Abstract
Background
The purpose of this study was to measure the prevalence of intimate partner and family violence amongst a population of Australian female nurses, doctors and allied health professionals.
Methods
We conducted a descriptive, cross-sectional survey in a large Australian tertiary maternity hospital with 471 participating female health professionals (45.0% response rate). The primary outcome measures were 12 month and lifetime prevalence of intimate partner violence (Composite Abuse Scale) and family violence.
Results
In the last 12 months, one in ten (43, 11.5%) participants reported intimate partner violence: 4.2% (16) combined physical, emotional and/or sexual abuse; 6.7% (25) emotional abuse and/or harassment; 5.1% (22) were afraid of their partner; and 1.7% (7) had been raped by their partner. Since the age of sixteen, one third (125, 29.7%) of participants reported intimate partner violence: 18.3% (77) had experienced combined physical, emotional and/or sexual abuse; 8.1% (34) emotional abuse and/or harassment; 25.6% (111) had been afraid of their partner; and 12.1% (51) had been raped by their partner. Overall, 45.2% (212) of participants reported violence by a partner and/or family member during their lifetime, with 12.8% (60) reporting both.
Conclusion
Intimate partner and family violence may be common traumas in the lives of female health professionals, and this should be considered in health workplace policies and protocols, as health professionals are increasingly urged to work with patients who have experienced intimate partner and family violence. Implications include the need for workplace manager training, special leave provision, counselling services and other resources for staff.
Similar content being viewed by others
Background
Violence against women, specifically intimate partner violence and family violence (hereafter referred to as ‘intimate partner and family violence’, is a serious and prevalent public health issue [1]. Intimate partner violence (IPV) is defined as “any behaviour that causes physical, psychological or sexual harm to those in that relationship” [2], and Family Violence (FV) is defined as harmful behaviour perpetrated by a non-intimate family member at any time in the life course, including the witnessing of violence between parents [3]. Throughout this paper, we use the terms: IPV when referring to violence by a partner, FV when referring to violence by a non-intimate family member, and intimate partner and family violence when referring to both violence by a partner and/or non-intimate family member. Global estimates of IPV are that it affects between 15 to 71% of ever-partnered women across their lifetime [4]. Australia’s IPV prevalence is towards the lower end of that spectrum, with 25% of adult women in a national survey experiencing at least one incident of physical or sexual IPV during adulthood, 2.1% in the last 12 months [5]. The prevalence of physical or sexual violence before the age of fifteen is 16%, predominantly occurring within the family of origin, while 13% of Australian women were exposed to FV as children [6]. IPV contributes to a range of physical, sexual, psychological and reproductive health issues [7]. Survivors of IPV present to health care services more than other women [7], and during pregnancy there are increased risks for the unborn baby [8]. Thus, health professionals are increasingly recognised as having an essential role to play in identifying IPV survivor patients and providing a timely evidence-based response [9]. However, there are barriers to health professionals providing such interventions [10]. These include discomfort discussing the issue, lack of time and knowledge [10], and personal history of IPV [11].
While the majority of nurses and allied health professionals employed at public hospitals are women, little is known about the prevalence of IPV and FV against these health professionals [12, 13]. An extensive search of the academic literature (1987–2017) using three main search terms and synonyms - intimate partner violence, family violence, personal experience and health professional - identified fourteen quantitative studies into intimate partner and family violence against nurses and other health professional groups globally [12, 14,15,16,17,18,19,20,21,22,23,24,25,26]. None of these studies were Australian. The lifetime prevalence rate ranged between 3.7% (doctors in the United States) [17] and 97.7% (doctors and nurses in Pakistan) [18]. A large study conducted in a country with a comparable population prevalence rate to Australia is that by Bracken et al. (2010) in the United States [12], who surveyed 1981 nurses and found that the lifetime physical or sexual IPV prevalence rate was 25%. The strengths of this study included the large sample size and response rate (52%); however, this study did not cite the use of a validated scale and asked a small number of IPV questions. More recently, the Cavell Nurses’ Trust surveyed 2254 British nurses about their health and well-being, including their exposure to IPV [26]. They found that, in the last 12 months, 12.2% of nurses had experienced non-physical abuse by a partner, while 3.1% had been physically abused, and these were substantially increased rates to that of the general community [26]. The limitations of the few studies on this issue include: a lack of rigor in the assessment of IPV [12, 14, 16, 17, 20, 22], low or unpublished response rates [20, 23, 26], small sample sizes [21, 23, 24], or publication ten or more years ago [15,16,17, 24, 25]. Another feature of these studies is their diversity: six of the studies were conducted in countries where a language other than English is the official language [15, 16, 18, 19, 21, 23], and in some countries prevalence studies were hard to generalise to the Australian context since the population prevalence was substantially higher than reported in the Australian community [18, 22, 23].
The primary objective of our study was to address a gap in the available evidence about exposure to 12 month and lifetime IPV and lifetime FV, against female health professionals in Australia. The secondary objectives were to investigate the prevalence of interpersonal violence perpetrated by people other than partners/family members (i.e. colleagues, neighbours, strangers) against health professionals, and to investigate whether age, professional background and/or years of experience were associated with a history of intimate partner and family violence.
Methods
We developed a cross-sectional survey about health professional’s personal experiences of IPV, FV and other violence in the context of professional clinical care. Our survey included questions about demographics, work-related characteristics, exposure to IPV during the last 12 months and adult lifetime, lifetime FV and lifetime other violence. We defined IPV as physical, sexual and/or psychological violence, including the threat of such violence, occurring within an ‘adult intimate relationship’ (lasting longer than one month) with a partner/boyfriend/girlfriend/husband/wife, since the age of sixteen. We used the Composite Abuse Scale (CAS) to measure the prevalence of IPV; a 30-item well validated self-report measure of physical, sexual and emotionally abusive behaviours [27, 28]. Hegarty et al. (1999) developed the CAS using a sample of 427 Australian nurses (33% response rate) [27]. It measures IPV in the previous twelve months using a 6-point scale, and we adapted it further to measure adult lifetime IPV (since the age of sixteen). The CAS uses cut-off scores, which groups participants into four categories of IPV: ‘Severe Combined Abuse’ (severe physical, emotional and/or sexual violence), ‘Physical Abuse combined with Emotional Abuse and/or Harassment’, ‘Physical Abuse’ alone (not in combination with any other category of abuse), and ‘Emotional Abuse and/or Harassment’ alone (not in combination with any other category of abuse).
We defined FV as encompassing violence directed at a participant by a family member at any time during the life course and/or the witnessing of violence between parents during childhood. Based on a review of the literature, we developed two questions to measure FV; “Have you ever experienced violence or abuse from a family member? (e.g. someone who is not your partner, like a parent, uncle, in-law, sibling) Yes/No”; and, “Growing up, was there ever violence or abuse in your home between your parents? Yes/No”. While the focus of our study was IPV and FV, we also wanted to capture a participant’s overall experience of interpersonal violence, so we asked one further question about incidents of lifetime violence perpetrated by someone not intimately known, i.e. a patient, colleague or neighbour: “Have you ever experienced violence or abuse from somebody other than a partner or family member? Yes/No. If yes, please describe”.
The survey, conducted between 8 August and 31 December 2013, was anonymous and voluntary, and completion implied consent. The research was conducted at a single site – a large, tertiary maternity hospital in Australia. Piloting of the survey led to modifications of the wording. We recruited via two methods: (1) online (Survey Monkey) and (2) a paper-based survey to ensure that health professionals without access to a computer in a confidential setting had the opportunity to participate. A third-party recruiter employed by the hospital administered the survey. The online survey link and encouragement to participate by the Chief Executive Officer were distributed via email to all part-time/permanent clinical staff - nurse/midwives, doctors and allied health professionals. Staff were excluded if they were employed casually, or did not work in a clinical capacity (i.e. administration staff). Two reminder emails were sent, at two and three weeks post recruitment commencement. The third-party recruiter had a de-identified list of identification numbers for all potential participants to ensure that a participant did not submit a survey more than once. Reminder emails were targeted to those who had not yet participated. The third-party recruiter arranged for a paper survey and a reply-paid envelope to be delivered to the timesheet pigeonhole of the remaining eligible health professionals who had not yet participated. Coffee vouchers at the hospital café were offered to all staff as incentive and appreciation for considering participation and were not conditional on having completed the survey. Ethics approval was granted by both the recruiting hospital and the University of Melbourne Human Research and Ethics Committees (Ethics ID: 1339986).
Statistical analysis
Univariate analyses using frequencies and percentages were performed to describe the sample, including demographics, work-related characteristics and exposure to IPV, FV and other violence. Odds ratios, 95% confidence intervals (CI) and P-values were used to assess the likely size of the association between demographic variables and categories of abuse. Data were imported, cleaned, coded and analysed with STATA version 13.
Results
We sent the survey to 1047 female health professional staff, and 471 participated: 366 completed the survey electronically, while 105 returned a paper version, giving a response rate of 45.0%. The professional background of our sample included: 67.5% (317) nurse/midwives; 14.7% (69) doctors and 13.0% (61) allied health professionals (i.e. social workers, physiotherapists) (Table 1). The participants were very practiced (70.8%, 331 had more than ten years’ experience) and just under half (48.2%, 226) supervised other staff. Participants commonly worked with pregnant women and babies (58.9%, 277 maternity/neonatal services), and were representative of their non-participating peers regarding age, clinical area of work, professional background and years of employment. Most participants (92.9%, 431) had been in an intimate relationship at some time since the age of sixteen.
Twelve-month prevalence of intimate partner violence
More than ten percent of our sample had experienced IPV in the previous 12 months; feeling afraid of a partner was reported by 5.1% (22/432), which when combined with any category of violence on the CAS, increased to 11.5% (50/434) (Table 2). The most common form of violence during the previous 12 months was Emotional Abuse/Harassment alone (6.7%, 25/375), 2.1% (8/375) had experienced Severe Combined Abuse, 2.1% (8/375) reported Physical Abuse and Emotional Abuse/Harassment, and 0.5% (2/375) reported Physical Abuse alone. Rape and/or attempted rape by an intimate partner was disclosed by 1.7% (7/375) of participants.
Adult lifetime prevalence of intimate partner violence
One in three (146/434, 33.6%) participants reported fear of a partner and/or scored as having experienced some form of violence since the age of sixteen (Table 2). The most common category of abuse was Severe Combined Abuse, 13.8% (58/421), followed by Emotional Abuse/Harassment alone, 8.1% (34/421), 4.5% (19/421) Physical abuse and Emotional Abuse/Harassment, and 3.3% (14/421) Physical Abuse alone. Around one in ten (51/421, 12.1%) participants had been raped by a partner since the age of sixteen.
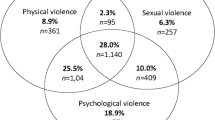
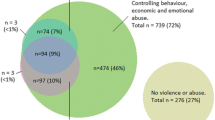
Lifetime prevalence of family violence
The proportion of participants who had experienced violence by a non-intimate family member was 28.4% (133/469) (Table 3). Of this group, 12.8% (60/469) had a combined history of both IPV and FV, and 15.6% (73/469) had survived FV alone with no coexisting history of IPV.
Lifetime prevalence of other interpersonal violence
Experiences of interpersonal violence from somebody other than a partner or family member were reported by 18.7% (87/466) of participants (Table 3), and two thirds (70.2%, 61/87) of these participants had a coexisting history of intimate partner and family violence. When asked to describe the type of violence they had experienced, qualitative descriptions were categorised as follows: sexual assault (52.8%, 28/53), physical and/or combined emotional abuse (17.0%, 9/53) and emotional abuse/harassment alone (30.2%, 16/53). The perpetrator of the violence was identified as a stranger by 7.1% (4/56) of participants who provided descriptions of their experience. In contrast, the perpetrators of other interpersonal violence most frequently reported were: friends/acquaintances (29.6%, 16/54), patients (29.6%, 16/54) and colleagues (20.4%, 11/54). Males perpetrated the majority (89.7%) of the other violence described by participants.
Professional background and violence
We examined whether a participant’s professional background was associated with a history of intimate partner and family violence and found that allied health professionals (65.6%, 40/61) were significantly more likely to report violence by an intimate partner or family member (p = 0.001) with increased odds at a level of 2.6 (CI: 1.4–4.6). This was compared to their peers in nursing/midwifery (42.5%, 134/315) and medicine (44.9%, 31/69). Neither age or relationship status was significantly associated with fear or violence during the adult lifetime.
Discussion
Our study suggests that intimate partner and family violence, including sexual assault, are frequent traumas in the lives of participating women health professionals. One in ten (11.5%) health professionals had felt fear of their partner, or experienced physical, emotional and/or sexual violence from them during the previous 12 months. To put this into context, this is a substantially higher prevalence than the Australian population community sample (2.1%, N= > 17,000) [5], double the prevalence rate identified in a large workplace survey of Australian teachers and nurses (5.0%, N = 3611) [29], but lower than a clinical sample of patients in primary care (19.6%, N = 1344) [30, 31]. The community surveys have used different methodologies and may not be directly comparable with our survey; however, our findings of a lower prevalence than the clinical sample cited above validates our results, since both samples were assessed using the CAS. We would expect the 12 month rate of IPV to be lower in a sample of currently employed healthcare workers compared with a sample of unwell patients presenting to a primary care doctor with clinical symptoms, since IPV prevalence is consistently higher among those seeking health care, including primary care [32].
Across their adult lifetime, one quarter (25.6%) of participants had experienced fear of a partner, which is similar to the clinical primary care sample discussed above, where the lifetime fear of a partner was 28% (N = 1836) [30]. More than one in ten (12.1%) participants had been raped by their partner, which is considerably higher than both the Australian population community sample (9.2%) [5], and a large community sample of women aged 34–39 years where the prevalence (assessed by the CAS) was 6.3% (N = 7768) [33]. Forty-five percent of our sample (45.2%) had experienced either violence from a partner or family member, with 12.8% having experienced both. Half (50.8%) of all participants had a lifetime history of interpersonal violence, perpetrated by either a partner, family member or somebody else. These findings are difficult to place in a broader context because of difference in the measures used. They indicate however, that the violence burden in health professional women’s lives may be high and overwhelmingly perpetrated by partners and family members. Further to this finding, while a fifth (19.8%) of participants identified that they had been the victim of violence by somebody outside the home, only a small proportion (5.6%) had experienced this category of violence in isolation; most survivors had a combined history of intimate partner and family violence. When asked about the perpetrator of the other violence, the majority (89.7%) were men known to the survivor: their friends, patients and colleagues.
We found that being an allied health professional was significantly associated with intimate partner and family violence. Since the majority of allied health professionals employed at the research site were social workers, and social workers are regularly referred to once a patient with a history of intimate partner and family violence is identified, they are therefore a professional group who are familiar with discussing narratives of violence [9]. Some research has indicated that people who work in the helping professions may have spent greater time confronting their personal trauma histories motivating them to support others recovering from trauma [34]. It follows then that allied health professionals may have been more willing to disclose intimate partner and family violence in this survey, or they may indeed have a higher prevalence of intimate partner and family violence. Social workers are also at higher risk of experiencing vicarious or secondary trauma from listening to the traumatic stories of their patients [35]. This warns of a potentially high cumulative trauma load stemming from the combination of primary and secondary trauma, and underscores the need for resources to assist health and other helping professionals in their work supporting patients.
Strengths of this study include the well-validated scale we used to measure IPV [27] and the representation of different health professionals. Our study is the first to publish the prevalence of IPV more than 12 months ago using the CAS, another strength of the research. The overall response rate of 45.0% is not optimal, but given the sensitive nature of this survey [36], its length, and the heavy work demands of our participants, it is comparable to similar rigorous research [12]. Other limitations of this study include; self-report and social desirability which might have led to under-reporting of violence, non-response bias and the single recruitment site which prevents generalisability of findings [37, 38]. There is the potential for recall problems with both 12 month, and lifetime measures, or “telescoping”, remembering incidents as occurring more or less than they did [39]. It is also possible that survivors of violence may be more interested and willing to participate in intimate partner and family violence research than other people [38]. These issues acknowledged, over-reporting is widely agreed to be rare in intimate partner and family violence research, while there is substantial concern about underreporting [40]. We found participants more frequently reported Emotional Abuse and/or Harassment in the previous 12 months and Severe Combined Abuse in the period longer than 12 months. Since no evidence suggests that the prevalence of emotional abuse decreases over time, we speculate that the tendency to report non-physically abusive behaviours might recede over time, indicating possible underreporting of lifetime Emotional Abuse and/or Harassment in our study.
Conclusions
Our study is the first to measure the prevalence of intimate partner and family violence in an Australian health professional population of nurses, doctors and allied health professionals. For the first time, it suggests that intimate partner and family violence may be common in the personal lives of Australian clinicians. These findings have implications for policy, practice and research. Healthcare organisations rarely consider what it means if the health professional is impacted by fear and violence in their home and are asked to intervene sensitively with patients affected by these same issues. Employment can be highly protective for someone experiencing violence [12], but it can simultaneously be a risk [41]. Attendance may be disrupted, as well as one’s capacity while at work [31]. Developing a workplace program that supports health professionals with a trauma history, including their clinical practice with patients experiencing intimate partner and family violence, requires organisational leadership, guidelines for a supportive response and trained individuals to receive disclosures (peer support workers, managers/supervisors, Human Resource staff and Employee Assistance Program professionals) [9]. Workplace programs may be especially necessary given that previous research with social workers has found a greater risk of vicarious trauma in response to working with traumatised patients when the social worker has a history of childhood trauma [42]. More research is required to better understand the needs of health professional women during and after intimate partner and family violence, including the role of the workplace. Intimate partner and family violence not only impacts the health professional survivor herself, we argue that it may have important ramifications for health services’ capacity to provide the best care to patients experiencing the traumatic health sequel of violence. Health services should have safe pathways to care for both health professionals and patients who are experiencing intimate partner and family violence.
Abbreviations
- CAS:
-
Composite abuse scale
- FV:
-
Family violence
- IPV:
-
Intimate partner violence
References
VicHealth: Violence against women in Australia: Research summary. Victoria; 2011.
Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R. World report on violence and health. Geneva: World Health Organization; 2002.
Ellsberg M, Heise L. Researching violence against women: a practical guide for researchers and activists. Washington DC, United States: World Health Organization; 2005.
García-Moreno C, Jansen H, Ellsberg M, Heise L, Watts C. WHO multi-country study on women’s health and domestic violence against women: summary report of initial results on prevalence, health outcomes and women’s responses. Geneva: World Health Organization; 2005.
Australian Bureau of Statistics. Personal Safety, Australia, 2012. Canberra: Australian Bureau of Statistics; 2012.
Australian Bureau of Statistics: Personal Safety, Australia. Edited by Australian Bureau of Statistics, vol. 4906.0. Canberra Australian Bureau of Statistics; 2016.
Campbell J. Health consequences of intimate partner violence. Lancet. 2002;359(9314):1331–6.
Donovan B, Spracklen C, Schweizer M, Ryckman K, Saftlasa A. Intimate partner violence during pregnancy and the risk for adverse infant outcomes: a systematic review and meta-analysis. BJOG Int J Obstet Gynaecol. 2016;123(8):1289–99.
Royal Commission into Family Violence (Victoria): Royal Commission into Family Violence: Summary and Recommendations. In. Edited by (Victoria) RCIFV, vol. Parl Paper No 132 (2014–16). Victoria: Royal Commission Into Family Violence (Victoria); 2016.
Sprague S, Madden K, Simunovic N, Godin K, Pham NK, Bhandari M, Goslings JC. Barriers to screening for intimate partner violence. Women & Health. 2012;52(6):587–605.
Mezey G, Bacchus L, Haworth A, Bewley S. Midwives' perceptions and experiences of routine enquiry for domestic violence. BJOG-An International Journal of Obstetrics and Gynaecology. 2003;110(8):744–52.
Bracken M, Messing J, Campbell J, La Flair L, Kub J: Intimate partner violence and abuse among female nurses and nursing personnel: prevalence and risk factors. Issues in Mental Health Nursing 2010, 31(2):137–148.
Australian Institute of Health and Welfare: Nursing and midwifery workforce 2012. In. Edited by Australian Institute of Health and Welfare, vol. no. 6. Cat. no. HWL 52. Canberra: Australian Institute of Health and Welfare; 2013.
Candib L, Savageau J, Weinreb L, Reed G. Inquiring into our past: when the doctor is a survivor of abuse. Fam Med. 2012;44(6):416–24.
Christofides N, Silo Z. How nurses' experiences of domestic violence influence service provision: study conducted in north-west province, South Africa. Nursing & Health Sciences. 2005;7(1):9–14.
Diaz-Olavarrieta C, Paz F, de la Cadena C, Campbell J: Prevalence of intimate partner abuse among nurses and nurses' aides in Mexico. Arch Med Res 2001, 32(1):79–87.
Doyle J, Frank E, Saltzman L, McMahon P, Fielding B. Domestic violence and sexual abuse in women physicians: associated medical, psychiatric, and professional difficulties. Journal of Women's Health & Gender-Based Medicine. 1999;8(7):955–65.
Khan A, Karmaliani R, Saeed Ali T, Asad N, Madhani F. Lifetime prevalence of emotional/psychological abuse among qualified female healthcare providers. Sociology Mind. 2014;4:174–82.
Stenson K, Heimer G. Prevalence of experiences of partner violence among female health staff - relevance to awareness and action when meeting abused women patients. Womens Health Issues. 2008;18(2):141–9.
Early M, Williams R. Emergency nurses' experience with violence: does it affect nursing care of battered women? J Emerg Nurs. 2002;28(3):199–204.
Al-Natour A, Gillespie G, Wang L, Felblinger D. A comparison of intimate partner violence between Jordanian nurses and Jordanian women. Journal of Forensic Nursing. 2014;10(1):13–9.
Mitchell V, Parekh K, Russ S, Forget N, Wright S. Personal experiences and attitudes towards intimate partner violence in healthcare providers in Guyana. International Health. 2013;5(4):273–9.
Sharma K, Vatsa M. Domestic violence against nurses by their marital partners: a facility-based study at a tertiary care hospital. Indian Journal Of Community Medicine: Official Publication Of Indian Association Of Preventive & Social Medicine. 2011;36(3):222–7.
Janssen P, Basso M, Costanzo R. The prevalence of domestic violence among obstetric nurses. Womens Health Issues. 1998;8(5):317–23.
deLahunta EA, Tulsky AA. Personal exposure of faculty and medical students to family violence. Jama-Journal of the American Medical Association. 1996;275(24):1903–6.
Cavell Nurses' Trust. Skint, Shaken yet still caring. But who is caring for our nurses? UK: Cavell Nurses' Trust; 2016.
Hegarty K, Sheehan M, Schonfeld C. A multidimensional definition of partner abuse: development and preliminary validation of the composite abuse scale. J Fam Violence. 1999;14(4):399–415.
Thompson M, Basile K, Hertz M, Sitterle D. Measuring intimate partner violence victimization and perpetration: a compendium of assessment tools. National Center for Injury Prevention and Control of the Centers for Disease Control and Prevention: Atlanta, Georgia; 2006.
Australian Institute of Health and Welfare: Authoritative information and statistics to promote better health and wellbeing. Edited by Australian Institute of Health and Welfare. Canberra: Australian Institute of Health and Welfare; 2016.
Australian Bureau of Statistics: 4442.0 Family Characteristics and Transitions 2006–07. Canberra: Australian Bureau of Statistics; 2008.
McFerran L: National Domestic Violence and the workplace survey. Edited by Australian domestic and family violence clearinghouse. New South Wales; 2011.
Hegarty K, Bush R. Prevalence and associations of partner abuse in women attending general practice: a cross-sectional survey. Aust N Z J Public Health. 2002;26(5):437–42.
Hegarty K. Measuring a Multidimensional Definition of Domestic Violence Prevalence of Partner Abuse in Women Attending General Practice. PhD Thesis. Queensland, Australia: University of Queensland; 1999.
Hegarty K. What is intimate partner abuse and how common is it? In: Roberts G, Hegarty K, Feder G, editors. Intimate partner abuse and health professionals New approaches to domestic violence. London: Elsevier; 2006. p. 19–40.
Holden L, Dobson A, Byles J, Chojenta C, Dolja-Gore X, Harris M, Hockey R, Lee C, Loxton D, McLaughlin D, et al. Mental health: findings from the Australian longitudinal study on Women’s health. Report prepared for the Australian Government Department of Health and Ageing. Canberra: Australian Government Department of Health and Ageing; 2013.
Elliott D, Guy J. Mental-health professionals versus non-mental-health professionals - childhood trauma and adult functioning. Professional Psychology-Research and Practice. 1993;24(1):83–90.
Bell H, Kulkarni S, Dalton L. Organizational prevention of vicarious trauma. Families in Society-The Journal of Contemporary Human Services. 2003;84(4):463–70.
Edwards P, Roberts I, Clarke M, DiGuiseppi C, Pratap S, Wentz R, Kwan I. Increasing response rates to postal questionnaires: systematic review. Br Med J. 2002;324(7347):1183–5.
Visschers J, Jaspaert E, Vervaeke G. Social desirability in intimate partner violence and relationship satisfaction reports: an exploratory analysis. Journal of Interpersonal Violence. 2017;32(9):1401–20.
McNutt L, Lee R. Intimate partner violence prevalence estimation using telephone surveys: understanding the effect of nonresponse bias. Am J Epidemiol. 2000;152(5):438–41.
Smith M. The incidence and prevalence of women abuse in Toronto. Violence Vict. 1987;2:173–87.
Ellsberg M, Heise L, Pena R, Agurto S, Winkvist A. Researching domestic violence against women: methodological and ethical considerations. Stud Fam Plan. 2001;32(1):1–16.
Adams AE, Bybee D, Tolman RM, Sullivan CM, Kennedy AC. Does job stability mediate the relationship between intimate partner violence and mental health among low-income women? Am J Orthopsychiatry. 2013;83(4):600–8.
Cunningham M. Impact of trauma work on social work clinicians: empirical findings. Soc Work. 2003;48(4):451–9.
Acknowledgements
The authors wish to acknowledge and thank the health professionals who generously participated in our survey on an extremely sensitive topic. We appreciate the Sidney Myer Fund for their great support of this work via the PhD stipend for EM. Finally, our thanks go to the Zouki Group of Companies for their assistance with coffee vouchers.
Funding
The authors declare that no funding was directly received for this study. The only financial support for this project was a stipend for the doctoral work of the lead author, EM. The stipend scholarship titled, The Sidney Myer Health Scholarship, was generously provided by the Sidney Myer Fund. In addition, financial support was provided by the Zouki group of Companies through coffee vouchers they sold to the project at a reduced cost. Neither the Sidney Myer Fund or the Zouki group of Companies were involved in any aspect of designing the study, data collection, analysis, or writing the manuscript. The authors have not received financial support from any other organisation for the submitted work, nor have relationships or activities influenced the work.
Availability of data and materials
At present, the data and materials (survey) are not publicly available but can be obtained from the authors upon reasonable request. The Composite Abuse Scale is publically available [27].
Author information
Authors and Affiliations
Contributions
This manuscript is part of the doctoral work of EM. EM, KH and CH participated in the design of the study. EM was primarily responsible for all aspects of the work, including data collection and analysis, with KH contributing significantly to data analysis. EM, KH and CH were all responsible for interpretation of the findings. EM wrote the manuscript, with important contributions during many reviews by KH and CH. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research was approved by both the recruiting hospital and the University of Melbourne Human Research and Ethics Committees (Ethics ID: 1339986, dated 10 May 2013). Consent to participate was implied through completed and returned surveys.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
McLindon, E., Humphreys, C. & Hegarty, K. “It happens to clinicians too”: an Australian prevalence study of intimate partner and family violence against health professionals. BMC Women's Health 18, 113 (2018). https://doi.org/10.1186/s12905-018-0588-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-018-0588-y