Abstract
Background
Cardiovascular disease (CVD) is the leading cause of death in the United States (US). Better cardiovascular health (CVH) is associated with CVD prevention. Predicting future CVH levels may help providers better manage patients’ CVH. We hypothesized that CVH measures can be predicted based on previous measurements from longitudinal electronic health record (EHR) data.
Methods
The Guideline Advantage (TGA) dataset was used and contained EHR data from 70 outpatient clinics across the United States (US). We studied predictions of 5 CVH submetrics: smoking status (SMK), body mass index (BMI), blood pressure (BP), hemoglobin A1c (A1C), and low-density lipoprotein (LDL). We applied embedding techniques and long short-term memory (LSTM) networks – to predict future CVH category levels from all the previous CVH measurements of 216,445 unique patients for each CVH submetric.
Results
The LSTM model performance was evaluated by the area under the receiver operator curve (AUROC): the micro-average AUROC was 0.99 for SMK prediction; 0.97 for BMI; 0.84 for BP; 0.91 for A1C; and 0.93 for LDL prediction. Model performance was not improved by using all 5 submetric measures compared with using single submetric measures.
Conclusions
We suggest that future CVH levels can be predicted using previous CVH measurements for each submetric, which has implications for population cardiovascular health management. Predicting patients’ future CVH levels might directly increase patient CVH health and thus quality of life, while also indirectly decreasing the burden and cost for clinical health system caused by CVD and cancers.
Similar content being viewed by others
Background
Cardiovascular disease (CVD) is the leading cause of mortality for both men and women in the United States (US), and accounts for almost 1 in every 4 deaths (https://www.medicalnewstoday.com/articles/282929.php). Cardiovascular health (CVH) metrics, defined by the American Heart Association (AHA), have important implications for CVD prevention [1,2,3,4,5,6]. Individuals with better CVH metrics have lower risk of CVD death and prevention efforts should focus on maintaining or improving CVH across the lifespan (https://www.medicalnewstoday.com/articles/324195.php). Management of CVH levels according to previously recorded measurements may be critical to better manage CVH level of patients, as closer attention to certain risk factors may maximize prevention. Thus, predicting future CVH levels may be associated with better management of CVD.
The seven cardiovascular risk factors which comprise CVH include: smoking status (SMK), physical activity, body mass index (BMI), diet, blood glucose, cholesterol, and blood pressure (BP) [2]. Recent studies [7, 8] have used previous measurements of weight and height data to predict BMI by employing regression analyses on population survey data. Other recent studies predicting changes in BP, [9, 10] hemoglobin A1c (A1C) [11], cholesterol (LDL) [12], and SMK [13] utilized electronic health record (EHR) data. These studies employed machine learning algorithms such as classification tree, feature selection algorithms, and correlation analyses.
Recently, healthcare organizations have employed deep learning models to discover useful patterns from the EHR, which contain rich longitudinal healthcare information such as diagnoses, procedures, laboratory test results, and medications. Deep learning algorithms can be effectively used to predict certain medical events by capturing features and patterns contained in EHR data [14]. For example, scalable deep learning algorithms were applied in a previous study to accurately predict mortality and readmission in EHR data from two academic medical centers [15].
In this paper, we investigated the prediction of future CVH from previous measurements of CVH among patients utilizing one type of recurrent neural network (RNN) – long short-term memory (LSTM) networks [16]. LSTM is one type of architecture from recurrent neural network (RNN) which can capture temporal dynamic behavior from a temporal sequence. LSTM architecture is well-suited to predict time series with time lags of unknown size by learning from the previous experiences [17]. Unlike previous studies, we implemented LSTM techniques based on a large and nationally-representative longitudinal dataset of patients. We also compared LSTM models with other two baseline models, i.e., logistic regression (LR) and random forest (RF). The EHR data used for these analyses was from more than 70 outpatient clinics across the US. We included five CVH submetrics (i.e., SMK, BMI, A1C, LDL and BP) in our analyses due to data availability.
Our purpose was to better understand the CVH trajectory of patients and whether steps could be taken by providers and patients to maximize prevention efforts and the worsening of CVH. For example, if the CVH level was predicted to be worsening based upon the previous measures, then providers and patients could better maintain or control CVH to prevent it from becoming worse.
Methods
The Guideline Advantage (TGA) is an ambulatory quality clinical data registry of EHR data from more than 70 different clinics across the US. The American Cancer Society, the American Diabetes Association, and the AHA established TGA for tracking and monitoring disease management and outpatient preventative care (https://www.scripps.org/sparkle-assets/documents/heart_rhythm_facts.pdf). In this paper, we used TGA data to predict their most recent CVH status based on previous CVH data. Each future CVH submetric was defined as the most recent measurement for each patient, while the previous CVH submetrics comprised all preceding measurements.
We first identified the patients with at least one CVH metric with a result date within a 13-year period (2004–2016) of observation. Among these patients, 230,800 had SMK data, and 53,882 patients had measurements of hemoglobin A1c (A1C) measures, 114,235 cholesterol (low-density lipoprotein, LDL), 163,147 BMI, and 261,526 BP, respectively. We identified 216,445 patients with at least two measures at different dates in any CVH submetric (25,080 patients for A1C, 58,385 patients for LDL, 121,267 patients for BMI, 197,387 patients for BP, and 126,709 patients for SMK).
Each of the five CVH measures as defined above were classified into one of three categories according to Table 1: ideal, intermediate, or poor. We utilized the Multum drug database [19] as a template to convert all drug names to their corresponding drug class. We employed the Levenshtein distance algorithm [20] in the conversion process to compare drug names in our data set with those in the Multum drug database. Medications were considered as treatments for A1C, LDL, and BP only if the Levenshtein distance between compared strings was less than five.
All CVH data for each submetric were sorted in a time order as shown in Fig. 1, which illustrates the trajectory of A1C measurements for two random patients. The last CVH category in the series were marked as labels (i.e., ideal, intermediate, or poor A1C). We set each CVH submetric value as 2 for the ideal category, 1 for intermediate category, and 0 for poor category for each CVH submetric label. All of the preceding categorical measures were used as features.
We first conducted predictions for each CVH submetric category by LSTM as shown in Fig. 2.
Flowchart of our prediction by LSTM for each CVH submetric from each submetric measures. Here m = 1. Where m is the threshold of number of measures, A1C patients means all the patients who had A1C measures and also number of measures was more than m. The same definition was used for LDL, BMI, BP, and SMK patients
For each CVH submetric, we selected patients who had at least two measurements and then combined the submetric name with its category. For example, if a patient had a poor category for BMI, we combined the submetric name “bmi” and category “poor” as “bmipoor”. Then we mapped the resulting features to 32-dimensional vectors by a word embedding technique Word2Vec in our model, from which the resulting features (e.g., bmipoor) were all denoted by numerical vectors. The Genism Word2Vec model was configured the hyperparameters as following: size (embedding dimension) as 32, window (the maximum distance between a target word and all words around it) as 5, min_count (the minimum number of words counted when training the model) as 1, sg (the training algorithm) as CBOW (The continues bag of words). We also added time information for all measurements as time steps. Each feature was associated with a time point which was calculated by the difference in days between the corresponding visit time and the latest measurement time. Sex and age information were also added for all patients. The input length was the maximum count of measures among patients in each prediction case. Thus, each patient was represented by a numerical embedding vector. Next, these embedding vectors were fed to a LSTM model. For each submetric, the dataset was randomly split into training dataset (80%) and testing dataset (20%). We used the area under the receiver operator curve (AUC) to evaluate the performance of the LSTM model.
We then applied the same methodology to patients who had at least two measures for each CVH submetric. For this patient subpopulation, we performed two types of predictions: one in which we used only one CVH submetric to predict future values for that category, and the other in which we used all 5 CVH submetrics to predict the 5 future submetrics by multi-label classification and multiclass classification approaches. Criterion of AUC and accuracy were utilized to evaluate the performance of the two types of predictions. Finally, we evaluated the difference in performance for these two types of predictions.
For predictions using all 5 CVH submetric measures, we listed AUC and accuracy for the multilabel classification approach which was designed to predict all 15 classes (5 submetrics × 3 classes each, method 1) and a multiclass classification approach was used to predict all 3 classes of each CVH submetric in which we repeated the analysis 5 times (method 2). We applied another prediction using only one CVH submetric to predict future values for that category. For each subpopulation, we trained our model using 7855 patient samples, and validated the model on 1964 samples. We listed accuracy as the ability to predict correctly for each case as equally important.
To compare the performance of the above methods, we investigated the correlations between the latest status of each of the 5 CVH submetrics. The three levels of each submetric were represented as numerical values (0, 1, 2) corresponding to CVH levels of poor, intermediate, and ideal. All patients were assigned numerical CVH levels for their 5 CVH submetrics. For example, if a patient had ideal A1C, intermediate LDL, poor BMI, poor BP, and ideal SMK, then the levels of the 5 CVH submetrics were represented as 2, 1, 0, 0, and 2. The Pearson’s correlation coefficients were calculated to evaluate correlations between these 5 CVH submetrics.
Our LSTM model was comprised of an input layer, one hidden layer (with 100 dimensions) and an output layer. A categorical cross-entropy loss function was employed as the output layer and a sigmoid function was used as the activation function for the hidden layer. Adam optimizer [21] was used to optimize the model with a mini-batch size of 64 samples. We did an extensive hyperparameter search for activation functions (i.e., Sigmoid, tanh, SeLU and ReLU), as well as the embedding dimensions of 32 or 64. We did not extensively search other hyperparameters such as number of LSTM layers, number of recurrent units, or batch size, as these hyperparameters were of minor importance upon initial investigation [22].
We also compared LSTM models with two baseline models: logistic regression (LR) and random forest (RF). The logistic regression model was configured as follows: the L2 norm was used in the penalization, i.e., the variance of predicted value and real value of training data; the stopping criteria was set as 1.0*10–4; the inverse of regularization strength, which reduces the potential overfitting, was set as 1.0. The RF model was configured as follows: the number of trees in the random forest was set 100; the number of maximum features can be used in each tree was set as the square root of the total number of features; the minimum number of samples at a leaf node of a tree was set as 1. Analyses were conducted by using the libraries of Scikit-learn, Scipy, and Matplotlib with Python, version 3.6.5 in 2019.
Results
Table 2 shows characteristics of our overall study population and of the subpopulation of patients with multiple measurements for each of the 5 submetrics. The overall population contained approximately 56% females and 48% white race with an average age of 45 years. For the overall population, the average values of CVH submetrics were as follows: A1C was 7.2%, LDL was 107 mg/dL, BMI was 28.5 kg/m2, systolic BP was 123 mmHg and diastolic BP was 73 mmHg. Around 16% patients were current smokers. The subpopulation was older (58 years), and BMI and BP were higher compared to the overall population.
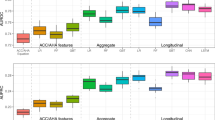
Figure 3 displays the performance of the LSTM models for each CVH submetric prediction. The AUC for the A1C category prediction using all measures was 0.21 for ideal category, 0.83 for intermediate category, and 0.93 for poor category; the micro-average and macro-average of AUC for A1C prediction was 0.91 and 0.89, respectively (Fig. 3a). Similarly, the micro-average and macro-average AUC for LDL prediction was 0.93 and 0.82 (0.97 and 0.97 for BMI, 0.84 and 0.81 for BP, 0.99 and 0.93 for SMK). The values of AUC for LDL predictions for ideal, intermediate, and poor categories were 0.81, 0.77 and 0.86 (0.98, 0.94 and 0.98 for BMI, 0.85, 0.73 and 0.85 for BP, 0.94, 0.87 and 0.96 for SMK), respectively (Fig. 3b–e). Additional file 1: Figure S1 and Additional file 2: S2 (in the supplementary material section) displays the performance of LR and RF by ROC curves for each submetric.
Table 3 lists other additional metrics, i.e., overall accuracy, precision, recall, and F1-score, to evaluate performance for LSTM, LR, and RF models. The results showed that LR performed better than RF in all cases, and LSTM performed the best in all the cases.
Table 4 lists the AUC and accuracy for the prediction of future CVH by LSTM models by using all five submetric measures and single CVH submetrics as predictors for the subpopulation.
Table 4 showed that AUC and accuracy values remained almost the same as predictions using all 5 CVH submetrics compared to only using data from a single CVH submetric. There were some differences between methodologies. For accuracy values for multi-label classification (Method 1), which predicted all 15 classes at one time, the model calculated an overall optimal score while ignoring some classes. As a result, there were some low values of accuracy which resulted from this method; for example, accuracy of predicting poor A1C was 50.7%.
Figure 4 lists the correlations between the latest status of each of the 5 CVH submetrics. The calculated values were Pearson’s correlation coefficients. Higher absolute values indicated stronger associations between variables. The correlation coefficient between A1C and BP was 0.1, 0.083 for A1C and BMI, and 0.074 for BMI and BP.
Discussion
In this study, we employed a RNN model – an LSTM model – to predict CVH measure categories in each submetric using 14-year longitudinal CVH measures from the EHR of more than 70 different outpatient clinics. We also studied a subpopulation of patients who had at least two measures for each CVH submetric to predict the CVH submetric measure categories using data from a single submetric data versus all 5 submetrics employing multi-label and multiclass classification techniques.
The comparison of LSTM models to two baseline models (i.e., LR and RF) indicated that LSTM models outperformed the other models. Our results indicated that CVH measure categories can be accurately predicted by previous CVH measures for that metric with LSTM models. BMI, SMK, A1C, and LDL predictions and all their corresponding micro-average AUC values were greater than 0.90. The micro-average AUC value for BP prediction was lower (0.84), which might result from the measurement variability of BP inhereherin EHR data.
We used all previous trajectories of a given CVH submetric to predict the most recent value for that submetric. We also used all available CVH submetrics to predict the most recent value for a given submetric considering there might be associations between different submetrics. Our results indicated that combining all CVH submetrics did not improve the prediction performance. Thus, the focus of our study was to predict one CVH submetric according to trajectories of the same submetric. In our subpopulation analyses, the criterion of AUC and accuracy were not improved by using all 5 CVH submetrics compared to data from a single submetric. One reason for this finding may be due to the low correlations between these 5 submetric labels.
One key strength of our study was the use of the TGA dataset which was a large and nationally representative longitudinal EHR dataset. The contribution of this study was the first to investigate the predictions of future CVH from all previous CVH measures by deep learning approaches using TGA longitudinal EHR data. We acknowledge that the conversion of numerical variables into categories may result in information loss, therefore our future work would focus on using the numerical values to predict the three classes.
LSTM models can effectively predict CVH trajectories of patients on a large ambulatory population. It is crucial to predict future changes in CVH to better manage CVH of patients. For example, if the A1C level was predicted to be worsening based upon the previous measures, then providers and patients could better maintain or control A1C to prevent it from becoming worse. Therefore, predicting future CVH could improve the health and quality of life of patients. Ideal CVH measures were associated with lower incidence of CVD and cancers [6, 23,24,25,26,27,28]. Thus, predicting future levels of CVH might indirectly decrease the cost and burden on the health system caused by CVD and cancers.
Limitations
A limitation in our analyses was that our results were based on the TGA data source, which is large and more representative, thus it might yield to different results on other data source.
Conclusions
We found that LSTM models can be effective at accurately predicting CVH measure categories in each submetric from the time-series CVH measures. The performance was not improved by using all 5 CVH submetric measures compare to using single submetric measures in the subpopulation. Predicting patients’ future CVH levels might increase patient CVH health and indirectly improve quality of life for patients and decrease the burden and cost for clinical health system caused by CVD and cancers. These findings have important implications for predicting trajectories of CVH in a patient population. Future research should work towards identifying optimal time to intervene on future CVH values.
Availability of data and materials
The datasets belong to a third-party and the authors do not have permission to share the data. Researchers need to apply from American heart association for the access to the datasets.
Abbreviations
- CVD:
-
Cardiovascular disease
- CVH:
-
Cardiovascular health
- EHR:
-
Electronic health records
- TGA:
-
The Guideline Advantage
- SMK:
-
Smoking status
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- A1C:
-
Hemoglobin A1c
- LDL:
-
Low-density lipoprotein
- LSTM:
-
Long short-term memory
- AUROC:
-
Area under the receiver operator curve
- AHA:
-
American heart association
- RNN:
-
Recurrent neural networks
- LR:
-
Logistic regression
- RF:
-
Random forest
- AUC:
-
Area under curve
References
Jin Y, Tanaka T, Banduneli S, Takegawkar SA. Overall cardiovascular health is associated with all-cause and cardiovascular disease mortality among older community-dwelling men and women. J Aging Health. 2017;29(3):437–53.
AHA. In: Association AH, editor. Life’s simple 7; 2013. http://mylifecheck.heart.org/.
Yang Q, Cogswell ME, Flanders W, et al. TRends in cardiovascular health metrics and associations with all-cause and cvd mortality among us adults. JAMA. 2012;307(12):1273–83. https://doi.org/10.1001/jama.2012.339.
Artero EG, España-Romero V, Lee D, et al. Ideal cardiovascular health and mortality: aerobics center longitudinal study. Mayo Clin Proc. 2012;87(10):944–52. https://doi.org/10.1016/j.mayocp.2012.07.015.
Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD. Community prevalence of ideal cardiovascular health, by the American heart association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011. https://doi.org/10.1016/j.jacc.2010.11.041.
Foraker RE, Abdel-Rasoul M, Kuller LH, et al. Cardiovascular health and incident cardiovascular disease and cancer: The Women’s Health Initiative. Am J Prev Med. 2016;50(2):236–40.
Haby MM, Markwick A, Peeters A, Shaw J, Vos T. Future predictions of body mass index and overweight prevalence in Australia, 20052025. Health Promot Int. 2012. https://doi.org/10.1093/heapro/dar036.
Mead E, Batterham AM, Atkinson G, Ells LJ. Predicting future weight status from measurements made in early childhood: a novel longitudinal approach applied to millennium cohort study data. Nutr Diabetes. 2016. https://doi.org/10.1038/nutd.2016.3.
Solomon JW, Nielsen RD. Predicting changes in systolic blood pressure using longitudinal patient records. J Biomed Inform. 2015. https://doi.org/10.1016/j.jbi.2015.06.024.
Golino HF, Amaral LS de B, Duarte SFP, et al. Predicting increased blood pressure using machine learning. J Obes. 2014. https://doi.org/10.1155/2014/637635.
Koga M, Murai J, Saito H, Kasayama S. Prediction of near-future glycated hemoglobin levels using glycated albumin levels before and after treatment for diabetes. J Diabetes Investig. 2011. https://doi.org/10.1111/j.2040-1124.2011.00107.x.
Garber AM, Olshen RA, Zhang H, Venkatraman ES. Predicting high-risk cholesterol levels. Int Stat Rev. 1994;62(2):203–28.
Mendel JR, Berg CJ, Windle RC, Windle M. Predicting young adulthood smoking among adolescent smokers and nonsmokers. Am J Health Behav. 2012. https://doi.org/10.5993/AJHB.36.4.11.
Goodfellow I, Bengio Y, Courville A. Deep learning; 2016. https://doi.org/10.1533/9780857099440.59.
Rajkomar A, Oren E, Chen K, et al. Scalable and accurate deep learning with electronic health records. NPJ Digit Med. 2018;1(1):18. https://doi.org/10.1038/s41746-018-0029-1.
Hochreiter S& S. Long short-term memory. Neural Comput. 1997;9:1735–80.
Azzouni A, Pujolle G. NeuTM: a neural network-based framework for traffic matrix prediction in SDN. In: IEEE/IFIP network operations and management symposium: cognitive management in a cyber world, NOMS 2018; 2018. https://doi.org/10.1109/NOMS.2018.8406199.
Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction. Circulation. 2010;121(4):586–613. https://doi.org/10.1161/circulationaha.109.192703.
Shickel B, Tighe PJ, Bihorac A, Rashidi P. Deep EHR: a survey of recent advances in deep learning techniques for electronic health record (EHR) analysis. IEEE J Biomed Heal Informatics. 2018. https://doi.org/10.1109/JBHI.2017.2767063.
Levenshtein VI. Binary codes capable of correcting deletions, insertions, and reversals. Sov Phys Dokl. 1966;10:707–10 doi:citeulike-article-id:311174.
Kingma DP, Ba J. ADAM: a method for stochastic optimization. CoRR. 2015; abs/1412.6.
Reimers N, Gurevych I. Optimal hyperparameters for deep LSTM-networks for sequence labeling tasks. arXiv. 2017; abs/1707.0.
Wang YQ, Wang CF, Zhu L, Yuan H, Wu LX, Chen ZH. Ideal cardiovascular health and the subclinical impairments of cardiovascular diseases: a cross-sectional study in central South China. BMC Cardiovasc Disord. 2017. https://doi.org/10.1186/s12872-017-0697-9.
Younus A, Aneni EC, Spatz ES, et al. A systematic review of the prevalence and outcomes of ideal cardiovascular health in US and Non-US Populations. Mayo Clin Proc. 2016. https://doi.org/10.1016/j.mayocp.2016.01.019.
Fang N, Jiang M, Fan Y. Ideal cardiovascular health metrics and risk of cardiovascular disease or mortality: a meta-analysis. Int J Cardiol. 2016. https://doi.org/10.1016/j.ijcard.2016.03.210.
Wang J, Shao B, Lin D, et al. Ideal cardiovascular health metrics associated with reductions in the risk of extracranial carotid artery stenosis: a population-based cohort study. Sci Rep. 2018. https://doi.org/10.1038/s41598-018-29754-3.
Ogunmoroti O, Allen NB, Cushman M, et al. Association between life’s simple 7 and noncardiovascular disease: the multi-ethnic study of atherosclerosis. J Am Heart Assoc. 2016. https://doi.org/10.1161/JAHA.116.003954.
Polonsky TS, Ning H, Daviglus ML, et al. Association of cardiovascular health with subclinical disease and incident events: the multi-ethnic study of atherosclerosis. J Am Heart Assoc. 2017;6(3):e004894. https://doi.org/10.1161/JAHA.116.004894.
Acknowledgements
None.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
R.F. contributed to the study design. A.G. conducted the analysis and wrote the manuscript. R.B., Y.K. and J.L. provided insightful discussions, reviewed the results and revised the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The need for informed consent for this study was waived and approved by the Institutional Review Board at the Washington University School of Medicine in St. Louis. We obtained a written acknowledgement of proprietary rights and non-disclosure and data use agreement from the American Heart Association (The Washington University_NDA_DUA_CONTRACTID 158065_2019.04.26_K).
Consent for publication
Not applicable.
Competing interests
There are no competing interests for A.G., R.B., Y.K., and J.L. R.F. is an editorial board member for the journal.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1
. The area under the curve (AUC) for predictions regarding 5 CVH submetrics by LR models. Figure (A) shows the prediction for A1C according to all the previous A1C measures, and (B)-(E) were for LDL, BMI, BP, and SMK predictions, respectively.
Additional file 2: Figure S2
. The area under the curve (AUC) for predictions regarding 5 CVH submetrics by RF models. Figure (A) shows the prediction for A1C according to all the previous A1C measures, and (B)-(E) were for LDL, BMI, BP, and SMK predictions, respectively.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Guo, ., Beheshti, R., Khan, Y.M. et al. Predicting cardiovascular health trajectories in time-series electronic health records with LSTM models. BMC Med Inform Decis Mak 21, 5 (2021). https://doi.org/10.1186/s12911-020-01345-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12911-020-01345-1