Abstract
Background
Hepatitis C is an important public health problem about which there is currently scarce epidemiological information. The objective of this study is to describe and analyse the demographic and epidemiological characteristics of hospitalized cases of hepatitis C in the Spanish population between 2004 and 2013.
Methods
The study uses the Hospital Discharge Records Database of the Spanish National Health System. It is a retrospective descriptive epidemiological study. The variables analysed were year of infection, age, sex, diagnostic category, days admitted and co-morbidity.
Results
There have been a total of 351,996 hospitalizations; 225,138 men (64%) and 126,858 women (36%). They are divided between acute hepatitis 8161 (2.3%); chronic hepatitis 325,185 (92.4%) and unspecified hepatitis 18,650 (5.3%). The mean age for men is 53.7 (+/−15.2) and for women 62.3 (+/−17.3). 22.8% also present with an Human immunodeficiency virus (HIV) disease coinfection, and 14.7% with opioid dependencies. The trend is for a gradual increase in cases without statistical significance.
Conclusions
The Hepatitis C cases hospitalized had high levels of chronicity, which entails two distinct patterns of illness in men and women – who are affected in different age ranges.
Similar content being viewed by others
Background
Despite the fact that hepatitis C is a disease of particular relevance to public health, the epidemiological information available remains scarce. This, in part, is due to the intrinsic characteristics of a disease which is difficult to diagnose, remains asymptomatic for many years and becomes chronic in a high percentage of cases. It is estimated that hepatitis C affects 150 million people globally, of which 350,000 to 500,000 die each year as a result. In the World Health Organization (WHO) European Region it is estimated that there are 15 million people infected [1]. In 2013 the European Centre for Disease Prevention and Control (ECDC) was notified of 31,513 cases of hepatitis C in 26 countries [2], of which 569 (1.8%) were acute, 4776 (15.2%) were chronic, and 23,230 (73.7%) were unknown. A number of studies have been undertaken in Spain to evaluate the prevalence of hepatitis C [3,4,5,6,7,8,9,10,11,12,13], in general they are reviews [3] or local-level studies, carried out in both distinct populations and the general population [4,5,6,7,8] (with a range of prevalence between 0.74% and 2.6%), school-age children [9] (0.36%), pregnant women [10,11,12] (0.4-1.4%) and the working population [13] (0.6%).
In the recently approved Strategic Plan for Tackling Hepatitis C in the Spanish National Health System [14], it is estimated that 1.7% of the Spanish adult population (688000) have antibodies against hepatitis C and 1.2% of adults have viremia (472000) [15, 16].
In addition to studies on the prevalence, other studies of mortality and disease burden show that when the chronic complications of hepatitis C – like cirrhosis and hepatocellular carcinoma – are taken into account, Hepatitis C leads the list of infectious disease related mortality in Spain [17] and is the leading cause of disability-adjusted-life-years (DALYs) among transmissible diseases in Spain [18].
The Hospital Discharge Records Database of the Spanish National Health System (CMBD in its Spanish acronym) registers the cases in National Health Service hospitals, as well as a number of private hospitals, with a 90% level of coverage at present [19]. The system collects information regarding the patient, the disease and the hospital. The information system based on the CMBD can be a useful tool to better understand the epidemiological pattern of the disease, and the associated assistance required.
The objective of this study is to describe and analyse the demographic and epidemiological characteristics of those cases hospitalized with a diagnosis of hepatitis C and in addition to identifying trends in the hospitalizations. The study uses the CMBD database as an information system.
Methods
This is a descriptive retrospective epidemiological study of the hospitalizations with hepatitis C diagnoses in the Spanish population from 2004 to 2013.
It has used data from the CMBD, which have been coded with the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) from the World Health Organisation [20].
CMBD is the Spanish mandatory hospital discharge registry. Similar registries are in place in western countries. In Spain the registry uses the ICD-9 CM for codifying the illnesses and in 2017 will begin to use the International Classification of Diseases, Tenth Revision (ICD-10). The registry does not permit distinguishing between hospitalization and patients. CMBD has been consolidated as the principal source for knowing about the causes of disease which receive treatment in hospitals. Its application to epidemiological studies is shown by many scientific articles [21,22,23].
It has studied all of those hospital admissions in which a primary or secondary diagnosis with one of the following codes appeared: 070.41 (acute hepatitis C with hepatic coma), 070.44 (chronic hepatitis C with hepatic coma), 070.51 (acute hepatitis C without mention of hepatic coma), 070.54 (chronic hepatitis C with no mention of hepatic coma), 070.70 (unspecified viral hepatitis C without hepatic coma), 070.71 (unspecified viral hepatitis C with hepatic coma).
The studied variables were: year of admission (2004-2013), sex (male/female), age, diagnosis (acute, chronic or unspecified hepatitis C) and days hospitalized. Co-morbidity with HIV has been studied (ICD-9-CM: 042, for Human immunodeficiency virus [HIV] disease and V08, for asymptomatic HIV). The database was cleaned to remove any potential duplicates of hospitalizations. The entries without complete values for age and sex were removed, as well as those entries with extreme values – using a refined average stay. From the initial 357,731 entries, 1.6% was eliminated and a total of 351,996 have been analysed.
For the computation of the rates we have used the population estimations of the studied period provided by the Spanish National Statistics Institute. [24]. For the purposes of standardization, the European population has been used [25].
Statistical analysis
A descriptive analysis was carried out, and in order to compare the qualitative variables Pearson’s chi-squared test was used. To compare the quantitative values, Student’s t technique was used for normal distributions, and Mann-Whitney’s U, as a non-parametric test, for non-normal distributions. Values of p < 0.05 were considered statistically significant.
For the statistical analysis we have used IBM-SPSS ver. 22 and for the trend-analysis, Jointpoint Regression Program 4.2.0.2., which, through Poisson regression models, allows the calculation of Annual Percent Change (APC) and the estimation of trend change points.
Results
Our study provides an analysis of 351,996 hospitalizations over a 10-year period, which equates to approximately 35,000 per year.
Table 1 shows the distribution of hospitalizations for the studied period, by sex, year and diagnostic category.
During the 10 years studied (2004-2013) a total of 351,996 hepatitis C hospitalizations were recorded (64% men; 36% women p = 0.031) with a 1.7 ratio of men to women. By diagnostic category, the cases are distributed between acute hepatitis (8161; 2.3%), chronic hepatitis (325,185; 92.4%) and unspecified hepatitis (18,650; 5.3%), maintaining the same ratios between men and women.
Age presents a bimodal distribution (Figs. 1 and 2, Table 2). The age group with the highest frequency in men is between 40 and 49 years (N 75025; 33.35%) with a smaller peak in the 70–79 age group (N 31363; 13.90%). In women the most frequent age group is 70–79 years (N 34439; 27.10%) with a smaller peak in the 40–49 age groups (N 20752, 16.40%).
Highest frequency in men occurs at age 45 and in women at 76 years. The median in men is 50 (interquartile range: 42–66) and in women is 66 (interquartile range 47–77). These differences are statistically significant p < 0.001.
A study of co-morbidity highlights that 22.8% of hospitalizations for hepatitis C also presented with HIV and 14.7% presented with opioid addiction. Both are more frequent in men than women p < 0.0001 (Table 3).
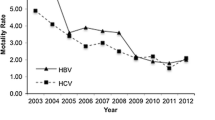
Hospitalization rates are shown in Fig. 3. They present a slight upward trend, which is statistical not significant, for both men and women – although some change-points can be observed. The trend for men is for an APC of 1.02 (p > 0.05) with a change-point in 2010; for women the APC is 0.81 (p > 0.05) with a change-point in 2007.
Discussion
To the best of our knowledge, this is the first study of hepatitis C hospitalizations at a national level during a recent 10-year period. The results show a high rate of chronicity, with over 90% of cases, and significant differences for sex and age in the epidemiological pattern of the disease.
Of those admitted with this disease 64% are men and 36% are women, although the proportions of hepatitis C types remain similar for both sexes.
When we compare our data with that of the surveillance system of ECDC, we can see that there is a 1.9 ratio of men to women in European cases [2], while in our study it was a little less: 1.7. The majority of the cases recorded in Europe are classified as “unspecified hepatitis”, due to the difficulties in classifying correctly, although it is assumed that the majority are chronic hepatitis, as found in our study. The most numerous group in the European study were 25 to 44 year-olds, somewhat younger than in our study, in which the 40–49 age range in men and 70–79 age range in women were the most numerous.
In our study the age of hospitalization presents a bimodal distribution in men and women with a reversed image with a most frequent age group 40-49 years in men opposite to 70-79 years in women.
The bimodal distribution suggests that two populations with different patterns of the disease can be observed in these findings, a younger population in which men predominate and an older population in which women predominate. This distribution may indicate that the populations have been subjected to different risk factors in the acquisition of the disease, something which other studies have already noted [3]. On one hand, hepatitis C principally affects young men, and in this group the prevalence of co-infection with HIV and that of opioid dependence is much higher than for women. According to a number of studies, the rate of hepatitis C infection in people with HIV is close to 30% [26]. For populations of injection drug users there is a substantial range of infection between 21 and 86% [27, 28]. On the other, for the predominantly more advanced ages in which infection in women is found, it is probable that the infections were a consequence of nosocomial infections in the past, as a result of blood transfusions before 1990 or the use of unsterilized syringes before 1975.
A possible hypothesis is that in the past women could have been subjected to an additional risk-factor, as pregnancy and birth admissions are principal causes of hospitalization. Some studies estimate that nosocomial transmission accounts for 15–25% of cases [29, 30].
The data of hospitalizations in our study are consistent with those found in another study carried out in Spain in which more than 3000 serum samples of patients were analyzed and differences were found in the genotypes related to the age cohort, with differences between those born before and after 1950 being found [31].
Although the trend in women is less noticeable than that in men, as is reflected by the percentage of annual change, we have identified a point of inflection or change in both (in 2010 for men and 2007 for women). Therefore, with less effect there is also a slight increasing trend.
This slight upward trend in hospitalization rates adjusted for age for hepatitis C goes contrary to the trend for general hospital admissions, which have declined during the last few years. In 2013 there was a decrease of 0.47% with respect to 2012 [19], more prominent in women – owing to a decrease in the number of consultations for pregnancy, delivery and puerperium.
However, it is important to highlight a number of limitations with the use of the CMBD related to the fact that it was created for hospital management and therefore its applications in epidemiology can be limited. As CMBD data are anonymous, it is impossible to identify hepatitis C cases being hospitalized more than once for the duration of the disease. We have taken into account new hospitalizations and readmissions, so all hospitalizations are included. Therefore the results should be taken with caution and the number of patients should not be inferred, because in that case it would be somewhat overestimated. We think that this limitation does not affect the disease trend and in the absence of direct incidence data is a good proxy for the behavior of the disease. And in the other hand, the information is easily accessible and the data cover the whole Spanish population, this means that the epidemiological information refers to the whole hospitalized Spanish population and it covers a period of 10 years.
Predictive mathematical models for hepatitis C indicate that, with the current treatment rate, the total number of viral hepatitis C infections could decrease or remain stable. Nevertheless, the number of patients with chronic hepatitis will tend to increase, with a consequent increase in mortality, morbidity and their associated costs. Therefore, alternative strategies are required [32].
The challenge now is to diagnose the unknown cases of hepatitis C, as it is estimated that only 35% of cases have been diagnosed [33].
Conclusions
Hospitalizations for hepatitis C entail a high level of chronicity, and they occur in two distinct patterns for women and men, for whom different age groups are affected. It is our view that the CMBD can be a useful tool to assess the scale of the problem and evaluate trends in hepatitis C. The knowledge of the epidemiological pattern of the disease is of considerable use to help orient health policy.
Abbreviations
- APC:
-
Annual Percent Change
- CMBD:
-
Hospital Discharge Records Database
- DALYs:
-
Disability-adjusted-life-years
- ECDC:
-
European Centre for Disease Prevention and Control
- HIV:
-
Human immunodeficiency virus
- ICD-10:
-
International Classification of Diseases, Tenth Revision
- ICD-9-CM:
-
International Classification of Diseases, Ninth Revision, Clinical Modification
- WHO:
-
World Health Organization
References
World Health Organization. Guidelines for the screening, care and treatment of persons with hepatitis C infection. Geneva: World Health Organization; 2014.
European Centre for Disease Prevention and Control. Hepatitis C surveillance in Europe – 2013. Stockholm: ECDC; 2015.
Bruguera M, Forns X. Hepatitis C in Spain. Med Clin (Barc). 2006;127:113–7.
Riestra S, Fernández E, Leiva P, Garcia S, Ocio G, Rodrigo L. Prevalence of hepatitis C virus infection in the general population of northern Spain. Eur J Gastroenterol Hepatol. 2001;13:477–81.
Domínguez A, Bruguera M, Vidal J, Plans P, Salleras L. Community-based seroepidemiological survey of HCV infection in Catalonia. Spain J Med Virol. 2001;65:688–93.
Sola R, Cruz de Castro E, Hombrados M, Planas R, Coll S, Jardi R, et al. Prevalence of hepatitis B and hepatitis C viruses in different counties of Catalonia, Spain: cross-sectional study. Med Clin (Barc). 2002;119:90–5.
Chimeno MM, Chocarro A, Brezmes P, Ochoa C, Perez J. Seroprevalence of hepatitis C virus in the general population. Enferm Infecc Microbiol Clin. 2002;20:64–7.
López-Izquierdo R, Udaondo MA, Zarzosa P, García-Ramón E, Garcinuño S, Bratos MA, et al. Seroprevalence of viral hepatitis in a representative general population of an urban public health area in Castilla y Leon (Spain). Enferm Infecc Microbiol Clin. 2007;25:317–23.
Gil Miguel A, Ruedas A, Santos Santos M, Rey Calero YJ. Prevalence of hepatitis C virus infection in school children in an urban and suburban area of Madrid. Aten Primaria. 1996;17:521–2.
Suárez González A, Solís Sánchez G, Otero Guerra L, de la Guerra G V, Navascués C Á, López R G. The prevalence of markers for the hepatitis a and B viruses in the population of Gijón between 6 and 25 years old. Gastroenterol Hepatol. 2004;27:347–52.
Gutiérrez-Zufiaurre N, Sánchez-Hernandez J, Muñoz S, Marín R, Delgado N, Sáenz MC, et al. Seroprevalence of antibodies against Treponema pallidum, Toxoplasma gondii, rubella virus, hepatitis B and C virus, and HIV in pregnant women. Enferm Infecc Microbiol Clin. 2004;22:512–6.
Ruiz-Extremera A, López-Garrido MA, Barranco E, Quintero MD, Ocete-Hita E, de Rueda P M, et al. Activity of hepatic enzymes from week sixteen of pregnancy. Am J Obstet Gynecol. 2005;193:2010–6.
Calleja Panero JL, Llop Herrera E, Ruiz Moraga M, de la Revilla NJ, Calvo Bonacho E, Pons Renedo F, et al. Prevalence of viral hepatitis (band C) serological markers in healthy working population. Rev Esp Enferm Dig. 2013;105:249–54.
Ministry of Health, Social Services and Equality. Strategic Plan for tackling Hepatitis C in the Spanish National Health System. Madrid; 2015. http://www.msssi.gob.es/ciudadanos/enfLesiones/enfTransmisibles/docs/plan_estrategico_hepatitis_C.pdf. Accesed 11 Feb 2016.
Gower E, et al. Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol. 2014;61(Suppl 1):45–57.
Bruggmann P, et al. Historical epidemiology of hepatitis C virus (HCV) in selected countries. J Viral Hepat. 2014;21(Suppl. 1):5–33.
García-Fulgueiras A, García-Pina R, Morant C, García-Ortuzar V, Génova R, Álvarez E. Hepatitis C and hepatitis B related mortality in Spain. Eur J Gastroenterol Hepatol. 2009;21:895–901.
García-Fulgueiras A, García-Pina C, Morant N, de Larrea-Baz F, Álvarez E. Burden of disease related to hepatitis C and hepatitis B in Spain: a methodological challenge of an unfolding health problem. J Viral Hepat. 2011;18:453–60.
Ministerio de Sanidad, Servicios Sociales e Igualdad. Informe de hospitalización - CMBD – Registro de altas. Informe resumen 2013. Madrid; 2015. www.msssi.gob.es/estadEstudios/estadisticas/cmbdhome.htm. Accesed 18 Feb 2016.
Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) 2014. http://www.msssi.gob.es/estadEstudios/estadisticas/docs/CIE9MC_2014_def_accesible.pdf. Accesed 18 Nov 2015.
Esteban-Vasallo MD, Domínguez-Berjón MF, Gil de Miguel Á, Astray-Mochales J, Blanco-Ancos LM, Gil-Prieto R. Characteristics of herpes zoster-associated hospitalizations in Madrid (SPAIN) before vaccine availability. J Inf Secur. 2016;72:70–9.
Gil-Prieto R, Gonzalez-Escalada A, Alvaro-Meca A, Garcia-Garcia L, San-Martin M, González-López A, Gil-de-Miguel A. Impact of non-routine rotavirus vaccination on hospitalizations for diarrhoea and rotavirus infections in Spain. Vaccine. 2013;31:5000–4.
López-de-Andrés A, Jiménez-García R, Hernández-Barrera V, Isabel Jiménez-Trujillo M, Gil-de-Miguel A, Carrasco-Garrido P. Trends in hospitalizations among children with type 1 diabetes in Spain, 2001-2009. J Pediatr Endocrinol Metab. 2013;26:85–9.
Instituto Nacional de Estadística. Proyecciones de población. http://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176953&menu=ultiDatos&idp=1254735572981. Accessed July 2017.
Waterhouse J, Muir CS, Correa P, Powell J, editors. Cancer incidence in five continents. Lyon: IARC Scientific Publications; 1976.
Diez M, Garriga C, Pons M, Ten A, Marcos H, Gutiérrez G, et al. A low-cost, sustainable, second generation system for surveillance of people living with HIV in Spain: 10-year trends in behavioural and clinical indicators, 2002 to 2011. Euro Surveill. 2014; 19 (20): pii=20805.
Nelson PK, Mathers BM, Cowie B, Hagan H, Des Jarlais D, Horyniak D, et al. Global epidemiology of hepatitis B and hepatitis C in people who inject drugs: results of systematic reviews. Lancet. 2011;378:571–83.
Rondy M, Wiessing I, Hutchinson SJ, Mathei C, Mathis F, Mravcik V, et al. Hepatitis C prevalence in injecting drug users in Europe, 1990–2007: impact of study recruitment setting. Epidemiol Infect. 2013;141:563–72.
Martínez-Rebollar M, Mallolas J, Pérez I, González-Cordón A, Loncà M, Torres B, et al. Acute outbreak of hepatitis C in human immunodeficiency virus-infected patients. Enferm Infecc Microbiol Clin. 2015;33:3–8.
Martínez-Bauer E, Forns X, Armelles M, Planas R, Solà R, Vergara M, et al. Hospital admission is a relevant source of hepatitis C virus acquisition in Spain. J Hepatol. 2008;48:20–7.
Echevarría JM, León P, Pozo F, Avellón A. Follow-up of the prevalence of hepatitis C virus genotypes in Spain during a nine-year period (1996-2004). Enferm Infecc Microbiol Clin. 2006;24(1):20–5.
Razavi H, Waked I, Sarrazin C, Myers RP, Idilman R, Calinas F, et al. The present and future disease burden of hepatitis C virus (HCV) infection with today’s treatment paradigm. J Viral Hepat. 2014;21(Suppl. 1):34–59.
Dore GJ, Ward J, Thursz M. Hepatitis C disease burden and strategies to manage the burden. J Viral Hepat. 2014;21:1–4.
Acknowledgements
We would like to thank Dr. Iñaki Galán (National Centre of Epidemiology, Madrid, Spain) for his valuable comments and the Institute of Health Information, from the Information and Statistics Department of the Spanish Ministry of Health, Social Services and Equality, which provided the data necessary to complete this study.
Funding
Not applicable.
Availability of data and materials
The data that support the findings of this study are available from Ministry of Health, Social Services and Equality but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon responsible request and with permission of Ministry of Health, Social Services and Equality.
Author information
Authors and Affiliations
Contributions
RB and RC designed the study. RB prepared and analysed the databases. All named authors - RB, RC, PG, FV, RFC, IN, AL- contributed to the interpretation of the results. All the signatories - RB, RC, PG, FV, RFC, IN, AL- have participated in the preparation of the manuscript have given their approval to the final version, and share responsibility for the article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
None.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Boix, R., Cano, R., Gallego, P. et al. Hepatitis C hospitalizations in Spain, 2004-2013: a retrospective epidemiological study. BMC Health Serv Res 17, 461 (2017). https://doi.org/10.1186/s12913-017-2410-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-017-2410-1