Abstract
Background
Music therapy is a standard palliative care service in many pediatric and adult hospitals; however, most research has focused on the use of music to improve psychosocial dimensions of health, without considering biological dimensions. This study builds on prior work examining psychosocial mechanisms of action underlying an Active Music Engagement (AME) intervention, designed to help manage emotional distress and improve positive health outcomes in young children with cancer and parents (caregivers), by examining its effects on biomarkers of stress and immune function.
Methods
This two-group randomized controlled trial (R01NR019190) is designed to examine biological mechanisms of effect and dose-response relationships of AME on child/parent stress during the consolidation phase of Acute B- or T-cell Lymphoblastic Leukemia (ALL) and T-cell Lymphoblastic Lymphoma (TLyLy) treatment. Child/parent dyads (n = 228) are stratified (by age, site, risk level) and randomized in blocks of four to the AME or attention control condition. Each group receives one session (30-minutes AME; 20-minutes control) during weekly clinic visits (4 weeks standard risk B-cell ALL; 8 weeks high risk B-cell ALL/T-cell ALL/TLyLy). Parents complete questionnaires at baseline and post-intervention. Child/parent salivary cortisol samples are taken pre- and post-session (sessions 1–4). Child blood samples are reserved from routine draws before sessions 1 and 4 (all participants) and session 8 (high risk participants). We will use linear mixed models to estimate AME’s effect on child/parent cortisol. Examining child/parent cortisol as mediators of AME effects on child and parent outcomes will be performed in an ANCOVA setting, fitting the appropriate mediation models using MPlus and then testing indirect effects using the percentile bootstrap approach. Graphical plots and non-linear repeated measures models will be used to examine dose-response relationship of AME on child/parent cortisol.
Discussion
During pediatric cancer treatment there are special challenges that must be considered when measuring cortisol and immune function. In this manuscript we discuss how we addressed three specific challenges through our trial design. Findings from this trial will increase mechanistic understanding of the effects of active music interventions on multiple biomarkers and understanding of dose-response effects, with direct implications for clinical practice.
Trial Registration
ClinicalTrials.gov: NCT04400071.
Similar content being viewed by others
Background
Music therapy has become a standard palliative care service in many pediatric and adult hospitals in the United States [1]. According to a survey of Children’s Hospital Association members, about 70% of the 245 hospitals surveyed reported offering music therapy services to their patients and families [2, 3]. Cancer treatment is an inherently stressful experience for both young children and their parents and their outcomes are interrelated [4,5,6,7]. Both children and parents experience emotional distress and poor quality of life, and many parents experience traumatic distress symptoms because of their child’s cancer diagnosis and treatment [8,9,10,11,12].
Although positive outcomes resulting from psychosocial interventions have been associated with improvements in biological function including decreased cortisol production and improved immune function [13,14,15,16,17,18,19], most music therapy research has focused on psychosocial dimensions of the cancer treatment experience, rather than its biological dimensions [20,21,22]. Coupled with growing evidence that active music experiences affect neuroendocrine and immune responses in other patient populations [23,24,25,26,27,28,29], an examination of active music to diminish emotional distress and improve positive health outcomes in children with cancer and parents is well justified and will address important gaps in our scientific knowledge about the use of music to improve health [30, 31].
The Active Music Engagement (AME) intervention uses interactive music play to counteract stressful qualities of the cancer treatment environment to reduce interrelated parent-child emotional distress and improve positive health outcomes during acute cancer treatment [32,33,34]. To counteract the lack of mechanistic understanding of music therapy approaches, we designed our current trial (R01NR019190) to examine AME’s effects on stress via Hypothalamic-Pituitary-Adrenal Axis (HPA-axis) activity and immune function (immunomodulatory cytokines). Within the context of pediatric cancer treatment there are special challenges that must be considered when measuring cortisol and immune function. In this manuscript we report our specific aims and study protocol. In addition, we identify and discuss three specific design challenges and how these were addressed.
Specific aims
Purposes of this two-group, randomized, controlled trial are to examine mechanisms of effect and dose-response relationships of AME on child/parent stress over time. Specific aims are to:
Aim 1
Compare the magnitude of change in child and parent cortisol levels between AME and control during Acute Lymphoblastic Leukemia (ALL) and T-cell Lymphoblastic Lymphoma (TLyLy) treatment.
Hypothesis 1.1
Compared to attention control, children in the AME group will have greater pre- to post-session percent decreases in cortisol.
Hypothesis 1.2
Compared to attention control, parents in the AME group will have greater pre-to post-session percent decreases in cortisol.
Aim 2
Examine cortisol as a mediator of AME effects on child and parent outcomes during ALL and TLyLy treatment.
Hypothesis 2.1
Reductions in child and/or parent cortisol will mediate the effect of AME on child immune function.
Hypothesis 2.2
Reductions in child and/or parent cortisol will mediate the effect of AME on child emotional distress and quality of life.
Hypothesis 2.3
Reductions in child and/or parent cortisol will mediate the effect of AME on parent emotional/traumatic distress symptoms and quality of life.
Aim 3 (Exploratory)
Examine the dose-response relationship of AME on child and parent cortisol during ALL and TLyLy treatment.
Hypothesis 3.1
While we make no hypotheses for this exploratory aim, we anticipate that AME effects may increase, decay, or remain constant over the course of treatment.
Methods
Methods for this trial are grounded in our previously published work including several pilot studies [33,34,35,36] and a manuscript that details of our treatment fidelity strategies [37].
Conceptual framework
Our conceptual framework (Fig. 1) is based on Robb’s Contextual Support Model of Music Therapy [32, 38], which is grounded in Self-Determination Theory [39] and further informed by Kazak’s Pediatric Medical Traumatic Stress Model [40], which provides a useful heuristic for understanding short and long-term consequences of pediatric cancer treatment for children and their parents. In our conceptual framework, recurring events related to cancer treatment (i.e., clinic visits, procedures) are viewed as stressful, potentially traumatic events.
Parent appraisal of events as traumatic or not traumatic is influenced by pre-existing factors that serve as covariates in our study. We based covariate selection on published research that indicates higher parent and child distress during cancer treatment is related to: (1) demographics (younger child/parent age, female parent gender, and lower socio-economic status/education) [41, 42], (2) higher parent/child distress with prior hospitalizations, and greater traumatic stress symptoms [5, 43, 44], and (3) disease and treatment characteristics (treatment intensity) [9,10,11, 45,46,47,48,49]. In addition, child and parent sex will be important covariates when analyzing our biological data based on evidence that sex hormones play a role in immune response [50, 51] and account for differences in salivary cortisol [52, 53].
We hypothesize that AME directly targets the mediators of child and parent biological stress (cortisol). Our study examines child and parent cortisol as mediators of AME intervention effect on outcomes for child (immune function, emotional distress, and quality of life) and parent (emotional distress, traumatic distress, quality of life). This study will allow us to determine how the AME intervention works at the biological level and the intersection of HPA-axis activity (cortisol) with reductions in emotional distress (emotional/traumatic stress; quality of life) associated with pediatric cancer treatment. Findings will have implications for the use of active music interventions to manage treatment-related distress in other populations.
Study design and randomization
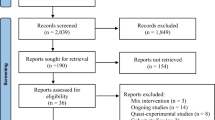
This study is a two group, stratified randomized controlled trial. The trial received Single Institutional Review Board Approval from Indiana University and is recruiting from three children’s hospitals in the United States. Children and one parent (enrolled as dyads) are stratified by child age (preschool 3–5 yrs; school-age 6–8 yrs), site, and treatment intensity (4 weeks standard risk B-cell ALL; 8 weeks high risk B-cell ALL, T-cell ALL, T-cell LyLy), and randomized in blocks of four to the AME intervention or attention control condition (audio-storybooks; ASB). See Fig. 2 for study schema.
Consolidation duration varies by risk level for B-cell ALL participants (4 weeks standard; 8 weeks high). Consolidation duration for all T-cell ALL and T-cell LyLy participants is 8 weeks. Treatment protocols and intensity of treatment are similar for high risk B-cell ALL and T-cell participants so we include all three diagnoses under the term “high risk” when referencing duration and intensity of treatment. As such, standard risk participants receive 4 weekly sessions and high risk participants receive 8 weekly sessions. We are enrolling both standard and high risk participants to examine whether dose-response differs based on treatment duration. It is important to examine changes in child-parent stress over the full treatment cycle, and we will control for variations in number of sessions through stratified randomization and our analytic methods.
Baseline data (Time 1) will be collected after consent and before the start of the consolidation phase of treatment. Time 2 data will be collected immediately following the last study session (and no later than 7 days following last study session). Following Time 2 questionnaires, parents randomized to AME will be offered an optional parent interview (completed within 3 weeks of T2 data collection). Parents/children are encouraged to use AME and low dose play activities between clinic visits and self-reported frequency and duration of activities will be collected during each session. Data collection timelines are based on positive findings from our preliminary studies and inform our primary aims that examine mediation [33, 54]. See Fig. 2 for study schema and Table 2 for assessment timelines.
Participants
Children and parents (or primary caregiver) will be enrolled as a dyad and must meet the following criteria to be study eligible. Inclusion criteria: (1) child is 3–8 years of age at time of enrollment, (2) child has diagnosis of standard or high-risk B- or T-cell ALL or T-cell lymphoblastic lymphoma (TLyLy), (3) child is currently receiving induction therapy, and (4) one parent (≥ 18 years of age) can be present for all sessions. Exclusion criteria: (1) child has Philadelphia positive ALL, (2) child has Cushing’s disease, (3) child takes steroid medication for asthma and/or has asthma that is not well-controlled, (4) parent does not speak English, or (5) the child has a significant cognitive impairment that might hinder participation (determination made in consultation with attending physician, oncologist, and parents).
Sample size and power analysis
We will recruit a total sample size of 228 child/parent dyads and assume 25% attrition to retain 170 child/parent dyads (85 dyads/group) at Time 2. The primary goal of this study is to examine mechanisms via the mediation effects of the AME intervention. We will use the percentile bootstrap method to estimate the indirect/mediated effect [55]. The sample size needed for this study is primarily driven by the power needed for the mediation hypothesis in Aim 2. Simulations of the two-path mediation model in Mplus [56] show that 170 subjects are needed to have 88% power to test the total indirect effect using the Sobel approach when the effect of the independent variable (AME in this case) on the mediator is at least medium (13% of variation explained), mediator on the outcome is between small and medium (7% of variation explained), and independent variable on the outcome is small (2% of variation explained). Via simulation, the Type I error with this sample size under a model that assumes no indirect effect is also less than 0.007, which will readily accommodate the multiple comparison adjustments planned below (e.g. with 7 cytokines a conservative Bonferroni adjustment would be 0.05/7 = 0.007). A sample size of 170 will also afford 90% power to detect a medium effect size for H1.1 and H1.2 based on a two-sample t-test with a two-sided alpha level of 0.05. Fitting models that allow for repeated measures across session will result in improved power. Using the percentile bootstrap method instead of Sobel should afford the same or greater power.
Setting
Young children (ages 3–8 years) and their parents are being recruited from three children’s hospitals. These hospitals are in metropolitan areas that serve large catchment areas. All three sites are members of the Children’s Oncology Group, and administer chemotherapy according to protocol guidelines, ensuring consistency of treatment across sites. Study conditions and data collection sessions will take place in the outpatient clinic setting.
Recruitment and informed consent
This study has received single Institutional Review Board Approval from the Indiana University Institutional Review Board which serves a central IRB for all participating institutions. Project managers at each site recruit children/parents during a scheduled clinic visit during the induction phase of treatment. During initial approach, project managers provide initial study introduction/brochure and verify eligibility. For interested families, child/parent dyads are enrolled following written, informed parental consent for parent and child and written assent for children ≥ 7 years, following human subjects review committee requirements.
Study condition procedures
Children/parents randomly assigned to AME or attention control receive sessions that are similar in length (30 min. AME; 20 min. ASB) and have the same timing of contact (4 weekly sessions standard risk; 8 weekly sessions high risk). In previous AME trials, the AME and ASB conditions were delivered in an in-patient setting and had an equal duration (45 min, with 30 min of music or stories) [33,34,35,36]. The current trial takes place in the outpatient clinic setting. To accommodate clinic flow and patient needs we needed to limit session duration to 30 min or less. As such, total session duration for AME sessions is 30 min total (5 min collaborative goal setting; 20 min of music-play; 5 min educational content). Total session duration for ASB is 20 min (5 min set-up; 15 min audio-storybooks – the length of one storybook). Although total session length is not equivalent, the amount of audio-visual stimulation is similar across groups, with the additional 10 min in AME attributed to assessment and educational activities that are unique to that condition. In addition to in-person sessions, participants take home a music-play or audio-storybooks kit to encourage between session use of the condition-related activities [33,34,35,36,37].
Both conditions are standardized (content, materials, and delivery), and all sessions are delivered by a board-certified music therapist in the outpatient clinic setting. All sessions are audio-recorded for quality assurance monitoring to ensure fidelity and prevent provider drift and/or contamination across treatment and control conditions (see Treatment Fidelity below).
Active music engagement (AME) intervention
The AME was designed based on the Contextual Support Model of Music Therapy (CSM-MT) [32] which is grounded in Self-Determination Theory [39], and further informed by Kazak’s Pediatric Medical Traumatic Stress Model [40]. The CSM-MT explains how music can be used to create a supportive environment by offering optimal levels of structure, autonomy support, and relationship support [38].
AME intervention sessions were designed for delivery by a board-certified music therapist who tailors music experiences to encourage active engagement in and independent use of music play as a strategy to manage emotional distress. During AME sessions, the music therapist provides children/parents repeated opportunities to experience competence, autonomy, and meaningful interactions through music play activities, which leads to active engagement and positive forms of coping. In addition, the therapist provides supportive education about ways music play can be used to manage distress and promote a sense of normalcy both during and between clinic visits.
There are three components to the AME intervention: (1) therapist-led music play activities, (2) the music play resource kit (to promote independent music play), and (3) tip sheets for parent education and support that focus on information and strategies aimed to help parents use music play to manage their child’s distress (the focus of the AME intervention) during clinic visits, and how to use music play at home. Table 1 shows the relationship of essential AME intervention content to CSM-MT theoretical principles.
Audio-storybooks (ASB) attention control condition
Trained music therapists also deliver the ASB condition, which was designed to control for attention from a provider, shared parent-child experiences, and audio-visual stimulation that comprise the non-therapeutic aspect of the AME condition. It offers parents/children opportunities to make choices and engage in an age-appropriate, non-music-based play activity. In each session, parents/children choose and listen to one of several illustrated children’s books with audio-recorded narration. In our prior work, this condition was acceptable to children and parents and did not demonstrate any significant benefits on our outcomes of interest, making it the best control condition for this trial [32,33,34].
Treatment fidelity strategies
For this trial, our team developed treatment fidelity strategies based on our prior studies [57] and NIH Behavior Change consortium recommendations [58]. Specific strategies for the five specified fidelity components (design, provider training, treatment delivery, treatment receipt, and treatment enactment) are central to ensuring study rigor and reproducibility. A description of treatment fidelity strategies for this trial, including strategies to reduce risk for bias and contamination between conditions, are detailed in a separate publication [37].
Outcome measures and data collection procedures
Parent (caregiver) report measures
Following informed consent, project managers at each site arrange a time for parents to complete baseline (T1) questionnaires during their first consolidation phase clinic appointment. A trained data collector administers questionnaires and remains available for questions. After completing T1 questionnaires, the project manager notifies the child/parent of their group assignment and schedules their first study condition session. Parents complete Time 2 questionnaires within 7 days of completing their last study session (session 4 for standard risk; session 8 for high risk).
The use of valid, reliable measures helps to ensure study rigor and reproducibility of results. All measures reflect careful consideration of psychometric properties, sensitivity to change, and response burden. Table 2 provides a list of measures, psychometrics, and administration schedule.
Biologic sample collections and storage during clinic visits
This study collects both saliva and blood. Both child and parent (caregiver) provide saliva for the detection of cortisol levels. Saliva collections occur before and after each intervention or attention control session at all 4 sessions for standard risk participants and the first 4 sessions for high-risk participants. The saliva is collected in a Salimetrics SalivaBio Oral Swab or SalivaBio Children’s Swab for the caregiver and child, respectively. The swab is immediately placed in the prelabeled storage tube, placed on dry ice post-collection, and stored at -80 C.
Blood is only collected from the children. At each site, 5 mL of blood is collected as part of routine study draws the morning of their sessions and used to isolate serum for cytokine analysis. This occurs at sessions 1 and 4 for all children with an additional draw at session 8 for high-risk children. Our primary site collects an additional 1 mL of blood to conduct a blood cortisol analysis for the purpose of monitoring adrenal function in a subset of the children on study. These collections occur at the child’s end of induction clinic appointment as well as sessions 1 through 4. Serum for cytokine analyses will be held until the end of the study at which point multiplexed analyses will be run. Serum for monitoring adrenal function in the children will be run on a yearly basis.
Treating physicians, at our three hospitals, have assigned clinic days and times (morning vs. afternoon). This will minimize variability in the timing of saliva collection between appointments. We will track day/time of collections and other factors that may contribute to child and parent cortisol interpretation (i.e., sleep, food/drink intake, medications).
Data collection on parent/child medications
We created a survey to identify and monitor sleep, food, and medication intake that may interfere with our ability to interpret cortisol collections. This survey is administered at the same time as our baseline participant questionnaires prior to any study sessions. The survey is structured in our database such that after parents fill out medication information for themselves and their children, they only need to update any changes that have occurred each visit for which there is a biologics collection. This process saves participants time and ensures smoother clinic flow.
Masking process
During study introduction and informed consent, the AME and ASB conditions are presented as equal conditions that inform our understanding about the use of play experiences, like music and stories, to reduce child and parent stress during cancer treatment. As such, child/parent dyads are masked to whether they are receiving the intervention or attention control condition. Data collectors administering baseline (T1) and post-intervention (T2) questionnaires are masked to participants’ group assignment. Should a data collector who is responsible for T2 data collection become aware of a participant’s group assignment, we assign another data collector unaware of group assignment to administer measures. Data collectors administering pre- and post-session saliva collections will not be masked to group assignment due to timing/proximity of collections to session delivery.
Data analysis
Analysis of biomarkers
Saliva samples cortisol levels will be analyzed using manufacturer validated R&D® ELISA kits and controls. The levels of IL-1\(\beta\), IL-6, TNF-\(\alpha\), IFN-\(\gamma\), IL-4, IL-10, and IL-13 in patient serum will be analyzed using a Bio-Rad multiplex immunoassay 7-plex kit and controls in the Multiplex Analysis Core. Reproducibility of these kits is validated by the manufacturer and each plate will be run with appropriate standards as well as internal controls to ensure reliability across lots. Kit lot numbers as well as certificates of analysis (provided by the manufacturer) will be kept with the study records.
Preliminary analyses
Prior to hypothesis testing, we will calculate coefficient alpha as a measure of internal consistency reliability on all multiple-item scales. Construct validity will be assessed by calculating Pearson or Spearman correlations among scales to determine if correlations are in the expected direction. We will present descriptive statistics for the AME group and the attention control group with respect to demographic and baseline outcome variables. We will control for child and parent age, site, risk level (standard or high), greater distress with prior hospitalizations, greater traumatic stress symptoms, time of collection of pre-session cortisol, and child and parent sex in all models. Age, site, and risk level are stratification variables. Time of collection of pre-session cortisol will account for differences based on standard diurnal differences. Although time of collection will be similar within each child, there will likely be between-child differences in time of collection (e.g., some children will have collections in morning and some in afternoon) that we will control for in analyses.
Missing data and multiple comparisons
We will compare all baseline variables between subjects who drop out of the study and those who do not using two-sample t tests, chi-square tests, or non-parametric equivalents as appropriate. MPlus software will incorporate participants who drop out before completion by using the MPLUS imputation method to perform a bias adjustment for missing data under maximum likelihood estimation and the assumption that data are missing at random. If we find that missing data are not missing at random, we will use a pattern mixture modeling approach to address; note we expect up to 25% attrition but minimal missing data on instruments (< 1%). We will adjust p value for multiple comparisons using the Bonferroni method for parent emotional/traumatic distress as there are two outcomes for this domain. For cytokine analyses, there are 7 cytokines of interest, so a Hochberg step-up approach will be used for these analyses.
Main analyses
For analyses below, we will analyze as randomized and attempt to collect outcome data on non-completers, following the intent-to-treat principle. For Aims 1 and 2, each outcome will be modeled separately, and we will examine sex as a biological variable by including sex as a covariate to control for its relationship with the outcomes and the interaction of sex and intervention group to examine if there are differential effects by intervention group. For Aim 1 (H1.1 and H1.2), the outcome will be the pre- to post- percent change in cortisol for each session. A linear mixed model will be fit with the independent fixed effects variables of intervention and session (1 to 4). Subject will be a random effect. We will use an F-test to test the intervention effect. For Aim 2 (H2.1, 2.2, 2.3), our primary goal is to test mediation effects. Mediation effects will be estimated in an ANCOVA setting, fitting the appropriate mediation models using MPlus [66] and then testing indirect effects using the percentile bootstrap approach to estimate the indirect effect [55]. The mediation model with two-path mediation effects specifies that the intervention will act through the mediator on the outcome and also have a direct effect on the outcome. Each outcome model will have 3 key predictors (intervention, two proximal mediators), and control for T1 outcome and covariates described above. For testing cortisol as a mediator, we will use (1) the estimated average percent change estimated from the mixed model, and (2) the % change from pre-session 1 to post session 4. In addition, we will look at child and parent cortisol levels both separately and together (multiple mediation model) in order to fully assess if/how they function together as mediators. Thus, for any single outcome, up to 6 models will be examined. For all mediation models in Aim 2, we will assess goodness-of-fit (GOF) using standard GOF measures (comparative fit index, root mean square error of approximation, and root mean square residual). For Aim 3, an exploratory aim, we will use graphical plots and non-linear repeated measures models to model the trend in percent changes in cortisol within and between intervention groups across the 4 sessions for all participants and across 8 sessions for high risk participants.
Discussion of biomarker strategy
Increased HPA-axis activity stimulates the release and production of inflammatory biomarkers [15, 67, 68], which in turn is associated with negative health outcomes for individuals with cancer (diminished immune function) [14, 15] and their parents (traumatic stress symptoms) [69]. This evidence supports investigation of biological pathways underlying the use of active music to mitigate cancer-related stress. To measure these during active cancer treatment, there were three primary challenges to overcome in designing this trial.
The first challenge was to avoid phases of treatment involving glucocorticoid therapy (e.g., prednisone or dexamethasone which are synthetic analogs of cortisol) [70]. Treatment for ALL and TLyLy in the United States currently consists of 5 phases: induction, consolidation, interim maintenance, delayed intensification, and maintenance. Based on our team’s review of Children’s Oncology Group protocols for treating standard and high risk pediatric B-cell ALL, T-cell ALL, and TLyLy, glucocorticoids are not used during the consolidation and interim maintenance phases. Children with ALL/TLyLy receive 2–4 weeks of glucocorticoid therapy during induction. Induction lasts for 28 days and consolidation starts 1–2 weeks post induction so they will have been off glucocorticoid therapy for at least seven days [71, 72]. At least 80% of children with ALL/TLyLy do not show adrenal insufficiency as early as 7–14 days after stopping either prednisone or dexamethasone [70, 73]. The 20% who have continued adrenal insufficiency are easily identified via morning cortisol levels of < 3mcg/dl and symptoms that would delay the onset of consolidation (e.g., fever, hypotension, vomiting) [73]. Therefore, these data suggest that cortisol can be measured in this population during consolidation.
To further address concerns about possible adrenal insufficiency at the start of consolidation, we will examine blood cortisol levels in a sub-sample of study participants (Indianapolis site) at the end of induction therapy, and on days during consolidation therapy when participants are scheduled to receive study sessions 1–4. This will allow us to identify participants in the sub-sample with adrenal insufficiency at the start of consolidation, which will enable us to better interpret alterations in salivary cortisol levels over time in those individuals. It may also allow us to recognize patterns in salivary cortisol levels that would indicate adrenal insufficiency to identify and control for participants at other sites with this same issue. The addition of the child blood cortisol collections will increase study rigor and interpretation of child salivary cortisol.
The second challenge was to select appropriate timing for cortisol collection while identifying strategies to avoid burdening children and parents [18, 19]. Cancer treatments’ interference with sleep schedules can disrupt diurnal rhythms of cortisol production [74]. To address these challenges, we will examine more immediate changes in cortisol that occur around the time of the AME or attention control experience (pre/post-session) and over time (across 4 weekly sessions); an approach taken in three previous pediatric studies [75,76,77]. This also mitigates the potential for increased burden on parents associated with collecting, storing, and transporting multiple samples from home to clinic, and related concern about sample viability. Over time, we expect that the size of within-child percent decrease in cortisol among AME children will become larger than the corresponding decrease observed in attention control children. Focusing on relative levels of cortisol within children minimizes the influence of children’s absolute levels of cortisol, for which the diurnal rhythms may be altered. With regard to timing, treating physicians at our three hospitals have assigned clinic days and times (morning vs. afternoon), and this will help minimize variability in the timing of salivary cortisol collection between appointments (e.g., patient A is always in clinic in the morning, patient B is always in clinic in the afternoon). In addition, we will statistically control for timing of cortisol collection as necessary.
The third challenge was to select and use highly sensitive measures of immune function. The capacity to modulate immune function in response to stress is fundamentally adaptive [14, 78,79,80], but chronic or severe stress can dysregulate the immune response, including the function of cytokines that act as messengers to the immune function cells [79]. Intensity and duration of stress can have significant negative effects on immune cell distribution and function via increases in glucocorticoids (e.g., cortisol). Effective immuno-protection requires that leukocytes rapidly respond to sites of infection or other potential risk (such as a wound or surgical site) [80]. This ability, in the face of short-term stress, is a necessary and underappreciated function of stress and stress hormones. However, in the long term, these same responses can lead to immune-pathology and decrease the child’s resistance to infection, wound healing, and even the cancer treatment itself [79]. The immune markers to be utilized in our study were chosen to capture information on the signaling occurring within the immune system that will modulate the function and phenotypes of immune cells and ultimately affect immune function.
Our team has worked to anticipate and address challenges associated with studying the interrelated stress of young children with cancer and parents during cancer treatment to create a rigorous trial design. However, as with any clinical trial, we recognize that a variety of factors such as the nature of the disease, unexpected drug interactions, and unanticipated treatment deviations will occur. This includes development of rigorous treatment fidelity strategies and the formation of interdisciplinary teams that remain engaged over the life of the trial - monitoring and assessing unexpected situations and making quick decisions to account for variations and maintain study integrity.
As one of the first pediatric music intervention studies to examine biomarkers of stress and immune function, findings from this trial will inform clinical practice in important ways including improved understanding about how active music effects parent and child stress (and the interrelated nature of their stress) at the biological level, and the potential benefit and clinical utility of active music to improve immune function in children during cancer treatment.
Data availability
Not applicable.
Abbreviations
- ALL:
-
Acute Lymphoblastic Leukemia
- AME:
-
Active Music Engagement
- ASB:
-
Audio-Storybooks
- CSM-MT:
-
Contextual Support Model of Music Therapy
- GOF:
-
goodness-of-fit
- HPA:
-
Hypothalamic-Pituitary-Adrenal
- TLyLy:
-
T-cell Lymphoblastic Leukemia
- T1:
-
Time 1 (baseline)
- T2:
-
Time 2
References
American Music Therapy Association. 2017 American Music Therapy Association Member Survey and Workforce Analysis. Silver Spring, MD; 2018.
Neugebauer C. Pediatric Music Therapy Task Force Report: American Music Therapy Association. Silver Spring, MD; 2014.
Knott D, Biard M, Nelson KE, Epstein S, Robb SL, Ghetti CM. A survey of music therapists working in Pediatric Medical Settings in the United States. J Music Ther. 2020;57(1):34–65.
Colletti CJ, Wolfe-Christensen C, Carpentier MY, Page MC, McNall-Knapp RY, Meyer WH, et al. The relationship of parental overprotection, perceived vulnerability, and parenting stress to behavioral, emotional, and social adjustment in children with cancer. Pediatr Blood Cancer. 2008;51(2):269–74.
Kazak AE, Barakat LP. Brief report: parenting stress and quality of life during treatment for childhood leukemia predicts child and parent adjustment after treatment ends. J Pediatr Psychol. 1997;22(5):749–58.
Robinson KE, Gerhardt CA, Vannatta K, Noll RB. Parent and family factors associated with child adjustment to pediatric cancer. J Pediatr Psychol. 2007;32(4):400–10.
Rodriguez EM, Dunn MJ, Zuckerman T, Vannatta K, Gerhardt CA, Compas BE. Cancer-related sources of stress for children with cancer and their parents. J Pediatr Psychol. 2012;37(2):185–97.
Bruce M. A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clin Psychol Rev. 2006;26(3):233–56.
Furlong W, Rae C, Feeny D, Gelber RD, Laverdiere C, Michon B, et al. Health-related quality of life among children with acute lymphoblastic leukemia. Pediatr Blood Cancer. 2012;59(4):717–24.
Kunin-Batson AS, Lu X, Balsamo L, Graber K, Devidas M, Hunger SP, et al. Prevalence and predictors of anxiety and depression after completion of chemotherapy for childhood acute lymphoblastic leukemia: a prospective longitudinal study. Cancer. 2016;122(10):1608–17.
Myers RM, Balsamo L, Lu X, Devidas M, Hunger SP, Carroll WL, et al. A prospective study of anxiety, depression, and behavioral changes in the first year after a diagnosis of childhood acute lymphoblastic leukemia: a report from the Children’s Oncology Group. Cancer. 2014;120(9):1417–25.
Rosenberg AR, Dussel V, Kang T, Geyer JR, Gerhardt CA, Feudtner C, et al. Psychological distress in parents of children with advanced cancer. JAMA Pediatr. 2013;167(6):537–43.
Antoni MH. Psychosocial intervention effects on adaptation, disease course and biobehavioral processes in cancer. Brain Behav Immun. 2013;30 Suppl:88–98.
Antoni MH, Dhabhar FS. The impact of psychosocial stress and stress management on immune responses in patients with cancer. Cancer. 2019;125(9):1417–31.
Costanzo ES, Sood AK, Lutgendorf SK. Biobehavioral influences on cancer progression. Immunol Allergy Clin North Am. 2011;31(1):109–32.
Green McDonald P, O’Connell M, Lutgendorf SK. Psychoneuroimmunology and cancer: a decade of discovery, paradigm shifts, and methodological innovations. Brain Behav Immun. 2013;30(Suppl):1–9.
Hulett JM, Armer JM. A systematic review of spiritually based interventions and psychoneuroimmunological outcomes in breast Cancer survivorship. Integr Cancer Ther. 2016;15(4):405–23.
Kang DH, Rice M, Park NJ, Turner-Henson A, Downs C. Stress and inflammation: a biobehavioral approach for nursing research. West J Nurs Res. 2010;32(6):730–60.
Moore IM. Advancing biobehavioral research in childhood cancer. J Pediatr Oncol Nurs. 2004;21(3):128–31.
Bradt J, Dileo C, Magill L, Teague A. Music interventions for improving psychological and physical outcomes in cancer patients.Cochrane Database Syst Rev. 2016(8):CD006911.
Burns DS. Theoretical rationale for music selection in oncology intervention research: an integrative review. J Music Ther. 2012;49(1):7–22.
Robb SL, Hanson-Abromeit D. A review of supportive care interventions to manage distress in young children with cancer and parents. Cancer Nurs. 2014;37(4):E1–E26.
Bittman BB, Berk LS, Felten DL, Westengard J, Simonton OC, Pappas J, et al. Composite effects of group drumming music therapy on modulation of neuroendocrine-immune parameters in normal subjects. Altern Ther Health Med. 2001;7(1):38–47.
Chanda ML, Levitin DJ. The neurochemistry of music. Trends Cogn Sci. 2013;17(4):179–93.
Fancourt D, Ockelford A, Belai A. The psychoneuroimmunological effects of music: a systematic review and a new model. Brain Behav Immun. 2014;36:15–26.
Fancourt D, Perkins R, Ascenso S, Atkins L, Kilfeather S, Carvalho L, et al. Group Drumming modulates Cytokine Response in Mental Health Services users: a preliminary study. Psychother Psychosom. 2016;85(1):53–5.
Fancourt D, Perkins R, Ascenso S, Carvalho LA, Steptoe A, Williamon A. Effects of Group Drumming Interventions on anxiety, Depression, Social Resilience and Inflammatory Immune response among Mental Health Service users. PLoS ONE. 2016;11(3):e0151136.
Fancourt D, Williamon A, Carvalho LA, Steptoe A, Dow R, Lewis I. Singing modulates mood, stress, cortisol, cytokine and neuropeptide activity in cancer patients and carers. Ecancermedicalscience. 2016;10:631.
Koyama M, Wachi M, Utsuyama M, Bittman B, Hirokawa K, Kitagawa M. Recreational music-making modulates immunological responses and mood states in older adults. J Med Dent Sci. 2009;56(2):79–90.
Cheever T, Taylor A, Finkelstein R, Edwards E, Thomas L, Bradt J, et al. NIH/Kennedy Center Workshop on Music and the brain: finding Harmony. Neuron. 2018;97(6):1214–8.
Collins FS, Fleming R. Sound Health: an NIH-Kennedy Center Initiative to explore music and the mind. JAMA. 2017;317(24):2470–1.
Robb SL. The effect of therapeutic music interventions on the behavior of hospitalized children in isolation: developing a contextual support model of music therapy. J Music Ther. 2000;37(2):118–46.
Robb SL, Clair AA, Watanabe M, Monahan PO, Azzouz F, Stouffer JW, et al. Non-randomized controlled trial of the active music engagement (AME) intervention on children with cancer. Psychooncology. 2008;17(9):957.
Robb SL, Haase JE, Perkins SM, Haut PR, Henley AK, Knafl KA, et al. Pilot randomized trial of active Music Engagement intervention parent delivery for Young Children with Cancer. J Pediatr Psychol. 2017;42(2):208–19.
Russ KA, Holochwost SJ, Perkins SM, Stegenga K, Jacob SA, Delgado D, Henley AK, Haase JE, Robb SL. Cortisol as an acute stress biomarker in young hematopoietic stem cell transplant patients/caregivers: active Music Engagement protocol. J Altern Complement Med. 2020;26(5):424–34.
Holochwost SJ, Robb SL, Henley AK, Stegenga K, Perkins SM, Russ KA, Jacob SA, Delgado D, Haase JE, Krater CM. Active Music Engagement and cortisol as an acute stress biomarker in young heamtopoietic stem cell transplant patients and caregivers: Results of a single case design pilot study. 2020;11.
MacLean JASK, Henley AK, Robb SL. Implementing NIH Behavior Change Consortium treatment fidelity recommendations in a multi-site randomized controlled trial of an active music engagement intervention for young children with cancer and parents. Integr Cancer Ther. 2022;21:15347354221140491.
Robb SL. Coping and chronic illness: music therapy for children and adolescents with cancer. In: Robb SL, editor. Music therapy in pediatric healthcare: Research and evidence-based practice. Silver Spring, MD: American Music Therapy Association; 2003. pp. 101–36.
Ryan RMDE. Self-determination theory: Basic Psychological needs in motivation. Development, and Wellness: Guilford Publications; 2017.
Kazak AE, Baxt C. Families of infants and young children with cancer: a post-traumatic stress framework. Pediatr Blood Cancer. 2007;49(7 Suppl):1109–13.
Kazak AE, Cant MC, Jensen MM, McSherry M, Rourke MT, Hwang W, et al. Identifying psychosocial risk indicative of subsequent resource use in families of newly diagnosed pediatric oncology patients. J Clin Oncol. 2003;21(17):3220–5.
Stevens B, Croxford R, McKeever P, Yamada J, Booth M, Daub S, et al. Hospital and home chemotherapy for children with leukemia: a randomized cross-over study.[see comment]. Pediatr Blood Cancer. 2006;47(3):285–92.
Best M, Streisand R, Catania L, Kazak AE. Parental distress during pediatric leukemia and posttraumatic stress symptoms (PTSS) after treatment ends. J Pediatr Psychol. 2001;26(5):299–307.
Barrera M, D’Agostino NM, Gibson J, Gilbert T, Weksberg R, Malkin D. Predictors and mediators of psychological adjustment in mothers of children newly diagnosed with cancer. Psycho-oncology. 2004;13(9):630–41.
Kazak AE, Boeving CA, Alderfer MA, Hwang WT, Reilly A. Posttraumatic stress symptoms during treatment in parents of children with cancer. J Clin Oncol. 2005;23(30):7405–10.
Kazak AE, Stuber ML, Barakat LP, Meeske K, Guthrie D, Meadows AT. Predicting posttraumatic stress symptoms in mothers and fathers of survivors of childhood cancers. J Am Acad Child Adolesc Psychiatry. 1998;37(8):823–31.
Hobbie WL, Stuber M, Meeske K, Wissler K, Rourke MT, Ruccione K, et al. Symptoms of posttraumatic stress in young adult survivors of childhood cancer. J Clin Oncol. 2000;18(24):4060–6.
Stuber ML, Kazak AE, Meeske K, Barakat L, Guthrie D, Garnier H, et al. Predictors of posttraumatic stress symptoms in childhood cancer survivors. Pediatrics. 1997;100(6):958–64.
Langeveld NE, Grootenhuis MA, Voute PA, de Haan RJ. Posttraumatic stress symptoms in adult survivors of childhood cancer. Pediatr Blood Cancer. 2004;42(7):604–10.
Klein SLFK. Sex differences in immune responses. Nat Rev Immunol. 2016;16(10):626–38.
Roved JWH, Hasselquist D. Sex differences in immune responses: hormonal effects, antagonistic selection, and evolutionary consequences. Horm Behav. 2017;88:95–105.
Hollanders JJ, vdVB, Rotteveel J, Finken MJJ. Is HPA axis reactivity in childhood gender-specific? A sysematic review. Biol Sex Differ. 2017;8(1):23.
van der Voorn BHJ, Ket JCF, Rotteveel J, Finken MJJ. Gender-specific differences in hypothalmus-pituitary-adrenal axis activity during childhood: A systematic review and meta-analysis.Biol Sex Differ. 2017;8(3).
Robb SL, Burns DS, Stegenga KA, Haut PR, Monahan PO, Meza J, et al. Randomized clinical trial of therapeutic music video intervention for resilience outcomes in adolescents/young adults undergoing hematopoietic stem cell transplant: a report from the Children’s Oncology Group. Cancer. 2014;120(6):909–17.
Fritz MS, Taylor AB, Mackinnon DP. Explanation of two anomalous results in statistical mediation analysis. Multivar Behav Res. 2012;47(1):61–87.
Thoemmes F, Mackinnon DP, Reiser MR. Power Analysis for Complex Mediational designs using Monte Carlo Methods. Struct Equ Modeling. 2010;17(3):510–34.
Robb SL, Burns DS, Docherty SL, Haase JE. Enusring treatment fidelity in a multi-site behavioral intervention study: implementing NIH behavior change consortium recommendations in the SMART trial. Psycho-Oncol. 2011;20:1193–201.
Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol. 2004;23(5):443–51.
Phipps S, Dunavant M, Lensing S, Rai SN. Psychosocial predictors of distress in parents of children undergoing stem cell or bone marrow transplantation. J Pediatr Psychol. 2005;30(2):139–53.
Lang AJ, Stein MB. An abbreviated PTSD checklist for use as a screening instrument in primary care. Behav Res Ther. 2005;43(5):585–94.
Landgraf J, Abetz L, Ware JE. Child Health Questionnaire (CHQ): a user’s Manual. Boston, MA: HealthAct; 1999.
Ravens-Sieberer U, Bullinger M. KINDLR: Questionnaire for measuring health-related quality of life in children and adolescents - revised form, Test Manual. Hamburg: University Clinic Hamburg-Eppendorf; 2000.
Shacham S. A shortened version of the Profile of Mood States. J Pers Assess. 1983;47(3):305–6.
Weiss DM. The impact of events scale-revised. In: Keane JWT, editor. Assessing psychological trauma and PTSD. New York: Guilford; 1997. pp. 399–411.
Moinpour C, Feigl P, Metch B, Hayden KA, Meyskens FL, Crowley J. Quality of life end points in cancer clincal trials: review and recommendations. J Natl Cancer Inst. 1989;81(7):485–95.
Muthen LK, Muthen BO. Mplus User’s Guide, 5th ed. Los Angeles: Muthen & Muthen; 1998–2007.
Glaser R, Kiecolt-Glaser JK. Stress-induced immune dysfunction: implications for health. Nat Rev Immunol. 2005;5(3):243–51.
Padgett DAG. How stress infuences the immune response. Trends Immunol. 2003;24(6):444–8.
Stoppelbein L, Greening L, Fite PJ. Brief report: role of cortisol in posttraumatic stress symptoms among mothers of children diagnosed with cancer. J Pediatr Psychol. 2010;35(9):960–5.
Rensen N, Gemke RJ, van Dalen EC, Rotteveel J, Kaspers GJ. Hypothalamic-pituitary-adrenal (HPA) axis suppression after treatment with glucocorticoid therapy for childhood acute lymphoblastic leukaemia. Cochrane Database Syst Rev. 2017;11:CD008727.
Cooper SL, Brown PA. Treatment of Pediatric Acute Lymphoblastic Leukemia. Pediatr Clin North Am. 2015;62(1):61–.
Hunger SP, Mullighan CG. Acute lymphoblastic leukemia in children. N Engl J Med. 2015;373(16):1541–52.
Einaudi S, Bertorello N, Masera N, Farinasso L, Barisone E, Rizzari C, et al. Adrenal axis function after high-dose steroid therapy for childhood acute lymphoblastic leukemia. Pediatr Blood Cancer. 2008;50(3):537–41.
Page GGCE, Dorsey SG, et al. Biomarkers as common data elements for symptom and self-management science. J Nurs Scholarsh. 2018;50(3):276–86.
Lane D. The effect of a single music therapy session on hospitalized children as measured by salivary immunoglobulin A, speech pause time, and a patient opinion likert scale. Case Western Reserve University; 1991.
Post-White J, Fitzgerald M, Hageness S, Sencer SF, Post-White J, Fitzgerald M, et al. Complementary and alternative medicine use in children with cancer and general and specialty pediatrics. J Pediatr Oncol Nurs. 2009;26(1):7–15.
Walco GA, Conte PM, Labay LE, Engel R, Zeltzer LK. Procedural distress in children with cancer: self-report, behavioral observations, and physiological parameters. Clin J Pain. 2005;21(6):484–90.
Dhabhar FS. Enhancing versus suppressive effects of stress on immune function: implications for immunoprotection and immunopathology. Neuroimmunomodulation. 2009;16(5):300–17.
Dhabhar FS. Effects of stress on immune function: the good, the bad, and the beautiful. Immunol Res. 2014;58(2–3):193–210.
Elenkov IJ, Chrousos GP. Stress hormones, Th1/Th2 patterns, Pro/Anti-inflammatory cytokines and susceptibility to Disease. Trends Endocrinol Metab. 1999;10(9):359–68.
Acknowledgements
None.
Funding
This trial is funded by the National Institutes of Health, National Institute of Nursing Research (R01NR019190, Robb, PI).
Author information
Authors and Affiliations
Contributions
SR conceived of the study, developed study conditions, and led/coordinated study conceptualization and design. All Authors contributed to overall study conceptualization and design – specifically, KR and SH provided expertise in biomarker selection, collection, and analysis; KS and SJ provided expertise in pediatric cancer treatment protocols and symptom management; SP provided statistical expertise in clinical trial design and planned analyses; AH and JM provided clinical expertise in music therapy and clinical trials management. SR is Principal Investigator, KR, SH, KS, SP, SJ and AH co-investigators, and JM key personnel for this NIH-funded trial. All Authors contributed to refinement of the study protocol and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been approved by the Indiana University Institutional Review Board (IRB 00000219/IRB-04; Protocol #1909060683). Informed consent will be obtained from all the participants involved in the study. Parent participants will provide written/signed informed consent for their own participation. For all child participants, we will obtain written/signed informed consent from the child’s parent and/or legal guardian. In addition to written/signed informed consent from the child’s parent and/or legal guardian, we will also obtain written assent from the child if they are 7 years of age or older. All methods for this study, including informed consent and the collection and storage of blood/saliva samples, will be carried out in accordance with guidelines and regulations set forth by the Indiana University Institutional Review Board.
Protocol version
Issue Date: 26 October 2022; Protocol Amendment Number: A033; Version 13.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Robb, S.L., Russ, K.A., Holochwost, S.J. et al. Protocol and biomarker strategy for a multi-site randomized controlled trial examining biological mechanisms and dosing of active music engagement in children with acute lymphoblastic leukemia and lymphoma and parents. BMC Complement Med Ther 23, 90 (2023). https://doi.org/10.1186/s12906-023-03909-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-023-03909-w