Abstract
Background
Disability in older adults is associated with loss of independence, institutionalization, and death. The aim of this study was to study the association between the Timed Up and Go (TUG) test and all-cause mortality in a population-based sample of older men and women.
Methods
Our study population was home dwellers aged 65 and above, who participated in the fifth wave of the Tromsø study. This study included the TUG test and a range of lifestyle and mortality predictors. Participants were linked to the Cause of Death Registry and followed up for mortality for a maximum of 11.8 years. Cox regression was used to investigate the association between TUG and total mortality.
Results
Mean TUG score was 12.6 s, and men performed better than women. The oldest participants had poorer TUG score compared to younger participants, increasing 0.25 s per year. There was a significant association between TUG and all-cause mortality, and the association was equally strong in men and women. Across the TUG-score categories, from quickest fifth to slowest fifth, the mortality increased in a step-wise fashion. Compared to the quickest fifth, the slowest fifth had hazard ratio (HR) of 1.79 (95% confidence interval (CI) 1.33, 2.42) in a model adjusted for age and gender. For each standard deviation TUG-score the increase in HR was 1.23 (95% CI 1.14, 1.33). The association between the TUG score and mortality remained significant after adjusting for self-reported health, body mass index, smoking and education.
Conclusions
A significant association between the TUG score and mortality was observed in both men and women. Identifying older people with poor TUG may aid in identifying those at risk and thus targeted interventions may be applied.
Similar content being viewed by others
Background
Disability in older adults is associated with loss of independence, institutionalization, and death [1]. Even a small reduction in disability may translate into large healthcare savings and improvements in the physical, emotional, and social well-being of older adults [2]. Population aging is associated with an increase in the number of people who are disabled. This increase presents a challenge for society because elderly persons disabled in one or more domains of life are hospitalized more often and need more medical and long-term care [3–7], and face a higher mortality rate than nondisabled persons [8–15].
Difficulties in mobility are often the first sign of functional decline, and may indicate that a person could benefit from preventive actions [16]. Maintaining independent mobility is an important goal, especially for old women who are at a greater risk for functional decline and disability than older men [17]. Furthermore, mobility, or the ability to move about independently and safely in one’s environment, is fundamental to independent living and to the quality of life [18–20]. Walking is the fundamental mobility task for human life and is a complex neuromotor activity [21]. With advancing age, however, maintaining mobility and walking capability may be jeopardised by the increasing risk of physical and sensory impairments [22]. Medical or health conditions or advanced aging may disturb these subsystems causing slow walking, and slowing of movement with age appears to be a universal biological phenomena [23]. It is documented that persons walking slower than one meter per second are likely to be limited in energy needed for self-care, and persons walking faster than one meter per second may be expected to have the capacity to perform household activities [23]. Mobility is frequently measured through self- reports such as the ability to walk 400 m [24–27]. Moreover, longitudinal predictors of mobility decline have been documented including; increasing age [1, 28–30], number of morbidities [31], poor self-rated health [31], obesity [32], reduced leg strength [27, 33, 34], and psychosocial factors [31].
The “Timed Up and Go” (TUG) test is recommended [35] for screening frail persons and it can be carried out at home [36, 37]. The TUG test is found to mirror the physiological changes that occur with aging and physical inactivity [38] and reflects physical performance during every-day life [39]. Previous research have shown that TUG scores increase with increasing age [40]. The TUG test has been reported to yield high; interrater reliability, intrarater reliability and test- retest reliability [41].
Most studies have focused on the association between TUG score and falls [35, 42–45]. Fewer studies have investigated the predictive validity of TUG for subsequent onset of ADL disability [36, 45–47], frailty [48], fear of falling [49], hospitalization [45], decline in global health [45], and mortality [48]. Predictors of mortality in older populations are known to be somewhat different in men and women [50]. For example, Tiainen et al. [50] provided evidence that difficulties in daily activities and poor self-reported mobility are stronger predictors of mortality in men than women. To our knowledge only two community-based studies [51, 52] have investigated the relationship between TUG score and mortality, and only one of these included both genders.
Our aim was to study the association between TUG and all-cause mortality during 11.8 years follow-up in a population-based sample of older men and women aged 65 years and older at baseline, taking into account a range of lifestyle and health related factors.
Methods
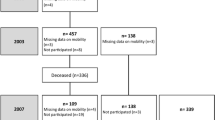
Participants were men and women in the fifth Tromsø study, phase 2 [53] in 2001–2002, aged 65 years or older at baseline (the majority being 75–79 years). The participation rate in this phase 2 study was 76%, and for our age group 1005 participated in the TUG test. Study participants were linked to the Cause of Death Registry and followed up for mortality until 01.01.2013. Mean follow-up time was 9.1 years (SD 3.2) and maximum follow-up time was 11.8 years. Reporting of data results was made in accordance to the STROBE statement checklist (see http://strobe-statement.org/index.php?id=available-checklists).
Timed up and go
TUG was measured as the time (in seconds) it takes for the study participant to rise from a chair (with armrests), walk three meters quickly but safely, turn and walk back to the chair and sit down. A walking aid was allowed if needed [54]. For each combination of gender and ages 65–69 years, 70–79 years, and 80–88 years, participants were grouped in five equally sized groups based on their TUG-score. These age and gender specific TUG quintiles were used as the main exposure in our study. In addition, standardized TUG scores (z-scores) were created to have mean of zero and a standard deviation of one, and this was done for the similar gender and age group combinations as for the quintiles.
Covariates at baseline
A priori we identified a small set of potential key confounders- that is, factors that have previously been shown to associate with both mobility and mortality. Height and weight were measured by trained personnel in The Tromsø study, and body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared (kg/m2) and grouped into five groups: < 20 kg/m2, 20–24.9 kg/m2, 25–26.9 kg/m2, 27–29.9 kg/m2, 30+ kg/m2. Smoking was self-reported in three groups as current, previous, or never-smoker. Education level was based on years of education grouped as low (7 or less years), middle (8–12 years) or high (13 or more years). Self-reported current health status was categorized as: poor, not so good, good or very good.
Statistics
Cox regression was used to investigate the association between TUG score at baseline and total mortality during follow-up. Attained age was used as time scale in the regression models, and participants who emigrated during followed up were censored at date of emigration. Analyses were run separately for men and women, as well as collapsed over genders (with the inclusion of an interaction term TUG by gender). First, analyses were adjusted for gender (age is already finely adjusted for because we use attained age as timescale). Secondly, we adjusted for BMI, self-reported health status, smoking and education. All analyses were performed on the sample with non-missing values for all the covariates (N = 864, 86% of full study sample). The proportional hazards assumption was checked on the basis of analysis of Schoenfeld residuals, and by graphical inspection of the estimated hazard function (on log-scale) on the Y-axis and analysis time on the X-axis. No violations of proportionality were observed (results not shown). Stata 13 was used for the analyses.
Results
The participants had a mean age 76.7 years (SD = 2.8, range = 65-88) and 56.4% were women (Table 2). The mean TUG score was 12.6 s (SD 6.5), with men performing better than women; 11.7 s (SD 5.6) versus 13.2 s (SD 7.1) (test for difference between genders: p < 0.01) (Table 1, Table 2).
The age adjusted difference in baseline registration of the TUG score between those who died during follow-up and those who were still alive was 1.5 s (p < 0.001). The oldest participants had worse score on TUG compared to younger participants, increasing 0.25 s per year (p = 0.001), with similar TUG score decrease with age across genders.
TUG scores were similar across most of the covariates, except for self-reported health (p-value <0.01) and BMI (p-value: 0.09) (Table 2). Those reporting poor health had a TUG score of 16.5 s and those reporting very good health scored 9.5 s on TUG. Those with BMI at 30 kg/m2 or above had the poorest TUG-performance, compared with the other BMI groups.
During follow-up, 506 of the 1005 participants died (50.4%). There was a significant association between TUG-score and mortality; (Table 3). This was the case in both men and women, and the interaction terms gender by TUG-score fifths were non-significant, in both the basically adjusted model and in the fully adjusted model. Across the TUG-score categories, from quickest fifth to slowest fifth, there was a tendency for increased mortality in a step-wise fashion, and especially those in the two poorest TUG performance fifths had high mortality rate; Compared to the quickest fifth, the slowest fifth had hazard ratio (HR) 1.79 (95% confidence interval 1.33, 2.42) in a model adjusted for age and gender. For each SD higher TUG-score the HR was 1.23 (95% CI 1.14, 1.33). The association was robust to further adjustment for BMI, self-reported health status, smoking and education. In such a model the HR for the quickest fifth compared to the slowest fifth was 1.63 (95% CI 1.20, 2.22), and 1.20 (95% CI 1.10, 1.30) per 1 SD increase in TUG-score (Table 3).
We performed a likelihood ratio test, testing the saturated model containing both TUG and self-reported health against a model without TUG. The saturated model had significantly better fit than the model without TUG (p = 0.028). Similarly, testing the saturated model against a model leaving out self-reported health (and keeping TUG in) provided even stronger p-value in favor for the saturated model. Hence, self-reported health is a stronger predictor than TUG regarding mortality, but TUG adds predictive value in a model already containing self-reported health. Thus, the association between TUG and mortality is not entirely attenuated by self-reported health.
Discussion
In this population based study of home dwellers aged 65 years and older followed up over a period of maximum 11.8 years, we found robust evidence of an association between poor TUG score and increased all-cause mortality, which was equally strong in men and women. This association was robust to adjustment for self-reported health, BMI, smoking and education.
To the best of our knowledge, this is the first population based study to examine the association between TUG score and mortality in both genders for subjects aged 65 years or older living at home. Our results of increased mortality for those with poor TUG performance correspond well with results from other similar studies [51, 52, 55–58]. However, some of these studies did not include both genders [51, 52]. The results of De Buyser et al. [51] showed an association of TUG with all-cause mortality in men aged 71–88 years at baseline with 15 years of follow-up. Idland et al. [52] concluded in a study of 300 community-dwelling women aged 75 and older that TUG predicted mortality during 13.5 years-follow up. Furthermore, according to Tice et al. [58] poor results on TUG were strongly associated with increased mortality during 9 years of follow-up in a study of middle-aged community-dwelling postmenopausal women with mean age 68 years.
Our results showed an association of TUG with all-cause mortality in both home-dwelling males and females, not referring to specific disease diagnosis. An example of a study focusing on the association with TUG and mortality in a diagnose specific population is the study of Roshanravan et al. [56] with a sample of 385 participants (mean age 61 years, SD = 13 years) with chronic kidney disease. Their study showed that each one-second longer TUG score was associated with 8% greater risk of death during the following three years, after adjustment for demographics and comorbidity [56]. Robinson et al. [59] found in a prospective cohort study of patients 65 years and older undergoing colorectal and cardiac operation that a preoperative TUG score slower than 15 s was associated with significant higher 1-year mortality. The study of Hoside et al. [56] showed that TUG-score of elderly patients over 80 years of age was associated with total and cardiovascular mortality. Furthermore, TUG was found to predict the risk of death within 6 months in onco-geriatric patients older than 70 years of age receiving chemotherapy [57]. A slower TUG predicts health decline and cognitive decline in community–dwelling older adults [45, 60].
The reasons why TUG is predictive of mortality might reflect underlying malaise as well as chronic illness. Despite, the TUG test has been proposed as a single measure to identify older adults who are at high risk for adverse health outcomes [61]. In older adults, the ability of the TUG test to capture comorbidity burden highlights the importance of the multiple interactions among several different body systems (e.g. nervous, cardiopulmonary, and musculoskeletal systems) involved in coordinating mobility and balance. For example, slower gait speed has been associated with subclinical cerebrovascular disease, even among apparently high functioning older adults [62–65]. Walking speed may capture both underlying age-related biological changes, as well as diagnosed and undiagnosed diseases [66]. Furthermore, it may reflect an individual’s vitality because walking requires energy and puts demand on body functions and structures [66]. Above-average physical performance probably reflects a resilience that enables a person to respond adequately to future stressors [67]. In fact walking speed is an important component in TUG [68].
As in other studies where data were analyzed by gender we found that men had significantly better TUG score than women [69–71], and that TUG was positively associated with age [70, 72]. However, we found no gender- specific association between TUG and mortality in our study. Hence, TUG seems to predict mortality equally well in men and women.
Non-participants tend to have higher mortality than participants in population-based studies [73], and if this was the case in our study and non-participants also were more frail than the participants, this may have underestimated the true relationship between TUG and mortality. Hence, our estimate might be a conservative one. Our study had an age range from 65 and above, but the majority were in the age group 75–79 (69%), and age specific results are therefore most robust in this age group. All observational studies are hampered by residual confounding to various degree. We included key health related confounders (self-reported health, smoking, education) which only to a limited degree attenuated the TUG-mortality association. However, mild cognitive impairment and early stage dementia may bias results since there is strong evidence of a consistent association between cognitive function and different aspects of physical fitness related to independent living such as gait speed, mobility, balance and muscle strength [74, 75]. The strength of the present study includes long follow-up time, objective measures of physical capability and the inclusion of key covariates. Death certificates were obtained from the official Cause of Death Register, which covers the whole population, and is of high quality.
Conclusions
The present study may add new knowledge to the limited research on gender specific analyses on the association between mobility and mortality in a general population, by showing that TUG score is an equally important predictor for survival in both men and women. Identifying older people with poor TUG score may aid in identifying those at risk and thus targeted interventions may be applied.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- SD:
-
Standard deviation
- TUG:
-
Timed up and go
References
Guralnik JM, Fried LP, Salive ME. Disability as a public health outcome in the aging population. Annu Rev Public Health. 1996;17(1):25–46.
Rula EY, Pope JE, Hoffman JC. Potential Medicare savings through prevention and risk reduction. Popul Health Manag. 2011;14(S1):35–44.
Allen SM, Ciambrone D. Community care for people with disability: blurring boundaries between formal and informal caregivers. Qual Health Res. 2003;13(2):207–26.
Anderson G, Knickman JR. Changing the chronic care system to meet people’s needs. Health Aff. 2001;20(6):146–60.
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59(3):255–63.
Van Nostrand JF, Miller B, Furner SE. Selected issues in long-term care: profile of cognitive disability of nursing home residents and the use of informal and formal care by elderly in the community. Vital Health Stat 3. 1993;27:143–85.
Wolinsky FD, Culler SD, Callahan CM, Johnson RJ. Hospital resource consumption among older adults: a prospective analysis of episodes, length of stay, and charges over a seven-year period. J Gerontol. 1994;49(5):240–52.
Bernard SL, Kincade JE, Konrad TR, Arcury TA, Rabiner DJ, Woomert A, et al. Predicting mortality from community surveys of older adults: the importance of self-rated functional ability. J Gerontol Ser B Psychol Sci Soc Sci. 1997;52(3):155–63.
Fried LP, Kronmal Richard A, Newman Anne B, Bild Diane E, Mittelmark Maurice B, Polak Joseph F, et al. Risk factors for 5-year mortality in older adults. J Am Med Assoc. 1998;279(8):585–92.
Kattainen A, Reunanen A, Koskinen S, Martelin T, Knekt P, Aromaa A. Disability predicted mortality in men but not women with coronary heart disease. J Clin Epidemiol. 2004;57(5):513–21.
Lamarca R, Ferrer M, Andersen PK, Liestol K, Keiding N, Alonso J. A changing relationship between disability and survival in the elderly population: differences by age. J Clin Epidemiol. 2003;56(12):1192–201.
Pudaric S, Sundquist J, Johansson S-E. Country of birth, instrumental activities of daily living, self-rated health and mortality: a Swedish population-based survey of people aged 55–74. Soc Sci Med. 2003;56(12):2493–503.
Scott WK, Macera CA, Cornman CB, Sharpe PA. Functional health status as a predictor of mortality in men and women over 65. J Clin Epidemiol. 1997;50(3):291–6.
Tager IB, Haight TJ, Hollenberg M, Satariano WA. Physical functioning and mortality in older women: an assessment of energy costs and level of difficulty. J Clin Epidemiol. 2003;56(8):807–13.
van den Brink CL, Tijhuis M, van den Bos GA, Giampaoli S, Nissinen A, Kromhout D. The contribution of self-rated health and depressive symptoms to disability severity as a predictor of 10-year mortality in European elderly men. Am J Public Health. 2005;95(11):2029–34.
Mänty M, Heinonen A, Leinonen R, Törmäkangas T, Sakari-Rantala R, Hirvensalo M, et al. Construct and predictive validity of a self-reported measure of preclinical mobility limitation. Arch Phys Med Rehabil. 2007;88(9):1108–13.
Gill TM, Gahbauer EA, Murphy TE, Han L, Allore HG. Risk factors and precipitants of long-term disability in community mobility: a cohort study of older persons. Ann Intern Med. 2012;156(2):131–40.
Gorgon E, Said C, Galea M. Mobility on discharge from an aged care unit. Physiother Res Int. 2007;12(2):72–81.
Ruuskanen J, Ruoppila I. Physical activity and psychological well-being among people aged 65 to 84 years. Age Ageing. 1995;24(4):292–6.
Tacken M. Mobility of the elderly in time and space in the Netherlands: an analysis of the Dutch National Travel Survey. Transportation. 1998;25(4):379–93.
Ferrucci L, Bandinell S, Benvenuti E, Di Iorio A, Macchi C, Harris T, et al. Subsystems contributing to the decline in ability to walk: bridging the gap between epidemiology and geriatric practice in the InCHIANTI study. Am Geriatr Soc. 2000;48(12):1618–25.
Cooper KM, Bilbrew D, Dubbert PM, Kerr K, Kirchner K. Health barriers to walking for exercise in elderly primary care. Geriatr Nurs. 2001;22(5):258–62.
Studenski S. Bradypedia: is gait speed ready for clinical use? J Nutr Health Aging. 2009;13(10):878–80.
Buchner DM. One lap around the track: the standard for mobility disability? J Gerontol A Biol Sci Med Sci. 2008;63(6):586–7.
Chaudhry SI, McAvay G, Ning Y, Allore HG, Newman AB, Gill TM. Geriatric impairments and disability: the cardiovascular health study. J Am Geriatr Soc. 2010;58(9):1686–92.
Hardy SE, Kang Y, Studenski SA, Degenholtz HB. Ability to walk 1/4 mile predicts subsequent disability, mortality, and health care costs. J Gen Intern Med. 2011;26(2):130–5.
Wang C-Y, Yeh C-J, Hu M-H. Mobility-related performance tests to predict mobility disability at 2-year follow-up in community-dwelling older adults. Arch Gerontol Geriatr. 2011;52(1):1–4.
Guralnik JM, Branch LG, Cummings SR, Curb JD. Physical performance measures in aging research. J Gerontol. 1989;44(5):141–6.
Guralnik JM, LaCroix AZ, Abbott RD, Berkman LF, Satterfield S, Evans DA, et al. Maintaining mobility in late life. I. Demographic characteristics and chronic conditions. Am J Epidemiol. 1993;137(8):845–57.
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):85–94.
Ayis S, Gooberman-Hill R, Bowling A, Ebrahim S. Predicting catastrophic decline in mobility among older people. Age Ageing. 2006;35(4):382–7.
Clark DO, Stump TE, Hui SL, Wolinsky FD. Predictors of mobility and basic ADL difficulty among adults aged 70 years and older. J Aging Health. 1998;10(4):422–40.
Buchman AS, Wilson RS, Boyle PA, Tang Y, Fleischman DA, Bennett DA. Physical activity and leg strength predict decline in mobility performance in older persons. J Am Geriatr Soc. 2007;55(10):1618–23.
Visser M, Goodpaster BH, Kritchevsky SB, Newman AB, Nevitt M, Rubin SM, et al. Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol A Biol Sci Med Sci. 2005;60(3):324–33.
American Geriatrics Society, Geriatrics Society, Orthopaedic Surgeons Panel On Falls Prevention. Guideline for the prevention of falls in older persons. J Am Geriatr Soc. 2001;49(5):664–72. http://onlinelibrary.wiley.com/doi/10.1046/j.1532-5415.2001.49115.x/abstract;jsessionid=C24BBE3FF23D4B4887313886D8ADE27D.f01t04?systemMessage=Wiley+Online+Library+will+be+unavailable+on+Saturday+17th+December+2016+at+09%3A00+GMT%2F+04%3A00+EST%2F+17%3A00+SGT+for+4hrs+due+to+essential+maintenance.
Lin MR, Hwang HF, Hu MH, Wu HDI, Wang YW, Huang FC. Psychometric comparisons of the timed Up and Go, one‐leg stand, functional reach, and tinetti balance measures in community‐dwelling older people. J Am Geriatr Soc. 2004;52(8):1343–8.
Eekhof JAH, De Bock GH, Schaapveld K, Springer MP. Short report: functional mobility assessment at home. Timed up and go test using three different chairs. Can Fam Physician. 2001;47(6):1205–7.
Samson MM, Meeuwsen I, Crowe A, Dessens J, Duursma SA, Verhaar H. Relationships between physical performance measures, age, height and body weight in healthy adults. Age Ageing. 2000;29(3):235–42.
Bischoff HA, Stähelin HB, Monsch AU, Iversen MD, Weyh A, von Dechend M, et al. Identifying a cut‐off point for normal mobility: a comparison of the timed ‘up and go’test in community‐dwelling and institutionalised elderly women. Age Ageing. 2003;32(3):315–20.
Bohannon RW. Reference values for the timed Up and Go test: a descriptive meta‐analysis. J Geriatr Phys Ther. 2006;29(2):64–8.
Rydwik E, Bergland A, Forsén L, Frändin K. Psychometric properties of timed Up and Go in elderly people: a systematic review. Phys Occup Ther Geriatr. 2011;29(2):102–25.
Barry E, Galvin R, Keogh C, Horgan F, Fahey T. Is the timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: a systematic review and meta-analysis. BMC Geriatr. 2014;14(1):14.
Schoene D, Wu SMS, Mikolaizak AS, Menant JC, Smith ST, Delbaere K, et al. Discriminative ability and predictive validity of the timed Up and Go test in identifying older people who fall: systematic review and meta‐analysis. J Am Geriatr Soc. 2013;61(2):202–8.
Thrane G, Joakimsen RM, Thornquist E. The association between timed up and go test and history of falls: the Tromsø study. BMC Geriatr. 2007;7(1):1.
Viccaro LJ, Perera S, Studenski SA. Is timed up and go better than gait speed in predicting health, function, and falls in older adults? J Am Geriatr Soc. 2011;59(5):887–92.
Shimada H, Sawyer P, Harada K, Kaneya S, Nihei K, Asakawa Y, et al. Predictive validity of the classification schema for functional mobility tests in instrumental activities of daily living decline among older adults. Arch Phys Med Rehabil. 2010;91(2):241–6.
Wennie Huang WN, Perera S, VanSwearingen J, Studenski S. Performance measures predict onset of activity of daily living difficulty in community‐dwelling older adults. J Am Geriatr Soc. 2010;58(5):844–52.
Davis DH, Rockwood MR, Mitnitski AB, Rockwood K. Impairments in mobility and balance in relation to frailty. Arch Gerontol Geriatr. 2011;53(1):79–83.
Austin N, Devine A, Dick I, Prince R, Bruce D. Fear of falling in older women: a longitudinal study of incidence, persistence, and predictors. J Am Geriatr Soc. 2007;55(10):1598–603.
Tiainen K, Luukkaala T, Hervonen A, Jylhä M. Predictors of mortality in men and women aged 90 and older: a nine-year follow-up study in the vitality 90+ study. Age Ageing. 2013;42(4):468–75.
De Buyser SL, Petrovic M, Taes YE, Toye KR, Kaufman JM, Goemaere S. Physical function measurements predict mortality in ambulatory older men. Eur J Clin Investig. 2013;43(4):379–86.
Idland G, Engedal K, Bergland A. Physical performance and 13.5-year mortality in elderly women. Scand J Public Health. 2013;41(1):102–8.
Jacobsen BK, Eggen AE, Mathiesen EB, Wilsgaard T, Njølstad I. Cohort profile: the Tromsø study. Int J Epidemiol. 2012;41(4):961–7.
Podsiadlo D, Richardson S. The timed“Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8.
Hoshide S, Ishikawa J, Eguchi K, Oowada T, Shimada K, Kario K. Cognitive dysfunction and physical disability are associated with mortality in extremely elderly patients. Hypertens Res. 2008;31(7):1331–8.
Roshanravan B, Robinson-Cohen C, Patel KV, Ayers E, Littman AJ, de Boer IH, et al. Association between physical performance and all-cause mortality in CKD. J Am Soc Nephrol. 2013;24(5):822–30.
Soubeyran P, Fonck M, Blanc-Bisson C, Blanc J-F, Ceccaldi J, Mertens C, et al. Predictors of early death risk in older patients treated with first-line chemotherapy for cancer. J Clin Oncol. 2012;30(15):1829–34.
Tice JA, Kanaya A, Hue T, Rubin S, Buist DS, LaCroix A, et al. Risk factors for mortality in middle-aged women. Arch Intern Med. 2006;166(22):2469–77.
Robinson TN, Wu DS, Sauaia A, Dunn CL, Stevens-Lapsley JE, Moss M, et al. Slower walking speed forecasts increased postoperative morbidity and 1-year mortality across surgical specialties. Slower walking speed forecasts increased postoperative morbidity and 1-year mortality across surgical specialties. Ann Surg. 2013;258(4):582–8.
Donoghue OA, Horgan NF, Savva GM, Cronin H, O’Regan C, Kenny RA. Association between timed Up‐and‐Go and memory, executive function, and processing speed. J Am Geriatr Soc. 2012;60(9):1681–6.
Savva GM, Donoghue OA, Horgan F, O’Regan C, Cronin H, Kenny RA. Using timed up-and-go to identify frail members of the older population. J Gerontol A Biol Sci Med Sci. 2013;68(4):441–6.
Rosano C, Aizenstein H, Brach J, Longenberger A, Studenski S, Newman AB. Special article gait measures indicate underlying focal gray matter atrophy in the brain of older adults. J Gerontol A Biol Sci Med Sci. 2008;63(12):1380–8.
Rosano C, Brach J, Longstreth JW, Newman AB. Quantitative measures of gait characteristics indicate prevalence of underlying subclinical structural brain abnormalities in high-functioning older adults. Neuroepidemiology. 2005;26(1):52–60.
Rosano C, Brach J, Studenski S, Longstreth Jr W, Newman AB. Gait variability is associated with subclinical brain vascular abnormalities in high-functioning older adults. Neuroepidemiology. 2007;29(3–4):193–200.
Stevens LA, Coresh J, Schmid CH, Feldman HI, Froissart M, Kusek J, et al. Estimating GFR using serum cystatin C alone and in combination with serum creatinine: a pooled analysis of 3,418 individuals with CKD. Am J Kidney Dis. 2008;51(3):395–406.
Van Kan GA, Rolland Y, Andrieu S, Bauer J, Beauchet O, Bonnefoy M, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009;13(10):881–9.
Blain H, Carriere I, Sourial N, Berard C, Favier F, Colvez A, et al. Balance and walking speed predict subsequent 8-year mortality independently of current and intermediate events in well-functioning women aged 75 years and older. J Nutr Health Aging. 2010;14(7):595–600.
Ingemarsson AH, Frandin K, Mellstrom D, Moller M. Walking ability and activity level after hip fracture in the elderly–a follow-up. J Rehabil Med. 2003;35(2):76–83.
Pondal M, del Ser T. Normative data and determinants for the timed “Up and Go” test in a population‐based sample of elderly individuals without gait disturbances. J Geriatr Phys Ther. 2008;31(2):57–63.
Steffen TM, Hacker TA, Mollinger L. Age-and gender-related test performance in community-dwelling elderly people: six-minute walk test, berg balance scale, timed Up & Go test, and gait speeds. Phys Ther. 2002;82(2):128–37.
Vereeck L, Wuyts F, Truijen S, Van de Heyning P. Clinical assessment of balance: normative data, and gender and age effects. Int J Audiol. 2008;47(2):67–75.
Bohannon RW, Bubela DJ, Magasi SR, Gershon RC. Relative reliability of three objective tests of limb muscle strength. Isokinetics Exerc Sci. 2011;19(2): 10.3233/IES-2011-0400.
Langhammer A, Krokstad S, Romundstad P, Heggland J, Holmen J. The HUNT study: participation is associated with survival and depends on socioeconomic status, diseases and symptoms. BMC Med Res Methodol. 2012;12(1):143.
Hesseberg K, Bergland A, Rydwik E, Brovold T. Physical fitness in older people recently diagnosed with cognitive impairment compared to older people recently discharged from hospital. Dement Geriatr Cogn Dis Extra. 2016;6(3):396–406.
Hesseberg K, Bentzen H, Ranhoff AH, Engedal K, Bergland A. P physical fitness in older people with mild cognitive impairment and dementia. J Aging Phys Act. 2016;24(1):92–100.
Acknowledgements
We are greatly thankful to the Tromsø Study for providing data and to the Tromsø Study participants for their participation and patience.
Funding
The study had no external funding.
Availability of data and materials
The data supporting the conclusions of this article are available in https://uit.no/ansatte/organisasjon/artikkel?p_menu=42374&p_lang=2&p_document_id=80172&p_dimension_id=88111.
Authors’ contributions
AB has made contributions to conception and design and interpretation of data as well as being the main responsible in drafting the initial manuscript and revising it critically for important intellectual content. BHS has contributed with analysis and interpretation of data and has also been involved in drafting the manuscript and revising it critically for important intellectual content. NE and LJ have been involved in conception and design and interpretation of data, and revising the manuscript critically for important intellectual content. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The current study was approved by the Regional Committee for Medical Ethics and the Norwegian Data Inspectorate approved the study (registration number 07/00886). Written informed consent was obtained from all participants in the Tromsø Study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bergland, A., Jørgensen, L., Emaus, N. et al. Mobility as a predictor of all-cause mortality in older men and women: 11.8 year follow-up in the Tromsø study. BMC Health Serv Res 17, 22 (2017). https://doi.org/10.1186/s12913-016-1950-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-016-1950-0