Abstract
Background
Colorectal cancer imposes threats to patients’ well-being. Although most physical symptoms can be managed by medication, psychosocial stressors may complicate survival and hamper quality of life. Mindfulness and Qigong, two kinds of mind-body exercise rooted in Eastern health philosophy, has been found effective in symptoms management, improving mental health, and reducing stress. With these potential benefits, a randomized controlled trial (RCT) is planned to investigate the comparative effectiveness of mindfulness and Baduanjin intervention on the bio-psychosocial wellbeing of people with colorectal cancer.
Methods/ design
A 3-arm RCT with waitlist control design will be used in this study. One hundred eighty-nine participants will be randomized into (i) Mindfulness, (ii) Baduanjin, or (iii) waitlist control groups. Participants in both the Baduanjin and mindfulness groups will receive 8-weeks of specific intervention. All three groups will undergo four assessment phases: (i) at baseline, (ii) at 4-week, (iii) at 8-week (post-intervention), and 6-month post-intervention (maintenance). All participants will be assessed in terms of cancer-related symptoms and symptom distress, mental health status, quality of life, stress level based on physiological marker.
Discussion
Based on prior research studies, participants in both the mindfulness and Baduanjn intervention group are expected to have better symptoms management, lower stress level, better mental health, and higher level of quality of life than the control group. This study contributes to better understanding on the common and unique effectiveness of mindfulness and Baduanjin qigong, as such patients and qualified healthcare professionals can select or provide practices which will produce maximum benefits, satisfaction, adherence, and sustainability.
Trial registration
The trial has been registered in the Clinical Trials Centre of the University of Hong Kong (HKCTR-2198) on 08 March 2017.
Similar content being viewed by others
Background
Colorectal cancer imposes threats to patients’ well-being. Although most physical symptoms can be managed by medication, psychosocial stressors may complicate survival and hamper quality of life [1]. People with colorectal cancer, especially those with colostomy, often experience psychosocial distresses such as depression, fear of relapse, altered self-image, and loss of social functioning and connections [2]. A recent study proposed reciprocity between physical symptoms and psychosocial stresses in cancer patients [3]. Studies in psycho-immunology have suggested that many cancer patients also have depressive symptoms and experience sleep disturbance, the latter of which can be a risk factor for depression and disease progression among cancer patients [4]. In addition, a survival study highlighted the connection between survival and depression, anxiety, and quality of life in patients with colorectal cancer [5]. Given the potential effects of psychosocial well-being on colorectal cancer survivorship, there is a need for psychosocial support that targets the reciprocal mind-body relationship in these patients.
The past two decades have witnessed the proliferation of rigorous empirical testing of cancer-related psychosocial interventions, such as cognitive-behavioral therapies, psycho-educational interventions, social support groups, and mindfulness-based programs [6,7,8,9,10]. Mind-body practices, such as relaxation training, meditation, qigong (also known as Chi-Gong), yoga, taiji (also known as tai chi), and biofeedback have been found to improve functioning; reduce treatment-related nausea, vomiting, and physical pain; and improve mood and quality of life [11, 12]. Mindfulness and qigong practice in particular have become increasingly popular because they are coupled with marked evidence pertaining to safety, feasibility, and effectiveness on various aspects of health in cancer patients.
Mindfulness and qigong as mind-body practices for cancer
The practice of mindfulness focuses on the development of awareness of emotions and sensations, the nurturing of a nonjudgmental mindset, and self-acceptance through practice [13]. The here-and-now orientation of mindfulness has been found to be effective in moderating cancer-related stressors, such as attribution of cancer, regrets about past life decisions, suffering of pain, loss, and grief regarding one’s own impending death [9, 10]. In a randomized, waitlist-controlled trial, the participants in the mindful meditation-based program resulted in less mood disturbance, tension, stress, and depressive symptoms and improved sleep and gastrointestinal symptoms after the intervention and at the 6-month follow-up visit, when compared with the control group [14]. Mindfulness meditation was also found to be effective in altering cortisol and immune patterns consistent with lower stress with sustainable effects at the 1-year follow-up visit [15]. Local studies on the application of mindfulness in a cancer population are rare, but the results of studies on the effects of mindfulness on chronic pain, psychiatric symptoms, and functioning are promising [16, 17].
Similar to mindfulness practice in its emphasis on practicing breath-centering techniques and developing awareness of emotions and sensations, qigong is a mild form of muscular activity accompanied by introspective and proprioceptive focus and an awareness of the flow of intrinsic energy, which is essential in the pursuit of health and well-being [18, 19]. Of all types of qigong practices, Baduanjin is the most popular. The practice of Baduanjin comprises eight movements and requires relatively little cognitive and physical effort [20], which makes it a popular form of exercise for people who are physically weak, including older adults and cancer patients during rehabilitation [21, 22]. In support of its positive effects in cancer patients, a systematic review of 13 randomized controlled trials concluded that the practice of qigong improves cancer-specific quality of life, fatigue, and immune functioning; alters cortisol levels [23]; and alleviates sleep disturbance [24], which is also a common issue among cancer patients.
Although they share the common components of breath-centering practice, mindfulness and qigong represent two very distinct approaches to mind-body practices. Mindfulness meditation is a technique used to cultivate the mind’s ability to influence bodily functions and symptoms by means of focused-awareness training [12], whereas qigong capitalizes on movement and attention to foster the mind-body connection via the physical body [20, 25, 26]. The foregoing review suggests how most studies on mindfulness and qigong have examined their effects independently, which calls for comparative intervention research to elucidate how such similar, yet contrasting, approaches to mind-body practices compare in terms of their psychosocial and physiological benefits and patient compliance.
Diurnal Cortisol rhythm and cancer
There is a physio-psychological basis for the prognosis of colorectal cancer. Studies have indicated that dysfunction of the HPA axis is associated with tumor characteristics and survival in these patients [27,28,29]. Salivary cortisol is a neuroendocrine indicator of the HPA axis, which is an established and reliable physiological marker for stress-related improvements after mindfulness and qigong practices [30, 31]. Understanding the changes in cortisol profiles after mindfulness and qigong practices can further elucidate the link between mind-body practices and patients’ total well-being.
Study design
To explore the comparative effectiveness of mindfulness meditation and Baduanjin qigong practice, this study will adopt a three-armed randomized-controlled study design with two experimental groups and a waitlist control group.
Research objectives and study hypotheses
The first main objective of this study is to independently examine the effectiveness of mindfulness meditation and Baduanjin qigong in Chinese patients with colorectal cancer compared with controls regarding cancer-related symptoms and symptom distress, mental health, quality of life, biomarkers, and mindfulness level. The other main objective is to examine the similarities and differential effectiveness of a movement-based (Baduanjin qigong) and a mind-based (mindfulness meditation) practice on the preceding outcomes, the magnitude and pace of change, and extended compliance throughout the 8-month study. The final objective is to examine the relationships among the physical, psychological, and psychophysical variables and their effects on mind and body. This study envisions that advancing relationships change over time.
To achieve the aforementioned research objectives, the following hypotheses are proposed.
-
1.
Baduanjin qigong is more effective than no-intervention control in (i) reducing cancer-related symptoms and symptom distress, (ii) improving mental health, (iii) enhancing quality of life, (iv) positively altering biomarkers, and (v) enhancing mindfulness levels;
-
2.
Mindfulness meditation is more effective than no-intervention control in similar areas and directionality as in the preceding (i)-(v);
-
3.
Similarities and differences exist between mindfulness meditation and Baduanjin qigong in (i) the type of outcome variables, (ii) the magnitude of change, (iii) the time when significant outcomes emerge, and (iv) the frequency and duration of self-practice and long-term compliance; and
-
4.
The associations among physical and psychological variables and psychophysiological biomarkers and the changes of such associations across the time points are exploratory.
Methods
Study setting
This study will adopt a three-armed randomized-controlled trial design with a waitlist control group. Eligible participants will be recruited from the community via networks of colorectal cancer self-help groups and local cancer support networks.
Eligibility criteria
Chinese-speaking patients 18 years of age or older with a diagnosis of primary colorectal cancer of any stage between 0 and III and an expected survival duration of 12 months or longer who completed their main cancer treatment within the past 6 months to 5 years will be invited to participate in the trial. Those who regularly practice Baduanjin, mindfulness meditation, or other forms of qigong, tai chi, meditation, or yoga once a week or more during the past 6 months will be excluded. Those with severe cachexia, dizziness, bone pain, nausea, significant orthopedic problem, or other contraindication to mild to moderate physical exertion, or a diagnosis of a major medical or psychiatric disorder other than cancer, will also be excluded, as will patients with recurrent colorectal cancer or other cancers.
Participants, interventions, and outcomes
Both intervention groups will consist of eight weekly sessions (90-min each), with a total of 12 contact hours. Interventions will be held in groups of about 10 participants led by two trainers qualified in the respective intervention form, one of whom will also be a mental health professional.
-
a)
The Baduanjin qigong intervention will consist of eight sequential forms of movements practiced with guidance on rhythmic breathing and mindful awareness. Each cycle of the eight movements requires 10 to 15 min to complete. Four cycles will be practiced in each session, with short breaks arranged between them. In addition to the in-session practices, the participants will be encouraged to practice Baduanjin qigong for at least 20 min each day and to keep a record of their daily practice in a log book.
-
b)
The mindfulness meditation intervention is based on the core components of the established Mindfulness-Based Stress Reduction and Mindful Self-Compassion programs with adaptation for local practice. The focus of the group will be to nurture mindful awareness, acceptance, and self-compassion. The group sessions will be composed of a combination of mindfulness-based practice, relaxation, and yoga exercise. The basic philosophy of this intervention is to emphasize the nurturing of self-kindness and a detached attitude towards interpersonal connectedness and letting go of self-criticism, the need for control, and defensive separation in times of adversity. Adjuvant to the in-session practices, the participants will be recommended to practice the mindfulness techniques for at least 20 min each day and to keep a record of their practice.
-
c)
The waitlist control group members will continue with routine care and can join either the Baduanjin or mindfulness intervention after the 6-month post-intervention assessment.
Sample size
Overall, 189 participants will be required to achieve the study objectives. To achieve a statistical power of 0.8 with a medium effect size (f2 = 0.25) and a significance level of 0.05 in repeated-measures multivariate analysis of variance under the proposed three-group, four-time-point design, a sample size of 126 will be needed. Assuming an attrition rate of about 33.5%, based on prior trials on cancer patients using qigong [32], a total of 189 participants (63 per arm) will be required.
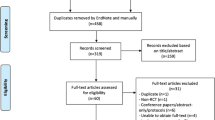
Recruitment strategy
Subjects will be recruited via referral from oncologists and from local colorectal cancer support networks by means of electronic mailing lists, printed promotional materials, and newsletters. Figure 1 illustrates the recruitment strategy, treatment received by the intervention group, the waitlist control condition, and the data collection time points of the study.
Assignments of interventions
A trained research assistant with a background in psychology or social work will be responsible for enrolling and contacting potential participants over the phone to conduct a screening interview. All eligible participants will be assigned a participant number and will be randomly assigned to one of the study conditions on 1:1:1 ratio using computer-generated random numbers generated by another research assistant on the study team.
Data collection, management, and analysis
After screening for inclusion and exclusion criteria, participants will be invited to visit the Centre for baseline data collection 1 week before the first group session. Participants from all three arms will be assessed at four time points: at baseline, at the midpoint of the intervention, after the intervention, and at 6-month follow-up.
Outcome measures
Assessments will pertain to several areas: (i) cancer-related symptoms and symptom distress, (ii) mental health, (iii) quality of life, (iv) biomarkers, (v) mindfulness, (vi) compliance, and (vii) demographic and clinical details. Self-rated scales and salivary cortisol will be collected from the participants, and blood pressure will be measured by the trained research assistant blinded to the randomization. Measurements will be taken at all time points, with the exception of demographic and clinical details.
Cancer-related symptom, symptom distress, and quality of life
-
(a)
Sleep quality. Quality of sleep will be indexed by the Chinese version of the Pittsburgh Sleep Quality Index (PSQI) [33]. The locally validated Chinese version of the PSQI is a self-report questionnaire that assesses multiple dimensions of sleep over the past month. The 19-item scale generates 7 component scores: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction. The sum of the seven component scores yields one global score of subjective sleep quality.
-
(b)
Cancer-related symptom distress. Cancer-related symptom distress is measured with the Chinese version of Memorial Symptom Assessment Scale (MSAS) [34]. The scoring of the 32-item MSAS yields a MSAS Global Distress Index (10 items) to measure overall symptom distress, a Physical Symptom Subscale score (12 items), a Psychological Symptom Subscale score (6 items), and a total MSAS score.
-
(c)
Health-related quality of life. Health-related quality of life will be assessed with the Chinese (HK) Short form-12 (SF-12) [35]. With 12 items, the scale yields a physical and a mental health summary.
-
(d)
Anxiety and depressive symptoms. Anxiety and depressive symptoms will be captured by the Cantonese/Chinese version of the Hospital Anxiety and Depression Scale (HADS) [36]. The 14-item scale consists of two subscales (anxiety and depression) of 7 items each, and the items are scored on a 4-point Likert-type scale (0-3).
-
(e)
Perceived stress. Perceived stress levels will be assessed by the Chinese Perceived Stress Scale (CPSS) [37]. Using a 5-point Likert scale (0-4), the scale consists of 10 items regarding the degree to which life events are appraised as stressful.
-
(f)
Salivary cortisol. Salivary cortisol collection will be conducted by the participants themselves. Saliva samples will be collected at five prescribed times (upon awakening, 45 min after awakening, 12:00 pm, 5:00 pm, and 9:00 pm) using a collection device, i.e., Salivette, that includes a cotton swab to place under the tongue. Smoking, eating, and drinking should be avoided for 1 h before saliva collection. The samples will be kept frozen at −20 °C. Measures of the participants’ health behaviors and activities on the day of saliva collection will be collected along with the cortisol level, including (i) sleep quantity that day (hours of sleep at night and nap hours), (ii) subjective sleep quality rated on a scale of 1-10, (iii) smoking habit and the number of cigarettes that day, (iv) alcohol/coffee drinking habit and the approximate amount that day, and (v) subjective evaluation of stress levels on the day of collection rated on a scale of 1-10. The preceding measures can affect the diurnal cortisol rhythm and must be considered in our analysis.
-
(g)
Blood pressure and heart rate. Following recommended procedures by the Canadian Medical Association [38], blood pressure and heart rates will be measured twice on each arm with a 5-min rest intervals between measurements, and the four collected readings will be averaged.
-
(h)
Mindfulness. The 20-item Chinese Five Facet Mindfulness Questionnaire (Short form) will be used [39]. The scale covers five mindfulness-related domains—observing, describing, acting with awareness, non-judgment of inner experience, and non-reaction to inner experience—on a 5-point Likert scale.
-
(i)
Compliance. The participants will record their daily duration of qigong or mindfulness meditation practice over the course of the study. This will provide information on the frequency and intensity of practice and the maintenance of self-practice habits after the intervention period.
-
(j)
Demographics. The participants’ sociodemographic data, such as age, gender, education level, employment status, and marital status, and their clinical profile, including cancer diagnosis, staging, treatment and medication record, onset of mood disturbances if any, critical events around the time of onset, physical exercise habits, complementary treatment used, and psychosocial support service use, will be self-reported.
Data management
Data entry will be conducted by a clerical staff trained in research data entry. All participants will be assigned a participant number, and all data will be stored in an onsite server accessible only to the research team members. A range check will be performed for data values.
Data analysis
To assess the effectiveness of Baduanjin qigong and mindfulness meditation, analysis of variance and chi-square independence tests will be carried out using SPSS to compare the demographic profiles of the three groups. The study will use latent growth modeling in Mplus 7 to explore the effectiveness of the two mind-body interventions over the four assessment time points, between the respective experimental and waitlist control groups. Traditional analytic techniques such as analysis of variance adopt traditional deletion or substitution methods and may not yield precise estimates in the presence of missing data. Latent growth modeling flexibly analyzes the overall population trajectories using nonlinear modeling such as quadratic growth and the between-person variation in outcome variables, thus allowing analysis of all available data via full information maximum likelihood under missing-at-random assumption. This matches the standard intent-to-treat analytic approach of clinical trials with missing data. The level of statistical significance (p) will be set at 0.05, and p values greater than 0.05 but less than 0.10 will be considered to indicate marginal significance. All models will be estimated using the robust maximum likelihood estimator.
To examine the similarities and differential effectiveness of Baduanjin qigong and mindfulness meditation, the treatment effects of the two interventions will be compared directly in multigroup conditional growth models. The linear slope factors of the outcomes will be contrasted across the two intervention groups by computing the difference in the intercepts of the slope factors between the two groups using the model constraint option. The demographic and clinical characteristics that differ significantly across the three groups in the preliminary analysis will be entered as covariates. Influential confounding variables such as the clinical prognosis or the frequency, intensity, and duration of maintenance (compliance) of practice will be controlled.
With baseline data from both the experimental and control groups, correlation analyses will be performed to understand the relationships between the parameters that reflect the mind and body, which include diurnal cortisol patterns, subjective stress, and assessments of psychological symptoms, sleep patterns, and health-related quality of life. Changes in those associations across time can be analyzed by latent growth modeling using Mplus.
The saliva samples will be centrifuged at 3000 rpm for 15 min at room temperature. Cortisol levels will be determined with an enzyme-linked immunosorbent assay kit (Salimetrics, Inc.) in the HKU Clinical Oncology Lab. The assay sensitivity is 0.193 nmol/l, and the intra-assay and inter-assay coefficients of variation are 3 and 10%, respectively. Due to the skewed distribution of salivary cortisol data, a natural logarithm will be used to transform the raw cortisol data to yield an unskewed distribution for analysis. The mean of the five daily cortisol levels will be used, and the total cortisol level will be measured by the area under the curve. To explore the individual trajectories of changes in the cortisol level over time and the complex relationships between different variables, a two-level individual growth curve model using Mplus software will be adopted as cortisol measures at five daily time points are nested within participants. This method is a variant of multiple regression modeling that is appropriate for the nested structure of our data.
Discussion
Despite the growing family of mind-body practices, few studies juxtaposed their differential outcomes, magnitude and pace of change and post-intervention compliance. Therefore, using a comparative randomized-controlled trial, this study is set out to further establish mind-body practices in psychosocial oncology by exploring the contrasting approaches with which qigong and mindfulness meditation exert their influences. This study will measure both physiological and psychological outcomes which offer a comprehensive understanding on the mental and bodily changes before, during, after each approach and their maintenance. Examining the effects of mind-body practices on circadian cortisol rhythm may shed light on the homeostatic effect of mind-body practices on the dysregulation of the HPA system. Better understanding on culturally popular interventions, in particular, the common and unique effectiveness of different approaches are crucial, as patients and qualified healthcare professionals can select or provide practices which will produce maximum benefits, satisfaction, adherence, and sustainability.
References
Zebrack BJ, Ganz PA, Bernaards CA, Petersen L, Abraham L. Assessing the impact of cancer: development of a new instrument for long-term survivors. Psycho-Oncology. 2006;15(5):407–21.
Phelan SM, Griffin JM, Jackson GL, Zafar SY, Hellerstedt W, Stahre M, Nelson D, Zullig LL, Burgess DJ, van Ryn M. Stigma, percieved blame, self-blame, and depressive symptoms in men with colorectal cacner. Psycho-Oncology. 2013;22(1):65–73.
Onitilo AA, Nietert PJ, Egede LE. Effect of depression on all-cause mortality in adults with cancer and fiffernetial effects by cancer site. Gen Hosp Psychiatry. 2006;28(5):396–402.
Irwin MR, Olmstead RE, Ganz PA, Hague R. Sleep disturbance, inflammation and depression risk in cancer survivors. Brain Behav Immun. 2013;30:S58–67.
Sharma A, Greenman J, Sharp DM, Walker LG, Monson JRT. Vascular endothelial growth factor and psychosocial factors in colorectal cancer. Psycho-Oncology. 2008;27:66–73.
Schou B, Kåresen R, Smeby NA, Espe R, Sørensen EM, Amundsen M, Aas H, Ekeberg Ø. Effects of a psychoeducational versus a support group intervention in patients with early-stage breast cancer: results of a randomized controlled trial. Cancer Nurs. 2014;37(3):198–207.
Chan CL, Ho RT, Lee PW, Cheng JY, Leung PP, Foo W, Chow LW, Sham JS, Spiegel D. A randomized controlled trial of psychosocial interventions using the psychophysiological framework for Chinese breast cancer patients. J Psychosoc Oncol. 2006;24:3–26.
Barsevick AM, Sweeney C, Haney E, Chung E. A systematic qualitative analysis of psychoeductional interventions for depression in patients with cancer. Oncol Nurs Forum. 2002;29(1):73–84.
Piet J, Würtzen H, Zachariae R. The effect of mindfulness-based therapy on symptoms of anxiety and depression in adult cancer patients and survivors: a systematic review and meta-analysis. J Consult Clin Psychol. 2012;80(6):1007–20.
Carlson L. Mindfulness-based cancer recovery: the development of an evidence-based psychosocial oncology intervention. Oncol Exchange. 2013;12(2):21–5.
Elkin G, Fisher W, Johnson A. Mind-body therapties in integrative oncology. Curr Treat Options in Oncol. 2010;11(3-4):128–40.
Astin JA, Shapiro SL, Elsenberg DM, Forys KL. Mind-body medicine: state of the science, impflications for practice. J Am Board Fam Pract. 2003;16(2):131–47.
Kabat-Zinn J. Some reflections on the origins of MBSR, skillful means, and the trouble with maps. Contemporary Buddhism. 2011;12(1):281–306.
Speca M, Carlson L, Goodey E, Angen M. A randomized, wait-list controlled clinical trial: the effects of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosom Med. 2000;62:613–22.
Carlson L, Speca M, Faris P, Patel KD. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav Immun. 2007;21(8):1038–49.
Chien WT, Thompson DR. Effects of a mindfulness-based psychoeducation programme for Chinese patients with schizophrenia: 2-year follow-up. Br J Psychiatry. 2014;205(1):52–9.
Wong SY, Chan FW, Wong RL, Chu MC, Lam KYY, Mercer SW, Ma SH. Comparing the effectiveness of mindfulness-based stress reduction and multidisciplinary intervention programs for chronic pain: a randomized comparative trial. Clin J Pain. 2011;27(8):724–34.
Jahnke R, Larkey L, Rogers C, Etnier J, Lin F. A comprehensive review of health benefits of qigong and tai chi. Am J Health Promot. 2010;24(6):e1–e25.
La Forge R. Aligning mind and body: exploring the discipline sof mindful exercise. ACSMs Health Fit J. 2005;9(5):7–14.
Chow YYY, Tsang HWH. Biopsychosocial effects of qigong as a mindful exercise for people with anxiety disorders: a speculative review. J Alternative Complement Med. 2007;13(8):831–40.
Tsang HW, Chan EP, Cheung WM. Effects of mindful and non-mindful exercises on people with depression: a systematic review. Br J Clin Psychol. 2008;47(3):303–22.
Molassiotis A, Fernadez-Ortega P, Pud D, Ozden G, Scott JA, Panteli V, Margulies A, Browall M, Magri M, Selvekerova S, et al. Use of complementary and alternative medicine in cancer patients: a European survey. Ann Oncol. 2005;16(4):655–63.
Zeng Y, Luo T, Xie H, Huang M, Cheng AS. Health benefits of qigong or tai chi for cancer patients: a systematic review and meta-analyses. Complement Ther Med. 2014;22(1):173–86.
Chen MC, Liu HE, Huang HY, Chiou AF. The effect of a simple traditional exercise program (Baduanjin exercises) on sleep quality of older adults: a randomized controlled trial. Int J Nurs Stud. 2012;49(3):265–73.
Ho RTH, Chan JSM, Wang CW, Lau BW, Kwok FS, Yuen LP, Sham JS, Chan CLW. A randomized controlled trial of qigong exercise on fatigue symptoms, functioning, and telomerase activity in persons with chronic fatigue or chronic fatigue syndrome. Ann Behav Med. 2012;44(2):160–70.
Chan JSM, Ho RTH, Chung KF, Wang CW, Yao TJ, Ng SM, Chan CLW. Qigong exercise alleviates fatigue, anxiety, and depressive symptoms, improves sleep quality, and shortens sleep latency in persons with chronic fatigue syndrome-like illness. Evid Based Complement Alternat Med. 2014;2014:1–10.
Lévi F, Dugué PA, Innominato P, Karaboué A, Dispersyn G, Parganiha A, Giacchetti S, Moreau T, Focan C, Waterhouse J, et al. Wrist actimetry circadian rhythm as a robust predictor of colorectal cancer patients survival. Chronobiol Int. 2014;31(8):891–900.
Mormon MC, Bogdan A, Cormont S, Touitou Y, Lévi F. Cortisol diurnal variation in blood and saliva of patients with metastatic colorectal cancer: relevance for clinical outcome. Anticancer Res. 2002;22(2B):1243–9.
Tsigos C, Chrousos GP. Hypothalamic-pituitary-adrenal axis, neurodocrine factors and stress. J Psychosom Res. 2002;53(4):865–71.
Matousek RH, Dobkin PL, Pruessner J. Cortisol as a marker for improvement in mindfulness-based stress reduction. Complement Ther Clin Pract. 2010;16(1):13–9.
Tsang HWH, Fung KM. A review on neurobiological and psychological mechanisms underlying the anti-depressive effect of qigong exercise. J Health Psychol. 2008;13(7):857–63.
Oh B, Butom P, Mullan B, Clarke S, Beale P, Pavlakis N, Kothe E, Lam L, Rosenthal D. Impact of medical qigong on quality of life, fatigue, mood and inflammation in cancer patients: a randomized controlled trial. Ann Oncol. 2010;21(3):608–14.
Ho RT, Fong TC. Factor structure of the Chinese version of the Pittsburgh sleep quality index in breast cancer patients. Sleep Med. 2014;15(5):565–9.
Cheng KK, Wong EM, Ling WM, Chan CW, Thompson DR. Measuring the symptom exprience of Chinese cancer patients: a validation of the Chinese version of the memorial symptom assessment scale. J Pain Symptom Manag. 2009;37(1):44–59.
Lam CL, Tse EY, Gandek B. Is the standard SF-12 health survey valid and equivalent for a Chinese population? Qual Life Res. 2005;14(2):539–47.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70.
Ng SM. Validation of the 10-item Chinese percieved stress scale in elderly service workers: one-factor versus two-factor structure. BMC Psychol. 2013;1:9.
Campbell NR, Ashely MJ, Carruthers SG, Lacourcière Y, McKay DW. Lifestyle modifications to prevent and control hypertension. 3. Recommendations on alcohol consumption. Canadian hypertension society, Canadian Coalition for High Blood Pressure Prevention and Control, Laboratory Centre for Disease Control at Health Canada, Heart and Stroke Foundation of Canada. CMAJ. 1999;160(9):S13–20.
Hou J, Wong SY, Lo HH, Mak WW, Ma HS. Validation of a Chinese version of the five facet mindfulness questionnaire in Hong Kong and development of a short form. Assessment. 2014;21(3):363–71.
Acknowledgements
The authors would like to acknowledge the volunteer teachers of Li Fai Centre of Tai Chi for their provision of support for this study.
Funding
This study is funded by the General Research Fund, Research Grants Council (GRF/ HKU 17611615).
Availability of data and materials
Not applicable. This is a study protocol, no datasets are generated at the present.
Author information
Authors and Affiliations
Contributions
Conceptualization and design of the study: RTHH, SNM, CLWC, KFC, JSMC, AHYW; Preparation of proposal for funding application: RTHH, SNM, CLWC, JSMC; Preparing the manuscript: RTHH, AHYW; Reviewing the manuscript: RTHH, AHYW, SMN, JSMC, KFC, CLWC. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research will perform in accordance with the Declaration of Helsinki, and ethical approval has been obtained from the Institutional Review Board of the University of Hong Kong/ Hospital Authority Hong Kong West Cluster (HKU/HA HKW IRB) (IRB Reference Number: UW 15-115). Written informed consent were obtained from all participants in prior to any data collection, randomization, and data analysis.
Consent for publication
Not applicable. There are no details on individuals to be reported within the manuscript.
Competing interests
This study is funded by the General Research Fund, Research Grants Council (GRF/ HKU 17611615). The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ho, R.T.H., Wan, A.H.Y., Chan, J.S.M. et al. Study protocol on comparative effectiveness of mindfulness meditation and qigong on psychophysiological outcomes for patients with colorectal cancer: a randomized controlled trial. BMC Complement Altern Med 17, 390 (2017). https://doi.org/10.1186/s12906-017-1898-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-017-1898-6