Abstract
Background
Care for people with an Intellectual Disability (ID) is complex: multiple health care professionals are involved and use different Health Information Systems (HISs) to store medical and daily care information on the same individuals. The objective of this study is to identify the HISs needs of professionals in ID care by addressing the obstacles and challenges they meet in their current HISs.
Methods
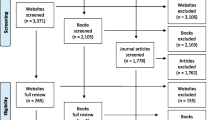
We distributed an online questionnaire amongst Dutch ID care professionals via different professional associations and care providers. 328 respondents answered questions on their HISs. An inventory was made of HIS usage purposes, problems, satisfaction and desired features, with and without stratification on type of HIS and care professional.
Results
Typical in ID care, two types of HISs are being used that differ with respect to their features and users: Electronic Client Dossiers (ECDs) and Electronic Patient Dossiers (EPDs). In total, the respondents mentioned 52 unique HISs. Groups of care professionals differed in their satisfaction with ECDs only. Both HIS types present users with difficulties related to the specifics of care for people with an ID. Particularly the much needed communication between the many unique HISs was reported a major issue which implies major issues with inter-operability. Other problems seem design-related as well.
Conclusion
This study can be used to improve current HISs and design new HISs that take ID care professionals requirements into account.
Similar content being viewed by others
Background
Around 0.85% of the Dutch population has an intellectual disability (ID) according to the definition of having an IQ below 70 [1]. People with an ID often live in longterm care facilities and have a large share in health care use in the Netherlands [2]. Care for people with an ID is complex and involves many professional caregivers. For example, a person with an ID is in close contact with a personal care aide who helps him or her with their daily activities and medication, but also sees a dentist, a general practitioner, and a physical therapist. All caregivers use some type of health information system (HIS) to register their activities and to ensure reimbursement of care provided. This is not without consequence: according to Hanekamp et al. [3], care professionals in long term care in the Netherlands spend 35% of their time on administrative tasks, mainly in their respective HISs.
Typically, HISs are not only used for reimbursement but also to assist professionals and organizations to contribute to highquality, efficient patient care [4,5,6]. Wellfunctioning HISs, are therefore an important building block in the care for people with an ID [7, 8]. In the context of our research HISs contain and manage (medical) information about the person with the ID. Other frequently used terms for HISs in ID care are: electronic health records, and electronic client (or patient) dossiers/records.
Because of the role of HISs in, amongst other, reimbursement [9], patient safety [10], communication amongst professionals [11] and the time spent on administrative tasks in HISs [12], it is essential to know about the HISs used in the complex care for people with ID. It is, however, unknown which HISs are used in ID care, how these systems cater to the needs of different groups of professionals, and what features are used and needed. Reports from multiple countries suggested that different HISs are not interoperable [13,14,15]. Despite several studies on HISs in other forms of care, such as hospital care and GP care [16,17,18,19,20], little research has been done on the problems professional involved in ID care experience with HISs, and on their requirements for HISs. Software developers and researchers need to know about tasks, problems and requirements of care professionals to develop better systems. Therefore, the objective of this study is to identify for ID care, the needs of care professionals by taking inventory of their experiences and wishes for HISs. To fulfill the objective, we set up the following research question: In care for people with ID, what are the key care professionals’ experiences with, and desired requirements for, HISs? With the following subquestions:
-
Which HISs do care professionals for people with an ID use and for which purposes?
-
How do care professionals for people with an ID assess their current HIS?
-
Which features are care professionals for people with an ID missing in their current HISs?
-
To answer these questions, we performed a crosssectional study in which Dutch care professionals working in ID care received a questionnaire informed by semistructured interviews.
Methods
In the following, we describe the design of the online questionnaire, the recruitment of study participants, and data analysis.
Questionnaire construction
As preparation of questionnaire design and to assure thorough familiarity with this diverse care field, we interviewed from our personal and professional networks fourteen health care professionals who differed in terms of their profession but who all worked in ID care. The semistructured interviews lasted about an hour on average and during site visits, interviewees also showed us their local HISs. All interviewees agreed with audiorecording. Transcriptions of the recordings were analyzed to identify routing requirements and in vivo coded (using Atlas.ti 8) to identify possible answer categories for the standardized questionnaire.
From the interviews and sitevisits we learned that two types of HISs were distinguished in practice which differed with respect to users and aim: Electronic Client Dossiers (ECDs) and Electronic Patient Dossiers (EPDs). Care professionals in ID care mainly used the ECDs to register daily activities for care continuity. The EPDs were used for clinical purposes by, for example, dentists and ID physicians. We, therefore, built three routings in the questionnaire: one for the ECDs, one for EPDs, and one for care professionals who used both kinds of systems.
The in vivo coding of the transcripts yielded a total of 18 features and 9 problems with HISs in ID care. Because of interview limitations, we also included an ‘Other, …. ’ answer option. The first concept of the questionnaire was pretested by means of a cognitive interview [21]. Based on this interview the questionnaire was improved, until after the third cycle no new issues appeared.
Recruitment of study participants
We recruited a wide range of health care professionals working in ID care as study participants via various Dutch professional associations and care providers. We were unable to obtain e-mail lists of the members of the professional organizations and the employees of the institutions due to Dutch privacy regulations. Therefore, we used tailored recruitment methods. Personal care aides, nurses, resident assistants (for assisted living), and sheltered workshop guides/job coaches received an email from longterm care providers and their professional association ‘Professional Association of Social Work Professionals’(BPSW). ID physicians were recruited by an email from the ‘Dutch Association of ID physicians’(NVAVG). Remedial educationalists and behavioral therapists were recruited via an email and the newsletter from their professional association ‘Dutch Association for Remedial Educationalists and Behavioral Therapists’(NVO). Psychologists were recruited via a LinkedIn post from the ‘Dutch Association for Healthcare Psychologists’(NVGzP). The ‘Dutch Association for Psychiatry’(NVvP) published an invitation for participation on their intranet. Pharmacists were approached by email through the ‘Dutch Association of Pharmacists for People with an Intellectual Disability’(NVAPVG). Dentists were approached via the website, newsletter, and Facebook page of The ‘Central Consultation for Special Dentistry’, and the newsletter and Facebook page of ‘Association for the Promotion of Dental Care for the Disabled’(VBTGG). The ‘Dutch Association of Physical Therapists for People with an ID’(NVFVG) invited their members via their newsletter.
Data collection procedure
After opening the online questionnaire, participants were requested to read information on the study’s objective and give informed consent. The first question inquired after profession and HIS(s) used to determine routing. The questionnaire continued with questions on satisfaction, features, and problems related to the HIS(s) and concluded with questions on gender, the region of employment, and work experience. Data were collected using Qualtrics [22]. Data collection took place between September 2nd 2019, and October 15th, 2019. All questionnaires are available upon request from the corresponding author. All methods were carried out in accordance with relevant guidelines and regulations.
Data analysis
‘Other, ...’ answers were carefully read, and categorized by three researchers independently. Differences in classifications were discussed until consensus was reached. Then, new categories were added to the data file. We distinguished four groups of care professionals based on where they provide care, frequency (daily or not) and kind of professional training (academic or not): Daily care, Intellectual Disability physician, Mental Health and Development (MH&D), and Other care (see Table 1). Members of the Daily care group, although diverse in terms of profession, all work for a ID care provider. In the ID physician group, we also included ID physicians in training. The Mental Health and Development group works with people with ID on a daily basis, either within an ID healthcare provider or not. The remaining Other group is involved in care for, amongst others, people with an ID.
We investigated differences between these groups, and between EPDs and ECDs. With the nonparametric KruskalWallis test we tested (with α = 0.05) differences between the four groups on HIS’ satisfaction. All statistics were obtained with R.
Results
Descriptives of respondents
Of the 328 respondents in Table 1, 275 also answered the last question (i.e. 16.2% dropout). All respondents answered three or more questions. Nearly half of the respondents belonged to the Daily care group (n = 144).
The respondents worked between one and 43 years in ID care, the median being 13 years (Table 2). Daily care professionals worked the longest in ID care with a median of 17.5 years. 80% of the respondents were women, only the ‘Other care’ group had a lower percentage, with 58%.
Which HISs do care professionals for people with an ID use and for which purposes?
In total, 52 unique HISs were identified (Table 2), of which the majority (32) were EPDs. Table 3 shows the features used in ECDs (n = 225) and EPDs (n = 118), and satisfaction/dissatisfaction with that feature. Overall, Patient/Client administration was most frequently mentioned, followed by Reporting and Client treatment and Support registration. The majority of ECD users indicated other registrations, e.g. freedom of movement, and visitations. In the Appendix in additional Table 1 results were shown for each of the four different groups of care professionals.
How do care professionals for people with an ID assess their current HIS?
The groups differed on their satisfaction level with respect to their ECD in general (Kruskal Wallis, p < 0.0001), with the Daily care group expressing higher levels of satisfaction than the other groups, in particular the Mental Health & Development group (Table 4). No evidence was found for different satisfaction levels with the general use of EPDs (KruskalWallis, p = 0.061). For general satisfaction with their EPD, all groups’ modes were ‘Satisfied’.
For the satisfaction with the suitability of ECDs for ID care a significant difference between groups was found (KruskalWallis, p < 0.0001). Daily care professional’s reports ranged from dissatisfied to very satisfied, with the most frequently occurring judgment ‘satisfied’ (Table Table 4). Based on range and mode, the ID physicians and Mental Health & Development groupappear less satisfied with the suitability of the ECD for ID care. For EPDs, no evidence for differences between groups was found (KruskalWallis, p = 0.12). The satisfaction with the suitable of EPDs for ID care appears rather low across all groups with the modes ‘dissatisfied’, and ‘neither satisfied nor dissatisfied’.
When we go back to Table 3 for more detailed information on dis/satisfaction with features, we see that although the modes suggested satisfaction with the most frequently used features of ECDs, there was no consensus: satisfaction ranged from very dissatisfied to very satisfied. The satisfaction with the less frequently mentioned ECD features, suggested that some people have experienced serious problems with the registration of medical patient information.
A similar situation can be seen for EPD features: although modes suggest that users were rather satisfied with most features, there was no consensus at all. The modes ‘neither satisfied nor dissatisfied’ for the features ‘registration of diagnoses’ and ‘prescribe medication’ should be seen as an important signal: not only because these features are crucial to medical treatment and monitoring but also because they support medication safety. The lowest mode, dissatisfaction, was found for the electronic exchange of patient/client dossier.
The overall most frequently mentioned problems related to HIS design were ‘hard to retrieve information from the system’ (185 times), followed by ‘difficult to exchange electronic client/patient records with other caregivers’ (Table 5). Most other problems mentioned by over 100 respondents related to system reliability: slow, and unavailable systems, and updates that changed the system.
Based on the ‘Other … ’ answers we added two new problem categories: Bad user interface, and User roles and permissions. Only 15 of the 277 care professionals indicated they had experienced no problems with one of their systems. (Table 5). See additional Table 2 in the Appendix for data on group level.
Which features are care professionals for people with an ID missing in their current HISs? Eighty-eight respondents suggested desired, missing, features. We categorized these into 24 missing features (Table 6). The most frequently mentioned missing feature was the link with other systems (20 times), followed by features to provide an overview of data in the system and to prescribe and monitor medication (12 times). Features that were reported missing by one respondent only were: assign tasks, calendar management, financial management, taking history and making careplan, open multiple dossiers at the same time, privacy robust procedures, suitability of system across disciplines, synchronization Windows and ECD, and ‘other registrations’. Additional Table 3 in the Appendix shows the missed features per group of care professionals.
Discussion
Reflection on the results
To the best of our knowledge, this is the first study on HISs in ID care that included both medical and nonmedical care professionals who all report on wellbeing and medical issues concerning the same individuals. We identified ECDs used by all groups involved in residential care and EPDs for medical care. Over 300 respondents reported a total of 52 unique HISs. Care professionals used different HISs for a variety of tasks ranging from administration to treatment registration and reporting. They also reported support registration and a client portal, features specific to ID care and illustrating complexity of this care setting. Information is scattered over different systems which challenges professionals in ID care.
Often people with ID express medical problems, like pain, in behavioral change [23]. This implies that medical staff may experience difficulties because they can’t access the ECD and professionals in daily care may be able to do a better job if they have access to EPDs. Despite a reasonable overall satisfaction with HISs, nearly all respondents reported problems. Many problems related to HIS design (e.g. problems with the user interface), and reliability (slow, and outdated systems). Other problems stem from the organization of ID care, with multiple HISs, information exchange needs, and missing features.
Related work
Previous studies reviewed HIS satisfaction and adoption level for one user group, i.e. medical doctors or nurses in hospitals [16,17,18, 24,25,26] or in other care domains [19, 20, 27,28,29,30,31]. In general, these studies showed dissatisfaction with HISs, despite high adoption rates. Comparability between these studies depends on the national organization of healthcare, and is therefore limited (e.g. the GP as gatekeeper for specialized care, the presence of an IDphysician) [32, 33]. Comparability with our study is also limited because the care for people with ID is characterized by a combination of support and care services [34,35,36].
Other studies [11, 37,38,39,40,41] assessed the adoption and satisfaction with HISs based on features but not on what was missing. Generally speaking these studies found, just like ours, similar levels of satisfaction with the features.
A study in the ID care setting, considered governmental databases as information systems is Karimi et al. [42]. The features they distinguished are, therefore, types of data saved in these databases, and resemble outcomes of our features ‘patient/client administration’, ‘reporting’, and ‘financial administration and reimbursement’. In their discussion, Karimi et al. [42] stressed the necessity of data exchange, which was also mentioned by our respondents.
Like ID care, geriatric care is a form of longterm care, but with better studies on HISs [43,44,45]. Wang and Biedermann [44] and Cherry et al. [45] primarily studied adoption and use of HISs, but not so much satisfaction. Sockolow et al. [43], conducted a survey on one HIS used in a geriatric community setting and concluded that although Philadelphian clinicians did not use the system as intended by the developers, they were satisfied with their HISs. We did not assess whether the care professionals used the systems as intended, since we did not study one HIS, but as it turned out, 52 HISs.
Strengths & weaknesses
The collaboration with nine professionals’ associations and various institutions’ willingness to participate shows the importance of this study. With their help, we could review a wide range of HISs used in ID care. Despite the limited role of GPs in care for institutionalized people with an ID we have attempted to gain the interest of multiple professional organizations for GPs, unfortunately they did not want to participate. Nonetheless we were able to review the most common GP HISs, mainly thanks to the Dutch ID physicians. We believe our sample reflects the main professions responsible for the daily care of people with intellectual disabilities. Nonetheless, there are professions from which no representatives were included in our sample or which were under-represented such as speech therapists, nutritionists and medical doctors other than ID physicians. However, problems with information exchange between these professionals and the respondents of our survey could be reported and, indeed, have been mentioned.
From the interviews, we derived our online questionnaire, including the set of features, which we tested and enhanced with cognitive interviews. We chose not to use a standardized set of features and criteria [46, 47], since these appeared too limited, and too coarse for ID care. The questionnaire contained some questions with a fillin ‘Other, … ‘answer option. By discussing and synthesizing these answers, we experienced the added value of authors from different disciplines.
For the satisfaction questions, we adopted Likert-type scales despite their metric limitations, because they are familiar and therefor easy for respondents. Despite our carefully designed questionnaire, the dropout rate was 16%. Fortunately our data was rich, because many and various respondents gave ‘Other, ...’ answers.
Practical implications
This study showed that the current EPDs are not satisfactory for the special needs in ID care. This indicates that indepth knowledge of the specific ID care setting is necessary for the development of HISs, since it is more complex than other types of care. In the Netherlands, complexity might further increase due to the recently introduced legal obligation to give people with ID access to their own dossier [48]. This access is usually provided through a client portal which is also listed as a feature in Table 3. In practice, relatives often also have access to this system, which allows them to monitor care. Also, the legal representatives make the decisions about what happens to the data of the people with intellectual disabilities, if they cannot decide about these topics this themselves. This creates a complexity for system access and usage of the data. Furthermore, the large number of identified HISs (52) causes multiple interoperability problems.
This complexity, and the aforementioned problems with usability calls for a modular system, that serves as an ECD, EPD, and client portal, where ID modules with particular features can be removed and added as required. The modular system may reduce costs, because of it’s decomposability.
A modular HIS for ID care should be based on standards for information exchange and a reference software architecture [49]. Furthermore, a reference architecture may help make data in ID care more suitable for research by combining privacy standards with the FAIR data principles [35].
Conclusions
In conclusion, answering the general research question, in care for people with ID a wide range of different HISs is used. Despite some satisfaction with the HISs, many problems remain to be solved. Future work will be the design of a reference architecture for modular HISs in ID Care.
Availability of data and materials
The individual surveys analysed during the current study are not publicly available due to confidentiality. Aggregated results are available from the corresponding author on reasonable request.
Abbreviations
- HIS:
-
Health Information System
- ID:
-
Intellectual Disability
- ECD:
-
Electronic Client Dossier
- EPD:
-
Electronic Patient Dossier
- MH&D:
-
Mental Health and Development
References
Woittiez I, Putman L, Eggink E, Ras M. Zorg beter begrepen. Verklaringen voor de groeiende vraag naar zorg voor mensen met een verstandelijke beperking. Den Haag: SCP; 2014.
Polder JJ, Meerding WJ, Bonneux L, van der Maas PJ. Healthcare costs of intellectual disability in the Netherlands: a cost-of-illness perspective. J Intellect Disabil Res. 2002;46(2):168–78.
Hanekamp M, Heesbeen S, van der Helm I, Valks R. Administratieve belasting langdurige zorg 2019. Berenschot: Technical report; 2019.
Yusof MM, Kuljis J, Papazafeiropoulou A, Stergioulas LK. An evaluation framework for Health Information Systems: human, organization and technology-fit factors (HOT-fit). Int J Med Inform. 2008;77(6):386–98.
Haux R, Ammenwerth E, Winter A, Brigl B. Strategic information management in hospitals: an introduction to hospital information systems. Springer Science & Business Media; 2004. https://doi.org/10.1007/978-1-4757-4298-5.
Haux R. Health information systems–past, present, future. Int J Med Inform. 2006;75(3–4):268–81. https://doi.org/10.1016/j.ijmedinf.2005.08.002.
World Health Organization. Everybody’s business: strengthening health systems to improve health outcomes. WHO’s Framework for Action. Geneva: World Health Organization; 2007. Technical report, World Health Organization, 2007
Skolnik R. Global health 101: New Haven, CT: Jones & Bartlett Publishers; 2015. ISBN 9781284050547
McAlearney AS, Robbins J, Hirsch A, Jorina M, Harrop JP. Perceived efficiency impacts following electronic health record implementation: an exploratory study of an urban community health center network. Int J Med Inform. 2010;79(12):807–16.
Sinard JH, Castellani WJ, Wilkerson ML, Henricks WH. Stand-alone laboratory information systems versus laboratory modules incorporated in the electronic health record. Arch Pathol Lab Med. 2015;139(3):311–8.
Raymond L, Paré G, Marchand M. Extended use of electronic health records by primary care physicians: does the electronic health record artefact matter? Health Inform J. 2019;25(1):71–82. https://doi.org/10.1177/1460458217704244.
Trudel M-C, Marsan J, Paré G, Raymond L, de Guinea AO, Maillet É, et al. Ceiling effect in EMR system assimilation: a multiple case study in primary care family practices. BMC Med Inform Decis Mak. 2017;17(1):46.
Brailer DJ. Interoperability: the key to the future health care system: interoperability will bind together a wide network of real-time, life-critical data that not only transform but become health care. Health Aff. 2005;24(Suppl1):W5–19.
Jardim SVB. The electronic health record and its contribution to healthcare information systems interoperability. Procedia Technol. 2013;9:940–8. https://doi.org/10.1016/j.protcy.2013.12.105.
Hovenga EJS. Importance of achieving semantic interoperability for national health information systems. Texto & Contexto-Enfermagem. 2008;17(1):158–67. https://doi.org/10.1590/S0104-07072008000100018.
Adler-Milstein J, Holmgren AJ, Kralovec P, Worzala C, Searcy T, Patel V. Electronic health record adoption in US hospitals: the emergence of a digital “advanced use” divide. J Am Med Inform Assoc. 2017;24(6):1142–8.
Alsohime F, Temsah M-H, Al-Eyadhy A, Bashiri FA, Househ M, Jamal A, et al. Satisfaction and perceived usefulness with newly-implemented Electronic Health Records System among pediatricians at a university hospital. Comput Methods Programs Biomed. 2019;169:51–7.
Kaipio J, Lääveri T, Hyppönen H, Vainiomäki S, Reponen J, Kushniruk A, et al. Usability problems do not heal by themselves: national survey on physicians’ experiences with EHRs in Finland. Int J Med Inform. 2017;97:266–81. https://doi.org/10.1016/j.ijmedinf.2016.10.010.
Holanda AA, Sá HL d C e, Vieira APGF, Catrib AMF. Use and satisfaction with electronic health record by primary care physicians in a health district in Brazil. J Med Syst. 2012;36(5):3141–9.
Soderberg K, Rajamani S, Wholey D, LaVenture M. Health Reform in Minnesota: An Analysis of Complementary Initiatives Implementing Electronic Health Record Technology and Care Coordination. Online J Public Health Inform. 2016;8(3):e204.
Willis GB. Cognitive interviewing: Thousand Oaks, California: A tool for improving questionnaire design: Sage Publications; 2004.
Qualtrics. Qualtrics survey software, 2020.
May ME, Kennedy CH. Health and problem behavior among people with intellectual disabilities. Behav Anal Pract. 2010;3(2):4–12.
Kim S, Lee K-H, Hwang H, Yoo S. Analysis of the factors influencing healthcare professionals’ adoption of mobile electronic medical record (EMR) using the unified theory of acceptance and use of technology (UTAUT) in a tertiary hospital. BMC Med Inform Decis Mak. 2016;16(1):12.
Guillem Marca, Angel J Pérez, in German Blanco-Garcia, Marte, Elena Miravalles, Pere Soley, and Berta Ortiga. The use of electronic health records in Spanish hospitals. Health Inform Manag, 43(3):37–44, 2014, DOI: https://doi.org/10.1177/183335831404300305.
Resnick HE, Alwan M. Use of health information technology in home health and hospice agencies: United States, 2007. J Am Med Inform Assoc. 2010;17(4):389–95.
Pfoh ER, Abramson E, Zandieh S, Edwards A, Kaushal R. Satisfaction after the transition between electronic health record systems at six ambulatory practices. J Eval Clin Pract. 2012;18(6):1133–9.
Viitanen J, Hyppönen H, Lääveri T, Vänskä J, Reponen J, Winblad I. National questionnaire study on clinical ICT systems proofs: physicians suffer from poor usability. Int J Med Inform. 2011;80(10):708–25. https://doi.org/10.1016/j.ijmedinf.2011.06.010.
Topaz M, Ronquillo C, Peltonen L-M, Pruinelli L, Sarmiento RF, Badger MK, et al. Nurse informaticians report low satisfaction and multi-level concerns with electronic health records: results from an international survey. AMIA Annu Symp Proc. 2016;2016:2016–25. American Medical Informatics Association.
Pickering BW, Dong Y, Ahmed A, Giri J, Kilickaya O, Gupta A, et al. The implementation of clinician designed, human-centered electronic medical record viewer in the intensive care unit: a pilot step-wedge cluster randomized trial. Int J Med Inform. 2015;84(5):299–307.
Grout RW, Cheng ER, Carroll AE, Bauer NS, Downs SM. A six-year repeated evaluation of computerized clinical decision support system user acceptability. Int J Med Inform. 2018;112:74–81. https://doi.org/10.1016/j.ijmedinf.2018.01.011.
Greenfield G, Foley K, Majeed A. Rethinking primary care’s gatekeeper role. BMJ. 2016;354:i4803. https://doi.org/10.1136/bmj.i4803.
Wammes JJG, Jeurissen PPT, Verhoef LM, Assendelft WJJ, Westert GP, Faber MJ. Is the role as gatekeeper still feasible? A survey among Dutch general practitioners. Fam Pract. 2014;31(5):538–44. https://doi.org/10.1093/fampra/cmu046.
Balogh R, McMorris CA, Lunsky Y, Ouellette-Kuntz H, Bourne L, Colantonio A, et al. Organising healthcare services for persons with an intellectual disability. Cochrane Database Syst Rev. 2016;4:CD007492.
Wilkinson J, Dreyfus D, Cerreto M, Bokhour B. “Sometimes I feel overwhelmed”: educational needs of family physicians caring for people with intellectual disability. Intellect Dev Disabil. 2012;50(3):243–50. https://doi.org/10.1352/1934-9556-50.3.243.
Thompson JR, Bradley VJ, Buntinx WHE, Schalock RL, Shogren KA, Snell ME, et al. Conceptualizing supports and the support needs of people with intellectual disability. Intellect Dev Disabil. 2009;47(2):135–46. https://doi.org/10.1352/1934-9556-47.2.135.
Whitt KJ, Eden L, Merrill KC, Hughes M. Nursing student experiences regarding safe use of electronic health records: a pilot study of the Safety and Assurance Factors for EHR Resilience guides. Comput Inform Nurs. 2017;35(1):45–53.
Adler-Milstein J, Everson J, Lee S-YD. Sequencing of EHR adoption among US hospitals and the impact of meaningful use. J Am Med Inform Assoc. 2014;21(6):984–91.
Makam AN, Lanham HJ, Batchelor K, Samal L, Moran B, Howell-Stampley T, et al. Use and satisfaction with key functions of a common commercial electronic health record: a survey of primary care providers. BMC Med Inform Deci Mak. 2013;13(1):86. https://doi.org/10.1186/1472-6947-13-86.
Kihuba E, Gathara D, Mwinga S, Mulaku M, Kosgei R, Mogoa W, et al. Assessing the ability of health information systems in hospitals to support evidence-informed decisions in Kenya. Glob Health Action. 2014;7(1):24859.
Tubaishat A, AL-Rawajfah OM. The use of electronic medical records in jordanian hospitals: a nationwide survey. Comput Inform Nurs. 2017;35(10):538–45.
Karimi M, Asadi F, Moghaddasi H, Rabiei R. Features of intellectual disability information system: a comparative study. Clin Rev Case Rep. 2018;18:20.
Sockolow PS, Weiner JP, Bowles KH, Abbott P, Lehmann HP. Advice for decision makers based on an electronic health record evaluation at a program for all-inclusive care for elders site. Appl Clin Inform. 2011;2(01):18–38.
Wang T, Biedermann S. Adoption and utilization of electronic health record systems by long-term care facilities in Texas. Perspectives in Health Information Management/AHIMA, American Health Information Management Association, 9 (Spring); 2012.
Cherry B, Carter M, Owen D, Lockhart C. Factors affecting electronic health record adoption in long-term care facilities. J Healthc Qual. 2008;30(2):37–47. https://doi.org/10.1111/j.1945-1474.2008.tb01133.x.
CCHIT Certification Commission for Healthcare Information Technology. CCHIT certification for ambulatory electronic health records, 2020. URL https://www.cchit.org/.
Raymond L, Paré G, de Guinea AO, Poba-Nzaou P, Trudel M-C, Marsan J, et al. Improving performance in medical practices through the extended use of electronic medical record systems: a survey of Canadian family physicians. BMC Med Inform Decis Mak. 2015;15(1):27.
Dutch Ministry of Health Welfare and Sport. “Act amending the Act on the use of the citizen service number in health care, etc. (client rights in the case of electronic data processing)” [Wijzigingswet Wet gebruik burgerservicenummer in de zorg, enz. (cliëntenrechten bij elektronische verwerking va, 2016.
Muller G. A reference architecture primer. Eindhoven Univ. of Techn., Eindhoven, White paper; 2012.
Acknowledgements
We would like to thank all interviewees, and the professional organizations and care providers for their assistance in recruitment.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. It is part of a larger set of projects that have been funded by the Dutch Ministry of Health, Welfare and Sport.
Author information
Authors and Affiliations
Contributions
JT, HT and BS designed the study, performed interviews, designed the questionnaire and data analysis plan. JT was responsible for recruitment and programmed the online questionnaire. JT and HT wrote the initial version of the paper. JT, HT, BS, BT & GL were involved in qualitative data analysis and contributed to the final version of the paper. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Digitally signed informed consent was obtained from all subjects. According to Dutch law this (non-experimental) survey study did not need approval from an ethics review board. All the work was done according to the Netherlands code of conduct for Research Integrity from the Dutch Research Council (NWO), Royal Netherlands Academy of Arts and Sciences (KNAW), Netherlands Federation of university medical centers (NFU), TO2 federation, Netherlands Association of Universities of Applied Sciences, and the Asociation of universities The Netherlands (VSNU) (https://www.nwo.nl/en/netherlands-code-conduct-research-integrity).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Table 1. Respondents’ satisfaction with the features they reported using (N = Respondents who use the feature, followed by Mode and Range; 1 = very dissatisfied, 2 = dissatisfied, 3 = neither satisfied nor dissatisfied, 4 = satisfied, 5 = very satisfied). Table 2. (Table 5 by care professional groups) Most frequently identified HIS problems, for each group of care professionals. Daily care = 123 responses, Intellectual Disability Physician = 133 responses, Mental Health and Development = 44 responses, Other care = 32 responses. Table 3. (Table 6 by care professional groups): The features the care professionals reported missing. Daily care = 14 responses, Intellectual Disability Physician = 48 responses, Mental Health and Development = 12 responses, Other care = 10 responses.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tummers, J., Tobi, H., Schalk, B. et al. State of the practice of health information systems: a survey study amongst health care professionals in intellectual disability care. BMC Health Serv Res 21, 1247 (2021). https://doi.org/10.1186/s12913-021-07256-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-021-07256-9