Abstract
Background
Multiple pro-competition policies were implemented during the new round of healthcare reform in China. Differences in conditions’ complexity and urgency across diseases associating with various degrees of information asymmetry and choice autonomy in the process of care provision, would lead to heterogeneous effects of competition on healthcare expenses. However, there are limited studies to explore it. This study aims to examine the heterogeneous effects of hospital competition on inpatient expenses basing on disease grouping according to conditions’ complexity and urgency.
Methods
Collecting information from discharge data of inpatients and hospital administrative data of Sichuan province in China, we selected representative diseases. K-means clustering was used to group the selected diseases and Herfindahl-Hirschman Index (HHI) was calculated based on the predicted patient flow to measure the hospital competition. The log-linear multivariate regression model was used to examine the heterogeneous effects of hospital competition on inpatient expenses.
Results
We selected 19 representative diseases with significant burdens (more than 1.1 million hospitalizations). The selected diseases were divided into three groups, including diseases with highly complex conditions, diseases with urgent conditions, and diseases with less complex and less urgent conditions. For diseases with highly complex conditions and diseases with urgent conditions, the estimated coefficients of HHI are mixed in the direction and statistical significance in the identical regression model at the 5% level. For diseases with less complex and less urgent conditions, the coefficients of HHI are all positive, and almost all of them significant at the 5% level.
Conclusions
We found heterogeneous effects of hospital competition on inpatient expenses across disease groups: hospital competition does not play an ideal role in reducing inpatient expenses for diseases with highly complex conditions and diseases with urgent conditions, but it has a significant effect in reducing inpatient expenses of diseases with less complex and less urgent conditions. Our study offers implications that the differences in condition’s complexity and urgency among diseases would lead to different impacts of hospital competition, which would be given full consideration when designing the pro-competition policy in the healthcare delivery system to achieve the desired goal.
Similar content being viewed by others
Introduction
In recent decades, competition was introduced in the healthcare market across countries, such as Germany, France, and the United Kingdom, with the objective of improving the efficiency of health care services [1,2,3,4,5,6,7]. The ongoing reform in China aims at promoting access to appropriate health care and controlling cost inflation. Multiple pro-competition policies including enlarging operational autonomy of public hospitals, and encouraging private hospital development [8,9,10], were also implemented during the reform to improve the efficiency of the healthcare delivery system in China [11].
With the implementation of pro-competition policies, the competition impact on healthcare expense has become a hot topic that received considerable attention in recent years [12,13,14,15]. The dispute about the effectiveness of competition in the healthcare market mainly stems from the particularities of the healthcare market [16]. Classical economics clearly predicts market competition would inspire the industry to reduce the value-adjusted price under specific prerequisites. Among them, consumers with enough information about the products or services can freely choose the providers as one of the main premises [17]. However, highly asymmetric information between physicians and patients, and patient’s limited choice autonomy in service selection exists in the healthcare market [16, 18], complicating the effectiveness of competition [19, 20].
The particularities of highly asymmetric information and patient’s limited choice autonomy in the healthcare market would reflect in the process of care provision associating with disease conditions. Patients with highly complex disease conditions, such as multiple complications, would have difficulties in obtaining or understanding the disease and treatment-related knowledge, leading these patients to face greater information asymmetry than the patients with common diseases. Patients who suffer from the disease with urgent conditions, such as acute myocardial infarction, need to be admitted to the hospital for treatment within a very short time, generally selecting the nearest hospital according to treatment capacity, leaving them or their companions limited opportunity to choose hospitals [21]. The prerequisite for market competition to play a role is missing in the above two kinds of diseases, leading to the uncertain impacts of competition for these diseases in the healthcare market. For the diseases of which conditions are generally less complex and less urgent, the information asymmetry and patient’s limited choice autonomy in the process of care provision would not be obvious. The services for these diseases would like the products in the “textbook market”, and competition effectiveness would be predicted by the classical economic theory.
Differences in conditions’ complexity and urgency across diseases associating with various degrees of information asymmetry and choice autonomy in the process of care provision, would lead to heterogeneous effects of competition on healthcare expenses. However, there are limited studies to explore it. Most of the previous studies have not considered the influences of differences in healthcare characteristics [12, 13, 15, 22, 23]. To our knowledge, C Deng and J Pan [19] is the only study considering the influences of differences in healthcare characteristics on the effects of hospital competition on healthcare expenses. Prostatectomies (elective surgery, representing treatments of non-acute common diseases) and appendectomies (emergency surgery, representing treatments of acute common diseases) are selected as the representative surgeries, and they found that greater hospital competition was significantly associated with lower total hospital charges for prostatectomies, while the opposite was true for appendectomies.
To bridge the gap in the literature, our study aims to explore the heterogeneous effects of hospital competition on inpatient expenses basing on disease grouping according to condition’s complexity and urgency. The significance of considering the heterogeneous effects of hospital competition among different diseases groups are as follows: (1) The findings of this study can provide empirical evidence for the influence of disease conditions on the effects of competition, indirectly examining the effects of hospital competition in various degrees of particularities in the healthcare market. (2) To achieve the pro-competition policies’ optimal impact on healthcare systems while minimizing the potential adverse outcomes, the heterogeneous effects of hospital competition among different diseases groups are needed to explore to find out what kinds of disease hospital competition could not play an ideal role in reducing inpatient expenses, providing important policy implications.
Methods
Study area
This study is based on Sichuan province located in southwest China between 26.40°N and 33.68°N latitude, and 98.31°E and 107.99°E longitude [24]. The province consists of 183 counties, and it is China’s fifth-largest province (486,052 km2) in land size, with 83.41 million residents in 2018.
There are great variations in topography, economy, and population distribution within the Sichuan province [25, 26]. In 2018, the maximum population in a county (Wuhou county with 1.87 million residents) was reported more than 65 times of the minimum one (Derong county with 28 thousand residents), while the most developed county (Longquanyi county with GDP about 22,000 dollars per capita) was reported over 14 times compared with the lowest one (Shiqu county with GDP about 1500 dollars per capita). The differences in the distribution of topography, economy, and population among regions would lead to large diversities in the local healthcare development as well as the healthcare market. In 2018, Wuhou county with the most hospitals (109) had more than 20 health technicians per 1000 population, while Jinkouhe county had only 1 hospital with 5.09 health technicians per 1000 population. The uneven distribution of healthcare facilities and medical resources has brought about great variations in the degrees of hospital competition among different regions, thus providing us an ideal opportunity for testing our hypothesisFootnote 1 [16, 25].
Data source
We collected the patient-level information from the inpatient discharge dataset during the period of the fourth quarter of 2018 (from September to December), and hospital-level information from the hospital administrative data in 2018. Both data were managed by and obtained from Sichuan Provincial Health Statistics Support System Database. The inpatient discharge dataset contains patient-level information, including as follows [16, 27]: (1) The patient’s basic information includes their age, gender, and health insurance program (Urban Employment Basic Medical Insurance, Urban Residents Basic Medical Insurance, New Cooperative Medical Scheme, full self-expenses, and others). (2) The admission information includes the admission source (transferred from the outpatient department within the hospital, from the emergency department within the hospital, from other hospitals, and others), the urgency at admission (critical urgent, urgent, and general), International Classification of Diseases, 10th Revision (ICD-10) codes and the names of primary and secondary diagnoses. (3) The discharge information includes the discharge method (following the doctor’s advice to leave the hospital, following doctor’s advice to transfer to other hospitals, not following the doctor’s advice to leave the hospital, and others), the discharge status (cured, improved, unhealed, death, and others), and the inpatient expenses (total expenses and sub-group expenses). (4) The basic information of the hospitals that patients are admitted to (e.g., hospital identifier, hospital level). The hospital administrative data reported annually by hospitals at the end of the year contains detailed hospital-level characteristics, such as hospital identifier, administrative division code, geographic location, number of beds, staffing level, whether general, whether for-profit, and whether public hospital [27]. In addition to these two datasets, we derive the region-level demographic, socioeconomic, and health resource data from the Sichuan Health Statistical Yearbook and Sichuan Statistical Yearbook, including the number of health technicians per 1000 population, the number of residences, and the GDP per capita. The inpatient discharge dataset was linked to the hospital administrative data by the hospital identifiers and further linked to the demographic, socioeconomic, and health resource data by the administrative division codes of hospitals [27]. The latitude and longitude of the hospital and patient locations were geocoded from the Gaode map based on the hospital name and address, as well as the patient’s address, which was utilized to obtain the distance metrics among hospitals, and between hospitals and patients [26].
Disease selecting
In this study, we focused on diseases with significant burdens. We used inpatient volume and medical expenses to reflect the disease’s burden [26]. According to the regulations in the authority file [28], the first three digits of the ICD-10 code can be used as a statistical classification, so we used 3 digits ICD-10 code to identify the observations in this study. Referring to previous study [26], the detailed process of disease selecting are as follows: (1) the diseases were arranged in descending order according to the inpatient volume, and the top 20 diseases with the largest inpatient volume were selected; (2) the diseases were arranged in descending order according to the total expenses of all inpatients, and the top 20 diseases were selected. This study also considers the characteristics of the diseases to ensure that the selected diseases could cover acute and chronic diseases, severe and mild diseases, as well as various departments (including orthopedics, gastroenterology, neurosurgery, endocrinology, etc.). Ultimately, 19 diseases were selected in this study, including bronchial and lung cancer (C34), non-insulin-dependent diabetes (E11), schizophrenia (F20), essential hypertension (I10), chronic ischemic heart disease (I25), cerebral infarction (I63), hemorrhoid (I84), pneumonia (J12-J18), acute bronchitis (J20), chronic obstructive pulmonary disease (J44), gastritis and duodenitis (K29), cholelithiasis (K80), spine joint stiffness (M47), intervertebral disc disorders (M50-M51), obstructive and reflux uropathy (N13), chronic kidney disease (N18), intracranial injury (S06), femoral fracture (S72), fractures of the lower leg (including the ankle) (S82),Footnote 2 involving more than 1.1 million hospitalizations (about 35% of total hospitalizations) in our empirical analysis.
We cleaned up the data of 19 selected diseases before analysis. Table 1 shows the details of the data cleaning process.
Competition measurement
We calculated Herfindahl-Hirschman Index (HHI) for each disease to measure hospital competition. To address the potential endogeneity of conventional estimation of HHI, such as fixed radius and geopolitical boundaries approach, we employed the predicted patient flow approach to define the hospital market and to calculate HHI [32,33,34].
The predicted patient flow approach was proposed by DP Kessler and MB Mcclellan [35] and defines the potential market capturing the potentially competitive hospitals, rather than defining geographic markets arbitrarily [32,33,34,35]. This method calculates the expected patient shares based on exogenous determinants of patient flows, such as distance between patients and hospitals, rather than potentially endogenous indicators.
Specifically, referring to previous studies [32,33,34,35], the process to measure the hospital competition by predicted patient flow method is as follows:
First, we constructed the patient’s hospital choice model,Footnote 3 and assume that patients choose the hospital that maximizes their utility. The choice model in this study mainly refers to [32, 35], and it is as followFootnote 4:
Where U ij denotes inpatient i’s indirect expected utility from choosing hospital j, as the sum of a function of the relative distances and hospital characteristics Zj1, Zj2, Zj3; a function of inpatient i’s demographic characteristics femalei, agei, lowseverityi, emergencyi and CCIi and hospital characteristics Zj1, Zj2, Zj3; and random error eij. Among them, Zj1, Zj2, Zj3 represents whether hospital j is a public hospital, whether hospital j is a tertiary hospital, whether hospital j is a big hospital (defined as the actual number of hospital beds over the median bed for a specific disease), respectively; femalei and agei denote the gender and age of inpatient i, respectively. highseverityi is binary indicator of whether inpatient i has more than three diagnosis codes in their secondary diagnoses (then low severity as the reference group). seriousi is binary indicator of the inpatient i’s urgency at admission is critical urgent or urgent (general as the reference group). emergencyi indicates whether inpatient i is admitted through the emergency department (admission not from the emergency department as the reference group). CCIi denotes Charlson Comorbidity Index (CCI) to reflect the complications of inpatients. \({d}_{ij}-{d}_{ij^{+}}^k\) is the distance from inpatient i’s residence to hospital j minus the distance from i’s residence to the nearest hospital with the same characteristics Zj1, Zj2, Zj3. \({d}_{ij}-{d}_{ij^{-}}^k\) is the distance from i’s residence to hospital j minus the distance from i’s residence to the nearest hospital with different characteristics in terms of Zj1, Zj2, Zj3 [32, 35] . According to the previous study, patient’s choice sets J was restricted to their chosen hospital and all hospitals within 100 km [32, 33, 35] (we also used different lengths to define the inpatients’ choice set J in the robust check).
Second, we predicted the probability of inpatient i admitted to hospital j in their choice set J based on the above hospital choice model.
where \({\hat{u}}_{ij}\) is the utility of inpatient i admitting to hospital j.
Third, the HHI for inpatient i was calculated.
Fourth, HHI for hospital j was calculated.
where I refers to these inpatients who might potentially choose hospital j, \({N}_j=\sum \limits_{i\in I}{\hat{P}}_{ij}\) indicates the expected volume of hospital j.
Statistical analysis
Diseases grouping
Using K-means clustering, we classified the selected diseases. K-means clustering, a common unsupervised algorithm in machine learning, divides the data into different groups according to their characteristics [36]. We used the Hopkins statistic value to test the cluster forming tendency of the data [37, 38].Footnote 5 The optimal number of clusters (K) was determined based on the sum of the squared error (SSE, also called the elbow method)Footnote 6 [40]. Cluster analysis was performed on scaled and centered values. Cluster labels were assigned based on the characteristics of individual cluster mean values of the indicators [41].
According to the aims of this study, the clustering indicators were selected from the point of complexity and urgency of the disease conditions. This study used the disease-specific inpatient emergency admission rate to measure the urgency of the disease conditions. We calculated the disease-specific inpatient average Charlson Comorbidity Index (CCI) to reflect the complexity of the disease conditions. A detailed explanation of why we use disease-specific inpatient emergency admission rate and CCI as the clustering indicators are shown in the appendix text (Text 3) in the supplementary file.
Regression analysis
First, the univariate analysis was performed. The continuous variables were described by the means (M) and standard deviation (SDs), while the categorical variables by frequency and percentage.
Second, the effects of hospital competition on the inpatient expenses were analyzed by the log-linear multivariate regression model. The model is set as follows:
where m denotes the market, h the hospital, d the disease, and i the inpatient. Expense is the explained variable, which denotes the inpatient expenses. The variable HHI is the key independent variable, which indicates the competition intensity (or concentration).
P is a vector of patient’s basic characteristics, including gender, age, and their health insurance program. A is a vector of the patient’s admission characteristics, including the admission source, the urgency of admission. T is a vector of the patient’s treatment information, including the CCI. H is a vector of variables related to the hospital’s characteristics, including the hospital level, ownership, whether general, whether for-profit, and the number of beds. C is the vector of county characteristics, including the number of health technicians per 1000 population, the number of residences, and the GDP per capita.ε is the error term.
We use robust standard errors to correct heteroskedasticity. Due to the positively skewed distribution of inpatient expenses, the number of beds, the number of health technicians per 1000 population, the number of residences, and the GDP per capita, we applied their logarithmic transformations in the regressions.
β1 is the coefficient of interest. A positive value means that hospital competition would reduce the inpatient expenses (or hospital concentration would increase the inpatient expenses). All analyses were performed using STATA 15.0. P < 0.05 was used to determine statistical significance.
Results
Descriptive statistics
Table 2 displays the means and standard deviation of continuous variables, and the frequency and percentage of categorical variables.Footnote 7
The average inpatient expenses of different diseases are distinct from which femoral fracture inpatients (S72) are the highest (25,665.93 Yuan), while acute bronchitis (J20) inpatients the lowest (2755.29 Yuan). The mean values of HHI of intervertebral disc disorder (M50-M51), spine joint stiffness (M47), obstructive and reflux uropathy (N13) inpatient are the smallest (0.04), while schizophrenia (F20) inpatient the largest. The average age of pneumonia inpatients (J12–18) is the youngest (19.78), while chronic obstructive pulmonary disease (J44) inpatients the oldest (72.88). Eight diseases’ female proportion is greater than male. Most of the inpatients’ health insurance programs are the Urban Employment Basic Medical Insurance, Urban Residents Basic Medical Insurance, and New Cooperative Medical Scheme. The intracranial injury (S06) inpatient’s emergency department admission rate is the highest (61.85%), while the spine ankylosis inpatient (M47) the lowest (6.09%). More than 50% (55.95) intracranial injury (S06) inpatients’ admission status is critical or urgent, while hemorrhoids (I84) inpatients only about 7% (7.08%). The mean value of CCI of hemorrhoid (I84) inpatients is the lowest (0.16), while the non-insulin dependent diabetes (E11) the highest (3.46). Most of the inpatients are treated in secondary or tertiary hospitals, general hospitals, public hospitals, and non-profit hospitals.
Clustering analysis
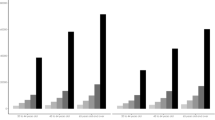
The Hopkins statistic value is 0.74 (> 0.5), suggesting that the dataset is significantly clusterable. As shown in Fig. 1, the elbow of the curve appeared when the K value is equal to 3.
Column 1 and 2 of Table 3 shows the clustering results. The bronchial and lung cancer, non-insulin-dependent diabetes, and chronic kidney disease were clustered into cluster 1. The cerebral infarction, cholelithiasis, obstructive and reflux uropathy, intracranial injury, femoral fracture, and fractures of the lower leg (including the ankle) were clustered into cluster 2. The schizophrenia, essential hypertension, chronic ischemic heart disease, hemorrhoids, pneumonia, acute bronchitis, chronic obstructive pulmonary disease, gastritis and duodenitis, spine joint stiffness, and intervertebral disc disorders were clustered into cluster 3.
Column 3, 4, and 5 of Table 3 shows the centroid point of each cluster, which could reflect the characteristics of each cluster (all clustering indicators were scaled before clustering). Cluster 1 refers to diseases with highly complex condition (DWC) group characterized by high CCI. Cluster 2 refers to diseases with urgent condition (DWU) group characterized by high emergency admission rates. Cluster 3 refers to diseases with less complex and less urgent condition (DWL) group characterized by low CCI and low emergency admission rates.
To verify whether the indicators used for clustering contribute to the results of the clustering process, the Kruskal-Wallis test was conducted in this study. The results show that the P-value of the cluster indicators in the three clusters are all < 0.05, suggesting that the difference in the three clusters is statistically significant. Therefore, the two indicators were used for cluster analysis of 19 diseases, and it is reasonable to use them as the indicators for cluster analysis.
Regression analysis
Figure 2 shows the estimated coefficient of HHI for all diseases and its 95% confidence interval.Footnote 8
Regression analysis. Note: (1) DWC group refers to diseases with highly complex conditions. DWU group refers to diseases with urgent conditions. DWL group refers to diseases with less complex and urgent conditions. (2) C34: bronchial and lung cancer. E11: non-insulin-dependent diabetes. N18: chronic kidney disease. (3) I63: cerebral infarction. K80: cholelithiasis. N13: obstructive and reflux uropathy. S06: intracranial injury. S72: femoral fracture. S82: fractures of the lower leg (including the ankle). (4) F20: schizophrenia. I10: essential hypertension. I25: chronic ischemic heart disease. I84: hemorrhoids. J12-J18: pneumonia. J20: acute bronchitis. J44: chronic obstructive pulmonary disease. K29: gastritis and duodenitis. M47: spine joint stiffness. M50-M51: intervertebral disc disorders
For diseases with highly complex conditions, the estimated coefficients of HHI are mixed in the direction and statistical significance in the identical regression model. For bronchial and lung cancer (C34) and chronic kidney disease (N18), the coefficients of HHI are − 0.612 and − 0.221 respectively, and both statistically significant, which means that these diseases’ inpatient expenses increase by 6.12 and 2.21% respectively, on average with 10% reduction in HHI. For non-insulin-dependent diabetes (E11), the coefficient of HHI is 0.028, and statistically insignificant at 5% level, indicating that there are no effects of hospital competition on inpatient expenses of this disease.
For diseases with urgent conditions, the estimated coefficients of HHI are also mixed in the direction and statistical significance in the identical regression model (almost all of them are statistically insignificant at 5% level). For cerebral infarction (I63), cholelithiasis (K80), intracranial injury (S06), femoral fracture (S72), and fractures of the lower leg (including the ankle) (S82), the coefficients of HHI are − 0.044, − 0.010, 0.113, − 0.063, and − 0.161, respectively, and all statistically insignificant at 5% level, indicating that there are no effects of hospital competition on inpatient expenses of these three diseases. For obstructive and reflux uropathy (N13), the coefficient of HHI is 0.185, and significant at 5% level, suggesting that the inpatient expenses decrease by 1.85% on average with 10% reduction in HHI.
For diseases with less complex and less urgent conditions, the coefficients of HHI are all positive, and almost all of them significant at the 5% level. Specifically, the coefficients of HHI of schizophrenia (F20), essential hypertension (I10), hemorrhoids (I84), pneumonia (J12-J18), acute bronchitis (J20), chronic obstructive pulmonary disease (J44), gastritis and duodenitis (K29), spine joint stiffness (M47), and intervertebral disc disorders (M50-M51) are 0.836, 0.320, 0.533, 0.257, 0.084, 0.196, 0.594, 0.283, and 0.364 respectively, and all significant at the 5% level, which shows that when HHI is reduced by 10% on average, the inpatient expenses of these diseases are reduced by 8.36, 3.20, 5.33, 2.57, 0.84, 1.96, 5.94, 2.83, and 3.64% on average respectively. The results suggest that hospital competition would reduce these diseases’ inpatient expenses. The coefficient of HHI of the chronic ischemic heart disease (I25) is 0.050, and insignificant at 5% level, indicating that there are no effects of hospital competition on inpatient expenses of this disease.
In summary, the results suggest that heterogeneous effects of hospital competition on inpatient expenses across disease groups: hospital competition does not play an ideal role in reducing inpatient expenses for diseases with highly complex conditions and diseases with urgent conditions, but it has a significant effect on reducing inpatient expenses of diseases with less complex and less urgent conditions.
Robust check
We used 3 digits ICD-10 code to identify the observations in this study. Only using 3-digits ICD-10-codes may make the categories overly broad in terms of complexity and acuteness. We also controlled a set of dummy variables of the complete ICD-10 code of primary diagnosis in the regression model to control the fixed effects of diseases furtherly, the findings are consistent with our main analysis. Appendix Fig. 2 in the supplementary file shows the results controlling a set of dummy variables of the complete ICD-10 code of primary diagnosis.
In the predicted patient flow approach, inpatients’ choice set J was restricted to their chosen hospital and all hospitals within 100 km. To test the robustness of our results, this study also used different lengths to define the inpatients’ choice set J, including 80 km, 150 km, and 200 km. Using the identical regression model as the main regression analysis, the results are similar to the main regression analysis, showing the robustness of our results. The result is shown in Appendix Fig. 3, 4, 5 in the supplementary file.
We conducted a series of tests before and after clustering to ensure and verify the accuracy of clustering results as much as possible. In addition, to avoid the potential bias caused by the K-means clustering method and test the robustness of our results, instead of grouping the selected diseases by the K-means clustering method, we directly added the disease-specific emergency admission rate and the disease-specific average CCI into the regression model as proxy variables for the urgency and complexity of diseases condition, and construct interaction terms with HHI to verify whether the heterogeneity of competition still exists. The results are displayed in Appendix Table 6. We also divided the disease-specific emergency admission rate and the disease-specific average CCI into three groups according to the quantile, and also construct interaction terms with HHI to verify whether the heterogeneity of competition still exists. The results are displayed in Appendix Table 7. The findings are still consistent with the main analysis, namely, the more complex and urgent the disease, the weaker the role of hospital competition in reducing inpatient expenses, and even increase expenses.
Discussion
This study selected 19 representative diseases with significant burden based on the inpatient volume and expenses and explored the heterogeneous effects of hospital competition on inpatient expenses basing on disease grouping according to condition’s complexity and urgency. Employing K-means clustering, the selected diseases were divided into three groups, including diseases with highly complex conditions, diseases with urgent conditions, and diseases with less complex and less urgent conditions. Calculating Herfindahl-Hirschman Index based on the predicted patient flow to measure the hospital competition, and using the log-linear multivariate regression model, we found heterogeneous effects of hospital competition on inpatient expenses across disease groups: hospital competition does not play an ideal role in reducing inpatient expenses for diseases with highly complex conditions and diseases with urgent conditions, but it has a significant effect in reducing inpatient expenses of diseases with less complex and less urgent conditions.
The difficulties of obtaining or understanding the disease- and treatment-related knowledge for patients who suffer from diseases with highly complex conditions would be bigger than their counterparts, which would lead to these patients facing greater information asymmetry. These patients in the process of care provision usually cannot know what treatment or service options are desirable or necessary for their specific medical condition. Since the major revenue of hospitals comes from patient fees [42] Footnote 9, hospitals facing huge competitive pressures would have incentives to provide more services for patients to earn more revenue. The hospitals in competitive market may not attract these patients with highly complex conditions by improving the efficiency to decrease the expenses as the providers in the general market but induce demand by using information asymmetry between physicians and patients or achieve the purpose of profit maximization by carrying out medical arms race, mixing the effectiveness of hospital competition in reducing the inpatient expenses of diseases with highly complex conditions [43,44,45].
The choice autonomy for the patients who suffer from the disease with urgent conditions would be limited greatly. These patients usually need to be admitted to the hospital for treatment within a very short time, generally selecting the nearest hospital according to treatment capacity [21]. Even in some emergencies, patients or their companions have to dial the emergency phone for medical help. In this case, the ambulance drivers are usually instructed to bring patients to the nearest emergency room [46], which would leave the patients or their companion limited opportunity to choose hospitals. The choice autonomy for these patients would be limited greatly, affecting the effectiveness of hospital competition on inpatient expenses [19, 20]. In addition, the patients suffering from the disease with urgent conditions typically exhibit a very low elasticity of demand for hospital treatment [21]. Since the distance from the patient to the hospital would be the main consideration of these patients, they would not be attracted dramatically by the hospital’s competitive behaviors, such as reducing medical expenses. As a result, the hospitals have not great incentives to reduce expenses to attract these patients, leading to the hospital competition insignificantly associated with inpatient expenses of diseases with urgent conditions.
The information asymmetry and patient’s limited choice autonomy in the process of care provision for the patients who suffer from diseases with less complex and less urgent conditions would not be obvious. Patients with these diseases can obtain information and knowledge about diseases or the treatment by searching the internet or asking their friends who have suffered from, helping them to judge to a certain extent what treatment or service options are desirable or necessary for their specific medical condition in the process of care provision. The information gap between physicians and patients would be reduced, decreasing the possibility that the hospitals adopt the strategies for their own benefits at the sacrifice of compromising patients’ interests. These diseases’ condition is less urgent, and the patients or their companion would have enough time to choose the hospital to maximize their utility. Compared with patients who suffer from the disease with urgent conditions, patients with these diseases exhibit higher elasticity of demand for hospital treatment or services. These patients would be more sensitive to the medical expenses than their counterparts, leading to the hospitals in competitive market would take measures, including reducing the inpatient expenses, to attract patients to obtain the competitive advantage. The care of diseases with less complex and less urgent conditions is more similar to the product in the general market, and the hospital competition could play a positive role in reducing the inpatient expenses.
The findings of this study are consistent with previous studies focusing on diseases with a specific condition from the United States [47, 48], and China [19]. Using the patients undergoing hepatic or pancreatic resection as the representative of highly complex and specialized surgery procedures, M Cerullo, et al. [47] examined the association between regional hospital market concentration and hospital charges for hepatopancreatic biliary surgical procedures. This study concluded that for complex, highly specialized procedures, hospital competition would negatively associate with overall charges. OY Tang, et al. [48] evaluated the relationship between interhospital competition and inpatient charges in patients undergoing cranial neurosurgery that is usually complex and found that hospitals in more competitive markets exhibited higher charges for admissions of patients undergoing an in-hospital cranial procedure. Both of their findings are consistent with our study’s finding that hospital competition does not play an ideal role in reducing inpatient expenses for diseases with highly complex conditions. C Deng and J Pan [19] evaluated and compared the relationships between hospital competition and the expenses of prostatectomies (elective surgery, representing treatments of non-acute common diseases) and appendectomies (emergency surgery, representing treatments of acute common diseases), and found that greater competition was significantly associated with lower total hospital charges for prostatectomies, while the opposite was true for appendectomies, which are consistent with our study, namely, hospital competition does not play an ideal role in reducing inpatient expenses for diseases with urgent conditions, while it has a significant effect in reducing inpatient expenses of diseases with less complex and less urgent conditions.
Taking into consideration multiple factors as discussed above, it is therefore highlighted as an essential implication in our study that the differences in condition’s complexity and urgency among diseases would lead to different impacts of hospital competition. When using hospital competition to achieve the optimal policy impact on healthcare systems while minimizing the potential adverse outcomes to improve the health services supply systems, the differences in conditions among diseases should be given full consideration. The authority should pay more attention to the diseases with highly complex and urgent conditions to reduce the potential negative influence caused by information asymmetry and limited choice autonomy.
It is noteworthy that some limitations should be addressed in this study. (1) This study collected data from the discharge data of inpatients of Sichuan province in the fourth quarter of 2018 (from September to December), there may be a potential seasonal trend. In future research, we can collect more longitudinal data to solve this problem. (2) The sample size only covers hospitals in Sichuan province. Although Sichuan province can reflect the overall situation of the country to a certain degree, for some specific regions, such as Shanghai and Shenzhen cities, the generalizability of our findings would be limited. More data collected from several provinces should be used to analyze furtherly in future studies. (3) Research focusing on the mechanisms of competition effects is needed. (4) This study used K-means clustering based on objective clustering indicators to group the diseases. Due to the data limitation, the selected indicators may not fully reflect the conditions’ complexity and urgency of diseases. More systematic and comprehensive indicators should be collected and selected as the cluster indicators to fully reflect disease conditions’ complexity and urgency in future studies.
Conclusion
Based on the results of K-means clustering and log-linear multivariate regression model, we concluded that heterogeneous effects of hospital competition on inpatient expenses across diseases groups: hospital competition does not play an ideal role in reducing inpatient expenses for diseases with highly complex conditions and diseases with urgent conditions, but it has a significant effect in reducing inpatient expenses of diseases with less complex and less urgent conditions. Our study offers implications that the differences in conditions’ complexity and urgency among diseases would lead to different impacts of hospital competition, which would be given full consideration when designing the pro-competition policy in the healthcare delivery system to achieve the desired goal.
Availability of data and materials
The data that support the findings of this study are available from the Health Commission of Sichuan Province but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the Health Commission of Sichuan Province.
Notes
The representativeness of Sichuan Province is discussed in the appendix text (Text 1) in the supplementary file.
Although senile cataract (H25) also meets the above inclusion criteria, there are many special subsidy policies for the patients with H25, such as reduction or exemption of operation expenses for the rural elderly poor, which would likely impact the effects of competition on the medical expenses. We excluded this disease in our study to avoid its confounding effects caused by the policies on our analysis [29,30,31].
The results of the choice model of all diseases are displayed in Appendix Table 1 in the supplementary file.
A detailed explanation of how to construct the HHI based on the predicted patient flow approach is shown in the appendix text (Text 2) in the supplementary file.
The elbow method is used to determine the number of clusters (K). This method consists of plotting the explained variation as a function of the number of clusters and picking the elbow of the curve as the optimal number of clusters [39].
Appendix Table 2 in the supplementary file displays the number and percentage of all kinds of hospitals for each disease.
The regression results of all variables are displayed in Appendix Table 3 (DWC group), 4 (DWU group), and 5 (DWL group) in the supplementary file.
In China, only about 10% of the hospital’s revenue comes from government subsidies, and the vast shortfall needs to be filled by patient fees [42].
Abbreviations
- HHI:
-
Herfindahl-Hirschman Index
- ICD-10:
-
International Statistical Classification of Diseases and Related Health Problems, 10th Revision
- DWC:
-
Diseases with highly complex condition group
- DWU:
-
Diseases with urgent condition group
- DWL:
-
Diseases with less complex and less urgent condition group
- CCI:
-
Charlson comorbidity index (CCI)
- M:
-
Means
- SDs:
-
Standard deviation
References
Siciliani L, Chalkley M, Gravelle H. Policies towards hospital and GP competition in five European countries. Health Policy. 2017;121(2):103–10.
Choné P. Competition policy for health care provision in France. Health Policy. 2017;121(2):111–8.
Schut FT, Varkevisser M. Competition policy for health care provision in the Netherlands. Health Policy. 2017;121(2):126–33.
Kifmann M. Competition policy for health care provision in Germany. Health Policy. 2017;121(2):119–25.
Fernando R, Leticia A-B. Antonio J T: how does managed competition affect hospital prices in a social health insurance system? The Colombian case Health Policy Plann. 2018;33(9):1037–46.
Barros PP. Competition policy for health care provision in Portugal. Health Policy. 2017;121(2):141–8.
Longo F, Siciliani L, Moscelli G, Gravelle H. Does hospital competition improve efficiency? The effect of the patient choice reform in England. Health Econ. 2019;28(5):618–40.
Liu GG, Vortherms SA, Hong X: China's Health Reform Update. In: Annual Review of Public Health, Vol 38. Volume 38, edn. Edited by Fielding JE; 2017: 431–448.
Yip W, Fu H, Chen AT, Zhai T, Jian W, Xu R, et al. 10 years of health-care reform in China: progress and gaps in universal health coverage. Lancet. 2019;394(10204):1192–204.
Pan J, Liu GG, Gao C. How does separating government regulatory and operational control of public hospitals matter to healthcare supply? China Econ Rev. 2013;27:1–14.
China's Central Committee and State Council: Opinions of the Central Committee and the State Council on deepening the health care system reform. In.: http://www.gov.cn/jrzg/2009-04/06/content_1278721.htm. (in Chinese); 2009.
Gaynor M, Vogt WB: Chapter 27- Antitrust and competition in health care markets. In: Handbook of Health Economics. Volume 1, edn. Edited by Pauly MV, McGuire TG, Barros PP: Elsevier; 2000: 1405–1487.
Dranove D: Chapter Ten - Health Care Markets, Regulators, and Certifiers. In: Handbook of Health Economics. Volume 2, edn. Edited by Pauly MV, McGuire TG, Barros PP: Elsevier; 2011: 639–690.
Gaynor M, Town RJ: Chapter Nine - Competition in Health Care Markets. In: Handbook of Health Economics. Volume 2, edn. Edited by Pauly MV, McGuire TG, Barros PP: Elsevier; 2011: 499–637.
Bhattacharya J, Hyde T, Tu P. Health economics: Macmillan international higher education; 2013.
Lu L, Pan J. The association of hospital competition with inpatient costs of stroke: evidence from China. Soc Sci Med. 2019;230:234–45.
Mankiw NG. Principles of economics: Cengage learning; 2020.
Arrow KJ: Uncertainty and the welfare economics of medical care. In: Uncertainty in Economics. edn.: Elsevier; 1978: 345–375.
Deng C, Pan J. Hospital competition and the expenses for treatments of acute and non-acute common diseases: evidence from China. BMC Health Serv Res. 2019;19(1):739.
Or Z, Rococco E, Touré M, Bonastre J. Impact of competition versus centralisation of hospital care on process quality: a multilevel analysis of breast Cancer surgery in France. Int J Health Policy Manag. 2020.
Colla C, Bynum J, Austin A, Skinner J: Hospital competition, quality, and expenditures in the US Medicare population. In.: National Bureau of economic Research; 2016.
Phelps CE. Health economics: Routledge; 2017.
Dranove D, Satterthwaite MA: Chapter 20-The Industrial Organization of Health Care Markets. In: Handbook of Health Economics. Volume 1, edn. Edited by Pauly MV, McGuire TG, Barros PP; 2005: 1093–1139.
Song C, Shi X, Bo Y, Wang J, Wang Y, Huang D. Exploring spatiotemporal nonstationary effects of climate factors on hand, foot, and mouth disease using Bayesian spatiotemporally varying coefficients (STVC) model in Sichuan, China. Sci Total Environ. 2019;648:550–60.
Lu L, Pan J. Does hospital competition lead to medical equipment expansion? Evidence on the medical arms race. Health Care Manage Sci. 2021:1–15.
Lu L, Chen T, Lan T, Pan J. The Comparison Between Different Hospital Market Definition Approaches: An Empirical Analysis of 11 Representative Diseases in Sichuan Province, China. Front Public Health. 2021;9:1165.
Lin X, Lu L, Pan J. Hospital market competition and health technology diffusion: an empirical study of laparoscopic appendectomy in China. Soc Sci Med. 2021;286:114316.
General Office of the Ministry of health: Notice on disease classification and code (Revised Version). In.: General Office of the Ministry of health,; 2011(in chinese).
Sichuan health and Health Committee, Sichuan Disabled Persons' Federation: Notice on Printing and Distributing the Implementation Plan of the 2017 Poor Cataract Patients' Rejuvenation Surgery Project in Sichuan Province. In.: http://wsjkw.sc.gov.cn/scwsjkw/yzyg/2017/8/1/1a4c0a7f3e6e4d3a8c936ea35d662e2e.shtml (in Chinese); 2017.
Sichuan health and Health Committee, Sichuan Disabled Persons' Federation: Notice on Printing and Distributing the Implementation Plan of the 2019 Poor Cataract Patients' Rejuvenation Surgery Project in Sichuan Province. In.: http://wsjkw.sc.gov.cn/scwsjkw/yzyg/2019/4/26/1b62a80f24094032b305a47a8cecf6b7.shtml (in Chinese); 2019.
General Office of the CPC Sichuan Provincial Committee, General Office of the People's Government of Sichuan Province: Notice on Issuing the ``Ten Livelihood Projects and 20 Livelihood Practical Implementation Plans of the Province in 2018″. In.: http://www.sc.gov.cn/10462/10464/10797/2018/2/6/10444643.shtml (in Chinese); 2018.
Lin X, Cai M, Fu Q, He K, Jiang T, Lu W, et al. Does hospital competition harm inpatient quality? Empirical evidence from Shanxi, China. Int J Env Res Public Health. 2018;15(10):2283.
Gaynor M, Moreno-Serra R, Propper C. Death by market power: reform, competition, and patient outcomes in the National Health Service. Am Econ J-Econ Policy. 2013;5(4):134–66.
Gowrisankaran G, Town RJ: Competition, payers, and hospital quality. Health Services Res 2003, 38(6p1):1403–1422.
Kessler DP, Mcclellan MB. Is hospital competition socially wasteful? Q J Econ. 2000;115(2):577–615.
Teknomo K. K-means clustering tutorial. Medicine. 2006;100(4):3.
Banerjee A, Dave RN: Validating clusters using the Hopkins statistic. In: 2004: IEEE: 149–153.
Aggarwal CC. Data mining: the textbook: springer; 2015.
Thorndike RL. Who belongs in the family? Psychometrika. 1953;18(4):267–76.
Rousseeuw PJ. Silhouettes: a graphical aid to the interpretation and validation of cluster analysis. J Comput Appl Math. 1987;20:53–65.
Anjana RM, Baskar V, Nair ATN, Jebarani S, Siddiqui MK, Pradeepa R, et al. Novel subgroups of type 2 diabetes and their association with microvascular outcomes in an Asian Indian population: a data-driven cluster analysis: the INSPIRED study. BMJ Open Diabetes Research and Care. 2020;8(1):e001506.
Qian J, Jingwei He A, Dean-Chen Yin J. The medical arms race and its impact in Chinese hospitals: implications for health regulation and planning. Health Policy Plann. 2019.
Robinson JC, Luft HS. The impact of hospital market-structure on patient volume, average length of stay, and the cost of care. J Health Econ. 1985;4(4):333–56.
Eggleston K, Ling L, Meng Q, Lindelow M, Wagstaff A. Health service delivery in China: a literature review. Health Econ. 2008;17(2):149–65.
Delamater PL, Messina JP, Grady SC, WinklerPrins V, Shortridge AM: Do More Hospital Beds Lead to Higher Hospitalization Rates? A Spatial Examination of Roemer's Law. PLoS One 2013, 8(2).
National health commission of the People's Republic of China: Guiding opinions on further improving pre hospital medical first aid service In.: http://www.nhc.gov.cn/yzygj/s3594q/202009/4b20d1ac72914b3997f76110ccc0103d.shtml (in chinese); 2020.
Cerullo M, Chen SY, Dillhoff M, Schmidt C, Canner JK, Pawlik T: Association of Hospital Market Concentration With Costs of Complex Hepatopancreaticobiliary Surgery. Jama Surg 2017, 152(9).
Tang OY, Perla KMR, Lim RK, Yoon JS, Weil RJ, Toms SA: Interhospital competition and hospital charges and costs for patients undergoing cranial neurosurgery. J Neurosurg 2020, 1(aop):1–12.
Acknowledgments
We would like to thank Ke Ju (Monash University) for their valuable suggestions concerning the revision of the manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (Grant No. 71874116, 72074163 and 72104158), Ministry of Education of China (Grant No. 18YJA790062), Taikang Yicai Public Health and Epidemic Control Fund, Chengdu Federation of Social Science Association (Grant No. ZZ05), Sichuan University (Grant No. 2018hhf-27 and SKSYL201811), China Medical Board (Grant No. 17–276), and the Chinese Postdoctoral Science Foundation (Grant No. 2020 M683297).
Author information
Authors and Affiliations
Contributions
JP conceptualized the study. LL processed and analyzed the relevant data, as well as wrote the manuscript. XL helped to process the data. All authors contributed to the study design, interpretation of the results, and manuscript revision, and have approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval and consent to participate are not applicable. This study was based on secondary data from the Sichuan Provincial Health Statistics Support System Database. All data were de-identified and the manuscript does not contain any individual person’s data. Therefore, this study was exempted from ethics approval and consent to participate.
The authors obtained all necessary administrative permission from the Health Commission of Sichuan Province to access data used in this study. All methods and processes carried out in this study were in accordance with relevant guidelines and regulations in China.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lu, L., Lin, X. & Pan, J. Heterogeneous effects of hospital competition on inpatient expenses: an empirical analysis of diseases grouping basing on conditions’ complexity and urgency. BMC Health Serv Res 21, 1322 (2021). https://doi.org/10.1186/s12913-021-07331-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-021-07331-1