Abstract
Background
While there are several existing eHealth technologies for drug-drug interactions and stand-alone drug adverse effects, it appears that considerably less attention is focussed on that of complementary and alternative medicine (CAM). Despite poor knowledge of their potential interactions and side effects, many patients use CAM. This justifies the need to identify what eHealth technologies are assisting in identifying potential 1) adverse drug interactions with CAM, 2) adverse CAM-CAM interactions or 3) standalone CAM adverse events or side effects.
Methods
A scoping review was conducted to identify eHealth technologies assisting in identifying potential adverse interactions with CAM or standalone CAM adverse events or side effects, following Arksey and O’Malley’s five-stage scoping review framework. MEDLINE, EMBASE, and AMED databases and the Canadian Agency for Drugs and Technologies in Health website were systematically searched. Eligible articles had to have assessed or referenced an eHealth technology assisting in identifying potential one or more of the three aforementioned items. We placed no eligibility restrictions on type of eHealth technology.
Results
Searches identified 3467 items, of which 2763 were unique, and 2674 titles and abstracts were eliminated, leaving 89 full-text articles to be considered. Of those, 48 were not eligible, leaving a total of 41 articles eligible for review. From these 41 articles, 69 unique eHealth technologies meeting our eligibility criteria were identified. Themes which emerged from our analysis included the following: the lack of recent reviews of CAM-related healthcare information; a large number of databases; and the presence of government adverse drug/event surveillance.
Conclusions
The present scoping review is the first, to our knowledge, to provide a descriptive map of the literature and eHealth technologies relating to our research question. We highlight that while an ample number of resources are available to healthcare providers, researchers, and patients, we caution that the quality and update frequency for many of these resources vary widely, and until formally assessed, remain unknown. We identify that a need exists to conduct an updated and systematically-searched review of CAM-related healthcare or research resources, as well as develop guidance documents associated with the development and evaluation of CAM-related eHealth technologies.
Similar content being viewed by others
Background
Considerable research has established that the concurrent use of pharmaceutical drugs and complementary and alternative medicines (CAMs) can lead to unwanted interactions; furthermore, certain CAMs have been shown to cause standalone adverse reactions [1]. It is currently estimated that more than 70% of North Americans have tried at least one form of CAM, which includes traditional medicines [2,3,4], and collectively spend billions of dollars on these therapies each year [5, 6]. An integral part of CAMs include natural health products (NHPs) in Canada, which are sold directly to Canadians and do not require a prescription nor the oversight of a healthcare professional, despite being regulated by Health Canada [7]. A 2010 Ipsos-Reid poll showed that 73% of Canadians took NHPs regularly [8], yet only 19% of Canadians surveyed by Health Canada considered themselves well-informed when purchasing NHPs. Furthermore, 12% of Canadians who used NHPs report that they experienced adverse reactions, and only 41% of Canadians who experienced adverse effects from NHPs reported them [8].
eHealth is used widely in managing patients’ medications, however, it is currently unknown what types of eHealth technologies are available to detect potential drug interactions with CAM or standalone CAM adverse effects. With regard to pharmaceutical technologies, there are some useful medication databases available that can be integrated into hospitals’ electronic data and used as a tool for computerized decision support systems (CDSS). Studies on programs such as the Swedish Finnish Interaction X-referencing or SFINX database have demonstrated a correlation between medication alert systems and a decrease in potentially adverse drug interactions [9]. In some hospitals, medication-related CDSSs are used which evaluate drug dosage, patients’ age, and comorbidities and send alarms when possible drug interactions and side effects are detected [10].
Additionally, there are several mobile apps that provide beneficial information regarding appropriate dosing, potential drug-drug interactions, and side effects. WebMD, Medscape, Epocrates, The Blue Book, and Micromedex are some of the most commonly used mobile drug information apps [11]. These types of mobile health (mHealth) apps are used by both health professionals and patients, and many are publicly available in the Google Play or the Apple App Store [12]. Some mobile apps have been developed to assist patients taking high-risk medications to manage their symptoms. For example, an app was developed by a team of collaborators in Oxford for patients undergoing treatment for colorectal cancer. This type of mHealth system shares the data recorded by the patient in symptom diaries with their health professional and will generate an alarm if a serious side effect occurs [13].
Moreover, computer-assisted history-taking systems (CAHTS) are other eHealth tools that have the potential to improve the monitoring of drug interactions and side-effects. CAHTS allow patients to enter their medication history prior to consultations, resulting in a more comprehensive record of medication information [14].
While there are several existing eHealth technologies for drug-drug interactions and stand-alone drug adverse effects, it appears that considerably less attention is focussed on CAM-drug interactions, CAM-CAM interactions, and standalone CAM adverse effects. Despite poor knowledge of their potential interactions and side effects, many patients use CAM. This justifies the need to identify what eHealth technologies exist for such CAM-related interactions and adverse effects.
Methods
Approach
A scoping review was conducted to identify eHealth technologies assisting in identifying potential adverse interactions with CAM or standalone CAM adverse events or side effects, following Arksey and O’Malley’s [15] five-stage scoping review framework, and supplemented by Levac, Colquhoun, & O’Brien [16] and Daudt, van Mossel, & Scott [17] which build upon Arksey and O’Malley’s work. The five steps are as follows: (1) identifying the research question, (2) identifying relevant studies, (3) selecting the studies, (4) charting the data, and (5) collating, summarizing, and reporting the results. This method was chosen in order to fulfill the prerequisites of a scoping review, which involve searching for and assessing the available literature on a given topic in order to identify the characteristics of eligible articles, summarize their contents and highlight knowledge gaps. We did not register a protocol.
Step 1: identifying the research question
The research question for this scoping review was as follows: “What eHealth technologies are assisting in identifying potential 1) adverse drug interactions with CAM, 2) adverse CAM-CAM interactions or 3) standalone CAM adverse events or side effects?”. While a multitude of definitions for “eHealth” exists [18], for the purpose of this scoping review, in order to define parameters of eHealth, we considered 3 domains and their subcategories based on a study by Shaw et al. [19]. The framework for defining eHealth technologies are summarized in Table 2 in Appendix 3 of their paper. CAM has also been defined in a multitude of ways [20], however, the National Center for Complementary and Integrative Health (NCCIH) defines a non-mainstream practice used together with conventional medicine as “complementary”, a non-mainstream practice used in place of conventional medicine as “alternative”, and the coordinated delivery or use of conventional and complementary approaches as “integrative” [21]. For the purpose of this scoping review, in order to define parameters of eHealth, we considered Wieland et al.’s [22] bibliometric and content analysis of the Cochrane Complementary Medicine Field specialized register of controlled trials, where the authors collected the number of CAM field specialized register citations classified by type of CAM therapies. What was included as CAM are shown in Table 4 in Appendix 3 of their paper. Finally, we define the term “adverse event” as “any untoward medical occurrence that may present during treatment with a medicine but which does not necessarily have a causal relationship with this treatment”, and “side effect” as “any unintended effect of a pharmaceutical product [or CAM] occurring at doses normally used in man, which is related to the pharmacological proprieties of the drug [or CAM]”. Our definition of the terms “adverse event” and “side effect” correspond with that of the World Health Organization [23].
Step 2: finding relevant studies
Following a preliminary scan of the literature, an experienced academic librarian was consulted to assist in devising a comprehensive, systematic search strategy on MEDLINE, EMBASE, and AMED academic databases. The search included literature published from 1995 up until November 6, 2019, as eHealth was only popularized in the late 1990s with the term itself was coined in 1999 [24]. The search strategy included Medical Subject Headings and keywords that reflect terms commonly used in the literature to refer to both eHealth and CAM. Following preliminary searches, it was decided not to also include search terms relating to adverse events or side effects, as many eligible articles were found to not be indexed using them and thus this would have excluded them. Additionally, the Canadian Agency for Drugs and Technologies in Health (CADTH) website (https://www.cadth.ca/) was also searched to account for any grey literature; terms searched included “eHealth”, “mHealth”, “complementary and alternative medicine” and “herbal”. A search strategy we used including Medical Subject Headings and keywords that reflect terms commonly used in the literature to refer to CAM and eHealth can be found in Appendix 1.
Step 3: selecting the studies
Preliminary searches indicated that the academic literature on this subject area exists as eligible articles could be found. We included primary research articles and research protocols; any relevant reviews were used to source additional eligible primary research articles or research protocols. In order to be included, the article had to have included an eHealth technology (either the authors’ own or referenced) of any kind that was assisting in identifying potential 1) adverse drug interactions with CAM, 2) adverse CAM-CAM interactions, or 3) standalone CAM adverse events or side effects, otherwise they were excluded. At this stage, articles were excluded if they did not make reference to our research question. Publications in the form of conference abstracts were not eligible. We also restricted eligibility to articles published in the English language and that were either publicly available or could be ordered through our library system. If there was any uncertainty, the article’s full-text was reviewed to determine eligibility. We placed no eligibility restrictions on type of eHealth technology; even if they were only accessible in a non-English language, we included them as long as English literature was written about them. All three authors (JYN, MM, and VM) pilot-screened a subset of all titles and abstracts independently and met to verify their agreement in applying the inclusion criteria prior to screening all items, including the full-texts of potentially eligible articles, independently in triplicate. Disagreement was solved by discussion, and in the case that consensus could not be reached, a majority vote was used to determine eligibility.
Step 4: charting the data
Articles meeting the inclusion criteria were critically reviewed using Arksey and O’Malley’s [15] descriptive-analytical narrative method. For each eligible article, the following data were extracted and charted: article title; author(s); year of publication; study country; study design; whether the article was original research or a review of resources; study aim; and name of eHealth technology(s) assessed or referenced in the eligible article that we assessed in this scoping review. For each included eHealth technology, the following data were extracted and charted: name; URL (if available), type (i.e. adverse drug reporting system, database, factsheets, etc.), format (i.e. website, mobile app, etc.), year established; if the eHealth technology still exists; whether it has been used in any context outside of the authors’ study; whether it is free and/or available to anyone; developer (and category); purpose; and intended user(s). All three authors (JYN, MM, and VM) participated in a pilot data extraction of a subset of eligible articles/eHealth technologies, and MM and VM independently extracted data from all eligible articles as well as from all eHealth technologies (i.e. the authors’ own or referenced). All three authors then met to discuss and resolve discrepancies. We did not conduct a critical appraisal of included sources of evidence nor did we collect included articles’ sources of funding, as no prior scoping review had been conducted on this topic before, thus we only aimed to provide a descriptive map of the literature and highlight a number of key themes that emerged from our analysis.
Step 5: collating, summarizing, and reporting the results
Charted data was summarized in the format of tables, and the descriptive data were analysed using content analysis. All three authors (JYN, MM, and VM) reviewed the descriptive data, and JYN identified codes relative to the findings, organized codes into thematic groups, and presented a narrative relating to the research question as well as highlighted knowledge gaps in the currently existing literature. All three authors then met to discuss and resolve discrepancies.
Results
Search results
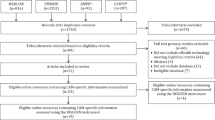
Searches identified a total of 3467 items, of which 2763 were unique, and 2674 titles and abstracts were eliminated, leaving 89 full-text articles to be considered. Of those, 48 were not eligible, because they did not include eHealth technology meeting eligibility criteria (n=44) or were an abstract (n=4), leaving a total of 41 articles that were included in this scoping review [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65]. A PRISMA diagram can be found in Fig. 1 of Appendix 2.
Eligible article characteristics
Eligible articles were published from 1997 to 2019 and originated from the United States (n=16), China (n=8), Germany (n=3), Republic of Korea (n=3), Singapore (n=3), Canada (n=1), Denmark (n=1), Greece (n=1), Italy (n=1), Sweden (n=1), and United Kingdom (n=1). Additionally, one study involved researchers from Australia, China, and Germany (n=1), and another from China and the United Kingdom (n=1). Of the 41 articles included, 27 were primary research articles with the following study designs: development (n=12) or evaluation (n=7) of an eHealth technology, analysis of data collected by an eHealth technology (n=7), and a usability study (n=1); the remaining 14 articles were reviews of one or more medical information resource(s) including at least one containing an eHealth technology addressing our research question. Here, we define a “review” as an article that reviewed an aspect of the entirety of an eligible eHealth technology, and not necessarily a systematic or scoping review. The details associated with all eligible article characteristics, including study aims, can be found in Table 1 of Appendix 3.
eHealth technology characteristics
Of the 69 included eHealth technologies, we characterized them as follows: databases (n=34), factsheets/healthcare information (n=13), adverse drug/event alerting, reporting and/or signal detection systems (n=11), search engines (n=4), interaction checkers (standalone) (n=1), bulletin (n=1), continuing education module (n=1), electronic pharmacovigilance system (n=1), model (n=1), and serious game (n=1). Additionally, one eHealth technology is both an adverse drug reaction detection/spontaneous reporting system and a database. These eHealth technologies were offered in the following formats: websites/web-based only (n=38), website and mobile app (n=10), mobile app only (n=6), software (n=2), artificial intelligence (n=1). The format was unclear for the remaining twelve. In many cases, it was difficult to ascertain the year the eHealth technology was created (n=29), however, 15 were identified to have been created from at least the mid-1970s to 2000, another 15 from 2001 to 2010, and 10 from 2011 to 2019. Forty-eight eHealth technologies were identified to currently exist, while 2 did not, and 1 was replaced by one of the 48, and for the remaining 18, their current existence was unclear. We found that 60 eHealth technologies had been used in any context outside of the authors’ study; for example, the technology or its data were cited in another research article not conducted by the developing authors. Thirty-two eHealth technologies were found to be available and entirely free to use by anyone, 12 are only accessible with a subscription, 1 was partially available without a subscription, required a partial-subscription, 3 were confirmed to be not available to the general public, and the status of the remaining 21 was unclear. eHealth technologies were developed by the following: companies (n=24), researchers or research groups (n=22) (11 of which by the authors of one or more of the eligible articles), government agencies/departments (n=17), botanical council (n=1), not-for-profit (n=1), practitioners (n=1), unclear (n=1). Additionally, 2 were developed by organizations that involved both researchers and government. Intended users of the eHealth technologies were not always clear, and we used our discretion in cases where this information was not provided explicitly. Our assessment was as follows: for healthcare providers (n=54), for researchers (n=36), for patients/public (n=32). These numbers reflect a large amount of overlap among these user types across many of the eHealth technologies. The details associated with all included eHealth technologies can be found in Table 2 of Appendix 3.
Findings from thematic analysis
In total, three main themes emerged from our analysis and are described below.
Obsolete reviews of CAM-related healthcare information
Upon accounting for all eligible articles, one immediate and striking finding was the fact that while a number of reviews have been published providing overviews or summaries of CAM-related healthcare or research resources, they have all been published in excess of one decade ago, with the exception of Xie et al. [41]‘s review, however it is only specific to natural product databases. The most recent reviews providing information on CAM, in general, were published approximately 15–20 years ago [25, 28, 32, 33, 48, 50, 56, 65]. As a result, the information contained within these articles is all, to varying extents, obsolete, including resources that are no longer available or updated. Furthermore, as these articles were published years before the methodologies of systematic or scoping reviews were published, many resources included in these reviews were found unsystematically or based on the authors’ knowledge.
Large number of databases
It was found that a large number of databases exist, primarily offered in website and/or mobile app formats, making up the largest category of types of eHealth technology in this scoping review (35 of 69). New databases have been created (and maintained) since the 1970s up to the present day, and their developers and content vary fairly widely. Perhaps unsurprisingly, the vast majority of databases developed by companies focus on the provision of resources for healthcare providers. These include a number of well-recognized, large companies in the healthcare industry, providing items such as monographs, clinical decision suites, dosing calculators and adverse event/interaction checkers in their respective databases [66,67,68,69,70,71]. In contrast, databases developed by government organizations or agencies collect information at the population level regarding pharmacovigilance and adverse events [49, 72, 73], though databases such as the Drug Product Database available on the Health Canada website also provides a search tool for drugs and certain natural health products available nationally with associated monographs. Interestingly, most databases developed by researchers or research groups emerge from Asia (notably China and the Republic of Korea). These databases serve a different purpose than the aforementioned company- and government-developed ones, instead housing information on traditional medicine (i.e. traditional Chinese medicine) ingredients such as interactions, mechanisms of action, compound structures, and their relationship to genes and diseases [30, 31, 39,40,41, 47, 55].
We did not formally assess the usability of these databases or the quality of the information contained within them, as this exceeded the scope of this scoping review. Despite this, it should be noted that initial impressions obtained simply by completing the data extraction step for this review indicated that these databases likely vary largely in quality, and the authors intend on assessing this in a future research study. The frequency of updates for each database is presented in Table 3 in Appendix 3; some of the most recent databases (updated and/or created within the last 3 years) are presented in Table 4 in Appendix 3.
Government adverse drug/event surveillance
We identified that the majority of adverse drug/event surveillance eHealth technologies including CAM identified were government initiated, and found across the following countries: China, India, the Republic of Korea, and the United States. These eHealth technologies are equipped with detection [34] and reporting systems [27, 31, 34, 74] and safety alerts [74, 75]. The countries with such government initiatives outside of the United States are unsurprising, given that a very large proportion of traditional and indigenous medical systems originate from these parts of the world, notably traditional Chinese and Korean medicine and Ayurvedic medicine [76]. Though a not-for-profit, as opposed to a government agency, our review also captured the Institute for Safe Medication Practices in Canada which runs a medication error reporting program and publishes newsletters, reports and safety alerts based on information received [77]. These government initiatives highlight the growing need to collect information surrounding CAM-related adverse events and side effects given they are widely used across the globe [78].
Discussion
The purpose of the present scoping review was to identify eHealth technologies that assist in identifying potential 1) adverse drug interactions with CAM, 2) adverse CAM-CAM interactions, or 3) standalone CAM adverse events or side effects. The amount of available literature on this topic as well as the number of eHealth technologies, while not overly voluminous, presents a broad range of different eHealth technologies that have emerged since the popularization of (and even before) the term “eHealth”. Given that, to our knowledge, this is the first study to present such eHealth technologies using a systematic search of the peer-reviewed and grey literature, it is hoped that these findings will provide both healthcare providers and researchers with an awareness of what research has taken place over the past few decades at the intersection of CAM and eHealth.
Resources for practitioners, researchers and patients: ample, but of unclear quality
This review also provides readers with a list of currently existing resources that they may not have been aware of to date, which may aid in their clinical practice or research. While these resources have been developed, evaluated, studied or assessed, at least to some degree, by academic researchers, this review was only designed to scope out the number of eHealth technologies and their key characteristics. Unfortunately, we did not find that any authors of included articles expressed an intention to create new upcoming eHealth technologies in this topic area, beyond improving their own existing resource. As expected, our scoping review captured some well-known and authoritative resources, such as Natural Medicines [69], MicroMedex [67] and the NCCIH’s Herbs at a Glance [79], however, some others may be less known and their quality may be questionable. Therefore, we encourage users of any of these resources to exercise caution and use their professional judgement when utilizing any of these resources, especially those which may be unfamiliar to them.
Areas identified for future research
We have identified a couple of areas for future research based on our findings.
Today there exists more information on the Internet about CAM and CAM-related adverse events and side effects than ever before, yet the quality of much of it is arguably questionable [80]. Clinicians, researchers, governments and policymakers, and patients alike all need resources that provide them with reliable, trustworthy, and current information. Combined with our finding that the vast majority of reviews on CAM-related healthcare or research resources are now decades old, this undoubtedly justifies a need for an updated review of CAM-related healthcare information given that many changes have occurred in the way in which both guidelines inform clinical practice and research methodologies have evolved.
While we did not formally assess the quality of the eHealth technologies (nor the information they contained), it was evident at face-value that they varied across eHealth technologies across all types, developers and content areas. We hypothesize that this may relate to the fact that little guidance exists in developing or evaluating CAM-related eHealth technologies, as the growth of research conducted in this area has been slow and the information limited. While there have been discussions surrounding the creation of comprehensive information resources about CAM, it appears that the most recent ones took place nearly two decades ago [81, 82], based on preliminary searches we conducted prior to finalizing our systematic search strategy. The development of CAM-related eHealth technologies should be viewed as a research method in itself similar to how guidelines for different study types exist [83]. As a result, additional and updated guidance documents are needed in creating eHealth technologies, let alone CAM-related ones, as to date only one appears to exist [84].
Strengths and limitations
Notable strengths of this study included the use of a comprehensive systematic search strategy to identify eligible articles, devised with the assistance of an experienced academic librarian. Interpretation of these findings was strengthened by the fact that all three authors independently screened, data extracted, and summarized the findings.
Limitations include the fact that this scoping review did not include non-English language articles, which perhaps would have been of importance given our finding that there is an emergence of new CAM-related eHealth technologies in Asia, among other countries. Additionally, it should be noted that many apps exist that likely also detect CAM-related adverse events or side effects which were not captured by this search. Though this is a limitation, it can be inferenced that higher-quality apps (or at least those that have been exposed to peer-review) would be those that would be captured in the published literature, which would be of greater use to healthcare providers and researchers as the primary audience of this review. Furthermore, a very large number of poor-quality apps exist on platforms such as the Google Play Store and the Apple App Store, and it would not be practical nor feasible to review them all.
Conclusion
The present scoping review involved a systematic search of the literature to identify eHealth technologies assisting in identifying potential 1) adverse drug interactions with CAM, 2) adverse CAM-CAM interactions, or 3) standalone CAM adverse events or side effects. Having identified 69 unique eHealth technologies that fall into this category, we provide a descriptive map of the literature on this area and highlight a number of key themes that emerged from our analysis. Additionally, we highlight that while an ample number of resources are available to healthcare providers, researchers, and patients, we caution that the quality and update frequency for many of these resources vary widely, and until formally assessed, remain unknown. Lastly, we identify that a need exists to conduct an updated and systematically-searched review of CAM-related healthcare or research resources, as well as develop guidance documents associated with the development and evaluation of CAM-related eHealth technologies.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
- CADTH:
-
Canadian Agency for Drugs and Technologies in Health
- CAM:
-
Complementary and alternative medicine
- CAHTS:
-
Computer-assisted history-taking systems
- CDSS:
-
Computerized decision support systems
- mHealth:
-
Mobile health
- NCCIH:
-
National Center for Complementary and Integrative Health
- NHP:
-
Natural health product
References
Fugh-Berman A. Herb-drug interactions. Lancet. 2000;355(9198):134–8.
Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Semin Integr Med. 2004;2(2):54–71.
Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompav M, et al. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA. 1998;280(18):1569–75.
Public Health Agency of Canada. Canada.ca: Government of Canada; 2019 [updated 2019 Dec 10; cited 2019 Dec 14]. Available from: http://www.phac-aspc.gc.ca/chn-rcs/cah-acps-eng.php.
Esmail N. Complementary and alternative medicine in Canada: trends in use and public attitudes, 1997-2006. Public Policy Sources. 2007;87:1–53.
Nahin RL, Barnes PM, Stussman BJ, Bloom B. Costs of complementary and alternative medicine (CAM) and frequency of visits to CAM practitioners: United States, 2007. Natl Health Stat Rep. 2009;(18):1–14.
Health Canada. Summary report on the consultation on a framework for consumer health products: what we heard [Internet]. Canada.ca: Government of Canada; 2016 [updated 2016 Apr 01; cited 2019 Dec 14]. Available from http://www.hc-sc.gc.ca/dhp-mps/consultation/natur/sum_chpf-som_cpsc-eng.php.
Ipsos Reid. Natural health product tracking survey - 2010 final report. Ottawa: Health Canada; 2011. 72 p. Available from http://epe.lac-bac.gc.ca/100/200/301/pwgsc-tpsgc/por-ef/health/2011/135-09/report.pdf.
Andersson ML, Böttiger Y, Lindh JD, Wettermark B, Eiermann B. Impact of the drug-drug interaction database SFINX on prevalence of potentially serious drug-drug interactions in primary health care. Eur J Clin Pharmacol. 2013;69(3):565–71.
Hammar T, Lidström B, Petersson G, Gustafson Y, Eiermann B. Potential drug-related problems detected by electronic expert support system: physicians’ views on clinical relevance. Int J Clin Pharm. 2015;37(5):941–8.
Apidi NA, Murugiah MK, Muthuveloo R, Soh YC, Caruso V, Patel R, et al. Mobile medical applications for dosage recommendation, drug adverse reaction, and drug interaction: review and comparison. Ther Innov Regul Sci. 2017;51(4):480–5.
Kim BY, Sharafoddini A, Tran N, Wen EY, Lee J. Consumer mobile apps for potential drug-drug interaction check: systematic review and content analysis using the mobile app rating scale (MARS). JMIR Mhealth and Uhealth. 2018;6(3):e74.
Larsen M, Rowntree J, Young A, Pearson S, Smith J, Gibson O, et al. Chemotherapy side-effect management using mobile phones. Conf Proc IEEE Eng Med Biol Soc. 2008;2008:5152–5.
Car J, Tan WS, Huang Z, Sloot P, Franklin BD. eHealth in the future of medications management: personalisation, monitoring and adherence. eHealth in the future of medications management: personalisation, monitoring and adherence. BMC Med. 2017;15(1):73.
Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69.
Daudt HM, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol. 2016;13(1):48.
Oh H, Rizo C, Enkin M, Jadad A. What is eHealth (3): a systematic review of published definitions. J Med Internet Res. 2005;7(1):e1.
Shaw T, Mcgregor D, Brunner M, Keep M, Janssen A, Barnet S. What is eHealth (6)? Development of a conceptual model for eHealth: qualitative study with key informants. J Med Internet Res. 2017;19(10):e324.
Ng JY, Boon HS, Thompson AK, Whitehead CR. Making sense of “alternative”, “complementary”, “unconventional” and “integrative” medicine: exploring the terms and meanings through a textual analysis. BMC Complement Altern Med. 2016;16(1):134.
National Center for Complementary and Integrative Health (NCCIH). Complementary, alternative, or integrative health: what's in a name? [Internet] U.S. Department of Health and Human Services; 2018 [updated 2018 Jul; cited 2019 Dec 14]. Available from: https://nccih.nih.gov/health/integrative-health.
Wieland LS, Manheimer E, Sampson M, Barnabas JP, Bouter LM, Cho K, et al. Bibliometric and content analysis of the Cochrane complementary medicine field specialized register of controlled trials. Syst Rev. 2013;2(1):51.
World Health Organization (WHO). Safety monitoring of medicinal products: guidelines for setting up and running a pharmacovigilance centre [Internet]. Geneva: World Health Organization and the Uppsala Monitoring Centre; 2000. [cited 2019 Dec 14]. Available from: https://www.who-umc.org/media/1703/24747.pdf.
Mitchell JG. From telehealth to e-health: the unstoppable rise of e-health. Canberra, A.C.T.: Commonwealth Department of Communications, Information Technology and the Arts; 1999.
Jackson EA, Kanmaz T. An overview of information resources for herbal medicinals and dietary supplements. J Herb Pharmacother. 2001;1(1):35–61.
Li C, Xia J, Deng J, Chen W, Wang S, Jiang J, et al. A web-based quantitative signal detection system on adverse drug reaction in China. Eur J Clin Pharmacol. 2009;65(7):729–41.
Zhang L. Pharmacovigilance of herbal and traditional medicines. Methods in pharmacology and toxicology evidence-based pharmacovigilance. New York: Humana Press; 2018. p. 37–65.
Motl SE, Timpe EM, Robinson M, Corsberg C, Phillips K. Health information web sites by therapeutic category for healthcare professionals. J Pharm Technol. 2004;20(2):106–18.
Chen YZ, Ung CY. Computer automated prediction of potential therapeutic and toxicity protein targets of bioactive compounds from Chinese medicinal plants. Am J Chin Med. 2002;30(1):139–54.
Chen X, Zhou H, Liu YB, Wang JF, Li H, Ung CY, et al. Database of traditional Chinese medicine and its application to studies of mechanism and to prescription validation. Br J Pharmacol. 2006;149(8):1092–103.
Woo Y, Hyun MK. Safety of herbal medicine for elderly patients with chronic disease in the Republic of Korea. Eur J Integr Med. 2019;30:100934.
Kiefer D, Shah S, Gardiner P, Wechkin H. Finding information on herbal therapy: a guide to useful sources for clinicians. Altern Ther Health Med. 2001;7(6):74–8.
Meyer JR, Generali JA, Karpinski JL. Evaluation of herbal–drug interaction data in tertiary resources. Hosp Pharm. 2004;39(2):149–60.
Ye X, Fu Z, Wang H, Du W, Wang R, Sun Y, et al. A computerized system for signal detection in spontaneous reporting system of Shanghai China. Pharmacoepidemiol Drug Saf. 2009;18(2):154–8.
Archer M, Proulx J, Shane-McWhorter L, Bray BE, Zeng-Treitler Q. Development of an alert system to detect drug interactions with herbal supplements using medical record data. AMIA Annu Symp Proc. 2014;2014:249–55.
Ogultarhan V, Shoshi A, Magnucki R, Kormeier B, Hofestädt R. KATIS: an eHealth system for complementary medicine. IOS Press Ebooks. 2016;223:167–73.
Clauson KA, Polen HH, Peak AS, Marsh WA, DiScala SL. Clinical decision support tools: personal digital assistant versus online dietary supplement databases. Ann Pharmacother. 2008;42(11):1592–9.
Fitzpatrick RB. Natural Standard Database. Med Ref Serv Q. 2010;29(2):154–65.
Yap KY, See CS, Kuo EY, Chui WK, Chan A. Utilizing mobile networks for the detection of clinically relevant interactions between chemotherapy regimens and complementary and alternative medicines. J Altern Complement Med. 2012;18(2):165–74.
Lee JH, Park KM, Han DJ, Bang NY, Kim DH, Na H, et al. PharmDB-K: integrated bio-pharmacological network database for traditional Korean medicine. PLoS One. 2015;10(11):e0142624.
Xie T, Song S, Li S, Ouyang L, Xia L, Huang J. Review of natural product databases. Cell Prolif. 2015;48(4):398–404.
Gregory PJ, Jalloh MA, Abe AM, Hu J, Hein DJ. Characterization of complementary and alternative medicine-related consultations in an academic drug information service. J Pharm Pract. 2016;29(6):539–42.
Olesen C, Harbig P, Barat I, Damsgaard EM. Absence of ‘over-the-counter’ medicinal products in on-line prescription records: a risk factor of overlooking interactions in the elderly. Pharmacoepidemiol Drug Saf. 2013;22(2):145–50.
Fischer JE, Crowell K, Curtis P. Complementary and alternative medical reference software for personal digital assistants: evidence of clinical applicability. Complement Health Pract Rev. 2005;10(1):57–72.
Kim E, Choi AS, Nam H. Drug repositioning of herbal compounds via a machine-learning approach. BMC Bioinformatics. 2019;20(S10):247.
Spanakis M, Sfakianakis S, Sakkalis V, Spanakis E. PharmActa: empowering patients to avoid clinical significant drug–herb interactions. Medicines. 2019;6(1):26.
Xu HY, Zhang YQ, Liu ZM, Chen T, Lv CY, Tang SH, et al. ETCM: an encyclopaedia of traditional Chinese medicine. Nucleic Acids Res. 2019;47(D1):D976–82.
Wootton JC. Directory of databases for research into alternative and complementary medicine. J Altern Complement Med. 1997;3(2):179–90.
Fucik H, Backlund A, Farah M. Building a computerized herbal substance register for implementation and use in the World Health Organisation international drug monitoring Programme. Drug Inform J. 2002;36(4):839–54.
Jackson EA. Resources for information on herbal medicinals and dietary supplements. J Herb Pharmacother. 2001;1(2):89–98.
Walker JB. Evaluation of the ability of seven herbal resources to answer questions about herbal products asked in drug information centers. Pharmacotherapy. 2002;22(12):1611–5.
Boddy K, Ernst E. Review of reliable information sources related to integrative oncology. Hematol Oncol Clin North Am. 2008;22(4):619–30.
Boehmer S, Karpa K. Evaluating the value of a web-based natural medicine clinical decision tool at an academic medical center. BMC Health Serv Res. 2011;11(1):279.
Faubert G, Lebe D, Bussières JF. A pilot study to compare natural health product–drug interactions in two databases in Canada. Pharm World Sci. 2010;32(2):179–86.
Sun Y, Shi S, Li Y, Wang Q. Development of quantitative structure-activity relationship models to predict potential nephrotoxic ingredients in traditional Chinese medicines. Food Chem Toxicol. 2019;128:163–70.
Sweet BV, Gay WE, Leady MA, Stumpf JL. Usefulness of herbal and dietary supplement references. Ann Pharmacother. 2003;37(4):494–9.
Tomasulo P. Natural standard–new integrative medicine database. Med Ref Serv Q. 2003;22(3):33–8.
Molassiotis A, Xu M. Quality and safety issues of web-based information about herbal medicines in the treatment of cancer. Complement Ther Med. 2004;12(4):217–27.
Gao P, Zhang CL, Zeng FD, Pu R, Zhang J, Huang R, et al. Pharmacovigilance in China: issues of concern identified through an analysis of the Chinese adverse drug reaction information bulletin 2001 to 2014. J Clin Pharm Ther. 2015;40(5):594–8.
Brink SG, Mcfarren AE, Lincoln JM, Birney AJ. Cancer CAM™: web-based continuing education for health professionals. Complement Health Pract Rev. 2004;9(1):43–60.
Hamre HJ, Glockmann A, Heckenbach K, Matthes H. Use and safety of anthroposophic medicinal products: an analysis of 44,662 patients from the EvaMed Pharmacovigilance network. Drugs Real World Outcomes. 2017;4(4):199–213.
Tabali M, Ostermann T, Jeschke E, Witt CM, Matthes H. Adverse drug reactions for CAM and conventional drugs detected in a network of physicians certified to prescribe CAM drugs. J Manag Care Pharm. 2012;18(6):427–38.
Yao Y, Wang Z, Li L, Lu K, Liu R, Liu Z, et al. An ontology-based artificial intelligence model for medicine side-effect prediction: taking traditional Chinese medicine as an example. Comput Math Methods Med. 2019;2019:1–7.
Ee RW, Yap KZ, Yap KY. Herbopolis – a mobile serious game to educate players on herbal medicines. Complement Ther Med. 2018;39:68–79.
Allais G, Voghera D, Lorenzo CD, Mana O, Benedetto C. Access to databases in complementary medicine. J Altern Complement Med. 2000;6(3):265–74.
Clinical Pharmacology. Clinical pharmacology [Internet]. Elsevier Gold Standard [cited 2019 Dec 14]. Available from: https://www.clinicalpharmacology.com/.
IBM Watson Health Products. Micromedex web applications access [Internet]. Armonk: IBM Corporation; 2019. [cited 2019 Dec 14]. Available from: https://www.micromedexsolutions.com/home/dispatch/ssl/true.
Lexicomp. Lexi-natural products. Alphen aan den Rijn: Wolters Kluwer Clinical Drug Information, Inc; 2019. [cited 2019 Dec 14]. Available from: http://webstore.lexi.com/Store/Individual-Databases/Lexi-Natural-Products.
Therapeutic Research Center. Natural medicines. Stockton: Therapeutic Research Center; 2019. [cited 2019 Dec 14]. Available from: https://naturalmedicines.therapeuticresearch.com/.
MedicinesComplete. Herbal medicines. London: The Royal Pharmaceutical Society; 2019. [cited 2019 Dec 14]. Available from: https://about.medicinescomplete.com/publication/herbal-medicines.
PEPID. Clinical decision support. Phoenix: PEPID; 2019. [cited 2019 Dec 14]. Available from: https://www.pepid.com/.
Interaktionsdatabasen Danish Medicines Agency. Interaktionsdatabasen.dk [Internet]. [cited 2019 Dec 14]. Available from: http://www.interaktionsdatabasen.dk/.
Uppsala Monitoring Centre. Vigibase. Swedan: WHO Collaborating Centre for International Drug Monitoring; 2019. [cited 2019 Dec 14]. Available from: https://www.who-umc.org/vigibase/vigibase/.
U.S. Food and Drug Administration (FDA). Center for Food Safety and Applied Nutrition (CFSAN) [Internet]. Silver Spring: FDA; 2018. [updated 2018 Sept 19; cited 2019 Dec 14]. Available from: https://www.fda.gov/about-fda/office-foods-and-veterinary-medicine/center-food-safety-and-applied-nutrition-cfsan.
U.S. Food and Drug Administration (FDA). Medical product safety information [Internet]. Silver Spring: FDA; 2019. [updated 2019 Dec 12; cited 2019 Dec 14]. Available from: https://www.fda.gov/safety/medwatch-fda-safety-information-and-adverse-event-reporting-program/medical-product-safety-information.
World Health Organization (WHO). WHO global report on traditional and complementary medicine 2019. Geneva: World Health Organization; 2019. [cited 2019 Dec 14]. Retrieved from https://www.who.int/traditional-complementary-integrative-medicine/WhoGlobalReportOnTraditionalAndComplementaryMedicine2019.pdf?ua=1.
Institute For Safe Medication Practices. About us [Internet]. Horsham: Institute for Safe Medication Practices; 2019. [cited 2019 Dec 14]. Available from: https://www.ismp.org/about.
Ekor M. The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Front Pharmacol. 2014;4:177.
National Center for Complementary and Integrative Health. Herbs at a glance [Internet]. Bethesda: U.S. Department of Health and Human Services; 2019. [updated 2019 Jun 20; cited 2019Dec14]. Available from: https://nccih.nih.gov/health/herbsataglance.htm.
Scarton LA, Del Fiol G, Treitler-Zeng Q. Completeness, accuracy, and presentation of information on interactions between prescription drugs and alternative medicines: an internet review. Stud Health Technol Inform. 2013;192:841–5.
Kronenberg F, Molholt P, Zeng ML, Eskinazi D. A comprehensive information resource on traditional, complementary, and alternative medicine: toward an international collaboration. J Altern Complement Med. 2001;7(6):723–9.
Richardson J. Building CAM databases: the challenges ahead. J Altern Complement Med. 2002;8(1):7–8.
The EQUATOR Network. Your one-stop-shop for writing and publishing high-impact health research [Internet]. Headington: UK EQUATOR Centre; 2019. [cited 2019 Dec 14]. Available from: https://www.equator-network.org/.
Baker TB, Gustafson DH, Shaw B, Hawkins R, Pingree S, Roberts L, et al. Relevance of CONSORT reporting criteria for research on eHealth interventions. Patient Educ Couns. 2010;81:S77–86.
Chen YZ, Zhi DG. Ligand–protein inverse docking and its potential use in the computer search of protein targets of a small molecule. Proteins Struct Funct Genet. 2001;43:217–26.
Acknowledgements
We gratefully acknowledge librarian Laura Banfield for providing guidance in constructing the search strategy. JYN was awarded a Research Scholarship and an Entrance Scholarship from the Department of Health Research Methods, Evidence and Impact, Faculty of Health Sciences at McMaster University.
Funding
This study was not funded.
Author information
Authors and Affiliations
Contributions
JYN: conceptualized and designed the study, collected the data, interpreted and analysed the data, drafted the manuscript, and gave final approval of the version to be submitted. MM: collected the data, interpreted and analysed the data, provided contributions and critically revised the manuscript, and gave final approval of the version to be submitted. VM: collected the data, interpreted and analysed the data, provided contributions and critically revised the manuscript, and gave final approval of the version to be submitted. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study involved a systematic search of the literature only; it did not require ethics approval or consent to participate.
Consent for publication
All authors consent to this manuscript’s publication in the order in which the authors are listed in the cover sheet.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Sample Search Strategy
MEDLINE Search Strategy for Scoping Review of eHealth Technologies Assisting in Identifying Potential 1) Adverse Drug Interactions with CAM, 1) Adverse CAM-CAM Interactions or 3) Standalone CAM Adverse Events or Side Effects Executed November 6, 2019
Database: Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Daily and Versions(R) <1946 to November 05, 2019> Search Strategy: | |
1 ((Alternative or Traditional or Complementary or Integrat*) adj2 (Therap* or Medicine*)).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] (103649) 2 Complementary Therapies/ or Integrative Medicine/ or exp Medicine, East Asian Traditional/ or exp Medicine, Chinese Traditional/ or exp Herbal Medicine/ or exp Plants, Medicinal/ or exp Phytotherapy/ or exp Drugs, Chinese Herbal/ or exp Medicine, Ayurvedic/ (151984) 3 (CAM or TCM or Traditional Chinese Medicine or Ayurved* or Medicinal Plant* or Herbalism).mp. (69971) 4 (Herb* adj1 (Medic* or Therap* or Supplement*)).mp. (23276) 5 or/1-4 (248865) 6 (Telemedicine or Telehealth or eHealth or e-Health or mHealth or m-Health or Mobile Health or Health Records, Personal or Mobile Application* or E-Prescription* or Electronic Prescri* or Electronic Health Record* or Electronic Medical Record* or Medical Records System* or Health Informatics or Medical Informatics or Computeri?ed Decision Support or Data Mining or Decision Support System* or Wearable Electronic Device* or Wearable Technolog* or Smartphone or Iphone or I-phone or Android or Handheld Computer or Personal* Digital or Deep Learning or Artificial Intelligence).mp. (166979) 7 Telemedicine/ or Health Records, Personal/ or Mobile Applications/ or Electronic Prescribing/ or Medical Records Systems, Computerized/ or Medical Informatics/ or Drug Therapy, Computer-Assisted/ or Drug Information Services/ or Hospital Information System/ or Computing Methodologies/ or Wearable Electronic Devices/ or Artificial Intelligence/ or "Neural Networks (Computer)"/ (112744) 8 or/6-7 (199016) 9 5 and 8 (1157) 10 limit 9 to (english language and yr="1995 -Current") (815) *************************** |
Appendix 2
Appendix 3
Data Extraction Tables
Table 1
Table 2
Table 3
Table 4
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ng, J.Y., Mooghali, M. & Munford, V. eHealth technologies assisting in identifying potential adverse interactions with complementary and alternative medicine (CAM) or standalone CAM adverse events or side effects: a scoping review. BMC Complement Med Ther 20, 239 (2020). https://doi.org/10.1186/s12906-020-02963-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-020-02963-y