mortality. Most studies (73.4%) observed an increase in hospitalization, but findings on increased admission to intensive care units were mixed (50%). Most studies (63.4%) that reported mortality data found an increased risk of death due to VOC, although health system capacity may influence this. No studies reported on screening staff and visitors or cohorting patients based on VOC.
Conclusion
While the findings should be interpreted with caution as most of the sources identified were preprints, evidence is trending towards an increased risk of hospitalization and, potentially, mortality due to VOC compared to wild-type SARS-CoV − 2. There is little evidence on the need for, and the effect of, changes to health system arrangements in response to VOC transmission.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The World Health Organization (WHO) declared a global pandemic from the SARS-CoV − 2 virus, responsible for COVID-19, in March 2020 [1]. Over 246 million cases of COVID-19 had been reported worldwide along with 5 million deaths [2]. The continued rise in COVID-19 cases is causing grave concerns on the threatened capacity of health systems to manage current and new admissions for COVID-19 while still providing sufficient care on all other health conditions. This situation has been made more acute by the emergence of variants of concern (VOC).
As of mid-November 2021, four variants of the original SARS-CoV − 2 lineage (i.e., wild-type) have been declared as a VOC by the WHO, with other variants of interest being continuously monitored [3]. According to the WHO, VOC are defined by their increased potential for transmission or changes in COVID-19 epidemiology, presence of genomic mutations, and rapid spread across countries or regions, possibly leading to the decreased effectiveness of public health measures or of diagnostic tests, vaccines, and therapeutics [4, 5]. Variants of concern may have a transmission advantage which, if present, over time will lead to replacement of circulating strains with new VOC [6]. Public health and hospital-based interventions and control measures in these circumstances may need to focus on the growth of more transmissible variants, rather than total numbers of cases.
In December 2020, the variants Alpha (B.1.1.7, identified in the United Kingdom [UK]) and Beta (B.1.351, identified in South Africa) were named the first VOC by the WHO, followed by Gamma (P.1, identified in Brazil) in January 2021, and Delta (B.1.617.2, identified in India) in May 2021 [5]. Data indicates that Alpha is associated with a 43-90% increased risk of transmission compared to wild type, [7,8,9], and Beta is between 1.5 [10, 11] and 2.5 [8] times more transmissible. Delta is estimated at 60% more transmissible than Alpha [12]. Trends suggest that all VOC to date have a transmission advantage over wild-type [6,7,8].
The increased transmissibility of VOC has led to surges in COVID-19 incidence and, consequently, more hospitalizations and higher mortalities in some areas [9]. The first wave of the pandemic demonstrated the potential for even well-equipped health systems to experience overwhelmed intensive care units (ICUs) and system disruption, with wide ranging health consequences [13]. Furthermore, due to the rapid and emergent nature of SARS-CoV − 2 and VOC, health systems and public health administrators have been challenged to make pragmatic decisions in the absence of evidence. With health systems continuously under stress as a result of changes to public health restrictions [14], having to address increased waitlists from restricted access to care, and the introduction of new VOC, there is an ever growing need to optimize management of VOC patients to reduce risk and maintain capacity.
Therefore, this rapid review aimed to provide a synthesis of current evidence related to health system impacts in the context of VOC. This review is part of a larger review on transmission [6] and public health impacts [15]. The objective of this rapid review was to identify, appraise, and summarize evidence about health system impacts of the four major WHO-defined SARS-CoV − 2 VOC known as of May 2021 (Alpha, Beta, Gamma, and Delta). Based on iterative knowledge user and shareholder meetings, the following questions were derived:
What is known about the implications of the WHO-defined VOC for health system arrangement (particularly for hospitals) on:
-
a)
Adjusting capacity planning to accommodate changes in the risk of re-infection and the risk of severe disease (e.g., hospitalization, admission to ICU, and death)
-
b)
Adjusting personal protective equipment (PPE) procedures for health workers
-
c)
Adjusting restrictions and screening of staff and visitors (e.g., visitor policy changes, approach to and frequency of screening)
-
d)
Adjusting service provision (e.g., cohorting patients in hospitals based on the VOC they have acquired)
-
e)
Adjusting patient accommodations, shared spaces, and common spaces (e.g., improvement to HVAC [heating, ventilation, and air conditioning systems])
Methods
Design
We conducted a rapid review following standardized rapid methodological guidelines [16, 17]. We used an integrated knowledge translation approach, as the question was initially designed by knowledge users and refined with the synthesis team with continuous exchange during the process through regular meetings. The knowledge user partners, who are health system and infectious disease experts, reviewed the results. Patient partners were engaged in the knowledge dissemination phase to provide feedback on the final report and provide recommendations from the patient perspective.
Protocol
A protocol was developed using Joanna Briggs Institute (JBI) guidance [18] and reported according to the Preferred Reporting Items for Systematic Reviews (PRISMA) for Protocols [19]. The protocol is available on Open Science Framework [20]. The results are reported using the PRISMA 2020 guidelines [21].
Literature search
A broad, comprehensive literature search was designed by an information specialist to retrieve all literature related to VOC. The electronic database search was executed on May 11, 2021 and updated on September 27, 2021 in MEDLINE (Ovid MEDLINE All), Embase (Elsevier Embase.com), the Cochrane Database of Systematic Reviews (CDSR) and Central Register of Controlled Trials (CENTRAL) (Cochrane Library, Wiley), Epistemonikos’ Living Overview of Evidence (L·OVE) on COVID-19, and medRxiv and bioRxiv concurrently. The MEDLINE, Embase, and Cochrane Library searches used modified versions of COVID-19 filters developed by the Canadian Agency for Drugs and Technology in Health (as they appeared at the time of search development in February 2021) [22]. The search was peer reviewed by a second information specialist using the Peer Review of Electronic Search Strategies (PRESS) guideline [23]. Full search details are available as Supplementary Material for all databases.
Eligibility criteria
All studies that reported on health system impacts due to VOC were included. Studies that reported on immune escape (vaccine/prior infection protection), non-VOC related impacts, testing approaches, transmission or public health impacts, case studies without health system impacts, or animal studies were excluded. Reviews, overviews, and news articles that presented no original data were excluded, but references were scanned to identify additional relevant studies. Only English-language searches were conducted, but non-English results were considered for inclusion.
Screening and data extraction process
After a pilot-test exercise amongst the team, titles/abstracts and full-text screening was completed by two reviewers in Covidence. The data extraction form was designed in consultation with knowledge user partners and pilot-tested amongst the team. Data extraction was completed by two reviewers and verified by a third.
Critical appraisal
Critical appraisal for observational studies was conducted using the Joanna Briggs Institute (JBI) appraisal tools [18]. Two team members independently conducted critical appraisals for all eligible studies. Reviewers met to discuss scores, and a third, independent team member was consulted to assist with resolving conflicts. Modeling studies and lab-based studies were not appraised due to the absence of a standardized appraisal tool for these study types. As the quality of preprints should be interpreted with caution, efforts were made to reflect this through the removal of two points from the overall score. Similarly, one point was removed from any published letters to the editor as they are not fully peer reviewed, yet they are published in a peer reviewed journal. Cohort studies were awarded a maximum of 11 points, case control studies awarded a maximum of 10 points, and cross-sectional studies were awarded a maximum of eight points. Final scores for observational studies were presented as a percentage, based on an average between the two appraiser scores. An overall quality rating of low, medium, or high was reported for each observational study, which correlated with a score of < 50%, 50-80% or > 80% respectively.
Synthesis
The results were presented descriptively in text, tables, and diagrams. A meta-analysis was not possible due to heterogeneity across the included studies regarding their study designs, participants included, and VOC.
Results
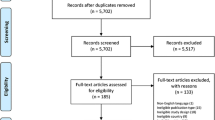
The search identified 7300 records; 4877 records were screened after duplicate removal using Covidence, and 59 studies that reported on health system impacts were included (25 identified in the search on May 11, 2021, and 34 identified on September 27, 2021) (see Fig. 1 for PRISMA Flow Diagram). Of note, the search was intended to be very broad due to the significant variation in reporting and terminology in early VOC literature. In total, 25 preprints and 34 peer-reviewed journal articles were identified (see Supplementary Material 2 for a summary table of included studies). In the updated search, six studies that were originally included as preprints had subsequently been published in a peer reviewed journal. Alpha was the most reported-on VOC (n = 28). Seven studies reported on Gamma, four studies reported on Beta, five studies reported on Delta, and fifteen studies reported on multiple VOC. Most of the studies were from the UK or England (n = 18), followed by Brazil (n = 7) and France (n = 6). Three studies reported on multiple European countries. Figure 2 provides an overview of country or region of data collection and VOC up to September 27, 2021, while Fig. 3 provides an illustration of the number of studies on each of the outcomes from all countries.
Critical appraisal
Of the 59 studies, 31 were cohort studies, 20 used a cross-sectional design, and one was a case control study; thus, they were subject to appraisal using the relevant JBI checklists. Among the 51 cohort/cross-sectional studies, five were appraised as low quality [24,25,26,27,28], 24 as medium quality [29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52], and 22 as high quality [53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74]. The case control study was of medium quality [75]. A complete overview of JBI scores by study can be found in Table 1. Of note, six were modeling studies and one was a lab-based study; these were therefore not included in the quality assessment.
Question A: Adjusting capacity planning to accommodate changes in the risk of re-infection and the risk of severe disease (e.g., hospitalization, admission to ICU, and death)
Figure 3 provides an overview of studies that explored various aspects of capacity planning in relation to country or region. While most studies related to this sub-question reported on the impact of VOC on hospitalization, admission to ICU, and mortality, six studies reported on outcomes in relation to vaccines. Haas et al. [59] conducted the first nationwide estimates on the vaccine effectiveness (VE) of two doses of the Pfizer vaccine on hospitalization and deaths in Israel during a period of high Alpha prevalence. They found that adjusted VE against COVID-19 hospitalization was 97.2% (95% CI 96.8-97.5), against severe and critical hospitalization was 97.5% (95%CI: 97.1-97.8), and against death was 96.7% (95%CI: 96.0-97.3). AlQahtani et al. [51] compared four vaccines (Astra-Zeneca, Pfizer/BioNtech, Sinopharm, and Sputnik V) and found that all were effective in decreasing risk of hospitalization, ICU admission, and mortality prior to and during the period when Delta was dominant, although the Sinopharm vaccine is less effective than the Pfizer/BioNtech on all outcomes. Agrawal et al. [40] found that in patients with pre-existing medical conditions who were infected with Delta but vaccinated were less likely to die than patients who were unvaccinated (p = 0.002); no difference was found in patients without pre-existing conditions who were infected with either Alpha or Delta. Havers et al. [42] found that hospitalization rates were > 10 times higher in unvaccinated individuals compared to vaccinated individuals during a period of high Delta prevalence. Twohig et al. [70] found that patients with Delta who were unvaccinated or < 21 days since first dose had a higher estimated risk of hospital admission and a higher risk of either hospital admission or emergency care than patients with Alpha; however, there was no significant interaction when comparing between vaccinated and unvaccinated individuals infected with either Delta or Alpha. Veneti et al. [72] found that after adjusting for sex, age group, country of birth, variant and underlying comorbidities, partially vaccinated individuals had a 72% reduced risk of hospitalization (95%CI 59–82%) and fully vaccinated had a 76% reduced risk of hospitalization (95%CI 61–85%) compared to unvaccinated individuals with Delta or Alpha.
Di Domenico et al. also reported on outcomes differently, in that they provided an age-stratified transmission model to estimate the role that curfew measures could have on hospitalization in France [76]. They found that if the epidemic progressed under curfew conditions (6:00 pm nightly, implemented nationwide January 16, 2021) before school holidays and vaccination was accelerated, hospital capacity would be reached around week 13 in France (which had 2.2% Alpha penetration), week 12 in Île-de-France (which had the highest Alpha penetration, 6.9%), and week 14 in Nouvelle Aquitaine (which had the lowest Alpha penetration, 1.7%). This was supported by data. The partial relaxation of social distancing (estimated at a 15% increase in effective reproduction number) would shorten these estimates by at least one week. Stronger social distancing, equivalent to the efficacy measured during the second lockdown (estimated at a 15% reduction in effective reproduction number), would maintain hospitalizations below the peak of the second wave in Île-de-France and Nouvelle Aquitaine but would not be enough to avoid a third wave in France, even under accelerated vaccination (100,000 − 200,000 doses/day). Accelerated (200,000 first doses/day) and optimistic vaccination rollouts (300,000 first doses/day) would reduce weekly hospitalizations by about 20 and 35% in week 16 (i.e., April 19 − 25, 2021) compared to a stable vaccination campaign without acceleration (100,000 first doses/day).
Finally, Ong et al. [66] reported on a composite measure of disease severity, defined by a composite outcome of oxygen requirement, ICU admission, and death, and found that Delta was associated with increased disease severity compared to non-VOC (unadjusted OR 5.55 (95% 1.66 – 34.44); adjusted OR 4.90 (95%CI 1.43 – 30.78)). No difference was found for Alpha or Gamma.
Impact of VOC on hospitalization/severity
Thirty-one studies reported on health system impacts related to hospitalization and/or severity of disease (see Table 2). Of the four VOC, Alpha was the most predominantly reported on, with fourteen studies finding an increase in hospitalization due to Alpha, while five studies reported no change. Fewer studies reported on the other VOC: five studies on Beta (three with increases in hospitalization and two with no change), two studies on Gamma (two reported increases in hospitalization) and four studies on Delta (two reported increases and two no change). Four studies reported on combined VOC, with all studies finding an increase in hospitalization compared to non-VOC. Overall, 73.5% of studies reported increases in hospitalization and/or severity due to any VOC compared to non-VOC.
Impact of VOC on admission to ICU
Twenty-six studies reported on health system impacts related to admission to ICU (see Table 3). Again, Alpha was the VOC most predominantly reported on (n = 12 studies), with six studies finding an increase in ICU admission due to Alpha, while six studies reported no change. Fewer studies reported on the other VOC: three studies on Beta (one with increases in ICU admission and two with no change), four studies on Gamma (one reported increases in ICU admission and three no change) and two on Delta (one reported increases in ICU admission and one no change). Five studies reported on combined VOC, with four studies finding an increase in ICU admission compared to non-VOC and one study finding no change. Overall, 50% of studies reported increases in ICU admission due to any VOC compared to non-VOC.
Impact of VOC on mortality
Forty-one studies reported on health system impacts related to risk of mortality (see Table 4). Again, Alpha was the VOC most predominantly reported on (n = 23 studies), with eleven studies finding an increase in mortality due to Alpha, four studies reporting mixed findings, and eight studies reporting no change. Five studies on Beta (four reported increases in mortality and one reported mixed findings), six studies on Gamma (all six reported increases in mortality), and three studies on Delta (all three reported increases in mortality) were reported. Four studies reported on combined VOC, with two studies finding an increase in mortality compared to non-VOC and two studies finding no change. Overall, 26/41 studies (63.4%) found an increased risk of mortality due to VOC compared to non-VOC.
Question B: Adjusting PPE procedures for healthcare workers
One modeling study reported on adjusting Personal Protective Equipment (PPE) procedures. Pham et al. [81] modeled the impact of different interventions on transmission, healthcare worker (HCW) absenteeism, and test positivity as markers of intervention efficiency against Alpha transmission. In the baseline scenario, it was assumed that HCWs were using PPE while in COVID wards when seeing patients but not during breaks or when in other parts of the hospital, assuming 95% of HCWs worked in the same wards over time. While specific PPE used was not defined, PPE efficiency was defined as percentage reduction of droplet transfer. Assuming 90% effective PPE use in COVID wards, they found that extending PPE use to non-COVID wards (all HCWs used PPE with 90% effectiveness when on ward) would prevent 93.7% of all transmissions and would also prevent outbreaks among patients and HCWs. Even if PPE effectiveness was reduced to 70%, findings did not change significantly; however, if it was reduced to 50% or below, screening HCWs every 3 days was more effective than PPE use in all wards. Overall, PPE use in all wards was modeled to be more effective than all other interventions.
One observational study found that the amount of disposable plastic generated by a single RT-PCR diagnostic test and the PPE used by PCR operators was 821.8 g [82]. Given the increased testing with greater spread of COVID-19 due to VOC, the authors argue that there needs to be greater attention paid to biomedical plastic waste to minimize the environmental impact.
Question C: Adjusting restrictions to and screening staff and visitors (e.g., visitor policy changes, approach to and frequency of screening)
No studies had reported on this outcome as of September 27, 2021.
Question D: Adjusting service provision based on VOC status (e.g., cohorting patients in hospitals based on the SARS-CoV-2 variants they have)
No studies had reported on this outcome as of September 27, 2021.
Question E: Adjusting patient accommodations, shared spaces, and common spaces (e.g., improvement to HVAC systems)
One study reported on the presence of SaRS-CoV-2 on regularly-touched environmental surfaces during high Alpha prevalence [82]. In shared spaces/surface contamination, patient bed handles, the nursing station, the reception desk, door handles of doctor’s office, toilet door handles, cell phones, patient toilet sinks, toilet bowls, and patient pillows (defined as high-touch surfaces) were considered as high-risk sources of transmission. Alcohol-based rubs (ethanol 70%) were effective at reducing the presence of SARs-CoV-2 on most surfaces after 15 min where sodium hypochlorite (0.001%) was mostly ineffective [82].
Discussion
This rapid review sought to identify, appraise, and summarize evidence related to the impact of VOC known as of September 27, 2021, (Alpha, Beta, Gamma, Delta) on health system arrangements. Among the studies that reported on the impact of VOC on hospitalization, trends suggest there is an increase in hospitalization due to VOC. There seems to be less agreement on the impact of VOC on ICU admissions, with only 50% finding an increase in ICU admissions due to VOC. Most studies (63.4%) reporting mortality data found an increased risk of death due to VOC, although health system capacity may influence this. One study reported on the effectiveness of PPE in reducing VOC transmission in the hospital and one study reported on PPE waste and the effectiveness of alcohol-based rubs (ethanol 70%) at reducing the presence of SaRs-CoV-2 on most surfaces after 15 min. No studies reported on screening staff and visitors or adjusting service provisions (e.g., cohorting), which is a significant gap in the literature.
Our search identified 59 studies related to health system arrangements, with almost all reporting on the impact on hospitalization, ICU admissions, and mortality. Due the rapid growth in the literature on VOC and COVID-19 broadly, there is variation in how data is collected, reported, and ultimately summarized. All studies on health system arrangements also came from three primary geographic areas – UK/Europe, Brazil, and France. Thus, the impact of VOC on other health systems around the world are predominantly unreported in the literature to date. Due to variation in study design, conduct, and local epidemiology of COVID-19 and VOC spread, it is difficult to tease apart reasons as to why different studies found variation in the impact of VOC on hospitalization, ICU admission, and mortality rates.
As evident in this rapid review, the findings on the impact of VOC on health system arrangements are quickly changing and emerging. We have identified several specific research gaps that need to be addressed to provide more robust evidence around health system arrangement decisions. In particular, given the lack of evidence this review identified on screening staff and visitors, cohorting patients based on VOC, or adjusting patient accommodations and shared spaces, future research should prioritize these areas to address this gap. Evidence is needed related to best practices for screening staff and visitors in health service organizations and adjusting service provisions. Evidence is also needed to determine whether adjusting patient accommodations and shared spaces in hospital settings is warranted based on the presence of VOC. The generation of evidence from countries that are experiencing significant impacts of VOC and for which there are no current reports should be the focus of future research. Finally, additional research is needed on Beta, Gamma, and Delta to determine whether the risks to health system arrangements are similar for all VOC.
Limitations
While this rapid review has several strengths, there are limitations that must be acknowledged. First, due to the rapid production of the literature on COVID-19 and VOC, 42% of the studies included in this review were preprints and have thus not yet undergone peer review. Nevertheless, most studies scored medium or high in the quality appraisal, suggesting that the evidence in this area is relatively reliable. Most studies used large health administrative databases as sources of evidence with reliable methods for determining exposures/outcomes. Additionally, our search strategy was limited to articles that specified reporting on one of the recognized VOC (Alpha, Beta, Gamma, and Delta). Given the growing trend that VOC are replacing the wild-type as the dominant strain as well as the continued emergence of other variants of interest, future consideration of expanding the search strategy may be warranted. It is also important to acknowledge the limitation of the epidemiology contact. Due to the variation in testing strategies in countries where studies occurred, the adequacy of case finding in the community and thus denominator completeness may vary, which impacts the ability to assess hospital rates and the impact of VOC on health system impacts and mortality. Finally, some studies reported mixed findings based on adjusted and unadjusted analyses, which must be considered when comparing across studies.
Conclusions
This rapid review provides synthesized evidence related to the health system impacts of the four SARS-CoV-2 VOC. While the findings should be interpreted with caution as many of the sources identified were preprints, the evidence is trending towards increased risk of severe outcomes including hospitalization and mortality in VOC cases compared to wild type SARS-CoV-2 cases. Currently, there is a lack of pragmatic studies to inform health system capacity expectations and health management practices. Further research is needed to address the gaps identified in this review, including the insufficient or lack of evidence on adjusting PPE procedures for healthcare workers, screening staff and visitors, cohorting patients based on VOC, or adjusting patient accommodations and shared spaces.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- Alpha:
-
variant of concern originating in the United Kingdom
also known as VUI 202012/01 and VOC 202012/01 formerly known as B.1.1.7
- Beta:
-
variant of concern originating in South Africa, also known as 20H/501Y.V2, formerly known as B.1351
- Delta:
-
variant of concern originating in India, formerly known as B.1.617.2
- Gamma:
-
variant of concern originating in Brazil, also known as B.1.28.1, formerly known as P.1
- ARF:
-
acute respiratory failure
- CI:
-
confidence interval
- CFR:
-
case fatality rate
- COG-UK:
-
COVID-19 UK Genetics Consortium
- HCW:
-
healthcare worker
- HR:
-
hazard ratio
- HVAC:
-
heating, ventilation, and air conditioning
- ICU:
-
Intensive Care Unit
- IQR:
-
interquartile range
- LOS:
-
length of stay
- OR:
-
odds ratio
- PCR:
-
polymerase chain reaction
- PPE:
-
personal protective equipment
- RR:
-
risk ratio
- SGTF:
-
S-gene target failure
- UK:
-
United Kingdom
- VE:
-
vaccine effectiveness
- VOC:
-
variant of concern
- WHO:
-
World Health Organization
- JBI:
-
Joanna Briggs Institute
References
Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed 2020;91:157–60. https://doi.org/10.23750/abm.v91i1.9397.
World Health Organization. COVID-19 Weekly Epidemiological Update (Edition 64). 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19%2D%2D-2-november-2021.
WHO. SARS-CoV-2 Variants. World Health Organization 2020. http://www.who.int/csr/don/31-december-2020-sars-cov2-variants/en/. Accessed 9 Mar 2021.
WHO. COVID-19 Weekly Epidemiological Update - 25 February 2021. 2021. https://www.who.int/publications/m/item/covid-19-weekly-epidemiological-update. Accessed 9 Mar 2021.
WHO. Tracking SARS-CoV-2 variants. https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/ . Accessed 7 Jun 2021.
Curran JA, Dol J, Boulos L, et al. Transmission characteristics of SARS-CoV-2 variants of concern: Rapid Scoping Review. medRxiv. 2021;2021.04.23.21255515. https://doi.org/10.1101/2021.04.23.21255515.
WHO. Weekly operational update on COVID-19 - 24 May 2021. 2021. https://www.who.int/publications/m/item/weekly-operational-update-on-covid-19%2D%2D-24-may-2021. Accessed 28 May 2021.
Innovation A for C. Living Evidence - SARS-CoV-2 variants. Agency for Clinical Innovation. 2021. https://aci.health.nsw.gov.au/covid-19/critical-intelligence-unit/sars-cov-2-variants. Accessed 24 Apr 2021.
Davies NG, Abbott S, Barnard RC, et al. Estimated transmissibility and impact of SARS-CoV-2 lineage B.1.1.7 in England. Science 2021;372. https://doi.org/10.1126/science.abg3055.
WHO. COVID-19 Weekly epidemiological update - April 13, 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19%2D%2D-13-april-2021. Accessed 24 Apr 2021.
Wibmer CK, Ayres F, Hermanus T, et al. SARS-CoV-2 501Y.V2 escapes neutralization by South African COVID-19 donor plasma. bioRxiv. Published Online First: 1 March 2021. https://doi.org/10.1101/2021.01.18.427166.
Mahase E. Delta variant: What is happening with transmission, hospital admissions, and restrictions? BMJ. 2021;n1513. https://doi.org/10.1136/bmj.n1513.
WHO. Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 27 August 2020. 2020. https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-EHS_continuity-survey-2020.1. Accessed 26 Apr 2021.
Tuite A, Fisman D, Odutayo A, et al. COVID-19 Hospitalizations, ICU Admissions and Deaths Associated with the New Variants of Concern. https://doi.org/10.47326/ocsat.2021.02.18.1.0.
Somerville M, Curran JA, Dol J, et al. Public health implications of SARS-CoV-2 variants of concern: a rapid scoping review. BMJ Open. 2021;11:e055781. https://doi.org/10.1136/bmjopen-2021-055781.
Tricco AC, Langlois EV, Straus SE, et al. Rapid reviews to strengthen health policy and systems: a practical guide. 2017. http://apps.who.int/iris/bitstream/10665/258698/1/9789241512763-eng.pdf. Accessed 9 Mar 2021.
Garritty C, Gartlehner G, Nussbaumer-Streit B, et al. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J Clin Epidemiol. 2020; https://doi.org/10.1016/j.jclinepi.2020.10.007.
Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI 2020. https://doi.org/10.46658/JBIMES-20-01.
Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. https://doi.org/10.1136/bmj.g7647.
Dol J, Curran J, Bolous L, et al. COVID-19 variants of concern – a rapid scoping review protocol. Open Science Framework Published Online First: 2021. https://osf.io/7ugpf/. Accessed 25 Jun 2021.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Canadian Agency for Drugs and Technologies in Health (CADTH). CADTH COVID-19 Search Strings - COVID-19 - Medline. 2021. https://covid.cadth.ca/literature-searching-tools/cadth-covid-19-search-strings/#covid-19-medline.
McGowan J, Sampson M, Salzwedel DM, et al. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6. https://doi.org/10.1016/j.jclinepi.2016.01.021.
de Andrade CLT, Lima SML, Martins M, et al. Has the age distribution of hospitalized Covid-19 patients changed in Brazil? medRxiv. 2021;2021.03.30.21254650. https://doi.org/10.1101/2021.03.30.21254650.
de Oliveira MHS, Lippi G, Henry BM. Sudden rise in COVID-19 case fatality among young and middle-aged adults in the south of Brazil after identification of the novel B.1.1.28.1 (P.1) SARS-CoV-2 strain: analysis of data from the state of Parana. medRxiv. 2021;2021.03.24.21254046. https://doi.org/10.1101/2021.03.24.21254046.
Moore CM, Sergienko R, Arbel R. SARS-CoV-2 alpha variant: is it really more deadly? A population level observational study. MedRxiv Published Online First: 18 August 2021. https://doi.org/10.1101/2021.08.17.21262167.
Jabłońska K, Aballéa S, Auquier P, et al. On the association between SARS-COV-2 variants and COVID-19 mortality during the second wave of the pandemic in Europe. medRxiv. 2021;2021.03.25.21254289. https://doi.org/10.1101/2021.03.25.21254289.
Freitas ARR, Beckedorff OA, Cavalcanti LP de G, et al. A emergência da nova variante P.1 do SARS-CoV-2 no Amazonas (Brasil) foi temporalmente associada a uma mudança no perfil da mortalidade devido a COVID-19, segundo sexo e idade. Published Online First: 26 March 2021. https://doi.org/10.1590/SciELOPreprints.2030.
Budhiraja S, Indrayan A, Aggarwal M, et al. Differentials in the characteristics of COVID-19 cases in Wave-1 and Wave-2 admitted to a network of hospitals in North India. MedRxiv Published Online First: 27 June 2021. https://doi.org/10.1101/2021.06.24.21259438.
Freitas ARR, Lemos DRQ, Beckedorff OA, et al. The increase in the risk of severity and fatality rate of covid-19 in southern Brazil after the emergence of the Variant of Concern (VOC) SARS-CoV-2 P.1 was greater among young adults without pre-existing risk conditions. medRxiv. 2021;2021.04.13.21255281. https://doi.org/10.1101/2021.04.13.21255281.
Dabrera G, Allen H, Zaidi A, et al. Assessment of Mortality and Hospital Admissions Associated with Confirmed Infection with SARS-CoV-2 Variant of Concern VOC-202012/01 (B.1.1.7) a Matched Cohort and Time-to-Event Analysis. SSRN Electronic Journal Published Online First: 1 January 2021. https://doi.org/10.2139/ssrn.3802578.
Erman A, Mishra S, Barrett KA, et al. Variant-of-concern-attributable health and health system-related outcomes: a population-level propensity-score matched cohort study. MedRxiv Published Online First: 3 June 2021. https://doi.org/10.1101/2021.06.02.21257869.
Fisman DN, Tuite AR. Progressive Increase in Virulence of Novel SARS-CoV-2 Variants in Ontario, Canada. MedRxiv Published Online First: 7 July 2021. https://doi.org/10.1101/2021.07.05.21260050.
Martin-Blondel G, Lescure F-X, Assoumou L, et al. Increased risk of severe COVID-19 in hospitalized patients with SARS-CoV-2 variant of concern alpha infection in France: a multicentre matched cohort study with retrospective data collection. SSRN Journal Published Online First: 2021. https://doi.org/10.2139/ssrn.3866550.
McAlister FA, Nabipoor M, Chu A, et al. Lessons from the COVID-19 Third Wave in Canada: The Impact of Variants of Concern and Shifting Demographics. MedRxiv Published Online First: 28 August 2021. https://doi.org/10.1101/2021.08.27.21261857.
Puech B, Legrand A, Simon O, et al. Prognosis of Critically Ill Patients With Acute Respiratory Failure Due To The SARS-CoV-2 501Y.V2 Variant: A Multicenter Retrospective Matched Cohort Study. In Review 2021. https://doi.org/10.21203/rs.3.rs-806080/v2.
Swann OV, Pollock L, Holden KA, et al. Comparison of children and young people admitted with SARS-CoV-2 across the UK in the first and second pandemic waves: prospective multicentre observational cohort study. MedRxiv Published Online First: 17 September 2021. https://doi.org/10.1101/2021.09.14.21263567.
Vassallo M, Manni S, Klotz C, et al. Patients admitted for variant alpha COVID-19 have poorer outcomes than those infected with the old strain. JCM. 2021;10:3550. https://doi.org/10.3390/jcm10163550.
Zavascki AP, Vieceli T, Wink PL, et al. Advanced ventilatory support and mortality in hospitalized patients with COVID-19 caused by Gamma (P.1) variant of concern compared to other lineages: cohort study at a reference center in Brazil. In Review 2021. https://doi.org/10.21203/rs.3.rs-910467/v1.
Agrawal N, Sharma A, Kumar Sahu S, et al. Clinical and demographic features of SARS-COV-2 variants of concern (VOC): B.1.1.7 and B.1.617.2 at a tertiary care hospital in southern Rajasthan. Eur J Mol Clin Med. 2021;8:702–8.
Snell LB, Wang W, Alcolea-Medina A, et al. First and second SARS-CoV-2 waves in inner London: A comparison of admission characteristics and the impact of the B.1.1.7 variant. medRxiv 2021;2021.03.16.21253377. https://doi.org/10.1101/2021.03.16.21253377.
Havers FP, Pham H, Taylor CA, et al. COVID-19-associated hospitalizations among vaccinated and unvaccinated adults ≥18 years – COVID-NET, 13 states, January 1 – July 24, 2021. MedRxiv Published Online First: 29 August 2021. https://doi.org/10.1101/2021.08.27.21262356.
Khedar RS, Mittal K, Ambaliya HC, et al. Greater Covid-19 Severity and Mortality in Hospitalized Patients in Second (Delta Variant) Wave Compared to the First: Single Centre Prospective Study in India. MedRxiv Published Online First: 7 September 2021. https://doi.org/10.1101/2021.09.03.21263091.
Maslo C, Messina A, Laubscher A, et al. COVID-19: A comparative study of severity of patients hospitalized during the first and the second wave in South Africa. MedRxiv Published Online First: 11 May 2021. https://doi.org/10.1101/2021.05.11.21257033.
Adhikari EH, SoRelle JA, McIntire DD, et al. Increasing severity of COVID-19 in pregnancy with Delta (B.1.617.2) variant surge. Am J Obstet Gynecol 2021;:S000293782101005X. https://doi.org/10.1016/j.ajog.2021.09.008.
Cetin M, Balci PO, Sivgin H, et al. Alpha variant (B.1.1.7) of SARS-CoV-2 increases fatality-rate for patients under age of 70 years and hospitalization risk overall. AMicr Published Online First: 11 August 2021. https://doi.org/10.1556/030.2021.01524.
Courjon J, Contenti J, Demonchy E, et al. COVID-19 patients age, comorbidity profiles and clinical presentation related to the SARS-CoV-2 UK-variant spread in the southeast of France. Sci Rep. 2021;11:18456. https://doi.org/10.1038/s41598-021-95067-7.
Loconsole D, Centrone F, Morcavallo C, et al. Rapid spread of the SARS-CoV-2 variant of concern 202012/01 in southern Italy (December 2020-March 2021). Int J Environ Res Public Health. 2021;18. https://doi.org/10.3390/ijerph18094766.
Louis G, Goetz C, Mellati N, et al. Preliminary data on severe SARS-CoV-2 infection caused by the 501Y.V2 variant. Anaesth Crit Care Pain Med 2021;40:100890. https://doi.org/10.1016/j.accpm.2021.100890.
Martínez-García L, Espinel MA, Abreu M, et al. Emergence and Spread of B.1.1.7 Lineage in Primary Care and Clinical Impact in the Morbi-Mortality among Hospitalized Patients in Madrid, Spain. Microorganisms 2021;9:1517. https://doi.org/10.3390/microorganisms9071517.
AlQahtani M, Bhattacharyya S, Alawadi A, et al. Morbidity and mortality from COVID-19 post-vaccination breakthrough infections in association with vaccines and the emergence of variants in Bahrain. In Review 2021. https://doi.org/10.21203/rs.3.rs-828021/v1.
Takemoto MLS, Nakamura-Pereira M, Menezes MO, et al. Higher case fatality rate among obstetric patients with COVID-19 in the second year of pandemic in Brazil: do new genetic variants play a role? medRxiv 2021;:2021.05.06.21256651. https://doi.org/10.1101/2021.05.06.21256651.
Bager P, Wohlfahrt J, Fonager J, et al. Risk of hospitalisation associated with infection with SARS-CoV-2 lineage B.1.1.7 in Denmark: an observational cohort study. Lancet Infect Dis. 2021;21:1507–17. https://doi.org/10.1016/S1473-3099(21)00290-5.
Challen R, Brooks-Pollock E, Read JM, et al. Risk of mortality in patients infected with SARS-CoV-2 variant of concern 202012/1: matched cohort study. BMJ. 2021;372:n579. https://doi.org/10.1136/bmj.n579.
Cusinato M, Gates J, Jajbhay D, et al. Increased risk of death in covid-19 hospital admissions during the second wave as compared to the first epidemic wave. A prospective dynamic cohort study in South London, UK. Infection Published Online First: 12 June 2021. https://doi.org/10.1101/2021.06.09.21258537.
Dennis JM, McGovern AP, Thomas NJ, et al. Trends in 28-day mortality of critical care patients with coronavirus disease 2019 in the United Kingdom: a National Cohort Study, march 2020 to January 2021*. Crit Care Med. 2021;49:1895–900. https://doi.org/10.1097/CCM.0000000000005184.
Frampton D, Rampling T, Cross A, et al. Genomic characteristics and clinical effect of the emergent SARS-CoV-2 B.1.1.7 lineage in London, UK: a whole-genome sequencing and hospital-based cohort study. Lancet Infect Dis 2021. https://doi.org/10.1016/S1473-3099(21)00170-5.
Grint DJ, Wing K, Houlihan C, et al. Severity of Severe Acute Respiratory System Coronavirus 2 (SARS-CoV-2) Alpha Variant (B.1.1.7) in England. Clinical Infectious Diseases 2021;ciab754. https://doi.org/10.1093/cid/ciab754.
Haas EJ, Angulo FJ, McLaughlin JM, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet. 2021;397:1819–29. https://doi.org/10.1016/S0140-6736(21)00947-8.
Jassat W, Mudara C, Ozougwu L, et al. Difference in mortality among individuals admitted to hospital with COVID-19 during the first and second waves in South Africa: a cohort study. Lancet Glob Health. 2021;9:e1216–25. https://doi.org/10.1016/S2214-109X(21)00289-8.
Nyberg T, Twohig KA, Harris RJ, et al. Risk of hospital admission for patients with SARS-CoV-2 variant B.1.1.7: cohort analysis. BMJ 2021;n1412. https://doi.org/10.1136/bmj.n1412.
Area I, Lorenzo H, Marcos PJ, et al. One year of the COVID-19 pandemic in Galicia: a global view of age-group statistics during three waves. IJERPH. 2021;18:5104. https://doi.org/10.3390/ijerph18105104.
Funk T, Pharris A, Spiteri G, et al. Characteristics of SARS-CoV-2 variants of concern B.1.1.7, B.1.351 or P.1: data from seven EU/EEA countries, weeks 38/2020 to 10/2021. Euro Surveill. 2021;26. https://doi.org/10.2807/1560-7917.ES.2021.26.16.2100348.
Garvey MI, McMurray C, Casey AL, et al. Observations of SARS-CoV-2 variant of concern B.1.1.7 at the UK’s largest hospital Trust. J Infect Published Online First: 28 April 2021. https://doi.org/10.1016/j.jinf.2021.04.026.
Graham MS, Sudre CH, May A, et al. Changes in symptomatology, reinfection, and transmissibility associated with the SARS-CoV-2 variant B.1.1.7: an ecological study. Lancet Public Health. 2021;6:e335–45. https://doi.org/10.1016/S2468-2667(21)00055-4.
Ong SWX, Chiew CJ, Ang LW, et al. Clinical and Virological Features of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Variants of Concern: A Retrospective Cohort Study Comparing B.1.1.7 (Alpha), B.1.351 (Beta), and B.1.617.2 (Delta). Clinical Infectious Diseases 2021;ciab721. https://doi.org/10.1093/cid/ciab721.
Pascall DJ, Mollett G, Blacow R, et al. The SARS-CoV-2 Alpha variant causes increased clinical severity of disease. MedRxiv Published Online First: 24 August 2021. https://doi.org/10.1101/2021.08.17.21260128.
Patone M, Thomas K, Hatch R, et al. Mortality and critical care unit admission associated with the SARS-CoV-2 lineage B.1.1.7 in England: an observational cohort study. Lancet Infect Dis. 2021;21:1518–28. https://doi.org/10.1016/S1473-3099(21)00318-2.
Stirrup O, Boshier F, Venturini C, et al. SARS-CoV-2 lineage B.1.1.7 is associated with greater disease severity among hospitalised women but not men: multicentre cohort study. BMJ Open Resp Res. 2021;8:e001029. https://doi.org/10.1136/bmjresp-2021-001029.
Twohig KA, Nyberg T, Zaidi A, et al. Hospital admission and emergency care attendance risk for SARS-CoV-2 delta (B.1.617.2) compared with alpha (B.1.1.7) variants of concern: a cohort study. Lancet Infect Dis 2021;S1473309921004758. https://doi.org/10.1016/S1473-3099(21)00475-8.
Veneti L, Seppälä E, Larsdatter Storm M, et al. Increased risk of hospitalisation and intensive care admission associated with reported cases of SARS-CoV-2 variants B.1.1.7 and B.1.351 in Norway, December 2020 –May 2021. PLoS One. 2021;16:e0258513. https://doi.org/10.1371/journal.pone.0258513.
Veneti L, Valcarcel Salamanca B, Seppälä E, et al. No difference in risk of hospitalisation between reported cases of the SARS-CoV-2 Delta variant and Alpha variant in Norway. MedRxiv Published Online First: 5 September 2021. https://doi.org/10.1101/2021.09.02.21263014.
Whittaker R, Kristofferson AB, Seppälä E, et al. Trajectories of hospitalisation for patients infected with SARS-CoV-2 variant B.1.1.7 in Norway, December 2020 – April 2021. J Infect 2021;83:e14–e17. https://doi.org/10.1016/j.jinf.2021.07.025.
Nonaka CKV, Gräf T, Barcia CA de L, et al. SARS-CoV-2 variant of concern P.1 (Gamma) infection in young and middle-aged patients admitted to the intensive care units of a single hospital in Salvador, Northeast Brazil, February 2021. Int J Infect Dis 2021;111:47–54. https://doi.org/10.1016/j.ijid.2021.08.003.
Abu-Raddad LJ, Chemaitelly H, Ayoub HH, et al. Severity, criticality, and fatality of the SARS-CoV-2 Beta variant. Clinical Infectious Diseases Published Online First: 4 August 2021. https://doi.org/10.1101/2021.08.02.21261465.
Di Domenico L, Sabbatini CE, Pullano G, et al. Impact of January 2021 curfew measures on SARS-CoV-2 B.1.1.7 circulation in France. Euro Surveill 2021;26. 10.2807/1560-7917.ES.2021.26.15.2100272.
Mitze T, Rode J. Early assessment of epidemiological trends associated with SARS-CoV-2 variants of concern in Germany. medRxiv 2021;2021.02.16.21251803. https://doi.org/10.1101/2021.02.16.21251803.
Davies NG, Jarvis CI, Edmunds WJ, et al. Increased mortality in community-tested cases of SARS-CoV-2 lineage B.1.1.7. Nature. 2021;1–5. https://doi.org/10.1038/s41586-021-03426-1.
Zhao S, Lou J, Chong MKC, et al. Inferring the association between the risk of COVID-19 case fatality and N501Y substitution in SARS-CoV-2. Viruses. 2021;13. https://doi.org/10.3390/v13040638.
Ackland JA, Ackland GJ, Wallace DJ. Evolution of case fatality rates in the second wave of coronavirus in England: effects of false positives, a Variant of Concern and vaccination. medRxiv. 2021;2021.04.14.21255385. https://doi.org/10.1101/2021.04.14.21255385.
Pham TM, Tahir H, van de Wijgert JHHM, et al. Interventions to control nosocomial transmission of SARS-CoV-2: a modelling study. BMC Med. 2021;19:211. https://doi.org/10.1186/s12916-021-02060-y.
Seif F, Noorimotlagh Z, Mirzaee SA, et al. The SARS-CoV-2 (COVID-19) pandemic in hospital: an insight into environmental surfaces contamination, disinfectants’ efficiency, and estimation of plastic waste production. Environ Res. 2021;202:111809. https://doi.org/10.1016/j.envres.2021.111809.
Funding
The SPOR Evidence Alliance (SPOR EA) is supported by the Canadian Institutes of Health Research (CIHR) under the Strategy for Patient-Oriented Research (SPOR) initiative. COVID-19 Evidence Network to support Decision-making (COVID-END) is supported by the Canadian Institutes of Health Research (CIHR) through the Canadian 2019 Novel Coronavirus (COVID-19) Rapid Research Funding opportunity. ACT is funded by a Tier 2 CRC in KS.
Author information
Authors and Affiliations
Contributions
JD, JAC, MS, and LB worked collaboratively to lead the project. LS, AD and SH led the question development and provided expert feedback on the interpretation and manuscript writing. HM was involved in formatting and layout design. ACT provided feedback on methods guiding the rapid review approach. All other authors were involved in screening and data extraction. All authors reviewed and provided feedback on the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dol, J., Boulos, L., Somerville, M. et al. Health system impacts of SARS-CoV − 2 variants of concern: a rapid review. BMC Health Serv Res 22, 544 (2022). https://doi.org/10.1186/s12913-022-07847-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-07847-0