Abstract
Background
Head and Neck Squamous Cell Carcinoma (HNSCC) has a high incidence in elderly patients. The postoperative complications present great challenges within treatment and they're hard for early warning.
Methods
Data from 525 patients diagnosed with HNSCC including a training set (n = 513) and an external testing set (n = 12) in our institution between 2006 and 2011 was collected. Variables involved are general demographic characteristics, complications, disease and treatment given. Five data mining algorithms were firstly exploited to construct predictive models in the training set. Subsequently, cross-validation was used to compare the different performance of these models and the best data mining algorithm model was then selected to perform the prediction in an external testing set.
Results
Data from 513 patients (age > 60 y) with HNSCC in a training set was included while 44 variables were selected (P < 0.05). Five predictive models were constructed; the model with 44 variables based on the Random Forest algorithm demonstrated the best accuracy (89.084 %) and the best AUC value (0.949). In an external testing set, the accuracy (83.333 %) and the AUC value (0.781) were obtained by using the random forest algorithm model.
Conclusions
Data mining should be a promising approach used for elderly patients with HNSCC to predict the probability of postoperative complications. Our results highlighted the potential of computational prediction of postoperative complications in elderly patients with HNSCC by using the random forest algorithm model.
Similar content being viewed by others
Background
Head and neck carcinoma (HNC) represents the sixth most common cancer worldwide [1], and squamous cell carcinoma (SCC) is the most common type of HNC. Surgery is regarded as one of the most effective treatments for HNSCC [1]. However, the postoperative complications present serious challenges for every surgeon in the management of patients with HNSCC, especially for elderly patients.
Many aspects contribute to the high risk of postoperative complications for elderly patients with HNSCC, but in general, it has been reported that patients over the age of 70 are more likely to experience postoperative complications [2] than younger patients. Poor physical health and poor living habits also confer a disadvantage, and Warner et al. contended that nonsmokers who undergo Coronary Artery Bypass Grafting (CABG) have a 66 % reduction in the risk for postoperative complications in the lung compared with smokers [3]. Cardiovascular complications are also significant causes of postoperative morbidity and mortality in patients undergoing surgery [4]. Co-morbidities are considered prognostic factors in studies of the benefit quality and the effectiveness of care where postoperative complications are the focus of discussion [5].
The following characteristics of treatment, especially the surgeries that are performed, are also influential factors for patients: the duration, the scale and the level of surgical operations. Fleisher et al. have found that patients who are ASA III and IV according to the American Society of Anesthesiologist, have a death rate of 13 and 26 % respectively [6].
The most widely used systems for predicting potential postoperative complications are the Acute Physiology and Chronic Health Evaluation II system (APACHE II) [7], the Physiological and Operative Severity Score for Enumeration of Mortality and Morbidity system (POSSUM) [8], and the American Society of Anesthesiologists (ASA) Physical Status Classification [9]. There are shortcomings in the aforementioned systems, such as the absence of choice for a surgical procedure, length of the procedure, a lack of a description of the surgical procedure, a lack of attention to the nutrition condition of the patients as well as the physiological state of the cardiovascular system.
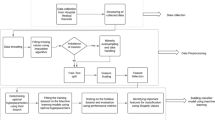
Due to the development of computational technology, Data Mining (DM) now plays an important role in medical data analysis and modeling [10]. In the process of data mining, three steps should be performed to recognize the rules and patterns among these enormous data sets: 1) Data preparation—collect the data under established inclusion criteria; 2) Data modeling and mining—find the logistic relationships among the data with the use of data mining algorithms; and 3) Results analysis—verify the data mining results to see whether they meet the needs of the study and whether the results are accurate and reliable [11]. Thus far, data mining has been widely used in the medical assessment of various cancer types. For instance, Roberta et al. found 40 genes that are up-regulated in HNSCC using ORESTES data mining analysis [12]. Zainab Abu Bakar et al. constructed a framework for the diagnosis of the tumor stage of primary oral cancer by using data mining of Bayesian reasoning [13].
However, there is lack of computational models that can be used to predict the postoperative complications that may occur in elderly patients with HNSCC. More specifically, there are rarely studies for Data Mining algorithm modelling of postoperative complications with HNSCC. In order to bridge the gap efficiently, three specific aims of the study have been proposed: 1) to design and implement a retrospective cohort study and enroll a sample of elderly patients with HNSCC; 2) to adapt data mining protocols to the study; and 3) to construct predictive models for the postoperative complications based on data mining, to check the reliability of those models and to select the optimal model for predicting postoperative complications in elderly HNSCC patients.
Methods
Patients’ data collection
This study had gained ethical approval from the department of Oral and Maxillofacial-Head Neck Oncology at the Affiliated Ninth People’s Hospital School of Medicine, Shanghai Jiao Tong University; The patients’ data were analyzed and collected from the medical records that were documented in the department above; Total 525 patients diagnosed with HNSCC including a training set (n = 513) and an external test set (n = 12) in our institution between 2006 and 2011 was recruited. The inclusion criteria are: 1) patients older than 60 years; 2) have a pathologically confirmed diagnosis of HNSCC; 3) have no history of other types of tumors; 4) undergo surgery with general anesthesia; and 5) undergo surgery with a curative intent that involved regions within the head and neck. Patients who underwent 1) surgery for benign tumors; 2) surgery for minor procedures with local anesthesia, such as biopsies; and 3) surgery with a duration that was shorter than 30 min were excluded from the study.
Variable selection
For variable selection, the variables within two operative severity scoring systems were adopted: Acute Physiology and Chronic Health Evaluation II (APACHE II) 7, and Physiological and Operative Severity Score for the enumeration of mortality and morbidity (POSSUM) [8]. Moreover, the variables of the types of surgery and the general condition were further selected through clinical knowledge and experience, and the variables related to poor living habits were evaluated by an SPSS toolkit (P < 0.05).
With respect to surgical procedures, as well as the standards of POSSUM score system, the types of surgery were classified into three groups: 1) Minor Operation (MO), primary closure of wounds without neck dissection; 2) Intermediate Operation (IO), primary closure of wounds with unilateral neck dissection; 3) Major operation (JO), primary closure of wounds with bilateral neck dissection or simultaneous flap repair. 4) Superior Major Operation (SMO), primary closure of wounds with bilateral neck dissection and simultaneous flap repair (using microsurgical vascular anastomosis).
Although all the variables are selected from the two operative severity scoring systems which are well accepted worldwide, our study also calculated the information gain (IG) for each variable to determine its effectiveness in a classification system. As listed in Table 1, most scores are very consistent with the clinical experience. Yet, few variables have low IG, which doesn't mean these variables are not important for classification results. For example, IG for rectal temperature is 0.01, but the variable is well used in the general surgery while our study focused on the region of head and neck. From our clinical experience, it still has potential relationship with postoperative complications. The effectiveness of such variables are not as much as the others, but none of them should be deleted.
Postoperative complications selection
The following postoperative complications were selected from the Adult Comorbidity Evaluation-27 (ACE-27) [14]. The other postoperative complications were selected through clinical experiences, especially for the flap reconstruction and tracheotomy as well as for the need of behavior management: infection (wound infection and free flap infection), edema, wound dehiscence, hematoma (with or without re-exploration), free flap necrosis (partial and total), respiratory disorder (pneumonia and pulmonary infarct), salivary fistula, gastrointestinal disorder (abdominal discomfort and hematemesis), deep vein thromphlebitis, angina, and delirium.
Algorithms for data mining
Five data mining algorithms were exploited in this study: Bayes Net, Naïve Bayes (NB) Net, Support Vector Machine (SVM), Random Forest (RF), and Rotation Forest (ROF) [15-17]. The Naïve Bayes (NB) Net, which is based on Bayes’ theorem, is known as the simplest probabilistic classifier with an assumption that there is no coupling relation between variable spaces. Support Vector Machine (SVM) is a machine learning approach that is based on the structural risk minimization principle of statistics learning theory that is applied in many complicated modeling problems; the decision tree algorithm demonstrates a tree-like graph or model of decisions and their possible consequences, where the sequence of a node is determined by the information entropy of the corresponding node because these variables are mapped to tree nodes in advance. The Random Forest (RF) and Rotation Forest (ROF) algorithms are two improved versions of the decision tree algorithm. In our study, all of the above data mining algorithms were used to construct the predictive models through software Orange 2.7.2 (Version 2.7.2, freely available at http://www.ailab.si/orange/).
Validation of predictive models and variables
Before a predictive model is constructed, its validity and reliability must be evaluated. The N-fold-cross-validation is a effectively optimal parameter selection tool for model construction and popular measurement tool for model evaluation. Firstly, each sub-dataset in the entire training dataset is singled out, in turn, as the testing sample followed by the remaining N-1 sub-datasets that constitute the new training dataset; this workflow continues until all of the sub-datasets in the complete training dataset are traversed. In this study, N is set to different values such as 3, 5, 10 or more extremely, N = 513 (leave-one-out cross-validation). Subsequently, the complete training dataset have been divided into N parts and then optimal model parameters have been selected from grid search based on model performance comparison. It is found that when N > =5, the optimal model parameters from grid search approximately keep consistent, which means that model optimization iterative process has stable convergence. Therefore, N was set to five and the Receiver Operating Characteristic (ROC) and the area under the ROC curve (AUC) were adapted to check the performance of all five predictive models. In the study, the collected data were subjected to analysis using SPSS (SPSS17.0) and the level of statistical significance was set at 5 % (P < 0.05). Furthermore, univariate analysis was performed firstly with the f-test and t-test for all selected variables; only the significant variables according to the analysis were included.
Results
Patient’s data from two independent sets were collected
In training set, Of the 513 patients, 52.0 % were men, and 48.0 % were women. The mean age of the sample was 71.0 years, while the age range was 61–101 years. Clinicopathological characteristic of the patients were listed in Table 2.
A total of 173 patients were found to have co-morbidities: 45.7 % (45: high blood pressure, 34: myocardial infarction) were diagnosed with cardiovascular disorder, 13.9 % (11 chronic obstructive pulmonary disease COPD, 13 bronchitis) were diagnosed with respiratory disorder, 25.4 % (31 diabetes, 10 hypothyroidism, 3 hyperthyroidism) were diagnosed with endocrine disorder, 4.6 % (5 agitatian, 3 delirium) neurological disorders, 6.9 % (6 metabolism, 6 acid reflux) had disorder of the GI, 3.5 % (6 renal failure) had urological disorder.
Most patients were treated for primary tumors (66.7 %), while the remaining patients were treated for recurrence (33.3 %). Approximately 56.2 % of the patients who were treated for primary OSCC had tumors in stage I or II, in detail were that: the tumor staging results were as follows: 148 in stage I, 262 in stage II, 113 in stage III, and 47 in unidentified.
According to the standards established by the American Joint Committee on Cancer (AJCC), the distribution results of the Tumor-Node-Metastasis criteria (TNM) [18] showed that 28.2 % of tumors were classified as T1 to T4. According to the gold standard for pathological analysis (H&E-stained tissue specimens and accompanying immunohistochemistry) [19]. And the final results were that: 148 in T1, 179 in T2, 47 in T3, and 139 in T4.
The main regions of HNSCC were as follows: 20 were in the lips (15 in lower lip, 5 in upper lip), 17 were in the maxillofacial region, 33 were in the floor of mouth, 122 were in tongue, 12 were in oral-pharyngeal, 12 were in hypopharynx, 49 were in neck, 52 were in the maxilla while 123 were in mandible, 65 were in buccal mucosa, the rest 6 were in the parotid gland. The classifications of the surgical operations were as follows: 149 in IO, 261 in JO, and 103 in SMO. Among the patients, 292 experienced postoperative complications.
The distribution of the postoperative complications (n = 292) were as follows: 58 had infections (35 wound infections, 23 free flap infection), 46 had edema (all in surgical region), 40 experienced wound dehiscence, 25 had hematoma (15 hematoma with re-exploration, 10 hematoma without re-exploration), 21 had flap necrosis (17 partial flap necrosis, 4 total flap necrosis), 20 respiratory disorder (19 pneumonia, 1 pulmonary embolus), 16 had a salivary fistula, 9 had gastrointestinal disorders (5 abdominal discomfort, 4 hematemesis), 8 had a central nervous system co-morbidity, 7 had a deep venous thrombosis (DVT) of the lower extremities, 6 had angina, and 8 had delirium. Detailed clinicopathological parameters of the external test set were summarized in Table 3.
Variable were further selected according to POSSUM system, APACHE II system and clinical experience
According to the POSSUM system, 18 variables were selected: age, cardiac function, respiratory function, ECG results, systolic blood pressure (BP), pulse rate, hemoglobin levels, white blood cell (WBC) count, levels of blood urea nitrogen, sodium and potassium, Glasgow coma scale (GCS), operation type, number of procedures, operative blood loss, peritoneal contamination, malignancy, and Confidential Enquiry into Perioperative Deaths (CEPOD). With regards to the APACHE II system, nine variables were considered: rectal temperature, mean arterial pressure, blood pH, heart rate, respiratory function, levels of sodium, potassium and creatinine, hematocrit.
The following 17 “new variables” were chosen through clinical experiences and were evaluated by an SPSS17.0 toolkit: preoperative WBC, preoperative blood urea, diameter of the tumor, the amount of blood loss, operation time, hematocrit of postoperative day 1 (POD1), glucose of POD1, the chronic diseases, smoking, alcoholism, preoperative radiotherapy, preoperative chemotherapy, preoperative surgery, primary/recurrence of tumor, surgery classification, clinical grading, and pathological grading.
The 17 new variables were classified into the following 4 parameters: the preoperative variables, the operative variables, the postoperative variables, and the other variables. All of the above variables were classified into 4 tables: the preoperative variables are listed in Table 4, the operative variables are listed in Table 5, the postoperative variables are listed in Table 6, and the other variables are listed in Table 7.
With the above variables, 4 types of variable systems were formed: the “POSSUM Variable” system, the “APACHE II Variable” system, the “NEW Variable” system, and the “All (All = POSSUM + APACHE + NEW) Variable” system.
The accuracy and reliability of each predictive model were evaluated under 4 different “All Variable” systems
In this study, five different data mining algorithms were used to construct predictive models. Eventually, five predictive models based optimal parameters selection were successfully constructed. Also it has been validated that the accuracy of each predictive model under four different variable systems. The performance of each predictive model is listed in Table 8. According to Table 8, each predictive model had the best accuracy under the “All variable” system. In addition, the predictive model that was based on the Random Forest algorithm had the best accuracy (89.084 %). Since the comparison among accuracy of each predictive model under the “All Variable” system was not comprehensively enough, it was necessary to know the reliability of each model under the “All Variable” system. The ROC curve was adapted to detect the difference in the reliability of the sensitivity of each predictive model under the “All Variable” system. The ROC of each predictive model under the “All Variable” system is shown in Fig. 1. The difference between each area under the curve (AUC) is shown in Table 9, which suggests that the predictive model based on the Random Forest algorithm generated the best AUC value of 0.949, which in turn, indicates the greatest reliability. Accordingly, It is verified that the difference performance among these data mining algorithms may come from the following reasons: random forest algorithm is one of the strongest algorithm in the classification problems, and moreover, these clinical data naturally have the distribution suitable for decision tree modeling, which is the basis model of random forest algorithm.
There are 5 ROC curves that illustrate the reliability of the predictive models based on 5 data mining algorithms under the “All Variable” system. The light blue curve signifies the predictive model based on the Random Forest algorithm, which has the largest AUC value. All AUC values are shown in Table 9. SVM = Support Vector Machine
The accuracy and reliability of the Random Forest algorithm model were among the best and tested in an external testing set
Our findings show that the predictive model based on the Random Forest algorithm under the “All Variable” system generated the best accuracy as well as the best reliability in the training set (n = 513). Furthermore, the performance of the Random Forest algorithm model was calculated under all 4 different variable systems. In Fig. 2, the ROC of the predictive model under the 4 different variable systems is shown. And the AUC values for Fig. 2 are listed in Table 10, which shows that the predictive model based on the Random Forest algorithm under the “All Variable” system, had the largest AUC value (0.949). This means that the Random Forest algorithm model under the “All Variable” system still produce the best reliability. In order to further test the accuracy and reliability of the Random Forest algorithm model under the “All Variable” system, an external test set (n = 12) was incorporated into the study, our results demonstrated that the model gave a Performance (accuracy = 83.333 % and the AUC value = 0.781), which was also showed in Table 11.
There are 4 ROC curves that illustrate the reliability of the predictive models based on the Random Forest algorithm under 4 different variable systems. The light blue curve signifies the predictive model based on the Random Forest algorithm under the “All Variable” system, which has the largest AUC value. All AUC values are shown in Table 10. All=”All Variable” system, New=”New Variable” system, Pos=”POSSUM Variable” system, Apa=”APACHE II Variable” system, RF = Random Forest algorithm
Even if there are rarely algorithm analysis references for the study of postoperative complications with HNSCC, the obtained prediction result (83.333 %) is also a promising result compared to algorithm results from similar clinical data modeling, which bridge the gap between clinical data and advanced algorithm modeling.
Discussion
The increase in life expectancy has resulted in an increasing number of malignant neoplasms in the elderly population [20]. Most head and neck squamous cell carcinoma (HNSCC) commonly arises between the fifth and seventh decades of life; therefore, their occurrence in the elderly population is not uncommon [20]. Surgery and/or radiotherapy are the primary locoregional treatment modalities [21] and are often followed by chemotherapy [22]. The postoperative complications are among the most difficult factors in the surgical management of elderly patients with HNSCC. HNSCC in elderly patients should be treated with curative intention [23]. In this study, the authors emphasize the importance of the prediction of postoperative complications.
Postoperative complications that occur within the first 24 h during or following surgery are regarded as early, and those that occur within the 2-week postoperative period are considered delayed [24]. Some postoperative complications with a high rate of occurrence that may elicit serious effects are as follows: 1) pulmonary embolus, diagnosed by a high-probability nuclear ventilation-perfusion scan or by pulmonary angiography, is a common complication that may also cause venous thromboembolism [24], and 2) a morbidity within the central nervous system, which is defined as a newly documented cerebrovascular accident, transient or reversible neurologic deficit, or neurologic deficits of any origin, including those related to ethanol withdrawal [24]. These may lead to the failure of behavior management, which has been a negative factor for the treatment of free flaps, possibly causing flap necrosis. 3) Infections of the wound and flap caused by the invasion of bacteria or foreign bodies to the wound or flap may be detected after a blood analysis; this is especially true after a WBC count, which can help determine the causes of fever and of the necrosis of the free flap or skin graft. 4) Deep venous thrombosis of the lower extremities, which is recognized as a cause of both pulmonary embolism (PE) and of post thrombotic syndrome [25], may cause sudden death in this patient population. Edema, wound dehiscence, hematoma under the skin, flap necrosis, salivary fistula, gastrointestinal disorders, and angina pectoris are also among the most common postoperative complications.
As a result, 5 different data mining algorithms were exploited to construct predictive models. It had also been validated that the accuracy of predictive model under four different variable systems. The predictive models based on the random forest, the rotation forest, and the support vector machine algorithms are the most accurate under the “All Variable” system (89.084, 85.965, and 83.431 %, respectively). Additionally, the random forest algorithm was regarded as the most suitable algorithm model in this study. The reliability of each model under the “All Variable” system was obtained through the ROC curve, then each area under curve (AUC) was also calculated; Subsequently the predictive model based on the Random Forest algorithm had the largest AUC value of 0.949, which suggested the best reliability. Furthermore, the performance of the random forest algorithm model was verified in an external testing set (accuracy = 83.333 % and the AUC value = 0.781).
Based on the results, there are some weaknesses and challenges in the study. First, our study is limited by its reliance on data from a single hospital, and thus the number of patients is small. Second, the study lacks input variables for patient variables, such as exercise behavior, nutrition, stress, and depression. Third, the quality may be impacted because the number of non-postoperative complication group was higher than the postoperative complication group. Finally, for data mining, the quantity and quality of the data are so important. Therefore, a multi-center study including more variables for prediction of postoperative complications by using the random forest algorithm model warrants further investigation.
In this study, for the first time, we demonstrated that the potential of computational prediction model of postoperative complications in elderly patients with HNSCC was founded by using data mining approach. The random forest algorithm model generated the best accuracy (89.084 %) and the best reliability (AUC = 0.781) in a training set, which was further verified in an external testing set (83.333 % and AUC = 0.781), suggesting the random forest algorithm would be a promising prediction model for postoperative complications in elderly patients with HNSCC.
Conclusions
Data mining (DM) techniques allow the possibility of statistically predicting postoperative complications in elderly patients with HNSCC. In the study, the Random Forest algorithm model provides a promising approach with the best accuracy (89.084 %) and the best AUC value (0.949). This was further verified in an external testing set, with a good accuracy (83.333 %) and the AUC value (0.781).
References
Malfertheiner P, Megraud F, O'Morain C, Bazzoli F, El‐Omar E, Graham D, Hunt R, Rokkas T, Vakil N, Kuipers EJ. Current concepts in the management of Helicobacter pylori infection: the Maastricht III Consensus Report. Gut. 2007;56:772–81.
Knott-Craig CJ, Danielson GK, Schaff HV, Puga FJ, Weaver AL, Driscoll DD. The modified Fontan operation: an analysis of risk factors for early postoperative death or takedown in 702 consecutive patients from one institution. J Thorac Cardiovasc Surg. 1995;109(6):1237–43.
Warner DO. Preventing postoperative pulmonary complications: the role of the anesthesiologist. Anesthesiology. 2000;92:1467–72.
Poldermans D, Boersma E, Bax JJ, Thomson IR, van de Ven LL, Blankensteijn JD, Baars HF, Yo T, Trocino G, Vigna C, Roelandt JRTC, Fioretti PM, Paelinck B, van Urk H. The effect of bisoprolol on perioperative mortality and myocardial infarction in high-risk patients undergoing vascular surgery. N Engl J Med. 1999;341:1789–394.
Greenfield S, Apolone G, McNeil BJ, Cleary PD. The importance of co-existent disease in the occurrence of postoperative complications and one-year recovery in patients undergoing total hip replacement: comorbidity and outcomes after hip replacement. Med Care. 1993;31:141–54.
Fleisher L. Risk of anesthesia. Anesthesia. 5th ed. Philadelphia: Churchill Livingstone; 2000. p. 795–823.
Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE. APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med. 1981;9:591–7.
Midwinter M, Tytherleigh M, Ashley S. Estimation of mortality and morbidity risk in vascular surgery using POSSUM and the Portsmouth predictor equation. Br J Surg. 1999;86:471–4.
Owens WD, Felts JA, Spitznagel Jr EL. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978;49:239–43.
Edwards D. Data mining. J Proteome Res. 2003;2:334–4.
Han J, Kamber M, Pei J. Data mining: concepts and techniques. Morgan kaufmann; 2006. p. 215–30.
Lessa RC, Campos AH, Freitas CE, Silva FR, Kowalski LP, Carvalho AL, Vettore AL. Identification of upregulated genes in oral squamous cell carcinomas. Head & neck. 2013;35:1475–81.
Zainab Abu B, Fatihah M, Noor Maizura Mohamad N, Zainul Ahmad R. Looking for Bayesian reasoning in the diagnosis of the primary tumor stage in oral cancer. International Conference on Computational Science and Information Management (ICoCSIM). 2012;1:126–9.
Nesic V, Petrovic Z, Sipetic S, Jesic S, Soldatovic I, Kastratovic D. Comparison of the Adult Comorbidity Evaluation 27 and the Charlson Comorbidity indices in patients with laryngeal squamous cell carcinoma. J Laryngol Otol. 2012;126:516–24.
Xindong W, Vipin K, Ross Quinlan J, Joydeep G, Qiang Y, Hiroshi M, McLachlan GJ, Ng A, Liu B, Yu PS, Zhou ZH, Steinbach M, Hand DJ, Steinberg D. Top 10 algorithms in data mining. Knowl Inf Syst. 2008;14:1–37.
Jiang Su, Harry Zhang, Charles X. Ling, Stan Matwin: Discriminative parameter learning for bayesian networks. Icml. 2008, 88(96):359--373.
Touw WG, Bayjanov JR, Overmars L, Backus L, Boekhorst J, Wels M, van Hijum SA. Data mining in the Life Sciences with Random Forest: a walk in the park or lost in the jungle? Brief Bioinform. 2013;14(3):315–26.
Tarquinio SB, Zhang Z, Neiva KG, Polverini PJ, Nör JE. Endothelial cell Bcl-2 and lymph node metastasis in patients with oral squamous cell carcinoma. J Oral Pathol Med. 2012;41:124–30.
Broglie MA, Stoeckli SJ. Long-term experience in sentinel node biopsy for early oral and oropharyngeal squamous cell carcinoma. Ann Surg Oncol. 2011;18:2732–8.
Sarini J, Fournier C, Lefebvre J-L, Bonafos G, Van JT, Coche-Dequéant B. Head and neck squamous cell carcinoma in elderly patients: a long-term retrospective review of 273 cases. Arch Otolaryngol Head Neck Surg. 2001;127:1089–92.
Vokes EE, Weichselbaum RR, Lippman SM, Hong WK. Head and neck cancer. N Engl J Med. 1993;328:184–94.
Pignon J, Bourhis J, Domenge C, Designe L. Chemotherapy added to locoregional treatment for head and neck squamous-cell carcinoma: three meta-analyses of updated individual data. Lancet. 2000;355:949–55.
Sesterhenn AM, Teymoortash A, Folz BJ, Werner JA. Head and neck cancer in the elderly: a cohort study in 40 patients. Acta Oncol. 2005;44:59–64.
Clayman GL, Eicher SA, Sicard MW, Razmpa E, Goepfert H. Surgical outcomes in head and neck cancer patients 80 years of age and older. Head & Neck. 1998;20:216–23.
Mewissen MW, Seabrook GR, Meissner MH, Cynamon J, Labropoulos N, Haughton SH. Catheter-directed Thrombolysis for lower extremity deep Venous Thrombosis: report of a national multicenter registry. Radiology. 1999;211:39–49.
Acknowledgments
The authors thank Department of Oral Maxillofacial-Head Neck Oncology, Ninth People’s Hospital, School of Medicine, Shanghai Jiao Tong University for sharing their patient data and the list of pathological statistic. We also thank Tong Ji for the helpful advices on modeling and data analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
YMC and WC conceived the concept of the clinical research. YMC and HSO designed and performed the selection of the variables. TJ provided the opportunity for handling the Patients’ data. TJ and XCG participated in helpful discussions. YMC wrote the manuscript with help from WC and TJ.
The authors thank the project of "Top Priority Clinical Medical Center of Shanghai Municipal Commission of Health and Family Planning" for financial support. All authors read and approved the final manuscript.
YiMing Chen and Wei Cao contributed equally to this work.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Chen, Y., Cao, W., Gao, X. et al. Predicting postoperative complications of head and neck squamous cell carcinoma in elderly patients using random forest algorithm model. BMC Med Inform Decis Mak 15, 44 (2015). https://doi.org/10.1186/s12911-015-0165-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12911-015-0165-3