Abstract
Introduction
Exclusive breastfeeding (EBF) means providing only breast milk for infants for up to six months without the addition of solid or liquid matter. Even though EBF had great benefits for infants and mothers, the rate of EBF is so limited below the global target. In Ethiopia, the overall EBF practice is 59%. This low EBF practice had a great unexplained variation among employed and unemployed mothers. Therefore, this study aimed to compare EBF practice and associated factors among employed and unemployed mothers of infants aged 6–12 months in Wolkite town, Southern Ethiopia, 2020.
Methods
A community-based comparative cross-sectional study was conducted in March 2020. A total sample of 485 (241 employed and 244 unemployed) study subjects was involved in the study. A simple random sampling technique was used to recruit study subjects. A pre-tested structured interviewer-administered questionnaire was used. Multivariable logistic regression was used to identify associated factors of EBF practice for the whole study participants and then for employed and unemployed mothers independently.
Results
The pooled prevalence of exclusive breastfeeding practice was 63.9% [95% CI (59.8–68.2%)]. Exclusive breastfeeding practice was 54.8% [95% CI (48.5–61.4%)] and 73% [95% CI (66.8–78.7%)] among employed and unemployed mothers respectively. Three or more years of a birth interval [AOR = 4.03; 95% CI (1.80–8.99)], three or more ANC visits [AOR = 5.39; 95% CI (1.49–19.45)], and having PNC service [AOR = 4.56; 95% CI (2.0–9.4)] significantly associated to exclusive breastfeeding practice among employed mothers. No history of breastfeeding counseling during ANC visits [AOR = 0.15; 95% CI (0.06–0.41)], had history of breast disease [AOR = 0.28; 95% CI (0.08–0.99)], three or more ANC visits [AOR = 5.11; 95% CI (1.66–15.8)], and having social support [AOR = 3.05; 95% CI (1.23–7.6)] significantly associated to EBF practice among unemployed mothers.
Conclusion
Employment among mothers was found to discourage EBF practice. The predictors of exclusive breastfeeding practice are different for employed and unemployed. Therefore Policymakers and program planners are called to come together and create a conducive environment for lactating employees, and appropriate intervention at respective predictor variables is needed to enhance EBF practice.
Similar content being viewed by others
Introduction
Exclusive breastfeeding (EBF) means providing only breast milk for infants for up to six months without the addition of solid or liquid matter with the exception of oral rehydration solution, or drops/syrups of vitamins, minerals, or medicines [1, 2]. Breast milk in the first six months contains all the necessary nutrients provided in a bioavailable and easily digestible form. It is among the most effective ways to promote maternal and child health [3]. Exclusively breastfed infants can be protected from diarrhea, acute respiratory infections, risk of obesity, and allergies [4]. It is also important to the mother in returning the uterus to pre-pregnancy size faster; reduces the risk of breast, ovarian, uterine cancers, and osteoporosis. It also creates a special bond between mother and infant and aids in household food security by saving money [5, 6]. World health organization recommends EBF for the first six months of life. Then safe and adequate foods should be started after the six months, and breastfeeding continued up to two years and beyond [1, 7].
Globally, in 2021 only 44% of infants 0–6 months old are exclusively breastfed [8]. In Sub-Saharan Africa and East Africa, EBF practice was 31% and 42% respectively [9]. Ethiopian demographic health survey (EDHS) 2019 showed that EBF practice in Ethiopia was estimated to be 59% [10]. Despite appropriate feeding practice, being the most cost-effective intervention to reduce child morbidity and mortality, WHO in 2013 reported that non-exclusive breastfeeding contributes to 11.6% of mortality in children under the age of five years. This was equivalent to about 804,000 child deaths [11]. UNICEF in 2018 noted that improving breastfeeding rates around the world could save the lives of more than 820,000 children under the age of five every year [3]. Non-exclusive breastfeeding results in an estimated 40% of under‐five stunting in Western and Central Africa [12]. In Ethiopia, adequate EBF practices are expected to save the life of 70,000 infant deaths per year which is 24% of the total infant deaths annually [13].
In 2016, Ethiopia developed several nutritional strategies to increase the nutritional status of the child. These are: Promoting EBF for the first 6 months, establishing a baby-friendly health facility initiative in all public and private health facilities, enforcing the International Code of Marketing for Breast milk Substitutes, promoting the enactment of maternity leave, implementing breastfeeding rooms in major service providing institutions, and support employed breastfeed mothers to exclusively breastfeed their child [14]. Although repeated recommendations were given to EBF practice in Ethiopia, a trend study from 200 to 2016 revealed that the improvement in EBF practice was not statistically significant [15]. Similarly, EDHS showed that EBF practice had no significant improvement from 2016 to 2019 since only one percent has been increased [10].
Several factors affect the EBF practice. Among these maternal employment, parity, maternal perception of the quantity of breast milk, maternal education, antenatal care visits (ANC), postnatal care (PNC) utilization, maternal health, and birthplace are the most frequently associated factors [16]. Concerning maternal employment, there is a great significant variation in EBF practice among employed and unemployed mothers [17,18,19]. Despite women's labor forces being increased at an alarming rate in Ethiopia, EBF practice among employed mothers is relatively lower than among unemployed mothers [17,18,19]. The reason for the wide observed difference in EBF practice among employed and unemployed women is not well explained unless a few hypotheses that explain early resumption to work will reduce EBF practice among employed mothers. The aforementioned studies were done when the post-partum maternity leave was three months. Even though no a day’s post-partum maternity leave is increased from three to four months as a national nutritional strategy, EBF practice after the policy change is not known. Therefore, this study aimed to assess the association between maternal employment and EBF practices among mothers with infants between the ages of 6 and 12 months.
The study provides important evidence inputs for designing programs to improve EBF practice by considering the factors that affect the EBF practice of mothers in each group. The result of this study also has a potential contribution for program planners to design strategies to support employed breastfeeding mothers; such as implementing a breastfeeding room program in their working area. Considering those and similar rationale this study intended to assess the level of exclusive breastfeeding practice and associated factors among employed and unemployed mothers with an infant aged 6–12 months in Wolkite town, Southern Ethiopia, 2020.
Method and materials
Study design, period, and setting
A community-based comparative cross-sectional study design was conducted from February 20 to March 28, 2020, at Wolkite town which is found 158 km away from Addis Ababa, the capital city of Ethiopia in the southwest direction along the main road from Addis Ababa to Jimma. Wolkite town administration is organized into 3 sub-city and 7 kebeles. According to the Wolkite town administration health office report of 2019, the population size of the town is estimated to be 72,929, from this 15,413 are estimated to be 15–49 years old women and 1,106 are infants between 6 and 12 months of age [20].
Population and sample
All mothers who had infants 6–12 months old (employed and unemployed mothers) and who live in the study area for at least six months were the source population. Mothers who had infants between 6 and 12 months old from simple randomly selected households were the study population. Mothers of babies with cleft lip, and/or cleft palate and severely ill mothers were excluded.
The sample size was determined for the two objectives (prevalence and associated factors).
The sample size for the first objective.
According to a previous study conducted in the Fafan zone, Somali regional state of Ethiopia in 2019, the prevalence of EBF among employed mothers was 25%, and the prevalence of EBF among unemployed mothers was 83% [17]. Then the sample size is determined by using the following statistical formula.
where P1 = 0.25 (prevalence of EBF among employed), q1 = 1 − p1, P2 = 0.83 (prevalence of EBF among unemployed), q2 = 1 − p2 and f (α, β) = 7.84; when the power = 80% and α = 5%.
The sample size for associated factors is calculated using a comparative study done at Gonder town with the assumptions of 95% confidence interval, 80% power using OpenEpi version 3.01 [19] presented as follows (Table 1).
Finally, the calculated sample sizes by using the first objective and associated factors were compared. Then the largest sample size was taken. Therefore, the largest sample size of 239 in each group was taken, and after considering of 5% non-response rates the total sample size for each group was 251,
Regarding the sampling procedure first, the sample size was proportionally allocated to each kebele based on the total number of targeted women-child pairs in each kebele. Then household survey was conducted before data collection to identify the employment status of the mother and to provide an identity code for each eligible household in all kebeles. After having the number of employed and unemployed mothers, again the total sample size was proportionally allocated by employment status in each kebele. Then computer-generated simple random sampling technique was used to select study participants.
Data collection instrument and procedure
Data were collected by face-to-face interviews using pre-tested structured questionnaires which were prepared after reviewing different literature such as EDHS,2016 questionnaires, and other published literature on related topics [17,18,19, 21,22,23,24]. The questionnaire consists of five parts; socio-demographic characteristics, maternal health service and infant related factors, breastfeeding and related items, maternal breastfeeding-related knowledge, and other barriers to exclusive breastfeeding. Data were collected by four clinical nurse professionals with the supervision of two public health professionals.
Study variables
Exclusive breastfeeding practice was the dependent variable. Independent variables include; socio-demographic factors such as maternal age, educational level, employment status, knowledge, working hours, paternal educational level, paternal occupation, Family size, household income, and social support. Maternal health-related factors including parity, number of ANC visits, breastfeeding counseling during pregnancy, Place, and mode of delivery, postnatal care, maternal illness, and Perceived adequacy of breast milk were predictor variables. Similarly, infant-related factors such as birth order and interval, Sex and health status of the infants, and Bottle feeding practice were independent variables.
Operational definitions
An employed mother is a mother who had employed at a governmental or private organization or day laborer who works for more than eight hours per day for at least five days per week, and who had employed from birth to six months of the eligible child age.
Unemployed mother: a mother, who works at her home as a housewife,
Social support: a woman who had given economic, psychological support, and/or breastfeeding counseling from the society or organization.
Maternal breastfeeding knowledge: There are ten maternal knowledge-related questions, and if a study participant responds to five and above correct answers, she has good knowledge and if she responds to less than five, she has poor knowledge [22, 25].
Data quality assurance
To ensure the quality of data, three days of training were provided to data collectors and supervisors.
To assess the appropriateness of wording, clarity of the questions, and respondent reaction to the questions and interviewer, a pre-test was done on 5% of the calculated sample size in Emdibir town which has socio-demographic similarities with our study population. Regular supervisions were made during data collection. The collected data were checked for completeness, consistency, and clarity on daily basis.
Data analysis
The data were coded and entered into EpiData version 3.12 statistical software and then exported to SPSS version 21 for further analysis. Descriptive statistics such as frequencies, mean, median, and proportions were computed to find out the prevalence of exclusive breastfeeding (EBF) and other indices. Bivariate logistic regression was used to check variables having an association with the dependent variable, and then those variables having a p-value of ≤ 0.2 were fitted to multivariable logistic regression for controlling the effects of confounders. Adjusted Odds Ratios with 95% CI and a P-value of < 0.05 in multivariable logistic regression models were used to declare a significant association of variables with the dependent variable. Three multivariable analysis models were fitted; first, the model was fitted for the whole study participants. Then the model was fitted separately for employed and unemployed study subjects.
Results
Socio-demographic characteristics
In this study, a total of 241 (49.7%) employed and 244 (50.3%) unemployed women participated with a cumulative response rate of 97%. Concerning age category 92 (38.2%) of employed and 87 (35.7%) of mothers are in the age group of 25–29 years. Most 211 (88%) of employed and 222 (91%) of unemployed mothers were married. Majority189 (78.4%) of employed mothers had a college education and above, but 22 (8%) of unemployed mothers had college and above educational level (Table 2).
Among employed study participants, 155 (64%) mothers were governmentally employed.
The majority of husbands among employed mothers 123 (55%) had a college education and above. Whereas only 49 (21%) of husbands among unemployed mothers had a college education and above.
Maternal health service and infant related characteristics
The study revealed that more than half 286 (59%) of mothers had one to two children. The majority of the employed study participant 232 (96.3%) had a history of at least one ANC service follow-up at a health facility throughout their pregnancy. The study showed that almost all 240 (99.6%) employed study participants and 241 (99.2%) unemployed study participants delivered at a health facility, but about 124 (51.5%) of employed and 107 (43.9%) unemployed study subjects had post-natal care service (Table 3).
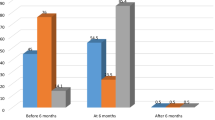
Prevalence of exclusive breastfeeding practice
The overall exclusive breastfeeding practice among the study participants was 63.9% (59.8–68.2%). The practice of exclusive breastfeeding among employed and unemployed mothers was 54.8% (95% CI 48.5–61.4%) and 73% (95% CI 66.8–78.7%) respectively.
In this study, the majority 236 (98%) of employed and 234 (96%) of unemployed mothers have fed the first breast milk or colostrum to their newborn. The most 26 (38.8%) frequently reported reason to discontinue exclusive breastfeeding among unemployed mothers was the perception of feeding breast milk only was not sufficient for the infant until six months. On the other hand, among 69 (63.3%) employed mothers the main reason to quit exclusive breastfeeding practice was lack of time.
This study also found that only 14 (5.8%) of employed mothers had breastfeeding rooms in their working areas, and 226 (94%) of them said that EBF is difficult to achieve at work. The study also revealed that about 180 (75%) of employed mothers had maternity leave with payments. Of those who had maternity leave with payment about 160 (97%) of them had 16 weeks and longer maternity leave.
Factors associated with exclusive breastfeeding practice
Factors associated with exclusive breastfeeding practice among all participants
In multivariable regression mothers who had three or more ANC, visits were 6.33[AOR = 6.33; 95% CI (2.85–14.06)] times more likely to exclusively breastfeed their infant than mothers who had less than three ANC visits. Mothers who had postnatal care were 3.77[AOR = 3.77; 95% CI (2.16–6.59)] times more likely to practice exclusive breastfeeding than those mothers who had no postnatal care. Having birth intervals of three or more years were 3.18 times more likely to practice EBF than those who had less than three years’ birth intervals [AOR = 3.18; 95% CI (1.79- 5.65)]. Unemployed mothers were 2.97 times more likely to exclusively breastfed their infant compared to employed mothers [AOR = 2.97: 95% CI (1.71–5.17)] (Table 4).
Factors associated with exclusive breastfeeding among employed mothers
Among employed mothers, a birth interval of three or more years was 4.03 more likely to practice EBF than those who had less than three years of a birth interval [AOR = 4.03; 95% CI (1.80–8.99)]. Employed mothers who had three or more ANC visits at health facilities were five times more likely to exclusively breastfeed their infant than those mothers who had less than three antenatal care visits [AOR = 5.39; 95% CI (1.49–19.45)]. Employed mothers who had postnatal care were 4.56 times more likely to practice EBF than those mothers who had no postnatal care [AOR = 4.56; 95% CI (2.0–9.4)] (Table 5).
Factors associated with exclusive breastfeeding among unemployed mothers
In multivariable analysis, unemployed mothers who had three or more ANC visits to a health facility were 5.11 times more likely to practice EBF as compared to mothers who had less than three ANC visits [AOR = 5.11; 95% CI (1.66–15.8)]. Unemployed mothers who were not given breastfeeding counseling during ANC visits were 85% less likely to EBF than those unemployed mothers who had breastfeeding counseling during ANC visits [AOR = 0.15; 95% CI 0.15 (0.06–0.41)]. Unemployed mothers who had social support were 3.05 times more likely to practice EBF than those mothers who had no social support [AOR = 3.05; 95% CI (1.23–7.6)]. Similarly, mothers who had a history of breast disease were 72% times more likely to cease EBF compared to mothers who had no history of breast disease [AOR = 0.28; 95% CI (0.08–0.99)] (Table 6).
Discussion
This study assessed the association between maternal employment status and exclusive breastfeeding practice among mothers of infants aged 6–12 months. Due to its several benefits for the child and the mother, WHO and UNICEF recommend exclusive breastfeeding for six consecutive months [1,2,3].
The prevalence of EBF in this study was 63.9% (59.8–68.2%) which is similar to the study done in different parts of Ethiopia such as; the Southern region 63.8%, Afar region 62%, Oromia region 65.6% [26], Hawassa 61% [27], Boditi Town, Woliata 64.8% [28] and with the study of global breastfeeding in twenty-first century 63% [29]. This finding is higher than the global target of exclusive breastfeeding practice of 50% in 2025 [7], Saudi Arabia 37% [30], African regions such as Zimbabwe 36% [31], Tanzania 38.8% [32], Kenya 45.5% [33], Ghana 50.6% [34], East Africa 42% [9], Somaliland 20.47% [35]. It is also higher than the mini Ethiopian demographic health survey,2019 report 59% [10], national trend studies in Ethiopia 59.9% [15], and Addis Ababa, Ethiopia 29.3% [36]. The potential variation of the finding of the current study from the two national studies might be due to study area difference since those studies use the national data which lower the prevalence while the current study focuses on a specific area (Wolkite town). The difference from the study in Addis Ababa might be the effect of the 2016 national nutritional strategy including the increment of maternity leave; since the study in Addis Ababa was done before the policy change. On the contrary, EBF practice in this study is lower than the study conducted in Bahirdar 86.4% [37]. The difference might be due to variation in measurement of exclusive breast feeding practice; since, the study in Bahirdar measures’ a one day pre survey EBF practice while the current study assess infant feeding during six months. The finding implies strong effort should be made to raise mother’s EBF practice including implementation of the national nutritional improvement strategy of 2016.
In this study, the prevalence of EBF among employed mothers was 54.8% (95% CI 48.5–61.4%) which is lower than EBF practice among unemployed mothers 73% (95% CI 66.8–78.7%). The finding is in line with the study conducted in Nepal [38], Ghana [23], and Kenya [24] and with studies done in Ethiopia at Injibara [18], Gondar [19], Debremarkos [22], and Somali region [17]. The significant difference might be due to the fact that employed mothers might not have adequate time to feed breast milk to their infants during working hours as unemployed mothers. Since, unemployed mothers usually have flexible working hours unlike employed mothers, which may contribute to relatively higher adherence to EBF practice than employed mothers.
Regarding factors associated with EBF, the study revealed that unemployed mothers were three times more likely to practice EBF than employed mothers. This finding is similar to the studies done in Tanzania [32], sub-Saharan countries [39], and the studies in Ethiopia such as; Debremarkos [22], Injibara [18], Bahirdar [37], Gondar [19], Hawassa [27] and Jigjiga [17]. The possible explanation might be unemployed women had more time to stay with their babies than employed mothers. In addition to this, lack of safe breastfeeding room at the workplace, less flexibility of managers for breastfeeding breaks, remoteness of working place from home, long working hours per day, and absence or short period of maternity leave might be the reasons for the decrement in EBF practice in employed mothers [38]. For instance, the presence of longer maternity leave was directly related to EBF practice compared with mothers who worked without maternity leave [40]. This finding suggests adequate support should be given to employed mothers including; permitting appropriate maternity leave so as to improve EBF practice.
Our study found that Mothers who had three or more ANC visits were 6.33 times more likely to practice EBF compared to women who had less than three ANC visits. This is consistent with the study on sub-Saharan countries [39]. This finding suggests adequate optimal breastfeeding counseling had been given to the mothers during frequent antenatal care visits since that is why EBF practice is higher in those mothers who have frequent antenatal care. The finding implies we should increase the frequency of ANC follow-up and breastfeeding counseling during ANC to increase EBF practice so as to improve maternal and child health.
The study also found that mothers who had a history of PNC are 3.77 times more likely to exclusively breastfeed their infant than their counterparts. This is in line with studies done in sub-Saharan countries [39] and studies in Ethiopia such as; Addis Ababa [36], Debremarkos [22], and Boditi [28]. This suggests providing effective postnatal care by committed health care providers can delay the introduction of breast milk substitutes/formula milk/ through exclusive breastfeeding counseling. Therefore, this counseling in post-natal care enhances EBF practice. Furthermore, mothers who had more than 36-month birth interval/spacing are 3.18 times more likely to exclusively breastfeed their infant than those mothers who had lower than three years birth interval. The possible reason might be the presence of a prolonged birth interval period leads to an optimized period of exclusive breastfeeding practice. This long birth interval might also assist the woman to get enough time to think and prepare herself for the upcoming healthy infant.
Apart from the analysis of the entire data set as a unit, separate analyses have been done for employed and unemployed mothers to appreciate the difference in factors affecting EBF practice. Accordingly, among employed mothers, having; an infant birth interval of three or more years, three or more ANC visits, and access to PNC services were more likely to exclusively breastfed their infant than their counterparts. The findings are consistent with studies done in Addis Ababa [36], and Gondar Ethiopia [19]. This finding implies strong effort should be made to increase awareness of mothers about birth spacing, ANC, and PNC service utilization to improve EBF practice so as to promote maternal and child health among employed mothers.
Similarly in the case of unemployed mothers, unemployed mothers who didn’t have breastfeeding counseling during ANC visits, are 0.15 times less likely to EBF than their counterparts. This finding is consistent with the study of Injibara [18] and Addis Ababa [36]. This might be because counseling that was given during ANC visits helps mothers to understand the advantage of EBF for their child as well as for themselves and enable them to exclusively breastfeed their child. In this study, unemployed mothers who had three or more ANC visits were five times more likely to breastfeed their infant than those mothers who had less than three ANC visits. The finding of this study is consistent with the study findings of Nepal [38], Ghana [41], Gondar [19], Injibara [18], and the Somali region [17]. The possible explanation for this result may be when unemployed mothers had frequent ANC visits; they might grasp more information about the benefits of exclusive breastfeeding practice upon potent counseling, so, this might enhance EBF practice. Similarly, Unemployed mothers who had social support from the community or organization were three times more likely to practice EBF than their counterparts. This finding is supported by the study done in Gondar [19], Hawassa [27], and the Somali region [17]. This finding suggests when women get economic, psychological, emotional, cultural, and informational support from the community or organization, the probability of EBF practice is extremely enhanced.
Unemployed mothers who had a history of breast disease are 0.28 times less likely to practice EBF than their counterparts. This finding is supported by studies conducted in Kumasi Metropolis, Ghana [34], Boditi [28], and Hawassa, Ethiopia [27]. This might be because when women had a history of breast-related problem during the lactation period, they may consider that the quality and quantity of breast milk is affected. Thus, they might have perceived breast milk as an inappropriate choice of food that affect the health of the infant.
The study only employed a quantitative method so that miss’s qualitative aspects that affect EBF practice including the attitude and beliefs of mothers related to EBF. So in the future, it is better to investigate the issue deeply by employing qualitative methods.
Conclusion
In our study, exclusive breastfeeding practice is found lower compared to the expected standard of achievement. There is a significant difference in the prevalence of exclusive breastfeeding practice between employed and unemployed mothers. Unemployed mothers are more likely to exclusively breastfed their children than employed mothers. This showed that maternal employment is associated with low EBF practice. Some predictor variables are different for employed and unemployed mothers. The study found that birth interval, number of ANC visits, postnatal care, and employment status were significantly associated with exclusive breastfeeding among overall study participants. Among employed mothers' birth interval, the number of ANC visits and PNC service utilization is positively associated with EBF practice among employed mothers. Finally, breastfeeding counseling during ANC visits, number of ANC visits, and maternal social support from the community or organizations are significantly associated with EBF practice among unemployed mothers. Therefore Policymakers and program planners are called to come together and create a conducive environment for lactating employees including daycare centers and breastfeeding rooms. Health care workers should enhance counseling on breastfeeding practice and birth spacing for mothers during antenatal and postnatal care visits. The community should provide social support for lactating women to promote exclusive breastfeeding at home and in working areas. Generally, appropriate intervention at respective predictor variables is needed to enhance EBF practice. Furthermore, researchers are expected to dig out detail on the attitude and beliefs of mothers related to EBF.
Availability of data materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- ANC:
-
Antenatal care
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- EBF:
-
Exclusive breastfeeding
- EDHS:
-
Ethiopian Demographic Health Survey
- PNC:
-
Postnatal care
- SNNPR:
-
Southern Nation Nationalities and People
- UNICEF:
-
United Nation International Children Fund
- WHO:
-
World Health Organization
References
World health organization. Exclusive breast feeding for optimal growth, development and health of infants: Geneva, Swizerland; 2019.
UNICEF. Optimal breastfeeding: New York, USA; 2019.
UNICEF. Breastfeeding a mother’s gift, for every child. New York, USA; 2018.
Turck D, Vidailhet M, Bocquet A, Bresson J, Briend A, Chouraqui J, et al. Breastfeeding: health benefits for child and mother. Archives de pediatrie: organe officiel de la Societe francaise de pediatrie. 2013;20:S29-48.
Horta BL, Victora CG. Long-term effects of breastfeeding: a systematic review. Geneva. 2013.
Shamir R. The benefits of breast feeding. Nestle Nutr Inst Workshop. 2016;86:67.
WHO/UNICEF. Global nutrition targets 2025: breastfeeding policy brief (WHO/NMH/NHD/14.7). Geneva. World Health Organization. 2014.
WHO. Key facts on infant and young child feeding. 2021.
World Health Organization. Infant and young child feeding; 2015.
Ethiopian Public Health Institute (EPHI) EaI. Ethiopia mini demographic and health survey: key indicators. Rockville, Maryland, USA: EPHI and ICF. 2019.
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427.
UNICEF. A successful start in life: Improving breastfeeding in West and Central Africa. New York: UNICEF. 2010.
Biks GA, Berhane Y, Worku A, Gete YK. Exclusive breast feeding is the strongest predictor of infant survival in Northwest Ethiopia: a longitudinal study. J Health Popul Nutr. 2015;34:9.
Federal Democratic Republic of Ethiopia. National nutrition program 2016–2020; 2016.
Ahmed KY, Page A, Arora A, Ogbo FA. Trends and determinants of early initiation of breastfeeding and exclusive breastfeeding in Ethiopia from 2000 to 2016. Int Breastfeed J. 2019;14:40.
Maharlouei N, Pourhaghighi AH, Raeisi Shahraki H, Zohoori D. Factors affecting exclusive breastfeeding, using adaptive LASSO regression. IJCBNM. 2018;6(3):260.
Tadesse F, Alemayehu Y, Shine S, Asresahegn H, Tadesse T. Exclusive breastfeeding and maternal employment among mothers of infants from three to five months old in the Fafan zone, Somali regional state of Ethiopia: a comparative cross-sectional study. BMC Public Health. 2019;19:1015.
Taddele M, Abebe L, Fentahun N. Exclusive breastfeeding and maternal employment in ethiopia: a comparative cross-sectional study. Int J Nutr Food Sci. 2014;3(6):497–503.
Chekol DA, Biks GA, Gelaw YA, Melsew YA. Exclusive breastfeeding and mothers’ employment status in Gondar town, Northwest Ethiopia: a comparative crosssectional study. Int Breastfeed J. 2017;12(27):1–9.
Wolkite City Administration Health Office. Population statistics. 2019.
Central Statistics Agency (CSA) (Ethiopia), ICF International. Ethiopia demographic and health survey. In. Addis Ababa, Ethiopia and Rockville, Maryland, USA:. Central Statistical Agency (CSA) and ICF International. 2016.
Mekuria G, Edris M. Exclusive breastfeeding and associated factors among mothers in Debre Markos, Northwest Ethiopia: a cross-sectional study. Int Breastfeed J. 2015;10(1):1–7.
Nkrumah J. Maternal work and exclusive breasted practice: a community based cross-sectional study in Efutu Municipal, Ghana. Nkrumah Int Breasteed J. 2017;12:10.
Hassan M, Yasmeen BHN, Ahmed TU, Begum M, Rob AWS, Ahmed AU, et al. Practice of giving exclusive breastfeeding among the babies of working mothers and house wife mothers- a comparative study. Northern Int Med Coll J. 2014;5(2):339–41.
(UNICEF) UNCsF. Infant and Young Child Feeding (IYCF). Nutrition Section, Programming Guide. 2011.
Alebel A, Tesma C, Temesgen B, Ferede A, Kibret GD. Exclusive breastfeeding practice in Ethiopia and its association with antenatal care and institutional delivery: a systematic review and meta-analysis. Int Breastfeed J. 2018;13:31.
Adugna B, Tadele H, Reta F, Berhan AY. Determinants of exclusive breastfeeding in infants less than six months of age in Hawassa, an urban setting, Ethiopia. Int Breastfeed J. 2017;12:45.
Azeze GA, Gelaw KA, Gebeyehu NA, Gesese MM, Mokonnon TM. Exclusive breastfeeding practice and associated factors among mothers in Boditi Town, Wolaita Zone, Southern Ethiopia, 2018: a community-based cross-sectional study. Int J Pediatr. 2019;8(3):1–11.
Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475–90.
Hafsa Raheel TS. Why mothers are not exclusively breastfeeding their babies till 6 months of age? Knowledge and practices data from two large cities of the Kingdom of Saudi Arabia. Sudanese J Paediatr. 2018;18(1):28–38.
Mundagowa PT, Chadambuka EM, Chimberengwa PT, Mukora-Mutseyekwa AF. Determinants of exclusive breastfeeding among mothers of infants aged 6 to 12 months in Gwanda District, Zimbabwe. Int Breastfeed J. 2019;14(30):1–8.
Hussein TH, Mgongo M, Uriyo JG, Damian DJ, Stray-Pedersen B, Msuya SE, et al. Exclusive breasted rates and factors associated with exclusive breasted practices in Northern Tanzania: measurement using two different methodologies—24 hours recall and recall since birth. Int J MC AIDS. 2019;8(1):32–43.
Mohamed MJ, Ochola S, Owino VO. Comparison of knowledge, attitudes and practices on exclusive breastfeeding between primiparous and multiparous mothers attending Wajir District hospital, Wajir County, Kenya: a cross-sectional analytical study. Int Breastfeed J. 2018;13(11):1–10.
Yeboah JY, Agyemang-Duah WW. Exclusive breastfeeding practices and associated factors among lactating mothers of infants aged 6–24 months in the Kumasi Metropolis, Ghana. BMC Res Notes. 2019;12(689):1–6.
Jama A, Gebreyesus H, Wubayehu T, Gebregyorgis T, Teweldemedhin M, Berhe T, et al. Exclusive breastfeeding for the first six months of life and its associated factors among children age 6–24 months in Burao district, Somaliland. Int Breastfeed J. 2018;15(5):1–8.
Shifraw T, Worku A, Berhane Y. Factors associated exclusive breastfeeding practices of urban women in Addis Ababa public health centers, Ethiopia: a cross sectional study. Int Breastfeed J. 2015;10:22.
Belachew A, Tewabe T, Asmare A, Hirpo D, Muche BZD. Prevalence of exclusive breastfeeding practice and associated factors among mothers having infants less than 6 months old, in Bahir Dar, Northwest, Ethiopia: a community based cross sectional study 2017. BMC Res Notes. 2018;17(768):1–6.
Sabin A, Manzur F, Adil S. Exclusive breastfeeding practices in working women of Pakistan: a cross sectional study. Pak J Med Sci. 2017;33(5):1148–55.
Ogbo FA, Eastwood J, Page A, Efe-Aluta O, Anago-Amanze C, Kadiri EA, et al. The impact of sociodemographic and health-service factors on breast-feeding in sub-Saharan African countries with high diarrhea mortality. Public Health Nutr. 2016;20(17):3109–19.
Rimes KA, MICdO, CSB. Maternity leave and exclusive breastfeeding. Rev Saude Publica. 2019;53(10):1–12.
Elvis J, Dun D, Laar AK. Exclusive breastfeeding amongcity-dwelling professional workingmothers in Ghana. Int Breastfeed J. 2016;11(23):1–9.
Acknowledgements
First of all, we would like to express our great thanks to Wolkite University, College of medicine and health sciences for giving the Ethical clearance for this research. Then, our heartfelt thanks go to the study participants for their gold time and the respected response they have provided to us.
Funding
The authors did not receive any funds for this research work.
Author information
Authors and Affiliations
Contributions
TT: Made conceptualizations of the study, Methodology, validation, and, Statistical analysis coordinate data collection. AZ, AWK, and AO: performed supervision, validation, Writing, review & editing. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the institutional review board of the College of Medicine and Health Science of Wolkite University with letter reference no. of CMHS/1012/2012. An official letter of permission was written from the town health office. Following an explanation of the purpose of the study written informed consent was obtained from participants. Also, affirmation was made that they are free to discontinue participation at any time without any form of prejudice. Confidentiality of information and privacy of participants was assured for all the information provided, to preserve the confidentiality the data is not exposed to the third party except investigators. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zewdie, A., Taye, T., Kasahun, A.W. et al. Effect of maternal employment on exclusive breastfeeding practice among mothers of infants 6–12 months old in Wolkite town, Ethiopia: a comparative cross-sectional study. BMC Women's Health 22, 222 (2022). https://doi.org/10.1186/s12905-022-01816-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-022-01816-9