Abstract
Background
A large proportion of staff working in hospital settings are overweight or obese, have poor dietary habits and low physical activity levels. The workplace is a priority setting for health promotion. This systematic review will describe dietary and physical activity workplace interventions that have aimed to improve the health of staff in hospital settings; and the barriers and enablers of implementing these interventions.
Methods
A systematic search retrieved 551 studies from 2004 to 2020 using the following databases CINAHL Complete, MEDLINE Complete, Academic Search Complete, Global Health, Health Source Nursing/Academic Edition and PsycINFO. Studies were included if they: (1) took place in a hospital setting; (2) employed a physical activity or dietary intervention to improve the well-being of staff; (3) the intervention duration was 12 weeks or over; (4) used a control group. The Integrated quality Criteria for the Review of Multiple Study designs (ICROMS) and National Institute of Health’s National Heart Lung and Blood Institute Quality Assessment Tools for Observational Cohort and Cross-Sectional Studies tools were used to assess quality of included studies. A narrative review was conducted.
Results
Quality analysis identified six studies of high quality, nine moderate quality, and three low quality. Of these 18 studies, 15 reported at least one positive health outcome. The evidence revealed that multi-component strategies, financial incentives and motivational strategies were the most effective approaches to improve health behaviours of hospital staff.
Conclusion
Hospital-based dietary and physical activity workplace interventions show promise as an effective strategy for improving health behaviours of hospital staff. Methodological limitations highlight the need for more research from high-quality, randomised control trials, to gain further insight into the benefits of workplace interventions in hospital settings.
Similar content being viewed by others
Background
In 2016, overweight and obesity affected 39% of the adult population worldwide [1] and in high income countries like Australia the overweight and obesity rates climbed to as high as 67% [2]. Obesity is also a well-known risk for chronic type 2 diabetes, cardiovascular disease, high blood pressure, musculoskeletal disorders and some cancers [1]. Despite awareness of modifiable risk behaviours such as physical inactivity, poor nutrition, smoking and alcohol [3], obesity rates persist and consequently aggregate a significant strain on the health care system [4]. Obesity is resistant to prevention and treatment because it is a complex condition driven by a range of factors from individual behaviours to obesogenic built environments [5].
The workplace is one of the settings prioritised for health promotion according to the World Health Organization due to the influence of the workplace on physical, mental, economic and social wellbeing of employees/workers and their families, which extends to the wider community and society [6]. There are benefits of promoting health within the workplace for both the organisation/employer and the employee/worker/staff member (hereon in referred to as staff for simplicity). Given that hospitals are wholly concerned with health, the hospital workplace setting seems a logical site for obesity prevention initiatives for their staff. For hospital staff, the often-stressful nature of the hospital environment which is also characterised by shift work and night work; increases the difficulty to maintain healthy lifestyle behaviours [7, 8].
Research has revealed staff who work in hospital settings have difficulty maintaining a healthy weight, have poor dietary habits, low physical activity levels, high levels of stress and musculoskeletal conditions [9,10,11]. In the UK, over 40% of healthcare workers were classified as overweight or obese, 45% failed to reach the recommended physical activity guidelines, 30% of employees described their role as sedentary, over 50% of staff were not reaching the daily target of fruit or vegetable servings per day, and over 30% were eating high fat and high sugar foods every day [11]. Furthermore, a multi-country study in Australia, New Zealand and the United Kingdom found that over 60% of midwives were overweight or obese [9].
Key modifiable behaviours to reduce the risk of overweight and obesity are diet and physical activity. Strategies trialled in hospital settings to improve diet have included food labelling in cafeterias [12, 13], healthy catering initiative [14], installing healthier vending machines [13, 15], healthy cookbook, water bottle, sandwich container, educational resources and messaging [16], workplace champions to role model health behaviours [13] and healthy messaging signage [13, 16]. Strategies to increase physical activity have included pedometers [13, 16], education with an online learning tool [17], programs (aerobic, sports) [18], electronic messaging and guided walks [16], and sit-stand desks [19]. To date there is no consensus on the most effective strategies to implement and improve health status of staff in hospital settings, however the strategies above have been promising in improving awareness and knowledge in nutrition [12]; along with improvements in diet [14,15,16] and physical activity behaviours [13, 16, 18, 19]. A recent review has revealed organisational barriers to healthy eating in nurses such as long work hours, shift work, high workload, low staffing and work breaks being too short or too few [20]. Environmental barriers (e.g. access/cost of unhealthy food, inadequate food storage and preparation facilities), social barriers (e.g. access to treat food, social unhealthy eating practices, stress-related eating) and individual behaviours (e.g. lack of knowledge, self-efficacy and motivation) were also reported [20].
Despite the clear need to improve the health of hospital staff, i.e. dietary consumption of fruit and vegetables and increase physical activity levels; there is no clear consensus on which intervention strategies produce the best outcomes, or recognition of the barriers and enablers for implementing these dietary and physical activity workplace interventions in hospital settings [21]. There has been some review and synthesis of trials targeting stress levels of nurses and health professionals [21,22,23], burnout in emergency nurses and mental health professionals [24, 25], and the ability to increase physical activity in other settings [26]. One systematic review examined the promotion of diet and physical activity in nurses, and whilst highlighting the lack of interventions to promote diet and physical activity in nurses; its inclusion criteria applied to a wider health care setting (e.g. hospital, academic medical centres, university, surgical units, long-term facilities), included all durations of interventions, included studies without control groups and did not examine barriers and enablers related to the included studies [21].
There are no systematic reviews that examine improving health behaviours of staff through diet and physical activity purely in a hospital setting, or that extended beyond nurses to all health staff; nor understanding about the barriers and facilitators of implementing these types of interventions in a hospital setting. Given the diverse range of occupations within the hospital setting, it is important we extend our health promotion focus beyond nurses alone. Furthermore, other reviews highlight the lack of quality studies found in their reviews [21, 27], which shaped this review to target higher quality evidence, for example interventions with control groups and intervention durations considered adequate to influence behaviour change. This systematic review therefore describes workplace interventions that have aimed to improve health of staff in hospital settings and the barriers and enablers that influence the success of those interventions. Understanding the breadth of workplace interventions is needed to set the next platform of initiatives towards preventing obesity.
Aims and objectives
Research questions to be addressed in this systematic review:
-
1.
What dietary and physical activity interventions have aimed to improve diet, physical activity in staff, specifically in a hospital setting, compared to no intervention?
-
2.
What are the barriers and enablers of implementing these types of workplace interventions in a hospital setting?
Methods
Registration
This systematic review was conducted respecting the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocols [28]. The protocol for this review was registered and published in the International Prospective Register of Systematic Reviews on 15 August 2018, PROSPERO registration CRD42018096797.
Data sources and search strategy
The search terms were agreed upon through consultation between the co-authors and Deakin University’s research librarian who had expertise in systematic reviews. The terms were categorised against a methodological approach, using the PICO (patient or problem; intervention, control or comparison, outcome) method as reference [29].
The final search terms are as follows: nutrition* or diet* or “physical activ*” or exercis* AND (workplace or worksite) and (health* or wellness or program* or intervention of “health promotion”) AND staff or employee* or provider* or nurse* or doctor* or midwi* or “shift work” AND Survey* or questionnaire* or “randomi?ed control trial” or stud* or interview* or “focus group*” AND “primary health*” or hospital* NOT patient*.
Note: * at the end of keywords will find variations of the word;? will look for alternate spelling of the word [30]. Refer to Supplementary Table 1 for search strategy outline.
Systematic searching of the literature was conducted across electronic databases CINAHL Complete, MEDLINE Complete, Academic Search Complete, Global Health, Health Source Nursing/Academic Edition and PsycINFO, between 3 April 2018 and 17 June 2020. Only peer reviewed, published articles, in English, from 1st January 2004 to 17 June 2020 and generated 551 results.
Inclusion and exclusion criteria
Only peer reviewed, published articles, from 2004 onwards were included in the review. This time frame coincides with the World Health Organization’s Global Strategy on Diet, Physical Activity and Health and when interventions started to become more prevalent in the workplace [31]. Eligible studies met the following criteria: (1) included participants who worked in hospital settings; (2) implemented dietary or physical activity intervention in the workplace; (3) reported on diet (fruit, vegetable, high fat and sugary foods), physical activity, anthropometric measurements, blood pressure, stress levels, or musculoskeletal outcomes. Stress and musculoskeletal outcomes were included given the potential relationship with stress, shift work and unhealthy eating practices in nurses [32] and the link between physical activity and musculoskeletal outcomes [33]. All studies were included except for reviews.
Studies were excluded if; staff and patients were combined as one intervention group and were not able to be disaggregated into the staff subpopulation only; the study involved multiple worksites including a hospital but failed to distinguish between the worksite settings in their analysis and reporting of findings; the setting was outside of a hospital; the outcomes focused on perceptions of an intervention; interventions took place in community settings; outcomes were not included in the inclusion criteria; there was no control group reported; the intervention was under 12 weeks duration as 12 weeks is suggested as a minimum length to see behaviour changes from an obesity prevention intervention [34]; did not report primary data; the publication was a review and if the study was not reported in English.
Study selection
A systematic review software, Covidence [35], was used to screen the electronic articles and keep record of the results. Two authors, VW and KAB, separately conducted screening of the titles and abstracts against the inclusion/exclusion criteria. All studies included for full text screening had their references scanned by VW and nine additional studies were located for screening. Any conflicts that arose from the screening process were reviewed by both authors again until all conflicts could be resolved. Included studies underwent a full text screening, independently by VW and KAB, to further ascertain that the chosen studies met the inclusion criteria.
Data extraction and quality assessment of studies
Included studies had their key characteristics extracted and were collated into Table 1. Data was extracted by one reviewer (VW) and checked for accuracy and completeness by a second reviewer (KAB). The Integrated quality Criteria for the Review Of Multiple Study designs (ICROMS) tool was used for the quality assessment (Table 2) in this review as it covers multiple study designs (randomised control trials, non-randomised control trials, controlled before-and-after, non-controlled before-and-after studies), yet it draws on thorough criteria for its analysis [36]. For the cross-sectional study that fell outside of the ICROMS tool, the National Heart and Blood Institute Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies was used [37]. VW and KAB conducted the quality analysis independently. Any disagreements were resolved by discussion until a consensus decision was made.
Data synthesis and analysis
Firstly, the table of key characteristics was used to assess any commonalities and differences between the studies. Secondly, the quality analysis was used to compare the strengths and weaknesses between the studies. Thirdly, a narrative synthesis was conducted, assessing the interventions by strategy.
Results
Search and selection findings
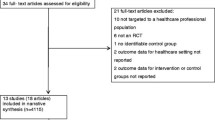
The search generated 551 journal articles. Following the title and abstract screening, the full text of 119 articles were screened against the inclusion/exclusion criteria. This resulted in 18 articles progressing to quality assessment (see Fig. 1) for inclusion in the review corpus.
Summary of studies
Studies included in the review consisted of five controlled-before-after studies (CBA), 12 randomised control trials (RCT) and one cross-sectional study (Table 1). Eight studies were from United States of America along with one study from each of Canada, Germany, Norway, United Kingdom, Japan, Netherlands, Australia, Israel, Taiwan and Ireland. The sample sizes ranged from 11 to 806 participants. The lengths of the interventions ranged from 3 months to 24 months and targeted combinations of interventions aiming to improve nutrition, physical activity, weight control, musculoskeletal injury risk and stress among hospital staff.
Quality assessment findings
Questions score two marks for meeting the quality criteria, one mark if the information is unclear, and 0 if the criteria has not been met. The ICROMS decision matrix was used to identify if studies had met the minimum criteria, the mandatory criteria, as well as a global score, to determine if the study was of high quality (Table 3) [36]. Six studies were considered of high quality, and met the ICROMS mandatory and global criteria for their respective study designs [13, 39, 43, 46, 47, 50]. Nine studies met the minimum score but failed to meet the mandatory criteria [18, 38, 40, 41, 44, 48, 49, 51, 52] and two studies were low quality [42, 45].
The quality analysis for the cross-sectional study by Geaney et al. [14] was analysed with the National Institutes of Health’s National Heart Lung and Blood Institute Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [37], was also low quality (Table 3). Questions 1, 2, and 4, regarding clear aims, study population, selection process, time period, and prespecified inclusion/exclusion criteria, were strong. There was no sample size justification mentioned and no baseline measures were conducted. Time frame, repeated exposure assessment, outcome measures, blinding of outcome assessors and statistical analyses were all insufficient and data was completed by self-report. Question 8 and 13, regarding exposure levels and loss to follow-up, were not applicable. Question 3 on participation rate could not be determined. The overall rating for this study was poor.
The ICROMS tool revealed that managing bias in sampling or between groups proved challenging for the RCT studies with nine producing adequate sequence generation [18, 38, 39, 42,43,44, 46,47,48] and six studies implementing adequate allocation concealment [18, 38, 39, 43, 46, 47]. Four RCTs used blinding to manage bias in their outcome measures [39, 43, 46, 47], five RCTs completed reliable follow-up of participants to protect against exclusion bias [39, 40, 43, 44, 46] and five studies did not address this issue [18, 42, 45, 47, 48]. All of the CBA studies used baseline measures to protect against selection bias however only two CBA studies employed a method to protect against contamination between study groups [13, 50].
Process analysis was adequately presented in 16 of the 17 RCT/CBA studies. Characterised as: sufficiently rigorous, implemented reliable outcome measures, provided clear and justified conclusions, blinded assessment of their primary outcome measures, and addressed ethical issues. All the studies addressed the issue of incomplete data and were free from selective outcome reporting. Although none of the studies explicitly reported that they protected against detection bias, none of the interventions were likely to affect data collection. Thirteen studies addressed their limitations adequately [13, 18, 39,40,41, 43,44,45,46,47, 49, 50, 52], nine studies were free from other forms of bias [13, 38, 39, 43, 46,47,48,49,50], and two studies had a high risk of other bias [42, 45].
Diet-related interventions
Two studies focused on interventions to decrease the intake of unhealthy food and drinks from their hospital cafeteria [14, 42]. A RCT by Lowe et al. [42] used food labelling, subsidies on low-energy-density foods, addition of more healthy foods to the menu, and four nutritional educational sessions to increase the intake of low-energy-dense foods. Their results showed no significant between-group differences (the difference between the control group and intervention group) but reported significant decrease in energy intake, fat intake and increase in energy from carbohydrates, across both groups. It is possible that the between-group differences were minimised as both groups received a baseline intervention, a coloured food labelling system paired with an increased selection of healthy food items such as steamed vegetables or low-fat options. Geaney et al. [14] conducted a repeat cross-sectional study of a catering initiative that saw significant decreases in consumption of fat, salt and sugar in the intervention group compared with the control group. These findings coincide with those by Gorton et al. [15] who found their environmental strategy, installing healthier vending machines in hospitals, produced decreases energy, fat and sugar intake.
Physical activity interventions
Six studies tested physical activity promoting strategies including supervised/unsupervised fitness classes [18], aerobic exercise training [38, 52], endurance training [46], resistance training classes [43], Thai Chi [45], pedometers [13, 49], personalised physical activity counselling [50] and educational materials [49]. Four RCTs showed significant improvements in oxygen uptake performance compared to controls through aerobic exercise classes, resistance training and endurance training [18, 38, 43, 46].
Twelve studies measured body mass index (BMI), of which three found significant decreases in BMI [18, 39, 52]. None of the studies reported significant differences in blood pressure. Matsugaki et al. [43] and Stenner et al. [46] met all the mandatory criteria from the quality assessment however Matsugaki’s study had a small sample size and the findings regarding improved fitness levels in the supervised exercise group may not be generalisable. Stenner et al. [46] revealed some positive improvements in fitness and work ability index in the intervention (endurance training) group, however most of the participants in the study were sedentary and there was a high drop out in the intervention compared to the control group. Hewitt et al. [38] and Yuan et al. [52] also had small sample sizes. Borg et al. [49] showed no between-group differences of walking minutes completed and total physical activity however did find a significant increase in moderate-to-vigorous physical activity (MVPA) in the intervention group compared to the control group, as well as a positive association with pedometer use and meeting public health recommendations [14]. Palumbo et al. [45] found that Tai Chi improved all outcome measures across the board; no time-off taken at work, an increase in productivity, and improvements in functional reach; however not at a significant level. Hamm et al. [50] showed that a personal physical activity counselling program may improve physical activity over 4 months, but it was dependent on those individuals with gym memberships.
Diet-related and physical activity interventions
Six studies focused on interventions consisting of both nutrition and physical activity outcome measures and all had large participant numbers [13, 39, 40, 44, 47, 48]. Five of these studies took place in USA [13, 39, 40, 44, 48]. Interventions included social marketing campaigns, the StairWELL campaign, physical activity challenges, motivational coaches, educational materials and seminars, website access, pedometers, food labelling and nutritional signage [13, 39, 40, 44, 47, 48]. LaCaille et al. [13], Kullgren et al. [39] and Strijk et al. [47] were high quality studies and the remaining three studies were of moderate quality.
LaCaille et al. [13] showed that their pedometers and StairWELL campaign, combined with food labelling, failed to produce significant between-group differences in BMI, however did significantly increase knowledge on dietary and physical activity behaviours. Lemon et al. [40] also found that their social marketing and StairWELL campaign failed to produce significant impact on BMI. Strijk et al. [47] observed a positive significant difference in fruit intake, need for recovery and sports activity, but not in MVPA, VO2max, or mental health, from their intervention. Kullgren et al. [39] included a financial incentive component which produced a significant decrease in weight compared to baseline in one intervention group but showed no significant differences in dietary or physical behaviours. Østbye et al. [44] found marginal changes in diet and physical activity and Thorndike et al. [48] found a decrease in body weight and improvements in dietary and physical activity behaviours, although no significant between-group differences.
Diet and/or physical activity and stress reduction interventions
Two studies implemented interventions consisting of gym access, workshops (on weight, diet, physical activity, stress), goal setting and motivational counselling [41, 51]. Low et al. [41] saw minimal changes in stress levels, exercise intensity and weight loss compared to the control group, from their intervention of goal setting and motivational counselling. Sallon et al. [51], a study from Israel, found that their intervention group who attended weekly sessions on topics such as mindfulness, relaxation, body awareness, listening circles, and trigger point massage, displayed a significant increase in their physical well-being, mental well-being, energy, ability to relax, ability to cope with stress inside and outside of the workplace.
Barriers and enablers
Analysis of the included studies revealed enablers and barriers to improving health behaviours of hospital staff. Enablers included physical activity programs being run outside of work hours [18]; during work hours [46]; the use of workplace health club [46]; supervision influencing higher adherence to training sessions [38] and intensity (but not adherence) [43]; financial incentives [39]; regular (e.g. weekly) encouragement [41]; regular communication [49]; tailored programs [46, 47]; supervised exercise programs [38, 43, 46]; motivational/counselling [41, 50, 51]; coaching [44, 47, 49]; influential employees [13]; persuasive messaging [13, 40]; pedometers [13]; convenience of accessing a program based on the internet [48].
Lack of time to participate was a common barrier [40, 43]. Other reported barriers included stress, limited flexibility during to participate (e.g. particularly for clinical staff/patient centred care staff), staffing challenges, shift work (i.e. shift workers potentially isolated from participating), organisational culture and environment [40], long commute times to and from work [41], initial high motivation to participate but in reality found it difficult to comply/continue with the program [41], environmental changes were slow [13], cost to employers to make changes [13], and some employers feared suggested changes may upset employees/customers [13]. High intensity activities resulted in a decrease in participation and were associated with more participant complaints about heavy workload [40, 43].
Discussion
Main findings
This systematic review sought to describe workplace interventions aiming to improve the health of staff in hospital settings. There were 18 studies that met the inclusion criteria in the study period between 2004 and 2020. Several studies were able to generate changes in modifiable risk among hospital staff for knowledge on dietary and physical activity behaviours, diet (fruit intake), physical activity (including cardiorespiratory fitness, fitness scores, flexibility), anthropometry (weight, body fat). In contrast, several studies were unable to produce significant improvements diet (energy intake, fat intake), physical activity (e.g. walking minutes, MVPA, VO2max, exercise intensity), anthropometry (weight), mental health, and stress. Reducing BMI proved difficult with the majority of studies unable to produce a significant decrease in BMI; and none of the studies reported significant differences in blood pressure. Six high quality studies [13, 39, 43, 46, 47, 50] provided strong evidence that workplace interventions in a hospital setting can increase in knowledge about health behaviours, improve diet, physical activity, fitness and cardiorespiratory fitness, and decrease body weight and body fat. The review uncovered numerous strategies employed to increase positive health behaviours in hospital settings focusing on diet and physical activity in isolation; or combined. The strategies included physical activity-based, financial, environmental, motivational, educational or multi-component. Intervention and study design quality were imperative to both the success and the evaluation of these interventions. Previous evaluations have suggested that low quality studies often produce inconsistent findings [21, 27] or may underestimate the intervention effects [53], compared to reviews with moderate to high quality studies that often achieve significant outcomes [54].
Reported enablers in the studies examined
Motivational strategies and counselling
Strategies that were affective in motivating change included role modelling, persuasive messaging, counselling, coaches and supervised exercise programs. Influential employees improved staff health behaviours and produced a flow on effect that continued after the intervention, for example requesting policy changes to install bike racks [13]. Hamm et al. [50] reflected that participant choice into the group activity facilitated better adherence and reflects life in the real world; and the ability to tailor counselling based upon Transtheoretic Model of Behaviour Change to be key enablers. A meta-analysis of workplace interventions in other settings agreed that motivational strategies increased physical activity [55]. Similarly, in this review there was good evidence that the inclusion of a motivation strategy could enhance positive outcomes. Personal, tailored guidance, with regular contact was thought to be a strong influence on compliance and motivation as problems could be detected and solved early [46]. This is similar to other research in primary care settings which have demonstrated motivational strategies to increase physical activity levels [56] and hospitals utilising motivational strategies being more likely to implement policies and practices more successfully [57].
Financial reward
Positive health behaviours can be increased through financial incentives, via subsidies of healthy food and drink options, or through financial reward for performing healthy behaviours such as exercise [39, 58]. Group incentives, where a financial reward was shared between group members, were more effective than individual incentives (no sharing of the reward), at improving healthy behaviours [39]. This finding was unique in that other studies have focused on individual rewards and subsidies [54, 59]. Financial incentive studies are scarce in the literature but are often largely effective, with subsidies of 35 to 50% shown to produce significant increases in fruit and vegetable purchases [54, 58]. This review found that a subsidy was unable to produce significant improvements in fruit and vegetable consumption, however the included subsidy intervention was implemented on top of an already established intervention (food labelling and introduction of low-energy-dense food options). This result may have caused “background noise”, dampening down their between-group intervention effects [60]. Furthermore, Finkelstein et al. [61] caution that although financial incentives appear to be effective, they often fail to maintain healthy behaviours once the incentives have ceased. However, financial interventions have been successful in other health areas such as smoking cessation [59]. To ensure long term effectiveness of workplace interventions, sustainability of positive behaviour change would also need to be addressed.
Multi-component interventions
Multi-component interventions were common in this review, with the majority of studies adopting this type of approach. Multi-component strategies were more likely to produce successful health outcomes (e.g. increased physical activity or increased vegetable intake) and often paired a motivational strategy with either an environmental, financial or educational strategy. For example, physical activity and healthy eating were increased when motivation was paired with a supportive environment and policy action [40]. Likewise, other researchers agree that multi-component strategies significantly improve staff health outcomes [53, 62]. Most of the multi-component studies incorporated motivational strategies, for example, designated “influential” staff members whose aim was to influence health practices and social norms and tended to increase their own positive health behaviours and considered themselves a role model to other staff [13]. There was no evidence in this review that certain pairings of strategies were more beneficial than other combinations. The heterogeneity of the workforce may require multi-component strategies to attain adequate levels of participant involvement [40].
Reported barriers in the studies examined
Barriers around time pressures, work schedules, work related fatigue and lack of flexibility in the workplace were frequent [40, 41, 43, 51]. For example, Lemon et al. [40] found that participants on second and third shifts were less likely to take part in intervention activities. The limited capacity of health staff to attend workplace interventions, due to their demanding job roles, may signify that structural components and personalised interventions should be incorporated to increase participation rates [21, 63]. In addition, low participation rates may signal high participant burden [44]. This review observed high intensity activities resulted in decreased participation, and increased participant complaints about heavy workload [40, 43]. Likewise, long interventions, for example maintenance interventions (an intervention following a previous intervention), were suggested to diminish participant motivation to complete the intervention [48]. High participant burden was also observed by a similar systematic review [21]. Nutritional interventions such as food labelling initiatives may not be a burden on participants but can be a burden on workers who deliver the intervention, for example LaCaille et al. referred to how the process of labelling all the foods in the cafeteria was time consuming and some cafeteria employees had low adherence updating the labels [13].
To overcome the barriers listed above, structural measures could be implemented in hospitals to encourage a supportive environment and enhance benefits to staff. Incorporating workplace policy such as decreased healthcare rates or monetary rewards could act as a motivator [40]. The European Network for Workplace Health Promotion recommends that successful dissemination of workplace interventions requires implementation of good policies to ensure organisational commitment is achieved as well as active participation [63]. Furthermore, a universal framework with specified standards for implementation and measuring outcomes is needed to ensure adequate evaluation of programs can be properly conducted [64].
Culture in the workplace can influence participation [65] and management’s flexibility (or inflexibility) regarding intervention strategies can have a significant impact on whether participants are able to actively participate [66, 67]. Having exercise facilities/health club/gym co-located within the hospital setting, may also give staff more flexibility to exercise around shifts. Nutritional interventions such as healthy catering/food policies may also change social and work environment norms to encourage healthy eating. A recent example of this is the Alfred Health, a metropolitan health service in Melbourne, Australia, who implemented state government healthy choice guidelines to improve the healthiness of food options (i.e. retail, vending machines) and catering using the traffic light system and an increase in sales of green/amber (healthier) products and reduction in red (unhealthy) products since implementation [68].
Limitations of the studies included in this review
The studies in this review were not without their limitations. A number of the studies reviewed presented relatively small sample size in relatively unique hospital environments (e.g. emergency department); and high attrition rates [18, 42, 45]. Concerns of self-selection (e.g. healthy individuals being less interested in health interventions [50] or participants who already have a very high level of physical activity) resulting in a ceiling effect [46] or the healthy worker effect [18, 47]; gender imbalance [50] and the Hawthorne effect need to be considered. The already existing health knowledge of hospital staff may also impact the finding [50].
Managing bias in the sampling process proved to be challenging for many of the studies in this review. Contamination between intervention groups due to close quarters was at times difficult to control [42, 51, 52]. Comparable reviews have stressed that a common downfall of workplace intervention studies is the lack of stringent methodology [27, 69]. Guidelines for an approved methodology and reporting on workplace interventions could be investigated to derive more significant findings in the workplace intervention field.
All the studies in this review included body measurements and the completion of questionnaires in their data collection. Although objective measures are reliable, questionnaires are inherently prone to recall and desirability bias [70]. Participants filling out questionnaires may suffer from inaccurate recall or unconsciously (or consciously) find themselves over-reporting healthy behaviours and under-reporting poor health behaviours. Research shows that individuals often have a difficult time interpreting their own weight status and may feel obliged to record a figure that is closer to social norms [71]. There is a gap in measuring the sustainability of the intervention effects, and future studies should measure for sustained impact in the long term [46] at least 1 year post-intervention.
Strengths and limitations of this review
A key strength of this review was the systematic approach used to identify studies according to clear inclusion/exclusion criteria. This review’s inclusion criteria aimed to target higher quality evidence by only examining interventions over 12 weeks that used control groups [34] which increases the strength of the findings. Another advantage was that 11/18 studies implemented follow-up periods of over 6 months [13, 18, 39,40,41,42, 44, 46, 48, 49, 51]. Sallon et al. [51] state that long interventions increase flexibility by absorbing obstacles and provide a more supportive framework that can account for unanticipated events that arise in hospital environments.
The review has limitations, notably non-English papers were excluded and only six databases were interrogated. Studies published in other languages were excluded and although the most common health databases were searched, the catalogues are not exhaustive of all listings that may publish research on workplace interventions for staff in hospital settings. Hand searching was employed to mitigate this risk and this process identified an additional nine papers. Grey literature was excluded which may limit findings. Two reviewers independently assessed the quality of the studies. Due to the large variance between the studies’ primary outcome measures; comparison of outcomes by meta-analysis was not possible. Similarly, due to the diversity and combination of strategies employed, which parts of the intervention had the greatest effect was not possible.
Implications and recommendations for future workplace interventions targeting staff in a hospital setting
The various intervention strategies used to improve health outcomes of hospital staff fills a knowledge gap of best practice for workplace interventions. The range in quality of the studies reviewed point to the need for high-quality research in the field. Studies in the current review largely had broad target populations i.e. “hospital employees” and it is recommended to expand future research into specific occupational groups within hospital settings, to fully understand how to best support healthy behaviours in each of these occupational groups (e.g. administration, laboratory, nursing staff etc). Further research would prove beneficial to fully understand the contribution that workplace interventions can have on creating positive behaviour change in staff. As expressed in previous research, agreement on a universal framework or standardised outcome measures could improve applicability of workplace intervention studies and should be investigated further [21, 27]. This addition would also enable meta-analysis to further determine high-quality evidence. The utilisation of structural components, sustainable policy, and context, could also help to achieve high participation rates and improve health outcomes [21, 63].
This review adds to the current body of research as its findings were only derived from studies with a control group and largely consisted of RCTs. Multi-component strategies, motivational strategies, and financial incentives were able to achieve moderate to high quality evidence that workplace interventions significantly improved positive health behaviour change or improved awareness of dietary intake and physical activity habits of staff. These findings concur with other researchers who have found multi-component strategies to be effective at improving health of staff in the workplace [27, 53].
The proportion of health care workers with overweight an obesity is too high. Along with the hospital labour force being largely made up of females; with demanding work tasks and rosters; and declines in physical activity; targeted efforts to promote physical activity [46] as part of a multi-component intervention tackling nutrition and the built environment is needed. The creation of a health promoting workplace is important to achieve a healthy, qualified and motivated workforce; and to achieve this, it will require the participation of employees, management and stakeholders to collectively act on promoting health [6]. An in depth understanding of and enabling staff to overcome the barriers they face in in eating healthy and being physically active is essential to improve the success of workplace interventions in hospital settings, and to improve the health status of hospital staff. Adults spend a large proportion of time in workplace settings. It is therefore critical that workplaces (including physical and psychosocial environments) are conducive to good health [72]. A healthy workplace is achievable with workplace policies supporting good health, supportive environments and evidence-based effective healthy practices [72]. There should be a partnership between employers and employees to protect, promote and sustain good health, safety and wellbeing [72].
Conclusion
Multi-component strategies, motivational strategies, and financial incentives were particularly effective methods at improving health behaviours of staff in hospital settings. However, difficulty with the heterogeneity of the studies, self-select bias, and some small sample sizes may limit the generalisability of any conclusions. More research is needed from high-quality, randomised control trials to gain further insight into the benefits of workplace interventions aimed at staff in hospital settings. Future studies should focus on incorporating more stringent methodology to address potential bias and longer follow-up time.
Availability of data and materials
All data generated or analysed during this study are included in this published article. Full papers from where data was extracted can be found in via Entrez PubMed and other databases listed in the methods section.
Abbreviations
- BMI:
-
Body Mass Index
- MVPA:
-
Moderate-to-vigorous physical activity
References
Obesity and overweight [http://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight ].
Australian Bureau of Statistics: National Health Survey: First Results, 2017–18. In.; 2018.
Opie CA, Haines HM, Ervin KE, Glenister K, Pierce D. Why Australia needs to define obesity as a chronic condition. BMC Public Health. 2017;17(1):500.
Allen L, Thorpe K, Joski P. The effect of obesity and chronic conditions on Medicare spending, 1987-2011. Pharmacoeconomics. 2015;33(7):691–7.
Witten K, Pearce J: Geographies of Obesity. Environmental Understandings of the Obesity Epidemic: Routledge; 2010.
Workplace health promotion [https://www.who.int/occupational_health/topics/workplace/en/].
Belkic K, Nedic O. Night work, total occupational burden and cancer/cardiovascular risk factors in physicians. Med Pregl. 2012;65(11–12):461–9.
Aneni EC, Roberson LL, Maziak W, Agatston AS, Feldman T, Rouseff M, et al. A systematic review of internet-based worksite wellness approaches for cardiovascular disease risk management: outcomes, challenges & opportunities. PLoS One. 2014;9(1):e83594.
Bogossian FE, Hepworth J, Leong GM, Flaws DF, Gibbons KS, Benefer CA, et al. A cross-sectional analysis of patterns of obesity in a cohort of working nurses and midwives in Australia, New Zealand, and the United Kingdom. Int J Nurs Stud. 2012;49(6):727–38.
Genc A, Kahraman T, Goz E. The prevalence differences of musculoskeletal problems and related physical workload among hospital staff. J Back Musculoskelet Rehabil. 2016;29(3):541–7.
Blake H, Mo PK, Lee S, Batt ME. Health in the NHS: lifestyle behaviours of hospital employees. Perspect Public Health. 2012;132(5):213–5.
Dawson J, Dwyer JJ, Evers S, Sheeshka J. Eat smart! Workplace cafeteria program evaluation of the nutrition component. Can J Diet Pract Res. 2006;67(2):85–90.
LaCaille LJ, Schultz JF, Goei R, LaCaille RA, Dauner KN, de Souza R, et al. Go!: results from a quasi-experimental obesity prevention trial with hospital employees. BMC Public Health. 2016;16:171.
Geaney F, Harrington J, Fitzgerald A, Perry I. The impact of a workplace catering initiative on dietary intakes of salt and other nutrients: a pilot study. Public Health Nutr. 2011;14(8):1345–9.
Gorton D, Carter J, Cvjetan B, Ni Mhurchu C. Healthier vending machines in workplaces: both possible and effective. N Z Med J. 2010;123(1311):43–52.
Hess I, Borg J, C. R: Workplace nutrition and physical activity promotion at Liverpool Hospital. . Health Promot J Austr 2011(Apr;22(1)):44–50.
Blake H, Gartshore E. Workplace wellness using online learning tools in a healthcare setting. Nurse Educ Pract. 2016;20:70–5.
Barene S, Krustrup P, Brekke OL, Holtermann A. Soccer and Zumba as health-promoting activities among female hospital employees: a 40-weeks cluster randomised intervention study. J Sports Sci. 2014;32(16):1539–49.
Edwardson CL, Yates T, Biddle SJH, Davies MJ, Dunstan DW, Esliger DW, et al. Effectiveness of the stand more AT (SMArT) work intervention: cluster randomised controlled trial. BMJ. 2018;363:k3870.
Nicholls R, Perry L, Duffield C, Gallagher R, Pierce H. Barriers and facilitators to healthy eating for nurses in the workplace: an integrative review. J Adv Nurs. 2017;73(5):1051–65.
Torquati L, Pavey T, Kolbe-Alexander T, Leveritt M. Promoting diet and physical activity in nurses. Am J Health Promot. 2017;31(1):19–27.
Guillaumie L, Boiral O, Champagne J. A mixed-methods systematic review of the effects of mindfulness on nurses. J Adv Nurs. 2017;73(5):1017–34.
Rudaz M, Twohig MP, Ong CW, Levin ME. Mindfulness and acceptance-based trainings for fostering self-care and reducing stress in mental health professionals: A systematic review. J Contextual Behav Sci. 2017;6(4):380–90.
Li H, Cheng B, Zhu XP. Quantification of burnout in emergency nurses: a systematic review and meta-analysis. Int Emerg Nurs. 2018;39:46–54.
O'Connor K, Muller Neff D, Pitman S. Burnout in mental health professionals: a systematic review and meta-analysis of prevalence and determinants. Eur Psychiatry. 2018;53:74–99.
Malik SH, Blake H, Suggs LS. A systematic review of workplace health promotion interventions for increasing physical activity. Br J Health Psychol. 2014;19(1):149–80.
Maes L, Van Cauwenberghe E, Van Lippevelde W, Spittaels H, De Pauw E, Oppert JM, et al. Effectiveness of workplace interventions in Europe promoting healthy eating: a systematic review. Eur J Pub Health. 2012;22(5):677–83.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647.
da Costa Santos CM, de Mattos Pimenta CA, Nobre MR. The PICO strategy for the research question construction and evidence search. Rev Lat Am Enfermagem. 2007;15(3):508–11.
Planning your search [https://www.deakin.edu.au/library/skills-for-study/planning-your-search].
World Health Organization. Global strategy on diet, physical activity and health. Geneva; 2004.
Buss J. Associations between obesity and stress and shift work among nurses. Workplace Health & Safety. 2012;60(10):453–8.
Bowden Davies KA, Pickles S, Sprung VS, Kemp GJ, Alam U, Moore DR, et al. Reduced physical activity in young and older adults: metabolic and musculoskeletal implications. Ther Adv Endocrinol Metab. 2019;10:2042018819888824.
Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;12:CD001871.
Veritas Health Innovation Ltd: Covidence systematic review software. In. Melbourne, Australia; 2018.
Zingg W, Castro-Sanchez E, Secci FV, Edwards R, Drumright LN, Sevdalis N, et al. Innovative tools for quality assessment: integrated quality criteria for review of multiple study designs (ICROMS). Public Health. 2016;133:19–37.
Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. [https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort].
Hewitt JA, Whyte GP, Moreton M, van Someren KA, Levine TS. The effects of a graduated aerobic exercise programme on cardiovascular disease risk factors in the NHS workplace: a randomised controlled trial. J Occup Med Toxicol. 2008;3:7.
Kullgren JT, Troxel AB, Loewenstein G, Asch DA, Norton LA, Wesby L, et al. Individual- versus group-based financial incentives for weight loss: a randomized, controlled trial. Ann Intern Med. 2013;158(7):505–14.
Lemon SC, Zapka J, Li W, Estabrook B, Rosal M, Magner R, et al. Step ahead a worksite obesity prevention trial among hospital employees. Am J Prev Med. 2010;38(1):27–38.
Low V, Gebhart B, Reich C. Effects of a worksite program to improve the cardiovascular health of female health care workers. J Cardiopulm Rehabil Prev. 2015;35(5):342–7.
Lowe MR, Tappe KA, Butryn ML, Annunziato RA, Coletta MC, Ochner CN, et al. An intervention study targeting energy and nutrient intake in worksite cafeterias. Eat Behav. 2010;11(3):144–51.
Matsugaki R, Kuhara S, Saeki S, Jiang Y, Michishita R, Ohta M, et al. Effectiveness of workplace exercise supervised by a physical therapist among nurses conducting shift work: a randomized controlled trial. J Occup Health. 2017;59(4):327–35.
Ostbye T, Stroo M, Brouwer RJ, Peterson BL, Eisenstein EL, Fuemmeler BF, et al. Steps to health employee weight management randomized control trial: short-term follow-up results. J Occup Environ Med. 2015;57(2):188–95.
Palumbo MV, Wu G, Shaner-McRae H, Rambur B, McIntosh B. Tai chi for older nurses: a workplace wellness pilot study. Appl Nurs Res. 2012;25(1):54–9.
Stenner HT, Eigendorf J, Kerling A, Kueck M, Hanke AA, Boyen J, et al. Effects of six month personalized endurance training on work ability in middle-aged sedentary women: a secondary analysis of a randomized controlled trial. J Occup Med Toxicol. 2020;15:8.
Strijk JE, Proper KI, van der Beek AJ, van Mechelen W. A worksite vitality intervention to improve older workers' lifestyle and vitality-related outcomes: results of a randomised controlled trial. J Epidemiol Community Health. 2012;66(11):1071–8.
Thorndike AN, Sonnenberg L, Healey E, Myint UK, Kvedar JC, Regan S. Prevention of weight gain following a worksite nutrition and exercise program: a randomized controlled trial. Am J Prev Med. 2012;43(1):27–33.
Borg J, Merom D, Rissel C. Staff walking program: a quasi-experimental trial of maintenance newsletters to maintain walking following a pedometer program. Health Promot J Austr. 2010;21(1):26–32.
Hamm NC, Kehler DS, Hay JL, Stammers AN, Strachan SM, Bouchard DR, et al. A quasi-experimental study examining the impact and challenges of implementing a fitness-based health risk assessment and a physical activity counseling intervention in the workplace setting. Health Serv Res Manag Epidemiol. 2019;6:2333392819884183.
Sallon S, Katz-Eisner D, Yaffe H, Bdolah-Abram T. Caring for the caregivers: results of an extended, five-component stress-reduction intervention for hospital staff. Behav Med. 2017;43(1):47–60.
Yuan SC, Chou MC, Hwu LJ, Chang YO, Hsu WH, Kuo HW. An intervention program to promote health-related physical fitness in nurses. J Clin Nurs. 2009;18(10):1404–11.
Schroer S, Haupt J, Pieper C. Evidence-based lifestyle interventions in the workplace--an overview. Occup Med (Lond). 2014;64(1):8–12.
Hendren S, Logomarsino J. Impact of worksite cafeteria interventions on fruit and vegetable consumption in adults. Int J Workplace Health Manag. 2017;10(2):134–52.
Hutchinson AD, Wilson C. Improving nutrition and physical activity in the workplace: a meta-analysis of intervention studies. Health Promot Int. 2012;27(2):238–49.
Gagliardi AR, Abdallah F, Faulkner G, Ciliska D, Hicks A. Factors contributing to the effectiveness of physical activity counselling in primary care: a realist systematic review. Patient Educ Couns. 2015;98(4):412–9.
Sharma S, Winston P, Jyothi V, Baun W, Perkison B, Phipps M, et al. Evaluation of worksite policies and practices promoting nutrition and physical activity among hospital workers. Int J Workplace Health Manag. 2016;9(1):46–62.
Patsch AJ, Smith JH, Liebert ML, Behrens TK, Charles T. Improving healthy eating and the bottom line: impact of a Price incentive program in 2 hospital cafeterias. Am J Health Promot. 2016;30(6):425–32.
Giles EL, Robalino S, McColl E, Sniehotta FF, Adams J. The effectiveness of financial incentives for health behaviour change: systematic review and meta-analysis. PLoS One. 2014;9(3):e90347.
Bolton KA, Kremer P, Gibbs L, Waters E, Swinburn B, de Silva A. The outcomes of health-promoting communities: being active eating well initiative-a community-based obesity prevention intervention in Victoria, Australia. Int J Obes. 2017;41(7):1080–90.
Finkelstein EA, Haaland BA, Bilger M, Sahasranaman A, Sloan RA, Nang EEK, et al. Effectiveness of activity trackers with and without incentives to increase physical activity (TRIPPA): a randomised controlled trial. Lancet Diabetes Endocrinol. 2016;4(12):983–95.
Christensen JR, Overgaard K, Carneiro IG, Holtermann A, Sogaard K. Weight loss among female health care workers--a 1-year workplace based randomized controlled trial in the FINALE-health study. BMC Public Health. 2012;12:625.
Guazzi M, Faggiano P, Mureddu GF, Faden G, Niebauer J, Temporelli PL. Worksite health and wellness in the European union. Prog Cardiovasc Dis. 2014;56(5):508–14.
Motalebi GM, Keshavarz Mohammadi N, Kuhn K, Ramezankhani A, Azari MR. How far are we from full implementation of health promoting workplace concepts? A review of implementation tools and frameworks in workplace interventions. Health Promot Int. 2018;33(3):488–504.
Cole JA, Tully MA, Cupples ME. "they should stay at their desk until the work's done": a qualitative study examining perceptions of sedentary behaviour in a desk-based occupational setting. BMC Res Notes. 2015;8:683.
Fitzgerald S, Geaney F, Kelly C, McHugh S, Perry IJ. Barriers to and facilitators of implementing complex workplace dietary interventions: process evaluation results of a cluster controlled trial. BMC Health Serv Res. 2016;16:139.
Bredahl TV, Saervoll CA, Kirkelund L, Sjogaard G, Andersen LL. When intervention meets organisation, a qualitative study of motivation and barriers to physical exercise at the workplace. ScientificWorldJournal. 2015;2015:518561.
Healthy Choices [https://www.alfredhealth.org.au/about/healthy-communities/healthy-food/healthy-choices].
Verweij LM, Coffeng J, van Mechelen W, Proper KI. Meta-analyses of workplace physical activity and dietary behaviour interventions on weight outcomes. Obes Rev. 2011;12(6):406–29.
Al-Eisa E, Alghadir AH, Iqbal ZA. Measurement of physical activity in obese persons: how and why? A review J Phys Ther Sci. 2016;28(9):2670–4.
Burke MA, Carman KG: You can be too thin (but not too tall): Social desirability bias in self-reports of weight and height. Econ Hum Biol 2017, 27(Pt A):198–222.
Burton J: WHO Healthy Workplace Framework and Model: Background and Supporting Literature and Practices In.; 2010.
Acknowledgements
The study was primarily conducted by VW as part of a Master of Public Health Degree. We gratefully acknowledge KAB and PF who kindly supervised all aspects of the study and provided constructive comments and suggestions throughout the entire review process. We are thankful to SA who provided invaluable critique of the draft manuscripts.
Funding
KAB, PF and SA were supported by a NHMRC Partnership Project titled “Whole of Systems Trial of Prevention Strategies for childhood obesity: WHO STOPS childhood obesity” (APP1114118). The funding body was not involved in the design of the study; the collection, analysis, or interpretation of data; nor in writing this manuscript.
Author information
Authors and Affiliations
Contributions
VW, KAB and PF contributed to the conceptualisation, methodology and writing. VW and KAB conducted the formal analysis. KAB and PF contributed to supervision. SA, KAB, PF and VW contributed to the writing and review editing. All authors approved the final publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Worley, V., Fraser, P., Allender, S. et al. Describing workplace interventions aimed to improve health of staff in hospital settings – a systematic review. BMC Health Serv Res 22, 459 (2022). https://doi.org/10.1186/s12913-021-07418-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-021-07418-9