Abstract
Background
Unsafe health practices are one of the leading causes of disability and even death. Competent nurses are crucial to ensure safe and high-quality healthcare services. The patient safety culture is concerned with internalizing safety beliefs, values, and attitudes, translating them into healthcare practices, and committing to maintaining an error-free health environment. A high level of competence ensures the achievement and compliance with the safety culture goal. This systematic review aims to identify the relationship between the level of nursing competence and the safety culture score and perception among nurses at their workplace.
Methods
Four international online databases were searched to find relevant studies published between 2018 and 2022. Peer-reviewed articles using quantitative methods, targeting nursing staff, and written in English were included. After reviewing 117 identified studies, 16 full-text studies were included. The PRISMA 2020 checklist for systematic reviews was used.
Results
Evaluation of the studies indicates safety culture, competency, and perception were assessed using various instruments. Safety culture was generally perceived as positive. No unique and standard tool has been developed to investigate the effect of safety competency on the perception of the safety culture in a standardized way.
Conclusions
Existing research provides evidence of a positive correlation between nursing competence and patient safety score. Future research is recommended to investigate ways to measure the effect of nursing competency level on safety culture in healthcare institutions.
Similar content being viewed by others
Background
Unsafe health practices are highly regarded to cause disability and death. It is estimated that the chance that unsafe practice can cause harm for the patient is 1 in 300 chance [1]. Nearly 400,000 deaths occur annually in the United States due to several reversible adverse events, such as medication error, infection transmission, and fall events [2]. In addition, poor quality care can cause death and a global health burden [3]. Patient safety is a health care discipline that evolved as a result of the increasing sophistication of health care systems and the increasing in adverse outcomes in health-care facilities. Its goal is to avoid and decrease risks, mistakes, and harm to patients while providing health care. Therefore, reliable, safe, equitable, effective, and highly standardized patient-centered care has become the ultimate goal of all health care institutions worldwide [4]. Besides that, patient safety culture focuses on organizational culture issues related to patient safety, patient safety culture is concerned with internalizing safety beliefs, values, and attitudes, translating them into health care practices and commitment to maintaining an error-free health setting and emphasizing reporting culture [5].
Competent nurses are key contributors to maintaining safe and effective health care services by integrating knowledge, skills, and attitudes that enable them to adapt to dynamic health environments [6]. Nurses are often the primary point of contact for patients and are responsible for ensuring that their needs are met. By providing patient-centered care, nurses can help create a culture that prioritizes patient safety. In addition, they can act as advocates for patient safety, promoting a culture of safety within the organization and encouraging others to do the same. Nurses should be given the power to make decisions about patient care and safety, as well as to report any harmful conditions or concerns. They can indeed act as role models for other healthcare professionals, emphasizing the importance of patient safety and providing a good example for others to follow.
Patient safety competencies are a core competency in the continuum of professional development activities that protect patients from unnecessary risks and hazards [7]. A high level of competence promotes the achievement and compliance with the patient safety goal.
Several studies found that patient safety culture and nurse safety competency are affected by many factors. For example, workplace regulations and climate, nursing fatigue, satisfaction, stress, demographics, type of health institution type, teamwork and learning opportunity, specialty, degree of bedside involvement, and job description are all factors that affect safety culture [5, 8,9,10,11].
Any improvement strategies to modulate these factors are unnegotiable. However, a better understanding of nurse competence and patient safety culture is essential to improve safe practice and professional development and minimize adverse events [12]. Therefore, this systematic review aimed to evaluate the literature concerning the relationship between self-reported competencies and the perception of patient safety among nurses in their workplace. In addition, to understand how related studies evaluated nurses’ core competencies and safety culture.
Methods
Study design
The present systematic review was designed and conducted from April 1, 2022, and April 11, 2022, by the electronic search from January 1, 2018, through May 1, 2022. This date period was chosen after agreement between the author to find the (five years) recent evidence regarding the respected review topic. The current systematic review was framed by SPIDER [13] with nurses as the Sample (S); clinical competence as the Phenomenon of Interest (PI); Design (D) as quantitative or mixed-methods studies; Evaluation (E) as covering assessments of patient safety culture; and Research Type (R) as referring to all types of studies with the exception of case studies and review articles. The protocol was performed based on the guidelines of the Preferred Reporting Items for Systematic Review and Meta-Analyses Protocol (PRISMA-P) [14].
Search strategy and data sources
Four online databases including MEDLINE (via PubMed), CINHAL (via EBSCOhost), Scopus (via Elsevier), and Embase were searched for published studies that describing the relationship between nurse competencies and patient safety culture. Search terms were developed based on experience and keywords from similar research. The search was structured using Boolean operators (AND, OR) and consisted of MeSH terms and free terms related to nursing, patient safety, competency, and safety culture. The term ‘OR’ was used between keywords or comparable MeSH phrases; meanwhile, the Boolean operator ‘AND’ was used to connect phrases or keywords with different meanings to refine the search (see Appendix A). Relevant studies were identified by two reviewers (R.A. and L.T.) independently, and search algorithm varied according to the specifications of each database. To identify the additional relevant studies being lost in the database search, we checked the references of the selected publications.
Inclusion and exclusion criteria
In this review, studies were included if they are using the quantitative approach mainly; targeting nursing staff; published in English language, and full text available. The exclusion criteria were studies in the form of letters, editorials, essays, case studies, comments or narrative, systematic reviews, and conference abstracts; studies focus on nursing students only; and studies of pre-hospital and ambulatory care.
Study selection and quality assessment
After preliminary selection of studies by the first reviewer (R.A) and their verification by the last reviewer (L.T.) the duplicated studies were excluded. Two reviewers (R.A. and L.T.) independently screened the titles, abstracts and full text of the studies.
The Mixed Methods Appraisal Tool (MMAT) [15] was used to evaluate the quality of the studies included in this review. With the MMAT, two basic screening questions must be asked first to determine whether or not the quality appraisal for a specific study will be continued. The first question is whether the related qualitative, quantitative, or mixed-methods study has clear research questions or objectives. The second question is whether the method of data collection addresses the research questions or objectives. When these initial screening questions are answered positively, qualitative (QUAL) or quantitative (QUAN) studies can be rated as follows: ‘*’ (25%) for one met criterion, ‘**’ (50%) for two, ‘***’ (75%) for three, or ‘****’ (100%) for the highest quality study. Studies with a rating of ** or higher were considered to be of acceptable quality for this review and were included for further analysis.
Data extraction
Data extraction table included: author(s) and publication year, country, design of study, method of data collection, quality assessment. Measurement Tools for Safety Culture and Nursing Competency and main findings focusing on Patient Safety Competency and the Patient Safety Culture. In this stage two authors (R.Z. and L.T.) independently extracted data from the included studies. In case of disagreement between two reviewers (R.Z. and L.T.), a third reviewer (N.S) was involved to make a final decision.
Data synthesis
An iterative narrative synthesis technique was used for data analysis [16] to identify key themes from every study that would adequately and accurately reflect the findings about clinical nurse competence and patient safety culture. The narrative synthesis was divided into four stages: (1) identifying a frame of how findings from related studies work, why and for whom; (2) synthesizing themes through an iterative process of comparing and examining findings from the included studies; (3) trying to explore themes’ relationships; and (4) evaluating the synthesis’s robustness.
Results
Results of the search strategy
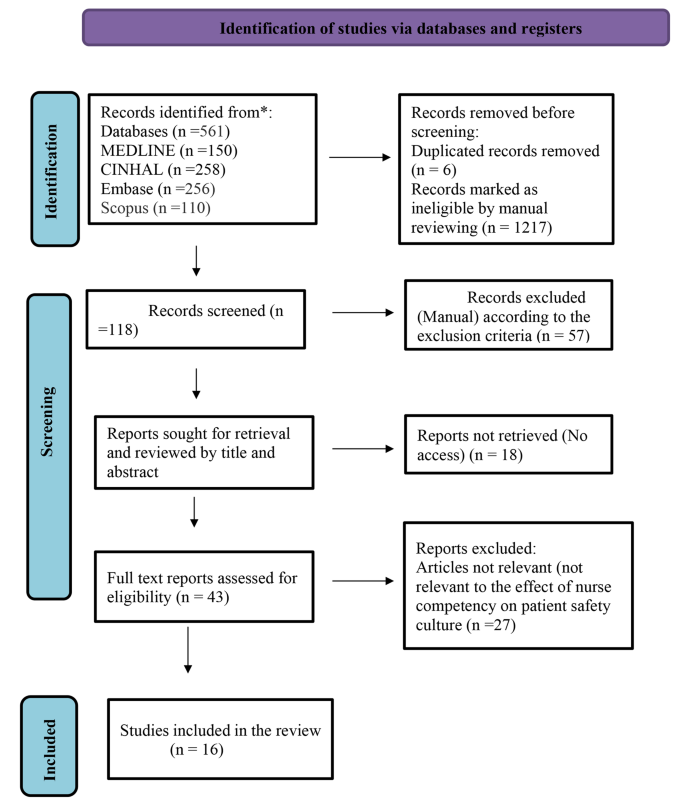
Through the flow of PRISMA-P, the search process found 1341 potentially relevant studies; initial screening revealed that 6 records were duplicated. After excluding the irrelevant studies by title and abstract review (1217) and applying exclusion criteria (57), reports not retrieved related to access issues (n = 18). Full text screening showed that 27 were not relevant. Finally, 16 studies remained and were included in the analysis (Fig. 1).
The design of the reviewed studies
Of the 16 qualifying studies, 14 were cross-sectional descriptive studies, one applied a quasi-experimental, pretest-posttest design [17], and one study used a mixed method approach [18]. Three out of the sixteen studies were conducted in South Korea [19,20,21], Canada [19] Three studies originated from Saudi Arabia [9, 22, 23]. Two studies from Iran [24, 25]. In addition, a study was conducted in each Australia [26], Belgium and Palestine [27], Brazil [28], Jordan [29], Spain [18], England [17], and China [11]. The aforementioned research studies were published from 2019 to 2022 in different journals. Summary of the characteristics of included studies are depicted in Table 1.
The sampling technique
Given the sampling technique, eight articles used the convenience sampling technique [9, 11, 19, 22, 23, 25, 26, 30]. The highest sample size was 2,836 participants in the study by Najjar et al. [27], while the least was 56 participants in [28] study.
Methodological quality of included studies
The assessment of the methodological quality of the included studies is presented in Table 2. After quality assessment, nine studies graded as ‘****’ (100%) and seven studies as ‘***’ (75%) quality using MMAT. Research conducted or published during the COVID-19 outbreak period [9, 11, 18,19,20,21,22,23,24,25,26, 28, 29] received additional review to ensure it met rationale for inclusion and standards for quality, to ensure rigor in response to the substandard work proliferating during this period [31].
Measurement tools for Safety Culture and nursing competency
The construct concepts of patient safety culture, safety climate, and patient safety competency were operationally measured using various tools or instruments throughout the sixteen studies. Nursing safety competency was measured using the Patient Safety Competency Self-Evaluation Tool, the Health Professional Education in Patient Safety Survey (H-PEPSS) [21], and the Nurses’ Attitudes and Skills Safety scale, the latest version of NASUS [23]. Furthermore, AS Alshehry [22] used the Health Professional Education in Patient Safety Survey (H-PEPSS) to assess safety competency. Halabi et al. [9] used the short version of Nurse Professional Competence (NPC).The self-reported Patient Safety Competency Nurse Evaluation Scale (PSCNES) was used by Yan et al. [11].
Three studies applied the Hospital Survey on Patient Safety Culture (HSOPSC) developed by the Agency for Healthcare Research and Quality to measure safety culture [21, 27, 32]. The safety climate was measured using the Safety Attitudes Questionnaire (SAQ) and the Safety Climate Survey (SCS); [26, 28, 29] (Table 2).
The patient safety culture
Patient safety culture was mentioned in the title of six studies [21, 23, 27, 28, 32, 33]. There was considerable variation of how this concept was perceived among nurses for example, LM Lousada, FC da Silva Dutra, BV da Silva, NLL de Oliveira, IB Bastos, PF de Vasconcelos and R de Carvalho [28] in his study found that professionals working in home care services perceived higher scores related to safety culture compared with those working in primary care services. The accredited primary center in Jordan had an average positive response rate in some safety cultures ranging from 58.54 to 75.63% [33], A total of 32 Iranian teaching hospitals out of 150 reported poor patient safety culture [32]. On the other hand, and with regard to the safety climate, the study by CJ Connell, S Cooper and R Endacott [26] revealed that novice-competent nurses in Australian emergency departments rated the safety climate higher than expert nurses in all domains except stress recognition.
Patient safety competency
Six studies examined patient safety competency and several studies connected safety competencies with the domains of safety culture. For example, L Yan, L Yao, Y Li and H Chen [11] assessed the safety competence scores of Chinese nurses with associate degree and they scored moderate level. A Habibi Soola, M Ajri-Khameslou, A Mirzaei and Z Bahari [25] found a positive correlation between safety competence and the dimension of team work, psychological safety, leadership, communication, mutual support, situation monitoring, and team structure. JH Han and YS Roh [20] found that the night shift among emergency nurses in Korean hospitals negatively affected safety competence and was significantly and positively correlated with the number of years of experience in the emergency department and number of reported adverse events by others.
In a medical city in Saudi Arabia, AS Alshehry [22] studied the correlation between the conflict between nurses and the patient, and safety competencies. The study revealed that nurses were highly competent in effective communication, but they had the lowest competency in ‘working in teams with other health professionals.’ Nurses perceived ‘mistrust of motivations’ and “contradictory communication” got the poorer self-reported safety competency.
Discussion
The purpose of this study was to provide a systematic review of the literature investigating the relationship between nursing competencies and perception of patient safety among nurses in their workplace. In this systematic review, and after a thorough analysis of the entire manuscript of the retrieved articles, we selected and discussed sixteen articles based on their conformity with the inclusion criteria.
Nurse’ competence refers to the knowledge, skills, and abilities that nurses possess to provide safe and effective care to patients in many fields such as clinical, safety, communication, and leadership. This can include things like knowledge of clinical guidelines, critical thinking skills, and the ability to identify and respond to changes in a patient’s condition, how to manage conflict and communicate with patients and other health care team. A positive patient safety culture is one in which all members of the healthcare team are committed to providing safe care and are empowered to identify and report potential hazards. Research has shown that, specifically, safety nurse competence is positively associated with a positive patient safety culture [34]. Nurses who are competent in their practice are more likely to be engaged in the safety culture of their organization and more likely to identify and report safety concerns [11]. Additionally, nurses who possess the knowledge, skills and abilities required to provide safe care are less likely to make errors which can lead to adverse patient outcomes [35]. Overall, clinical nurse competence is a critical component of a positive patient safety culture, as it helps ensure that nurses are able to provide safe and effective care to patients and promotes engagement and active participation in the safety culture of the organization.
None of the reviewed articles explicitly explored the relationship between clinical or professional nursing competencies and the safety culture dimensions and how they affect each other. Furthermore, studies identified no specific comprehensive tool with high reliability and validity and mostly recommend assessing the relationship between nursing safety competency and the dimensions of safety culture. Rather, the included articles examined patient safety culture, health care safety climate, and other nursing competencies that influenced or affect safety climate independently. Most of the retrieved studies investigated the very specific competencies for nurses which were safety competency and the level of this competency varied among different clinical setting or nationality and range between poor and moderate level and this similar to SM Cho and J Choi [36] in their study investigated relationship between the three parts of safety competency and domains of patient safety culture among 343 registered nurses in an educational hospital in, South Korea and found that the safety competency was highly correlated with teamwork within units. Teamwork within and across units, supervisor or manager expectations, and each of the three patient safety competencies were strongly associated to attitudes, while teamwork within units and learning were significantly connected to skills. Knowledge was only significantly correlated with organizational learning.
The concentration on assessing and improving Safety competency for nurses instead of more general clinical nurse competence may due to that many health care institutions tend to adopt the principles of patients safety as their institutional goal and so try to improve nursing skills, knowledge and attitude related to patient safety and it would be better to assess the level of nurses’ culture of safety and their safety competency level in order to improve area of weakness or poor practices and reduce adverse events [37, 38].
Measurement of patient safety culture
Measuring patient safety culture involves assessing the attitudes, perceptions, and behaviors of healthcare staff related to patient safety in a healthcare organization. There are several tools and survey instruments available to measure patient safety culture. In this review, two self-reported questionnaires were found to have been applied to understand the dimensions and scores of patient safety culture in health institutions. The Safety Attitude Questionnaire (SAQ) [28, 33] and the Hospital Survey on Patient Safety Culture (HSOPSC) [21, 23, 27, 32] were two assessment tools that employed Likert scales. However, in their study, G Alsalem, P Bowie and J Morrison [39] revealed that five instruments are used to assess the patient safety culture and climate in health institutions. Furthermore, these tools vary in their psychometric properties and scope.
The aforementioned survey instruments assess various aspects of patient safety culture, such as communication, teamwork, error reporting, and leadership. The results of these surveys can be used to identify areas of strength and areas for improvement in the patient safety culture of an organization.
In general, patient safety culture measurement is a continuous activity that should be conducted on a regular basis to assess success and identify areas for improvement. The information gathered through these surveys and other ways may be utilized to design and execute plans to improve the patient safety culture.
The most common study design among the studies was a questionnaire-based descriptive quantitative approach. Using different study designs, such as qualitative research and a variety of data collection methods, could help improve understanding of the safety culture and health care provider perceptions and would be required to address the existing relationship between safety culture and nursing competency [40].
Measurement of safety nursing competency
Eight of the studies, or 50% of the literature, in this review showed that nurses were more competent in communicating effectively than working in teams with colleagues, and their overall safety culture score was positive. Likewise, LM Zabin, RSA Zaitoun and AA Abdullah [41] found that both organizational learning and continuous improvement, as well as cooperation within units, received the highest composite frequency of patient safety perception.
In the current findings, the reviewed literature mentioned four self-reported measurement tools for safety competency. Despite that, there was no consensus on the best tool for measuring safety competencies, and the lack of a key self-reported tool for measuring safety culture and linking it to nursing safety competency limited the ability to directly assess the effect of nursing competency on safety culture [42]. As a result, more research is needed to enrich the literature, improve the understanding of the effect of safety competency on safety culture scores among nurses, and help in providing more appropriate operational definition of safety culture and nursing safety competency [43].
Although we used broad keywords to search different online databases, the retrieved articles did not specifically discuss the relationship between the dimensions of the safety culture, perception, and competency in nursing safety. Additionally, the lack of a standardized tool to measure the concepts of safety culture and nursing safety competency made it difficult to find a robust number of targeted studies and limited our ability to find specific operational definitions to the concepts of safety culture and nursing safety competency that was used consistently across the literature.
Moreover, using self-reported surveys and relying on convenient sampling eased data collection and provide more objective data for many of the studies in this review. However, there were drawbacks that limited the generalizability and might not cover all aspects of the studies’ content. Therefore, future use of mixed designs with the use of qualitative methods is highly recommended to deepen the study issue and explore the unique relationship between the dimensions of the safety culture and nursing competency that can play a pivotal role in improving safety practices.
This review study recognizes the importance of conducting additional searches and reviews and broadening the scope of keywords used to search online databases to focus on the core of this study. In addition, it is recommended to investigate the effect of nursing competency on perceptions of dimensions of safety culture and to make valid comparisons between demographics and cultures.
More research would provide a better understanding and may have a greater clinical impact and aid in improving and delivering highly effective, safe, and efficient care. Furthermore, the findings would support synchronicity between academic clinical programs and nursing staff safety practices. For example, nursing students receive competency-based training that allows them to live in a safe environment and directly implement the dimension of safety culture [44].
Limitations
This systematic review study has several limitations. First, we restricted the databases to four primary resources considered suitable for gathering eligible articles for the study purpose. The second is that the delimiters of this review included only articles in English, so some related articles may not have been included. Another limitation that should be highlighted is that we reviewed articles published between 2018 and 2022 to include the most recent data, but this also restricted the number of retrieved studies.
Another potential limitation was that the results of the reviewed studies could not be generalized. The articles were only published in peer-reviewed journals to ensure the high quality of evidence and the reported findings, which omitted many worthwhile studies such as grey and unpublished studies. Additionally, the study designs of the majority of the retrieved papers were descriptive, which restricts the generalizability of their findings and prevents access to many relevant studies. Therefore, it is recommended to conduct further systematic or integrative reviews that might include qualitative and descriptive studies as well as expand the inclusion criteria for other types of literature.
Conclusions
This systematic review draws several conclusions from the sixteen reviewed articles. First, the study showed no specific tool to measure the safety culture and nursing safety competency dimensions. Additionally, no study explicitly discussed the effect of nursing safety competency on safety culture scores among nursing staff. However, most of the studies employed a questionnaire-based descriptive approach. Conducting more research with different study designs such as the experimental, qualitative, and longitudinal approaches may enhance the understanding and assist in constructing a valid and more reliable tool to measure the effect of nursing safety competency on safety culture. Second, rigorous research needed to establish a well-designed competency-based training program to improve safety scores among more diverse demographics and cultures is needed. The findings can motivate administrators to promote safety culture in different health care facilities, as well as increase professional awareness of the factors that impact safety culture and, consequently, patient safety. Finally, the key to improving safety competency for nurses is to create a culture of continuous learning and improvement, where nurses are encouraged and supported to develop their knowledge, skills and abilities in order to provide safe, high-quality care to patients.
Data Availability
All data generated or analyzed during this study are included in this published article. The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Patient safety [https://www.who.int/news-room/facts-in-pictures/detail/patient-safety].
Patient Safety Representatives Unite to Implement Global Patient Safety Action Plan. in the United States [https://blogs.cdc.gov/safehealthcare/patient-safety-action-plan/].
Kruk ME, Gage AD, Joseph NT, Danaei G, García-Saisó S, Salomon JA. Mortality due to low-quality health systems in the universal health coverage era: a systematic analysis of amenable deaths in 137 countries. The Lancet. 2018;392(10160):2203–12.
Patient Safety. [https://www.who.int/news-room/fact-sheets/detail/patient-safety].
Khoshakhlagh AH, Khatooni E, Akbarzadeh I, Yazdanirad S, Sheidaei A. Analysis of affecting factors on patient safety culture in public and private hospitals in Iran. BMC Health Serv Res. 2019;19(1):1009.
Fukada M. Nursing competency: definition, structure and development. Yonago acta medica. 2018;61(1):001–7.
Huh A, Shin JH. Person-centered care practice, patient safety competence, and patient safety nursing activities of nurses working in geriatric hospitals. Int J Environ Res Public Health. 2021;18(10):5169. https://doi.org/10.3390/ijerph18105169
Al Ma’mari Q, Sharour LA, Al Omari O. Fatigue, burnout, work environment, workload and perceived patient safety culture among critical care nurses. Br J Nurs. 2020;29(1):28–34.
Halabi JO, Nilsson J, Lepp M. Professional competence among registered nurses working in hospitals in Saudi Arabia and their experiences of quality of nursing care and patient safety. J Transcult Nurs. 2021;32(4):425–33. https://doi.org/10.1177/1043659621992845
Wang KY, Chou CC, Lai JC. A structural model of total quality management, work values, job satisfaction and patient-safety-culture attitude among nurses. J Nurs Adm Manag. 2019;27(2):225–32.
Yan L, Yao L, Li Y, Chen H. Assessment and analysis of patient safety competency of chinese nurses with associate degrees: a cross-sectional study. Nurs Open. 2021;8(1):395–403. https://doi.org/10.1002/nop2.640
Wami SD, Demssie AF, Wassie MM, Ahmed AN. Patient safety culture and associated factors: a quantitative and qualitative study of healthcare workers’ view in Jimma zone Hospitals, Southwest Ethiopia. BMC Health Serv Res. 2016;16:495.
Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res. 2012;22(10):1435–43.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Pluye P, Robert E, Cargo M, Bartlett G, O’cathain A, Griffiths F, Boardman F, Gagnon M-P, Rousseau M. Proposal: a mixed methods appraisal tool for systematic mixed studies reviews. Montréal: McGill University. 2011;2:1–8.
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, Britten N, Roen K, Duffy S. Guidance on the conduct of narrative synthesis in systematic reviews. Prod ESRC methods programme Version. 2006;1(1):b92.
Letourneau RM, McCurry MK. The effect of transition to Practice Programs on the Self-Assessment of newly licensed registered Nurses’ confidence in Quality and Safety Competency Attainment. Nurs Educ Perspect. 2019;40(3):151–6. https://doi.org/10.1097/01.Nep.0000000000000438
Peñataro-Pintado E, Rodríguez-Higueras E, Llauradó-Serra M, Gómez-Delgado N, Llorens-Ortega R, Díaz-Agea JL. Development and Validation of a Questionnaire of the Perioperative Nursing Competencies in Patient Safety. Int J Environ Res Public Health 2022, 19(5). https://doi.org/10.3390/ijerph19052584
Huh A, Shin JH. Person-Centered Care Practice, Patient Safety Competence, and Patient Safety Nursing Activities of Nurses Working in Geriatric Hospitals. Int J Environ Res Public Health 2021, 18(10).
Han JH, Roh YS. Teamwork, psychological safety, and patient safety competency among emergency nurses. Int Emerg Nurs. 2020;51:100892. https://doi.org/10.1016/j.ienj.2020.100892
Han Y, Kim JS, Seo Y. Cross-sectional study on Patient Safety Culture, Patient Safety Competency, and adverse events. West J Nurs Res. 2020;42(1):32–40. https://doi.org/10.1177/0193945919838990
Alshehry AS. Nurse–patient/relatives conflict and patient safety competence among nurses. INQUIRY: The Journal of Health Care Organization Provision and Financing. 2022;59. https://doi.org/10.1177/00469580221093186
Mahsoon AN, Dolansky M. Safety culture and systems thinking for predicting safety competence and safety performance among registered nurses in Saudi Arabia: a cross-sectional study. J Res Nurs. 2021;26(1–2):19–32.
Kakemam E, Gharaee H, Rajabi MR, Nadernejad M, Khakdel Z, Raeissi P, Kalhor R. Nurses’ perception of patient safety culture and its relationship with adverse events: a national questionnaire survey in Iran. BMC Nurs. 2021;20(1):1–10. https://doi.org/10.1186/s12912-021-00571-w
Habibi Soola A, Ajri-Khameslou M, Mirzaei A, Bahari Z. Predictors of patient safety competency among emergency nurses in Iran: a cross-sectional correlational study. BMC Health Serv Res. 2022;22(1):1–10. https://doi.org/10.1186/s12913-022-07962-y
Connell CJ, Cooper S, Endacott R. Measuring the safety climate in an australian emergency department. Int Emerg Nurs. 2021;58:101048.
Najjar S, Baillien E, Vanhaecht K, Hamdan M, Euwema M, Vleugels A, Sermeus W, Schrooten W, Hellings J, Vlayen A. Similarities and differences in the associations between patient safety culture dimensions and self-reported outcomes in two different cultural settings: a national cross-sectional study in palestinian and belgian hospitals. BMJ Open. 2018;8(7):e021504. https://doi.org/10.1136/bmjopen-2018-021504
Lousada LM, da Silva Dutra FC, da Silva BV, de Oliveira NLL, Bastos IB, de Vasconcelos PF, de Carvalho R. Patient safety culture in primary and home care services. BMC Fam Pract. 2020;21(1):188. https://doi.org/10.1186/s12875-020-01263-1
Khamaiseh A, Al-Twalbeh D, Al-Ajlouni K. Patient safety culture in jordanian primary health-care centres as perceived by nurses: a cross-sectional study. East Mediterr Health J. 2020;26(10):1242–50. https://doi.org/10.26719/emhj.20.044
Son YJ, Lee EK, Ko Y. Association of Working Hours and Patient Safety Competencies with Adverse Nurse Outcomes: A Cross-Sectional Study. Int J Environ Res Public Health 2019, 16(21). https://doi.org/10.3390/ijerph16214083
Bramstedt KA. The carnage of substandard research during the COVID-19 pandemic: a call for quality. J Med Ethics. 2020;46(12):803–7.
Kakemam E, Gharaee H, Rajabi MR, Nadernejad M, Khakdel Z, Raeissi P, Kalhor R. Nurses’ perception of patient safety culture and its relationship with adverse events: a national questionnaire survey in Iran. BMC Nurs. 2021;20(1):60.
Khamaiseh A, Al-Twalbeh D, Al-Ajlouni K: Patient safety culture in Jordanian primary health-care centres as perceived by nurses: a cross-sectional study. East Mediterr Health J. 2020;26(10):1242–1250.
Hwang J-I. What are hospital nurses’ strengths and weaknesses in patient safety competence? Findings from three korean hospitals. Int J Qual Health Care. 2015;27(3):232–8.
Mahsoon AN, Dolansky M: Safety culture and systems thinking for predicting safety competence and safety performance among registered nurses in Saudi Arabia: a cross-sectional study. Journal of Research in Nursing. 2021;26(1–2):19–32.
Cho SM, Choi J. Patient Safety Culture Associated with Patient Safety Competencies among registered nurses. J Nurs Scholarsh. 2018;50(5):549–57.
Rodziewicz TL, Houseman B, Hipskind JE. Medical Error Reduction and Prevention. In: StatPearls. edn. Treasure Island (FL): StatPearls Publishing Copyright © 2022,StatPearls Publishing LLC.; 2022.
Hafezi A, Babaii A, Aghaie B, Abbasinia M. The relationship between patient safety culture and patient safety competency with adverse events: a multicenter cross-sectional study. BMC Nurs. 2022;21(1):292.
Alsalem G, Bowie P, Morrison J. Assessing safety climate in acute hospital settings: a systematic review of the adequacy of the psychometric properties of survey measurement tools. BMC Health Serv Res. 2018;18(1):353.
Alqattan H, Morrison Z, Cleland JA. A narrative synthesis of qualitative studies conducted to assess patient Safety Culture in Hospital settings. Sultan Qaboos Univ Med J. 2019;19(2):e91–8.
Zabin LM, Zaitoun RSA, Abdullah AA. Patient safety culture in Palestine: university hospital nurses’ perspectives. BMC Nurs. 2022;21(1):204.
Arzahan ISN, Ismail Z, Yasin SM. Safety culture, safety climate, and safety performance in healthcare facilities: a systematic review. Saf Sci. 2022;147:105624.
Kalteh HO, Mortazavi SB, Mohammadi E, Salesi M. The relationship between safety culture and safety climate and safety performance: a systematic review. Int J Occup Saf Ergon. 2021;27(1):206–16.
Debourgh GA. Synergy for patient safety and quality: academic and service partnerships to promote effective nurse education and clinical practice. J Prof nursing: official J Am Association Colleges Nurs. 2012;28(1):48–61.
Acknowledgements
Not applicable.
Funding
This work was not supported by research funding.
Author information
Authors and Affiliations
Contributions
R.A.: Conceptualization, Introduction, Methodology, Analysis and results, Discussion, and Conclusion. L.T.: Conceptualization, Methodology, Analysis, Discussion, and Conclusion.N.S.: Review & Editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zaitoun, R.A., Said, N.B. & de Tantillo, L. Clinical nurse competence and its effect on patient safety culture: a systematic review. BMC Nurs 22, 173 (2023). https://doi.org/10.1186/s12912-023-01305-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12912-023-01305-w