Abstract
Background
Overuse is a leading contributor to the high cost of health care in the United States. Overuse harms patients and is a definitive waste of resources. The Johns Hopkins Overuse Index (JHOI) is a normalized measure of systemic health care services overuse, generated from claims data, that has been used to describe overuse in Medicare beneficiaries and to understand drivers of overuse. We aimed to adapt the JHOI for application to a commercially insured US population, to examine geographic variation in systemic overuse in this population, and to analyze trends over time to inform whether systemic overuse is an enduring problem.
Methods
We analyzed commercial insurance claims from 18 to 64 year old beneficiaries. We calculated a semiannual JHOI for each of the 375 Metropolitan Statistical Areas and 47 rural regions of the US. We generated maps to examine geographic variation and then analyzed each region’s change in their JHOI quintile from January 2011 to June 2015.
Results
The JHOI varied markedly across the US. Across the country, rural regions tended to have less systemic overuse than their MSA counterparts (p < 0.01). Regional systemic overuse is positively correlated from one time period to the next (p < 0.001). Between 2011 and 2015, 53.7% (N = 226) of regions remained in the same quintile of the JHOI. Eighty of these regions had a persistently high or persistently low JHOI throughout study duration.
Conclusions
The systemic overuse of health care resources is an enduring, regional problem. Areas identified as having a persistently high rate of systemic overuse merit further investigation to understand drivers and potential points of intervention.
Similar content being viewed by others
Background
Overuse—the provision of care where the potential for harm exceeds the potential for benefit—has been cited as a leading contributor to the high cost of the US health care system [1,2,3,4]. Overuse is often physically and psychologically harmful to patients [5,6,7] and is a definitive misuse of resources. Such wasteful utilization helps to explain why health care spending is inconsistently associated with measures of health care quality [8,9,10]. More is not always better. The identification and elimination of overused services could improve health outcomes and reduce spending, while redirecting important resources toward the delivery of high-value care [11, 12].
The direct measurement of overuse requires researchers to isolate episodes of care in which patients had a test or treatment that was contrary to published recommendations [13]. Recent studies have estimated that 14 to 25% of Medicare beneficiaries and 8% of commercially insured adults experience one or more overuse events per year [14,15,16,17]. Related work has found that the volume of low-value services delivered to Medicare patients varies across regions and physician organizations [15, 16, 18,19,20]. Analyses of individual procedures have discovered heterogeneous trends in overuse over time. Some interventions, such as renal artery stenting, have declined across years, while others have increased or remained stable [21, 22]. Thus, the measurement of individual overused services does little to inform our understanding of overuse as a broad phenomenon.
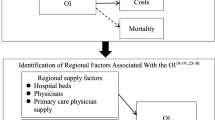
We previously defined systemic overuse as the general tendency of an organization or region to overuse medical services [23, 24]. To measure this concept, we used claims from Medicare beneficiaries and a portfolio of 20 “bellwethers” to create an index that differentiated regions by their propensity to overuse health care services. In this work, we adapt and validate the Johns Hopkins Overuse Index (JHOI) in a commercially insured US population. We then use the JHOI to examine regional variation in systemic overuse and analyze trends over time to inform whether systemic overuse is an enduring problem [25,26,27].
Methods
Data sources and sample population
We used the IBM MarketScan® Research Databases. The Commercial Claims and Encounters Database includes inpatient, outpatient, and prescription drug claims that are submitted by private health plans and employers. These are claims from more than 47 million US residents aged 0 to 64 years old with employer-sponsored private health insurance from all 50 states and the District of Columbia. The databases capture medical claims and spending for employees and their insured dependents.
We analyzed inpatient and outpatient claims in semiannual, 6-month intervals. Beneficiaries were included if they were 18 to 64 years old and had continuous health insurance coverage during the specified time period. For our analysis, individuals were assigned to a Metropolitan Statistical Area (MSA) (N = 375) or to the rural region of their state (N = 47) based on the geographic location of the primary beneficiary’s residence. Data from 2010 was used to adapt and validate the index, while the data from 2011 to June 2015 was used to examine trends over time.
Generating the index in commercial claims
Adapting the indicator procedures
The JHOI was originally developed and validated in the Medicare population. It includes 20 clinically diverse claims-based measures of overuse that are aggregated into an index [23] (Additional file 1: Table S1). We used three criteria to consistently and transparently assess whether the indicators from the original specification of the JHOI were suitable for use with these new data [28]. We assessed whether each of the indicators was “specifiable” – the indicator can be operationalized in these data; “indicated” – relevant to a 18–64 year old population of beneficiaries; and “variable” – having as much frequency and variance across regions as was observed in the Medicare data [24]. These criteria ensure that each indicator adds reliable and valuable information to the index.
Creating the index
We constructed the index as previously specified [16]. First, we created a dataset for each indicator and removed beneficiaries who were ineligible for the indicator procedure (e.g., hysterectomy in men) or in whom use of the procedure would not be considered to be an overuse event (e.g., low back imaging in a patient with metastatic cancer). We then concatenated these data into a single dataset to construct an unbalanced panel. Here we created the dependent variable, denoted Pijk, which is equal to 1 if there was overuse in the ith beneficiary, as measured by the jth procedure in the kth region, and equal to 0 if otherwise. Our multilevel model is described in the following equation:
where Xi is a vector of patient specific factors, ψj is a set of procedural fixed effects, and Φk is a set of regional fixed effects. The patient specific factors included age, sex, and a claims-based count of diseases derived from the Agency for Healthcare Research and Quality (AHRQ) Clinical Classifications Software (CCS) for single-level diagnoses [29]. From each model, the Φk estimate represents the systemic tendency for the kth region to overuse across the j procedures. This measure was then standardized to create the JHOI as a Z-score, where the value of the index for the kth region is estimated as:
where \( \overline{\Phi} \) is the average of the 422 regional fixed effects and SD(Φ) is the standard deviation across the fixed effects that were estimated in Eq. 1. Through standardizing the index, we also created a test statistic. We considered regions with Z-scores more extreme than 2.0 or − 2.0 to be outlier regions.
To examine the effect of risk-adjustment on variation in the index, we added each of the patient specific factors to Eq. 1 in a step-wise fashion. First, a model without risk-adjustment was used, then models with patient demographics and clinical co-morbidities were created. To make a final determination on risk-adjustment, we examined changes in each model’s R-squared and calculated the Spearman rank correlation between the different versions of the JHOIk.
Validating the index
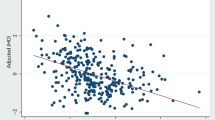
Given the definition of overuse, we hypothesized that systemic overuse should be associated with higher aggregate costs and without clinical benefit in a region. With Spearman rank correlation, we assessed the relationship between regional systemic overuse (JHOIk) and regional measures of total costs and total mortality. Because Medicare spending is less susceptible to price and local market effects, costs were tabulated using publicly available Medicare files [30]. Total regional mortality was calculated for the 18–64 year old population using publicly available information from the Centers for Disease Control and Prevention’s Wide-ranging ONline Data for Epidemiologic Research (CDC WONDER) database [31].
Geographic variation and trends
The JHOIk were generated for each 6-month period, from January 2011 to June 2015. To illustrate geographic variation, we generated a map displaying the JHOIk for each half year period with each region assigned to a quintile based on its Z-score.
To examine changes across the 4.5 year period, we calculated the Spearman rank correlation for each JHOIk compared to the base period, which was the first half of 2011. Additionally, we generated a “difference score” for each region by subtracting the JHOIk quintile for each time period from the prior time period. These values were then summed in order to estimate net change within a given geography across all years of observation. To visualize geographic patterns in net change over time, we generated a map of the difference in the JHOIk quintile between the first and last time period. We then computed the proportion of regions that had persistently high or persistently low systemic overuse, defined as having a JHOIk in the top or bottom quintile for all time periods. We utilized a lasagna plot to visualize region-specific trajectories across study duration [32].
Analyses were performed using SAS version 9.4 and Stata 14 software. Maps were created using the spmap command in Stata [33, 34]. Data from South Carolina are not displayed in maps due to contractual restrictions. Our study was determined to be exempt from review by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board (IRB8729).
Results
The final sample included more than 300 million beneficiary-level observations from 2010 to June 2015, with an average of 27,366,474 individuals per time period. The data included information for beneficiaries in all possible geographic units, with an average sample size of 69,331 beneficiaries and a minimum of 1087 beneficiaries per region. The total sample was 52% female and had an average age of 42.3 years (SD 13.6). Across the study period, approximately 86% of beneficiaries resided in an MSA. As required, age ranged from 18 to 64 years old and beneficiaries had a full 6 months of insurance coverage during a specified time period.
The JHOI in commercial claims
Among the 20 indicators that were used to measure systemic overuse with Medicare claims [16, 24], we found that 19 of these 20 procedures met our criteria for application to a younger, commercially insured population. The indicator entitled “More than 1 emergency department visit in the last 30 days of life” could not be operationalized in these commercial claims due to a lack of information on deaths outside of the hospital. The remainder of the 19 procedures could be specified in this new data, are clinically relevant to the 18–64 year old population, and had satisfactory frequency and variation across regions (Table 1). The retained 19 indicators included 13 diagnostic tests, 2 tests used for screening, 1 for monitoring, and 3 therapeutic procedures. The clinical areas included 4 relevant to primary care practice, 3 to otolaryngology, 3 to radiology, 2 to cardiology, and 1 each to neurology, emergency practice, allergy, oncology, urology, physical therapy, and surgery. During each semiannual period, an average of 4.0% (range: 3.9 to 4.2%) of commercially insured adults experienced one or more of the indexed overuse events. This rate consistently varied by more than fourfold across the country (e.g., 1.7 to 8.2% in January through June 2010). Individuals were subjected to between 0 and 5 of the 19 procedures.
The index did not significantly change with alternative risk-adjustment methods. The Spearman rank correlation between the unadjusted and the fully risk-adjusted JHOI was high (ρ = 0.98, p < 0.0001) (Additional file 1: Figure S1). The regional fixed effects alone accounted for an R2 of 18.93%. The addition of patient demographics and clinical co-morbidities only increased the R2 by 0.02 and 0.13%, respectively. We opted to use the age and sex-adjusted JHOI for the remainder of our analyses.
In the first half of 2010, the JHOIk had a mean of 0 and standard deviation of 1, with a minimum of − 2.60 and maximum of 3.23 (Additional file 1: Figure S2). Regions with a JHOI that was in the upper or lower tail of the standard normal distribution are listed in Table 2. As hypothesized for the validation, the index was positively correlated with total per capita spending on Medicare beneficiaries (ρ = 0.32, p < 0.001); annual per capita costs were $1181 higher in regions with a JHOI in the 90th percentile as compared to regions with a JHOI in the 10th percentile. Similarly consistent with our validation hypothesis, the index was not directly associated with an indicator of clinical benefit, operationalized as mortality in the 18–64 year old population (ρ = 0.02, p = 0.61) (Additional file 1: Figures S3 and S4).
Geographic variation and trends
The JHOI showed marked regional variation (Fig. 1). As illustrated by the data from 2015, systemic overuse was prevalent in a number of coastal metropolitan regions. Examples include multiple MSAs in Washington, California, Texas, Florida, New Jersey, and New York. Six of the top 10 overusing regions were metropolitan areas in California. This group includes the most overusing region, the Oxnard–Thousand Oaks–Ventura, California MSA. While much of the central and northwestern parts of the US had relatively low rates of systemic overuse, Chicago, IL and Pittsburgh, PA are metropolitan outliers with high systemic overuse. Across the entire country, the rural regions of states tended to have less systemic overuse than their MSA counterparts (p < 0.01). Illustrating this, only 4 rural regions were in the top quintile of systemic overuse, while 18 rural regions were in the bottom quintile.
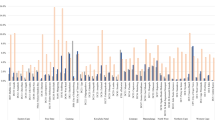
There was a positive, significant correlation in the JHOI across years. This ranged from ρ = 0.96 (p < 0.001) between the first and second half of 2011 and ρ = 0.79 (p < 0.001) between the first halves of 2011 and 2015. The strength of the correlation decreased with the distance between time periods (Additional file 1: Table S2). Across the entire observation period, the average difference score was 0.05 quintiles and the majority of regions, 53.68% (N = 226), experienced zero net change. The largest net changes were + 3 quintiles (N = 2 regions) and − 3 quintiles (N = 9 regions). A map of the net change in the JHOI between 2011 and 2015 is presented in Fig. 2. Patterns of increasing or decreasing overuse did not differ across rural and urban regions.
Numerous regions fell into the top or bottom quintile of the JHOI for all time periods (Fig. 3). Specifically, 37 (8.76%) regions had persistently high systemic overuse and 43 (10.18%) regions had persistently low systemic overuse. Only metropolitan areas met criteria for the persistently high overuse phenotype, while 9 rural regions had persistently low systemic overuse. Examples of persistently high overusing metropolitan areas include Pittsburgh, PA, Corpus Christi, TX, Miami, FL, Los Angeles–Long Beach–Glendale, CA, and New York–Wayne–White Plains, NY-NJ (Additional file 1: Table S3).
Region-specific changes in the Johns Hopkins Overuse Index from 2011 to 2015. Each region’s trajectory over time is a horizontal layer. The simultaneous plotting of trajectories results in a stacking of layers. Shading is used to represent the 5 JHOI quintiles. The JHOI quintile from the first half of 2011 fixes the vertical position of each region
Discussion
In the United States, more than 60% of insured individuals have commercial insurance [35]. Despite this, our knowledge about health care utilization is often based on analyses of data from Medicare beneficiaries [36]. In this work, we generated and validated an index to measure systemic overuse in 18 to 64 year old adults with commercial insurance. The JHOI exposed significant variation and revealed a distinct geographic signature of systemic overuse, with higher scores in coastal metropolitan areas and lower scores in central and rural regions of the country. These findings are similar to what has been observed in the Medicare population [15, 16].
Relatively few studies have examined patterns of overuse over time. Those that do tend to focus on a handful of individual low-value services at a national level [21, 22]. One such study analyzed nationwide trends for 16 different services, from 2009 to 2014. Representative of this small but growing area of research, some of the low-value services were successfully deadopted, while many others remained stable or became increasingly common over time [21]. As older, low-value technologies become unpopular there is the potential for new, equally low-value technologies to emerge [37]. While measuring any one specific service may be a valid way to evaluate the impact of a local quality improvement initiative, a single measure cannot reliably characterize overuse as a broad phenomenon. Additionally, any one measure has the potential to be distorted by differences in coding, whether intentional or unintentional.
With a collection of overuse bellwethers, we found that systemic overuse is a resolute problem. From 2011 to 2015, the majority of regions experienced zero change in JHOI quintile, making “consistency” the most common phenotype. This was particularly true in the tails—19% of regions were in the top or bottom quintile throughout study duration. The 37 regions that had persistently high rates of systemic overuse support the concept of a distinguishable “culture of overuse” [2, 13, 16]. These findings should encourage policy makers and health system leaders to address structural and system-wide drivers of overuse, which may be more impactful than a focus on individual overused procedures.
By our adapting an index that was originally developed in the Medicare population, there is now a validated tool to measure systemic overuse across the adult lifespan. This work adds to the growing literature on the direct measurement of overuse in claims data. While an indirect assessment of waste that is based on variation in risk-adjusted utilization or spending can provide information on the potential scale of the problem, these methods cannot distinguish between variation in underuse or overuse [13, 17]. For this reason, direct measures are better able to differentiate between more and less efficient regions. Moreover, we found that the measurement of systemic overuse is not meaningfully impacted by differences in patient health status. Taken together, the observed variation in the JHOI indicates that there is substantial room to reduce overuse.
This paper is not without limitations. While some may not agree with each of the included indicators, they were selected because they were identified by reputable professional bodies as being overused services (Additional file 1: Table S1). Additionally, this set of indicators includes diverse clinical activities and each indicator itself is regionally variable. We recognize that some fraction of events may have been misclassified as overuse, but it is unlikely that these clinical encounters would occur in a way that would systematically bias the JHOI or alter its interpretation, particularly given that we are reporting relative differences between regions. As the literature on overused procedures continues to grow, the included indicators might even be swapped out, similar to how the Consumer Price Index regularly changes what is in its basket of goods.
The studied population is comprised of enrollees from large employers and group health plans. While the data include close to 25% of the 18 to 64 year old population with employer-based health insurance in the US [38], our analyses may not be generalizable to the entire commercially-insured US population. We are also unable to control for differences in patient preferences regarding receipt of health care, however prior research has indicated that this is unlikely to be a strong driver of variation in overuse [39, 40]. While not perfectly representative, the included population raises intriguing operational questions; we would expect that self-insured employers have the motivation and power to reduce health care inefficiencies among their beneficiaries. A minor limitation is that we had to allocate beneficiaries to regions based on their primary residence rather than on where the indexed care was received. To the extent that residents of rural regions may travel to urban areas to receive care, our analyses would underestimate the association between metropolitan areas and systemic overuse.
Finally, the JHOI is a relative measure of systemic overuse—it compares the extent of health care overuse in one area relative to the national average. This precludes us from being able to make statements about the absolute magnitude of systemic overuse. It also prevents a direct analysis of the costs that are associated with this phenomenon. While we have demonstrated that the JHOI is associated with increased health care spending, it is infeasible to directly measure the entire universe of overused procedures and their downstream consequences. Further, overuse of healthcare contributes to patient harm in a way that may not be directly quantifiable.
Several extensions of this research would be useful. While we demonstrated that systemic overuse varies regionally, it may be informative to examine patterns of systemic overuse across different insurance types, different systems of care, and different patient populations. Payer type and insurance status do not seem to influence rates of overuse of individual services, and we would expect these trends to hold when overuse is more broadly measured [41,42,43]. We identified regions that had persistently high or persistently low systemic overuse; investigating the drivers of this phenomenon is essential. Studies in the Medicare population have identified associations between overuse and certain regional characteristics of the health care system, such as the number of specialists in an area, the supply of hospital resources, and physician concentration [15, 19]. It would also be worthwhile to examine the few regions that experienced a meaningful reduction in systemic overuse. As measures of overuse become an increasingly common component of performance measurement, additional research is also needed to understand the relationship between the JHOI and other indicators of health care quality [44,45,46].
This research relies on the premise that geography is a useful unit of analysis for policy. While this work highlights meaningful variation in wasteful health care utilization at the level of the MSA, it does not necessarily mean that this unit of analysis is the right unit for an intervention related to systemic overuse. Aggregating at any level of geography is likely to minimize the true variation that exists and pull the extremes to the regional mean—clinicians within any geographic area are known to have different practice patterns [18, 20, 36, 47, 48]. There are many reasons to believe that health care systems or networks of clinicians might be better targets for intervention. With that said, choosing to implement a national, state, or system-level policy involves tradeoffs related to administrative burden and need for program specificity [49]. Operationalizing the JHOI across and within multiple geographic and non-geographic units of analysis may inform the deployment of interventions to reduce systemic overuse.
Conclusions
We demonstrated that the measurement of systemic overuse is feasible in commercial claims data. We found that systemic overuse varies across geographies, and that a number of regions have a distinguishable culture of overuse. These findings are similar to those of previous studies among older adults and children, which suggests that interventions to improve care efficiency should include patients across the entire age spectrum [50]. Systemic overuse is a persistent, regional issue which will require experimentation and collaboration by many different stakeholders.
Abbreviations
- AHRQ:
-
Agency for Healthcare Research and Quality
- CA:
-
California
- CCS:
-
Clinical Classifications Software
- CDC:
-
Centers for Disease Control and Prevention
- FL:
-
Florida
- JHOI:
-
Johns Hopkins Overuse Index
- MSA:
-
Metropolitan Statistical Area
- NJ:
-
New Jersey
- NY:
-
New York
- PA:
-
Pennsylvania
- SD:
-
Standard deviation
- TX:
-
Texas
- US:
-
United States
- WONDER:
-
Wide-ranging ONline Data for Epidemiologic Research
References
Agency for Healthcare Research and Quality. Glossary: underuse, overuse, misuse. https://psnet.ahrq.gov/glossary/u (cited 16 Nov 2018).
Emanuel EJ. The perfect storm of overutilization. JAMA. 2008;299:2789–91.
Institute of Medicine. Best care at lower cost: the path to continuously learning health care in America. http://www.nationalacademies.org/hmd/Reports/2012/Best-Care-at-Lower-Cost-The-Path-to-Continuously-Learning-Health-Care-in-America.aspx (cited 16 Nov 2018).
Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307:1513–6.
Shaffer VA, Scherer LD. Too much medicine: behavioral science insights on overutilization, overdiagnosis, and overtreatment in health care. Policy Insights Behav Brain Sci. 2018;5:155–62.
O’Donoghue C, Eklund M, Ozanne EM, et al. Aggregate cost of mammography screening in the United States: comparison of current practice and advocated guidelines. Ann Intern Med. 2014;160:145.
Lipitz-Snyderman A, Korenstein D. Reducing overuse—is patient safety the answer? JAMA. 2017;317:810–1.
Fisher ES, Wennberg DE, Stukel, et al. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138:273–87.
Fowler FJ, Gallagher PM, Anthony DL, et al. Relationship between regional per capita Medicare expenditures and patient perceptions of quality of care. JAMA. 2008;299:2406–12.
Sirovich BE, Gottlieb DJ, Welch HG, et al. Regional variations in health care intensity and physician perceptions of quality of care. Ann Intern Med. 2006;144:641–9.
Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27:759–69.
Miller G, Rhyan C, Beaudin-Seiler B, et al. A framework for measuring low-value care. Value Health. 2018;21:375–9.
Brownlee S, Chalkidou K, Doust J, et al. Evidence for overuse of medical services around the world. Lancet. 2017;390:156–68.
Schwartz AL, Landon BE, Elshaug AG, Chernew ME, McWilliams JM. Measuring low-value care in Medicare. JAMA Intern Med. 2014;174:1067–76.
Colla CH, Morden NE, Sequist TD, et al. Choosing wisely: prevalence and correlates of low-value health care services in the United States. J Gen Intern Med. 2014;30:221–8.
Segal JB, Nassery N, Chang HY, et al. An index for measuring overuse of health care resources with Medicare claims. Med Care. 2015;53:230–6.
Reid RO, Rabideau B, Sood N. Low-value health care services in a commercially insured population. JAMA Intern Med. 2016;176:1567–71.
Schwartz AL, Zaslavsky AM, Landon BE, et al. Low-value service use in provider organizations. Health Serv Res. 2018;53:87–119.
Zhou M, Oakes AH, Bridges JF, et al. Regional supply of medical resources and systemic overuse of health care among Medicare beneficiaries. J Gen Intern Med. 2018;33(12):2127-31.
Mafi JN, Wee CC, Davis RB, et al. Association of primary care practice location and ownership with the provision of low-value care in the United States. JAMA Intern Med. 2017;177:838–45.
Carter EA, Morin PE, Lind KD. Costs and trends in utilization of low-value services among older adults with commercial insurance or Medicare advantage. Med Care. 2017;55:931–9.
Rosenberg A, Agiro A, Gottlieb M, et al. Early trends among seven recommendations from the choosing wisely campaign. JAMA Intern Med. 2015;175:1913–20.
Nassery N, Segal JB, Chang E, et al. Systematic overuse of healthcare services: a conceptual model. Appl Health Econ Health Policy. 2015;13:1–6.
Segal JB, Bridges JF, Chang HY, et al. Identifying possible indicators of systematic overuse of health care procedures with claims data. Med Care. 2014;52:157–63.
Badgery-Parker T, Pearson SA, Chalmers K, et al. Low-value care in Australian public hospitals: prevalence and trends over time. BMJ Qual Saf. 2019;28(3):205-14.
McAlister FA, Lin M, Bakal J, Dean S. Frequency of low-value care in Alberta, Canada: a retrospective cohort study. BMJ Qual Saf. 2018;27:340–6.
Mafi JN, Parchman M. Low-value care: an intractable global problem with no quick fix. BMJ Qual Saf. 2018;27:333–6.
Chalmers K, Badgery-Parker T, Pearson SA, et al. Developing indicators for measuring low-value care: mapping choosing wisely recommendations to hospital data. BMC Res Notes. 2018;11:163.
HCUP Clinical Classifications Software (CCS) for ICD-9-CM. Healthcare cost and utilization project (HCUP). Rockville: Agency for Healthcare Research and Quality; 2008. www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed 28 Nov 2018
Geographic Variation Public Use File. 2018. United States Centers for Medicare and Medicaid Services, Baltimore. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Geographic-Variation/GV_PUF.html. Accessed 28 Nov 2018.
United States Department of Health and Human Services (US DHHS), Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS), Underlying cause of death 1999-2016 on CDC WONDER online database, released 2017. https://wonder.cdc.gov/ucd-icd10.html. Accessed 28 Nov 2018.
Swihart BJ, Caffo B, James BD, et al. Lasagna plots: a saucy alternative to spaghetti plots. Epidemiology. 2010;21:621–5.
StataCorp. Stata statistical software: release 14. College Station: StataCorp LLC; 2015.
SAS Institute Inc. SAS 9.4. Cary: SAS Institute, Inc.; 2013.
Hartman M, Martin AB, Espinosa N, et al. National health care spending in 2016: spending and enrollment growth slow after initial coverage expansions. Health Aff (Millwood). 2018;37:150–60.
IOM (Institute of Medicine). Variation in health care spending: target decision making, not geography. Washington, DC: The National Academies Press; 2013.
Garber S, Gates SM, Keeler EB, et al. Redirecting innovation in U.S. health care: options to decrease spending and increase value. https://www.rand.org/content/dam/rand/pubs/research_reports/RR300/RR308/RAND_RR308.pdf. Accessed 16 April 2019.
Henry J Kaiser Family Foundation. Health insurance coverage of adults 19–64. https://www.kff.org/other/state-indicator/adults-19-64/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed 28 Nov 2018.
Schwartz AL, Chernew ME, Landon BE, et al. Changes in low-value services in year 1 of the Medicare Pioneer accountable care organization program. JAMA Intern Med. 2015;175:1815–25.
Cutler DM, Skinner JS, Stern AD, et al. Physician beliefs and patient preferences: a new look at regional variation in health care spending. Cambridge: National Bureau of Economic Research Working Paper Series; 2013.
Colla CH, Morden NE, Sequist TD, et al. Payer type and low-value care: comparing choosing wisely services across commercial and Medicare populations. Health Serv Res. 2018;53:730–46.
Charlesworth CJ, Meath TH, Schwartz AL, et al. Comparison of low-value care in Medicaid vs commercially insured populations. JAMA Intern Med. 2016;176:998–1004.
Keyhani S, Falk R, Howell EA, et al. Overuse and systems of care: a systematic review. Med Care. 2013;51:503–8.
Baker DW, Qaseem A, Reynolds PP, et al. Design and use of performance measures to decrease low-value services and achieve cost-conscious care. Ann Intern Med. 2013;158:55–9.
de Vries EF, Struijs JN, Heijink R, et al. Are low-value care measures up to the task? A systematic review of the literature. BMC Health Serv Res. 2016;16:405.
Chan KS, Chang E, Nassery N, et al. The state of overuse measurement: a critical review. Med Care Res Rev. 2013;70:473–96.
Rosenberg BL, Kellar JA, Labno A, et al. Quantifying geographic variation in health care outcomes in the United States before and after risk-adjustment. PLoS One. 2016;12:e0166792.
Harvard Medical School Department of Health Care Policy. Final technical report: geographic variation in health care spending, utilization, and quality among the privately insured. http://www.nationalacademies.org/hmd/%7E/media/Files/Report%20Files/2013/Geographic-Variation/Sub-Contractor/Harvard-University.pdf.
Khullar D, Wolfson D, Casalino LP. Professionalism, performance, and the future of physician incentives. JAMA. 2018. https://doi.org/10.1001/jama.2018.17719. Accessed 16 April 2019.
Chua KP, Schwartz AL, Volerman A, et al. Use of low-value pediatric services among the commercially insured. Pediatrics. 2016;138:e20161809.
Acknowledgements
Not applicable.
Funding
This study is funded by a research grant from the National Institute for Health Care Management and the National Institute on Aging, United States (K24 AG049036-01A1). The funders had no role in the design of the study, collection, analysis and interpretation of the data or writing of the manuscript.
Availability of data and materials
The SAS code used to generate the Johns Hopkins Overuse Index is available upon request to the authors.
Author information
Authors and Affiliations
Contributions
AHO and JBS developed the research question. HC facilitated access to the data and assisted with programming the indicators. AHO performed the analysis and drafted the article. JBS provided overall supervision and direction to the project and assisted in drafting the article. All authors read and approved the final article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our study was determined to be exempt from review by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board (IRB8729). Patient consent was not required for this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Description of indicator procedures included in the Johns Hopkins Overuse Index and results from supplementary analyses. (PDF 249 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Oakes, A.H., Chang, HY. & Segal, J.B. Systemic overuse of health care in a commercially insured US population, 2010–2015. BMC Health Serv Res 19, 280 (2019). https://doi.org/10.1186/s12913-019-4079-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-019-4079-0