Abstract
Background
Acute kidney injury (AKI) is a serve and harmful syndrome in the intensive care unit. Comparing to the patients with AKI stage 1/2, the patients with AKI stage 3 have higher in-hospital mortality and risk of progression to chronic kidney disease. The purpose of this study is to develop a prediction model that predict whether patients with AKI stage 1/2 will progress to AKI stage 3.
Methods
Patients with AKI stage 1/2, when they were first diagnosed with AKI in the Medical Information Mart for Intensive Care, were included. We used the Logistic regression and machine learning extreme gradient boosting (XGBoost) to build two models which can predict patients who will progress to AKI stage 3. Established models were evaluated by cross-validation, receiver operating characteristic curve, and precision–recall curves.
Results
We included 25,711 patients, of whom 2130 (8.3%) progressed to AKI stage 3. Creatinine, multiple organ failure syndromes were the most important in AKI progression prediction. The XGBoost model has a better performance than the Logistic regression model on predicting AKI stage 3 progression. Thus, we build a software based on our data which can predict AKI progression in real time.
Conclusions
The XGboost model can better identify patients with AKI progression than Logistic regression model. Machine learning techniques may improve predictive modeling in medical research.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Acute kidney injury (AKI) is a common syndrome in intensive care unit with an incidence of nearly 50% [1]. It is characterized by sudden increase of serum creatinine and decrease of urine volume [2]. The survival rate of patients with AKI will decrease, which may relate to the duration of AKI [1]. A previous study found that comparing to patients with AKI duration of less than 7 days, the 1-year survival of patients with AKI lasting the entire hospital stay decreased from 90% to 44% [3]. According to the KDIGO criteria, AKI is classified into stage 1, stage 2, and stage 3 for severity [2]. Comparing to the patients with AKI stage 1/2, the patients with AKI stage 3 have higher in-hospital mortality [1] and risk of progression to chronic kidney disease (CKD) [4]. Therefore, early prediction of progression of AKI stage 1/2 to AKI stage 3 is of great importance. It is an alert for clinicians to prompt measures to avoid additional kidney damage or delay in recovery [5].
Currently, few methods were developed to predict AKI stage 1/2 to AKI stage 3. Furosemide stress test (FST) was considered as a robust predictive approach to identify who will progress to AKI stage 3 [6]. However, the clinical application has been hampered for several reasons such as lacking of high quality RCT [5], not stable for patients with unstable hemodynamics [7], no standardization of dosage and time [8] and ambiguous effect of other factors such as fluid balance and diuretic on the outcome [9].
Machine learning is a series of algorithms with set objective and without being explicitly programmed. It performs well in development of prediction model and has been widely used in medical data in recent years [10]. Machine learning technology may be helpful to establish a robust prediction model predicting AKI stage 1/2 to AKI stage 3. Currently, there are studies predicting AKI by machine learning [11,12,13]. However, there is no study in predicting AKI progression by machine learning. In this study, we developed prediction models to predict AKI stage 3 progression by using machine learning techniques (extreme gradient boosting) and Logistic regression.
Method
Data source
MIMIC-III (Medical Information Mart for Intensive Care III) is a large, de-identified comprehensive data set. It includes patients from the ICU at Beth Israel Deaconess Medical Center in Boston, Massachusetts from 2001 to 2012 [14]. This database includes general information, vital sign measurements, laboratory test results, and so on. As this study was an analysis of a third-party anonymous public database that has been approved by the Institutional Review Board (IRB), IRB approval from our institution was waived.
Participants
Definition of AKI was: an increase in serum creatinine of 0.3 mg/dl or 50% from the baseline value or urine output < 0.5 ml/kg h [2]. This definition was consistent with the recommendations given by the Kidney Disease Improving Global Outcomes (KDIGO) criteria. The critically ill patients were included if their primary diagnosis was AKI stage 1/2. Patients who are younger than 18 years old or suffering from chronic kidney disease (CKD) were excluded. Furthermore, Patients who received RRT or progressed to AKI stage 3 within 72 h or over 28 days of first AKI diagnosis were also excluded.
Predictors of model
We collected clinical and laboratory variables obtained within 72 h before and after the AKI diagnosis. For some variables measured multiple times in these 6 days, the outcome closest to the date of diagnosed AKI will be included in the model. We analyzed age and vital signs including heart rate, blood pressure, respiratory rate, and temperature. Besides, we followed the factors of other studies including sodium, potassium, glucose, creatinine, lactate, blood urea nitrogen (BUN), anion gap, PaO2, and pH [15]. Furthermore, we also analyzed participants whether received vasoactive drugs, cardiac surgery, mechanical ventilation, and whether have sepsis, respiratory failure, and multiple organ failure syndromes (MODS) [16]. Specifically, creatinine was calculated the mean of measurement within 6 days because serial measurements have better predictive capability than single time-point [17]. As for FST, we calculate the patient’s mean hourly urine output volume over 6 hours after receiving furosemide [18].
Data preprocessing
Variables with missing values of more than 70% were excluded because of possible bias from missing data. Extreme gradient boosting (XGBoost) can automatically process missing values. As for the Logistic regression model, we complete missing values using the multiple imputation method in scikit-learn [19]. In this algorithm, we models that a feature column is designated as output and other feature columns are treated as inputs by using that estimating for imputation iteratively [20]. And, most classification algorithms will only perform optimally when the number of samples of each class is roughly the same [21]. The low rate of progression patients (8.3%) may have bad effect on model generalization. A combination of over-sampling and under-sampling [22] can balance the proportion of patients in the two groups. This algorithm first over-sample minority class examples by generating examples and then under-sample majority class examples by deleting examples [23]. We divided the original data into a train set (70%) and a teat set (30%). Both XGBooost and Logistic regression were train on the train set and assessed on the test set.
Model selection and development
We compared characteristics between groups by Student t-test. In addition, as for categorical and nonnormal variables, we used the Chi-square test and the Kruskal–Wallis Rank Sum Test respectively.
Logistic regression model to predict AKI progression was established by forward selection and backward elimination. In this process, we iteratively assess model by Akaike Information Criteria (AIC) after including or excluding a feature. AIC give consideration to the features incorporated into the model and the predictive performance [23]. Therefore, the final model have best prediction performance and contain the fewest features.
Extreme gradient boosting (XGBoost) is an ensemble method of machine learning based on decision trees [24]. The decision trees was set as the weak learners and binary logistic was set as objective. We iteratively re-fit the weak classifier (decision tree) to the residuals of the previous model. Each iteration adds a tree to the existing tree to fit the residuals between the predicted and true values of the previous tree. XGBoost hyperparameters included learning rate, maximum depth of trees, minimum child weight, subsample ratio, minimum split loss, parameters for subsampling of columns and parameters for regularization. In this study, we performed 100 iterations of the cross-validation process, which is also the default and recommended value [25]. All analyses were performed using Python, version 3.7.9.
In train set, the data was randomly divided into five equal-sized subsamples. Four subsamples were used to train the model and then validated in the remaining one. On this basis, hyperparameters were tuned for the higher area under receiver operating characteristic curve (AU-ROC) which can evaluate the predictive ability of the model. We used grid search which can cycle through tuning and scoring to select the hyperparameters. Learning curve that demonstrates AU-ROC of the model by changing the subsample ratio helps prevent overfitting or overfitting. After choosing the hyperparameters, the XGBoost was trained for the final model on the whole train set. Then, the model was estimated on the test set.
Results
Participants
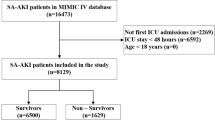
Of the 61,532 patients in MIMIC-III, 34,440 (56.0%) patients were diagnosed AKI stage 1/2 of the first AKI diagnosis. 8729 patients were excluded according to the pre-designed criteria. A total of 25,711 patients were included in our analysis; 2130(8.3%) patients finally progress to AKI stage 3, and 23,581 (91.7%) patients did not (Fig. 1).
Characteristic differences between groups are shown in Table 1. There were more women (44.5% vs. 41.3%; p = 0.005) and emergency patients in progression group. Fewer patients underwent cardiac surgery in the progression group than in the non-progression group (72.9% vs. 80.8%; p < 0.001). The creatinine (2.4 ± 2.0 vs. 1.1 ± 0.9 mg/dl; p < 0.001) and the BUN (39.0 ± 26.2 vs. 23.5 ± 17.0 mg/dl; p < 0.001) were higher, and FST (93.6 ± 108.6 vs. 108.8 ± 113.1 ml/h; p < 0.001) was lower in the progression group. The progression group had higher heart rate (90.2 ± 21.2 vs. 86.1 ± 17.9; p < 0.001), higher respiratory rate (20.3 ± 6.9 vs. 19.1 ± 5.9; p < 0.001) than the non-progression group. As for laboratory data, lactate (2.5 ± 2.3 vs. 2.1 ± 1.6 mmol/l; p < 0.001), glucose (144.9 ± 105.2 vs. 136.3 ± 68.4 mg/dl; p < 0.001), and potassium (4.3 ± 0.8 vs. 4.2 ± 0.6 mmol/l; p < 0.001) were higher in progression group. But sodium (138.5 ± 4.6 vs. 137.6 ± 5.6 mmol/l; p < 0.001) was lower in progression group. And progression group had higher rate of mechanical ventilation (34.3% vs. 28.2%; p < 0.001), higher rate of MODS (94.1% vs. 59.2%; p < 0.001), higher rate of respiratory failure (63.7% vs. 34.0%; p < 0.001), higher rate of sepsis (41.4% vs. 14.7%; p < 0.001).
The logistic regression model
The results of the Logistic regression model are shown in Table 2 and Additional file 2: Fig. S1. After excluding the variables with high colinearity through the variance inflation factor (VIF) [26], the final variables included in the analysis are as follows. As expected, with MODS (odds ratio [OR] 1.55; 95% confidence interval 1.50 to 1.60), sepsis (OR 1.71; 95% CI 1.60 to 1.82), respiratory failure (OR 1.47; 95% CI 1.41 to 1.54), and creatinine (OR 1.20; 95% CI 1.15 to 1.25) were associated with increased probability of AKI progression(Table 1). Besides, BUN, lactate, and so on are also considered to be associated with AKI progression. On the contrary, male (OR 0.91; 95% CI 0.87 to 0.95) and previous cardiac surgery (OR 0.86; 95% CI 0.81 to 0.91) were associated with a reduced likelihood of AKI progression (Table 2).
The XGBoost model
Determining by grid search, the hyperparameters used in our analysis were set as learning rate = 0.19, minimum child weight = 8, maximum tree depth = 3, and the number of rounds = 100 (Additional file 1: Table S1). With these hyperparameters, the training score increases as the number of rounds increases, and the cross-validation score test log-loss is only slightly higher than the training log-loss as the tree grows (Fig. 2A).
The training process of the extreme gradient boosting machine. A Cross-validation during XGBoost hyperparameter tuning. The log-loss value for the training and testing datasets is shown in the vertical axis. The dashed vertical line indicates the number of rounds with the minimum log-loss in the test sample. B Learning curve of the XGBoost model after hyperparameter tuning. AU-ROC value for the testing and training datasets is shown in the vertical axis. With the subsample ratio increasing, AU-ROC of training datasets decreases, and AU-ROC of testing datasets increases. The training score is always higher than the test score
Learning curve demonstrated the cross-validation on train set and represent the generalization performance of the model as a function of the size of the training set [27]. Model was train on four-fifths of train set and validate on one-fifth of train set iteratively by AU-ROC. As the size grows, the difference between performance of the model on the train and test sets gradually narrowed (Fig. 2B) suggesting the model is generalizable and robust [28].
Model performance
The model was evaluated using receiver operating characteristic curve (ROC) and precision–recall curve (PRC) on test set. AU-ROC of XGBoost is significantly higher than the Logistic regression model (AU-ROC 0.926; 95% CI 0.917 to 0.931 vs. 0.784; 95% CI 0.771 to 0.796, respectively; Fig. 3A). And area under precision–recall curve (AU-PRC) of XGBoost is also significantly higher than the Logistic regression model (AU-PRC 0.855; 95% CI 0.844 to 0.861 vs. 0.584; 95% CI 0.575 to 0.593, respectively; Fig. 3B) We also showed the confusion matrix for the two models in predicting AKI progression (Fig. 3C).
Performance of the XGBoost and Logistic regression model A Receiver operating characteristic curve for estimating the discrimination between the Logistic regression model and the XGBoost model. B Precision–recall curve for estimating the discrimination between the Logistic regression model and the XGBoost model. C Confusion matrix of the Logistic regression model and XGBoost model. The color represents the number of patients. Whether progress is represented by numbers
Tree interprets
SHAP (SHapley Additive exPlanations) is a game theory method which can intuitively and accurately explain the output of machine learning model [29]. As for this dichotomous classifier, the higher SHAP value, the higher probability of AKI progression. The base value is defined as the output when each variable in the training dataset is averaged, which can represent the average of the sample. With original data, we calculate the base value is − 0.468. Therefore, the average of these patients is unlikely to progress to AKI stage 3, which can be explained by the relatively low proportion of progression patients (8.3%).
SHAP value can intuitively show features each contribution to push the model output from the base value (Additional file 3: Fig. S2). SHAP value can be considered as a quantified contribution. We can easily find the contribution of all features and which contribution is most (Fig. 4). The features are ordered in order of importance. Feature importance was calculated by the mean contribution of every observation, which is equal to the traditional method [30]. The serum creatinine was the most important variable, followed by MODS and respiratory failure. The specific importance of each variable is shown in Additional file 4: Fig. S3.
Software for prediction
A web calculator based on this data was developed for clinicians to predict patients’ AKI progression (https://260147169.github.io/AKI-progression/AKI-progression-calculator.html) (Fig. 5). After inputting the corresponding data of the patient, the prediction can be made automatically. Besides, misssing value is acceptable, because XGBoost can complete automatically.
The calculator for predcting AKI progression in real time. Feature importance was calculated by the mean contribution of every observation, which is equal to the traditional method. Abbreviations and annotations: BUN, blood urea nitrogen; FST, furosemide stress test; MODS, multiple organ failure syndromes
Discussion
In this study, we analyzed data in MIMIC-III and proposed machine learning models predicting AKI progression. The machine learning model had excellent performance in predicting AKI stage 1/2 to AKI stage 3 with ROC of 0.926, which was significantly better than the performance of logistics model (0.926 [95% CI 0.917–0.931] vs. 0.784 [95% CI 0.771–0.796]). By interpreting the importance of each variable of the model (Additional file 4: Fig. S3), we found creatinine and MODS were more important than others.
Comparing AKI stage 1, patients with AKI stage 3 have higher risk of mortality in the intensive care unit (odds ratio (OR) 2.19 [95% CI 1.44–3.35] vs. OR 7.18 [95% CI 5.13–10.04]) [31]. Therefore, predicting AKI progression is always one of research highlights. FST, a method for predicting AKI progression, had desirable prediction ability, which of AU-ROC was 0.88 [6]. Our model and previous FST studies have comparable prediction ability (AU-ROC 0.926 vs. 0.88). However, FST has some limitations including not stable for patients with unstable hemodynamics [7] and no standardization of dosage and time [8]. Our model is based on vital signs and laboratory data, which are easily assessable in most institutions. These features are also significant predictors of AKI in the others model such as sepsis and creatinine [11, 13]. Real-time automated prediction and analysis of main cause are also advantages of our study.
We employed visualization function in SHAP [32] to find the effect of the specific value of each variable on model output. There are some factors contributing most including creatinine, MODS, BUN, sepsis and so on. The KDIGO criteria proposed some similar exposures that may cause AKI including sepsis and shock [2]. Advanced age, underlying CKD, sepsis, and cardiac surgery were also proposed as risk factors for AKI [1, 33]. SHAP value was found to increase with the increase of creatinine until creatinine probably reach 3 mg/dl (265.2 \(\upmu\)mol/L) (Fig. 6A). This is in line with the mainstream view in clinicians [34, 35]. The relationship between SHAP value and FST (Fig. 6B) is consistent with previous studies that FST < 100 ml/h increases the risk of AKI progression [7, 18].
Our study found that machine learning has better performance than logistic regression, which is similar to the previous prediction study of AKI [13, 36]. Lee et al gradient boosting tree has better performance than logistic regression (0.78 vs. 0.69) on predicting AKI after cardiac surgery [13]. Zhang et al found the machine learning model outperformed the logistic regression model (AU-ROC 0.860 vs. 0.728) in differentiating between the volume-responsive and volume-unresponsive AKI [36]. The advantages of machine learning include ability of capturing complex non-linear relationships [37] and focusing more on misclassified observations , especially when the sample size is large enough [37]. And, machine learning can automatically input missing values and give the prediction as soon as possible for intervention in time.
A limitation of this study is a retrospective study with inevitable bias. And, the proportion of patients who eventually progressed to AKI stage 3 (8.3%) is significantly lower than that without progression (91.7%). Even if we use the algorithm to balance the sample, it may still have bad effect on model generalization and reliability. Furthermore, external validation is still required in the following study.
Conclusion
We collected data from MIMIC-III and proposed a predicting model for AKI progression from stage1 to stage 2/3 by machine learning. The model had excellent performance in predicting AKI progression and was significantly better than the performance of logistics model. In the final model, creatinine, MODS and BUN were factors contributing most. The reasons of performance gap and important factors require further study.
Availability of data and materials
The datasets used for the analysis in the current study are available from the corresponding author on reasonable request.
References
Ronco C, Bellomo R, Kellum JA. Acute kidney injury. Lancet. 2019;394(10212):1949–64.
Group KDIGOKAKIW. Kdigo clinical practice guideline for acute kidney injury. Kidney Int. 2012;1–138.
Kellum JA, Sileanu FE, Bihorac A, Hoste EA, Chawla LS. Recovery after acute kidney injury. Am J Respir Crit Care Med. 2017;195(6):784–91. https://doi.org/10.1164/rccm.201604-0799OC.
Chawla LS, Amdur RL, Amodeo S, Kimmel PL, Palant CE. The severity of acute kidney injury predicts progression to chronic kidney disease. Kidney Int. 2011;79(12):1361–9. https://doi.org/10.1038/ki.2011.42.
Vanmassenhove J, Kielstein J, Jorres A, Van Biesen W. Management of patients at risk of acute kidney injury. Lancet. 2017;389(10084):2139–51. https://doi.org/10.1016/S0140-6736(17)31329-6.
Chen J-J, Chang C-H, Huang Y-T, Kuo G. Furosemide stress test as a predictive marker of acute kidney injury progression or renal replacement therapy: a systemic review and meta-analysis. Crit Care. 2020;24(1):202. https://doi.org/10.1186/s13054-020-02912-8.
Koyner JL, Davison DL, Brasha-Mitchell E, Chalikonda DM, Arthur JM, Shaw AD, Tumlin JA, Trevino SA, Bennett MR, Kimmel PL, Seneff MG, Chawla LS. Furosemide stress test and biomarkers for the prediction of AKI severity. J Am Soc Nephrol. 2015;26(8):2023–31. https://doi.org/10.1681/ASN.2014060535.
Coca A, Aller C, Reinaldo Sánchez J, Valencia AL, Bustamante-Munguira E, Bustamante-Munguira J. Role of the furosemide stress test in renal injury prognosis. Int J Mol Sci. 2020;21(9):3086. https://doi.org/10.3390/ijms21093086.
Rewa OG, Bagshaw SM, Wang X, Wald R, Smith O, Shapiro J, McMahon B, Liu KD, Trevino SA, Chawla LS, Koyner JL. The furosemide stress test for prediction of worsening acute kidney injury in critically ill patients: a multicenter, prospective, observational study. J Crit Care. 2019;52:109–14. https://doi.org/10.1016/j.jcrc.2019.04.011.
Deo RC. Machine learning in medicine. Circulation. 2015;132(20):1920–30. https://doi.org/10.1161/CIRCULATIONAHA.115.001593.
Koyner JL, Carey KA, Edelson DP, Churpek MM. The development of a machine learning inpatient acute kidney injury prediction model. Crit Care Med. 2018;46(7):1070–7. https://doi.org/10.1097/CCM.0000000000003123.
Sanchez-Pinto LN, Venable LR, Fahrenbach J, Churpek MM. Comparison of variable selection methods for clinical predictive modeling. Int J Med Inform. 2018;116:10–7. https://doi.org/10.1016/j.ijmedinf.2018.05.006.
Lee HC, Yoon HK, Nam K, Cho YJ, Kim TK, Kim WH, Bahk JH. Derivation and validation of machine learning approaches to predict acute kidney injury after cardiac surgery. J Clin Med. 2018;7(10):322. https://doi.org/10.3390/jcm7100322.
Johnson AE, Pollard TJ, Shen L, Lehman LW, Feng M, Ghassemi M, Moody B, Szolovits P, Celi LA, Mark RG. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3:160035. https://doi.org/10.1038/sdata.2016.35.
Pozzoli S, Simonini M, Manunta P. Predicting acute kidney injury: current status and future challenges. J Nephrol. 2018;31(2):209–23. https://doi.org/10.1007/s40620-017-0416-8.
Wu L, Hu Y, Liu X, Zhang X, Chen W, Yu ASL, Kellum JA, Waitman LR, Liu M. Feature ranking in predictive models for hospital-acquired acute kidney injury. Sci Rep. 2018;8(1):17298. https://doi.org/10.1038/s41598-018-35487-0.
Isshiki R, Asada T, Sumida M, Hamasaki Y, Nangaku M, Noiri E, Doi K. Modest impact of serial measurements of acute kidney injury biomarkers in an adult intensive care unit. Nephron. 2018;139(3):243–53. https://doi.org/10.1159/000488219.
Chawla LS, Davison DL, Brasha-Mitchell E, Koyner JL, Arthur JM, Shaw AD, Tumlin JA, Trevino SA, Kimmel PL, Seneff MG. Development and standardization of a furosemide stress test to predict the severity of acute kidney injury. Crit Care. 2013;17(5):207. https://doi.org/10.1186/cc13015.
Pedregosa F, Varoquaux G, Gramfort A, Michel V, Thirion B, Grisel O, Blondel M, Prettenhofer P, Weiss R, Dubourg V, Vanderplas J, Passos A, Cournapeau D, Brucher M, Perrot M. Scikit-learn: machine learning in Python. J Mach Learn Res. 2011;12(85):2825–30.
van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1–67. https://doi.org/10.18637/jss.v045.i03.
Yu H, Yang X, Zheng S, Sun C. Active learning from imbalanced data: a solution of online weighted extreme learning machine. IEEE Trans Neural Netw Learn Syst. 2019;30(4):1088–103. https://doi.org/10.1109/TNNLS.2018.2855446.
Lemaitre G, Nogueira F, Aridas CK. Imbalanced-learn: a python toolbox to tackle the curse of imbalanced datasets in machine learning. J Mach Learn Res. 2017;18:559–63.
Batista GEAPA, Prati RC, Monard MC. A study of the behavior of several methods for balancing machine learning training data. SIGKDD Explor Newsl. 2004;6(1):20–9. https://doi.org/10.1145/1007730.1007735.
Chen T, Guestrin C. Xgboost: a scalable tree boosting system. https://doi.org/10.1145/2939672.2939785
Tang CQ, Li JQ, Xu DY, Liu XB, Hou WJ, Lyu KY, Xiao SC, Xia ZF. Comparison of machine learning method and logistic regression model in prediction of acute kidney injury in severely burned patients. Zhonghua Shao Shang Za Zhi. 2018;34(6):343–8. https://doi.org/10.3760/cma.j.issn.1009-2587.2018.06.006.
Ferrari F, Puci MV, Ferraro OE, Romero-Gonzalez G, Husain-Syed F, Rizo-Topete L, Senzolo M, Lorenzin A, Muraro E, Baracca A, Serrano-Soto M, Molano Trivino A, Coutinho Castro A, De Cal M, Corradi V, Brendolan A, Scarpa M, Carta MR, Giavarina D, Bonato R, Iotti GA, Ronco C. Development and validation of quick acute kidney injury-score (q-aki) to predict acute kidney injury at admission to a multidisciplinary intensive care unit. PLoS One. 2019;14(6):0217424. https://doi.org/10.1371/journal.pone.0217424.
Perlich C. In: Sammut C, Webb GI, editors. Learning Curves in Machine Learning. Boston: Springer; 2010. p. 577–80.
Thoma M. Analysis and optimization of convolutional neural network architectures. CoRR. 2017. arXiv:1707.09725
Lundberg SM, Lee SI. A unified approach to interpreting model predictions. Advances in Neural Information Processing Systems 30 (Nips 2017), 2017;30.
Lundberg SM, Nair B, Vavilala MS, Horibe M, Eisses MJ, Adams T, Liston DE, Low DK, Newman SF, Kim J, Lee SI. Explainable machine-learning predictions for the prevention of hypoxaemia during surgery. Nat Biomed Eng. 2018;2(10):749–60. https://doi.org/10.1038/s41551-018-0304-0.
...Hoste EAJ, Bagshaw SM, Bellomo R, Cely CM, Colman R, Cruz DN, Edipidis K, Forni LG, Gomersall CD, Govil D, Honoré PM, Joannes-Boyau O, Joannidis M, Korhonen A-M, Lavrentieva A, Mehta RL, Palevsky P, Roessler E, Ronco C, Uchino S, Vazquez JA, Vidal Andrade E, Webb S, Kellum JA. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41(8):1411–23. https://doi.org/10.1007/s00134-015-3934-7.
Lundberg SM, Erion G, Chen H, DeGrave A, Prutkin JM, Nair B, Katz R, Himmelfarb J, Bansal N, Lee S-I. From local explanations to global understanding with explainable AI for trees. Nat Mach Intell. 2020;2(1):56–67. https://doi.org/10.1038/s42256-019-0138-9.
Levey AS, James MT. Acute kidney injury. Ann Intern Med. 2017;167(9):66–80. https://doi.org/10.7326/AITC201711070.
Flechet M, Falini S, Bonetti C, Guiza F, Schetz M, Van den Berghe G, Meyfroidt G. Machine learning versus physicians’ prediction of acute kidney injury in critically ill adults: a prospective evaluation of the AKIpredictor. Crit Care. 2019;23(1):282. https://doi.org/10.1186/s13054-019-2563-x.
Bhatraju PK, Zelnick LR, Katz R, Mikacenic C, Kosamo S, Hahn WO, Dmyterko V, Kestenbaum B, Christiani DC, Liles WC, Himmelfarb J, Wurfel MM. A prediction model for severe AKI in critically ill adults that incorporates clinical and biomarker data. Clin J Am Soc Nephrol. 2019;14(4):506–14. https://doi.org/10.2215/CJN.04100318.
Zhang Z, Ho KM, Hong Y. Machine learning for the prediction of volume responsiveness in patients with oliguric acute kidney injury in critical care. Crit Care. 2019;23(1):112. https://doi.org/10.1186/s13054-019-2411-z.
Goecks J, Jalili V, Heiser LM, Gray JW. How machine learning will transform biomedicine. Cell. 2020;181:92–101. https://doi.org/10.1016/j.cell.2020.03.022.
Acknowledgements
We would like to thank all the workers involved in MIMIC III database system maintenance. Especially to Aijia Ma and RuoRan Wang, for their help in data processing.
Funding
This project was supported by 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYGD18020).
Author information
Authors and Affiliations
Contributions
LFZ and CZW designed the study. LFZ, CZW, YXF and AJM managed data and its quality. LFZ and CZW performed the statistical analysis. All authors participated in data interpretation. LFZ drafted the manuscript. CZW, YXF and AJM contributed substantially to its revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
MIMIC-III is a deidentified dataset. Under The Health Insurance Portability and Accountability Act (HIPAA), the research using it does not constitute human subjects research, and as a result we do not need IRB approval for this study. And the Institutional Review Boards (IRBs) at both MIT and the Beth Israel Deaconess Medical Center (BIDMC) approved the use of the MIMIC-III for research.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S1.
Hyperparameters of the XGboost model
Additional file 2: Figure S1.
Results of the Logistic regression model. The odds ratio[OR] of each feature is shown in the horizontal axis
Additional file 3: Figure S2.
The waterfall plot of a single patient. The SHAP value each feature is shown in the horizontal axis.
Additional file 4: Figure S3.
Feature importance derived from the XGBoost model. The importance of each feature calculated by the average of the absolute value of SHAP value is shown in the horizontal axis
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wei, C., Zhang, L., Feng, Y. et al. Machine learning model for predicting acute kidney injury progression in critically ill patients. BMC Med Inform Decis Mak 22, 17 (2022). https://doi.org/10.1186/s12911-021-01740-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12911-021-01740-2