Abstract
Background
Breast cancer is the most frequent malignancy among women in Eastern Morocco. In this paper, we provide the first report on molecular breast cancer subtypes in this region. This is the largest population–based study on breast cancer among Moroccan women.
Methods
We analyzed 2260 breast cancer cases diagnosed at the Hassan II Regional Oncology Center between October 2005 and December 2012. Clinico-pathological and therapeutic features were studied. Molecular subtypes were determined and their associations with the clinico-pathological characteristics of the tumors were examined.
Results
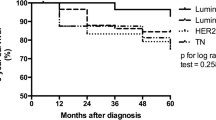
The mean age at diagnosis was 48.7 years ±11.4. Invasive ductal carcinoma was the predominant histological type (77.1%), followed by lobular invasive carcinoma (15.3%). The mean size of breast tumors was 3.5 cm ± 1.96, and 84% of our patients are diagnosed with tumors of more than 2 cm. Histological grade II tumors were the most frequent (70.4%), followed by advanced histological grade (18%). Lymph node positive tumors were observed in 64.8% of cases and 29.3% of patients had distant metastasis. Most tumors were hormone receptor-positive (73%) and 28.6% were HER2 positive. 86.1% of patients with hormone receptor-positive breast cancer were given hormone therapy, while 68.9% of patients with HER2+ breast cancer received targeted therapy with Herceptin. Luminal A was the commonest molecular subtype, followed by Luminal B, Triple Negative and HER2. The highest prevalence of premenopausal patients was observed in Triple Negative subtype (72.2%), followed by HER2 (64.1%), Luminal B (62.2%), and Luminal A (55.1%). Luminal B subtype had a poorer prognosis than Luminal A. Compared with Triple Negative, HER2 subtype tend to spread more aggressively and is associated with poorer prognosis.
Conclusions
Unlike Western countries, breast cancer occurs at an earlier age and is diagnosed at a more advanced stage in Eastern Morocco. In this region, hormone receptor-positive tumors are predominant and so the majority of breast cancer patients should benefit from hormone therapy. HER2 subtype presents an aggressive tendency, suggesting the importance of anti-HER2 therapy. This study will contribute in developing appropriate screening and cancer management strategies in Eastern Morocco.
Similar content being viewed by others
Background
Breast cancer is a major public health problem worldwide. It is the most frequently diagnosed cancer in women worldwide, accounting for a quarter of all cancers in women [1]. In 2012, 1.67 million women were diagnosed with breast cancer [1, 2]. Based upon 2008 estimates, the incidence of breast cancer increased by more than 20%, and mortality increased by 14% [1]. Breast cancer is the most common cause of deaths from cancer in women [1].
Breast cancer is a complex disease characterized by the accumulation of multiple molecular alterations which confer to each tumor a specific phenotype [3–5]. It is a heterogeneous disease, with a variable clinical and pathological behavior and also a different prognosis and response to cancer therapies [6]. In 2000, a molecular classification of breast cancer based on gene expression profiles was proposed for the first time by Perou and his colleagues [7–11]. Then this molecular classification has been validated by several teams [7–11]. Therefore, at least four breast cancer subgroups can be identified: Luminal A and Luminal B (which are positive for the hormone receptors), HER2 (which overexpresses the HER2 growth factor), and Basal-like (which is triple negative: estrogen receptor-negative (ER-), progesterone receptor-negative (PR-), and HER2-negative (HER2-). The identification of these breast cancer molecular subgroups provides important information on the prognosis and the response to treatment of the disease. Indeed, Luminal tumors are associated with a better prognosis compared with basal-like or HER2 tumors which have a more aggressive clinical outcome. Many studies have shown that it is possible to reproduce this molecular classification by using simple immunohistochemical tests based on the expression of ER, PR, HER2, Ki-67 and other biomarkers such as high and low molecular weight cytokeratin CK5/6 [4, 12–16]. Thus, immunohistochemical analysis was used as an alternative to determine the molecular subtypes of breast cancer and their distribution in several populations.
We have shown recently that breast cancer is the most frequent malignancy among women in Eastern Morocco [17]. However, nothing is known about the characteristics of this disease among women in Eastern Morocco. To our knowledge, only two studies on breast cancer molecular subtypes among Moroccan women were published so far. These studies were conducted in the same laboratory and during overlapping time periods. Moreover, these studies were carried out on a small sample size (366–390 cases) and they showed very discrepant results [18, 19]. Therefore, to gain further insight into breast cancer and molecular subtypes among Moroccan women, we studied the clinico-pathological and therapeutic characteristics of 2260 breast cancer cases from Eastern Morocco. Then, molecular subtypes were determined and their associations with the clinico-pathological characteristics of the tumors were examined. This study represents the largest population–based study on breast cancer among Moroccan women.
Methods
Setting
Eastern Morocco is located in the north east of the Kingdom of Morocco, and is the third largest region of the Kingdom [17]. The present retrospective study was based on all female breast cancer cases that were registered at the Hassan II Regional Oncology Center (ROC), since it was created in October 2005 until December 2012. During this study period, the ROC was the only health care facility for cancer management in Eastern Morocco.
Data collection
The data were collected from patient medical records, pathology reports and admission records. A form has been used for collecting information recorded on each breast cancer case, such as the record number, name and surname of the patient, gender, place of residence, age at diagnosis, menopausal status, and clinical characteristics including tumor size, Scarff-Bloom Richardson grade, lymph-node positivity, metastasis status, immunohistochemical (IHC) markers status (ER/PR/HER2), and treatment.
Classification of breast cancer molecular subtypes using IHC data
Tumors were classified into molecular subtypes based on IHC markers status findings [20, 21]. Thus, four subtypes were defined:
Luminal A:
-
ER-positive, PR-positive (>20%), HER2-negative, Ki-67 < 14%.
Luminal B:
-
ER-positive, HER2-negative, and at least one of: Ki-67 ≥ 14%, PR < 20%.
-
ER-positive, HER2-positive, Any Ki-67, Any PR.
HER2:
-
ER-negative, PR-negative, HER2-positive.
Triple Negative:
-
ER-negative, PR-negative, HER2-negative.
Statistical analysis
Data collection was performed on Excel. Statistical analysis was performed using SPSS software version 21.0. To evaluate the correlation between molecular subtypes and clinicopathologic variables we used Chi2 test. To assess the differences between molecular subtypes with regards to age at diagnosis and tumor size we used one-way analysis of variance (ANOVA). The results were considered significant when p (degree of significance) is less than 0.05, very significant when p < 0.01 and highly significant when p < 0.001.
Results
A total of 2406 new cases of female breast cancer were registered at the ROC since it was created in October 2005 until December 2012. 27 cases were in situ breast cancer and were eliminated (1.2% of total) because this study was restricted to invasive breast cancer. 119 cases for which IHC data were not available were also excluded from the study. Thus, 2260 cases of invasive breast cancer were analyzed in this study. Data for age at diagnosis were available for 2220 cases. Among these, the age of patients at diagnosis ranged from 19 to 105 years with a mean age of 48.7 years ±11.4 and a median age of 48 years (Table 1).
Regarding histological tumor type, invasive ductal carcinoma was the most common histological type accounting for 77.1% of all cases, followed respectively by invasive lobular carcinoma (15.3%), medullary carcinoma (1.9%), mucinous carcinoma (1.3%), and papillary carcinoma (0.5%). 3.9% of the cases had cancers of rare histology and were grouped as other types (Table 1). The tumor size was higher than 2 cm in 84% of cases and the mean tumor size was 3.5 cm ± 1.96 (Table 1). According to the SBR grading system, the majority of tumors were grade II accounting for 70.4% of cases, followed respectively by the grade III (18%), and grade I (11.6%) (Table 1). In this study, among patients with known lymph node status, 64.8% had positive lymph-nodes, and among patients with known metastasis status, 29.3% developed distant metastases (Table 1).
Immunohistochemical data revealed that 73% of tumors were hormone receptor-positive breast cancers (ER + and / or PR +), 64.2% were estrogen receptor-positive (ER+), 66.5% were progesterone receptor-positive (PR+) and 28.6% were HER2 positive (HER2+) (Table 1). Among patients with HER2+ breast cancer, 68.9% received targeted therapy with Herceptin (Table 1). While of the cases with hormone receptor-positive breast cancer, 86.1% received hormone therapy (Table 1). Among postmenopausal women with hormone receptor-positive breast cancer and treated with hormone therapy, 79.3% of the cases received Tamoxifen, 15.2% were treated with aromatase inhibitors, and 5.5% received Tamoxifen then aromatase inhibitors (Table 1). In premenopausal patients with hormone receptor-positive breast cancer and treated with hormone therapy, 100% received Tamoxifen (Table 1).
On the basis of the immunohistochemical markers status, the breast cancer cases were classified into four breast cancer molecular subtypes. The distribution of these subgroups is shown in Table 2. Luminal A was the most common subtype (61.1%), followed respectively by Luminal B (16.1%), Triple Negative (14.2%), and then HER2 (8.6%). The characteristics of these breast cancer molecular subtypes in Eastern Morocco are presented in Table 2. The molecular subtypes differed significantly by age at diagnosis (p-value = 0.038) (Table 2). The molecular subtypes have also shown a very significant difference according to menopause status (p-value = 0.004) (Table 2). Indeed, among Triple Negative tumors, 72.2% were premenopausal, while among Luminal A tumors only 55.1% were premenopausal (Table 2).
The molecular subtypes differed significantly by histological type (Fisher exact test p-value = 0.02) (Table 2). The Triple Negative subtype showed the highest prevalence of medullary carcinoma histological type, 5% versus 0.8% Luminal A, 0.5% Luminal B and 0% HER2 (Table 2). Furthermore, Triple Negative subtype showed the lowest prevalence of invasive lobular carcinoma and mucinous carcinoma histological types compared with the other subtypes (Table 2).
The molecular subtypes did not differ by mean size of tumors at diagnosis (p-value = 0.097) (Table 2). However, we found significant difference by tumor size among breast cancer subtypes when stratified into groups: < 2.0 cm, 2.0 – 5.0 cm, and > 5.0 cm (p-value = 0.005) (Table 2). Regarding the histological grade, the molecular subtypes differed significantly (p-value <0.0001) (Table 2). The HER2 and Triple Negative subtypes had the highest percentage of advanced histological grade (grade III) in comparison with the Luminal subtypes (Table 2).
All molecular subtypes had a high percentage of vascular emboli, with 73%, 72%, 67.1%, and 61.9% for Luminal B, HER2, Luminal A, and Triple Negative respectively (Table 2). However, the molecular subtypes did not differ significantly with regards to vascular emboli status (p-value = 0.209). Nevertheless, in comparison to Triple Negative, patients with HER2 subtype had a higher percentage of vascular emboli. Regarding lymph node status at time of diagnosis, the molecular subtypes did not differ significantly (p-value = 0.114) (Table 2). HER2 subtype had the highest prevalence of positive lymph nodes (71.4%), followed respectively by Luminal B (67.1%), Luminal A (63.9%) and finally Triple negative (59.2%) (Table 2). Concerning the metastasis status, the molecular subtypes did not differ significantly (p-value = 0.059) (Table 2). HER2 subtype showed with the highest level of metastases, 41.9% versus 27.6% Luminal A and 25.5% Luminal B (Table 2). Moreover, in comparison to Triple Negative, patients with HER2 subtype had a higher level of metastases.
Discussion
Breast cancer is the main cause of death among women worldwide [22, 23]. Breast cancer is a complex and heterogeneous disease associated with clinical, pathological and biological factors that are variable from one population to another [4]. These prognostic factors are essential for the management of breast cancer. Moreover, molecular classification of breast cancer is now an important tool to guide patient management. Therefore, to gain further insight into breast cancer and molecular subtypes among Moroccan women, we analyzed 2260 breast cancer cases from Eastern Morocco. Thus, to our knowledge this paper represents the first study in Morocco on breast cancer using a large series of patients.
Age at diagnosis of breast cancer in Eastern Morocco
Our study revealed that in Eastern Morocco the age at the time of breast cancer diagnosis was between 19 and 105 years, with a mean age of 48.7 years ±11.4 and a median age of 48 years. This result is similar to those reported in other North African countries, Iraq, Sub-Saharan Africa, Korea, China, and Taiwan [18, 24–32]. However, in Western countries and other Arab and Asian countries breast cancer occurs at an older age [26, 27, 33–36]. The age at diagnosis represents an important prognostic factor since tumors diagnosed at younger ages are generally more aggressive and/or less responsive to treatment [37–39]. Multiple factors may be involved in the age at diagnosis, including the structure of the population, genetic and environmental factors. In Eastern Morocco, this young age at diagnosis of breast cancer may be simply due to the young population in this region [40]. Further studies are needed to confirm the involvement of these factors in the occurrence of cancer at a younger age in Eastern Morocco.
Histological types of breast cancer in Eastern Morocco
In our study, invasive ductal carcinoma was the predominant histological type, which is similar to most previous studies on breast cancer [13, 28–30, 41–47]. Lobular invasive carcinoma was the second most common histological type accounting for 15.3% of all cases. This level of lobular invasive carcinoma in our study is higher compared to what has been reported in Fez (Morocco) (4%), Egypt (9%), Saudi Arabia (3%) and Iraq (3.9%) [18, 26, 36, 48].
Clinico-pathological features of breast cancer in eastern Morocco
In Western countries the majority of breast tumors measure less than 2 cm, reflecting the early detection of the disease [33, 36, 49–51]. In our series, the mean size of breast tumors was 3.5 cm ± 1.96, which is similar to those reported in Fez (Morocco), and in other Arab countries [18, 24, 36]. However, the percentage of tumors that measure larger than 2 cm was higher in our study as compared to those observed in other Arab and Asian studies [27, 35, 52–55]. In this study, we found a high percentage of histological grade II tumors (70.4%) and an intermediate level of advanced histological grade (18%). Such a finding is far from that reported in Fez, where a lower percentage of grade II tumors (54.7%), and a higher level of histological grade III (30.7%) were observed [33]. Lymph node positive tumors were observed in 64.8% of cases and 29.3% of patients had distant metastasis. The previous Fez study showed a lower percentage of positive lymph nodes (53%) and distant metastasis (17.5%) [33]. In developed countries, the majority of patients have a negative lymph node status [13, 50, 56, 57]. This is due to efficient breast cancer screening programs, which contribute to the early diagnosis of breast cancer [58, 59]. Therefore, the high rate of metastasis observed in this study is probably due to late diagnosis of breast cancer and highlights the necessity of establishing an effective breast cancer screening program in Eastern Morocco.
Hormone receptor status and hormone therapy in Eastern Morocco
Our study revealed that in Eastern Morocco, 64.2% of tumors were ER+. Such a finding is similar to those observed in other North African countries, Saudi Arabia, China and the United States [13, 28, 41, 60–65]. Regarding the PR status, we found that the majority of tumors were PR+ (66.5%). This result is similar to those reported in Fez, Saudi Arabia, but higher than the figure reported in other North African countries [13, 28, 41, 60–65]. Hormone Receptor (HR) status has important implications for breast cancer prognosis and management. Indeed, hormone receptor-positive tumors are usually associated with a favourable prognosis and can be given endocrine therapy. Thus, the assessment of HR using IHC assays is essential before any treatment. However, in low-income countries, HR status is not performed for patients of low-resource. In such countries, if the prevalence of hormone receptor-positive tumors is very high it is possible to apply hormone therapy even among patients in whom HR status has not been conducted [66, 67]. Regarding hormone therapy, a number of studies have previously shown that treatment of ER+ breast cancer with Tamoxifen significantly reduces the risk of recurrence and mortality [68, 69]. Tamoxifen is a drug that works by preventing the binding of estrogen to tumor cells, and is effective in both postmenopausal and premenopausal patients. Aromatase inhibitors (AIs) are another class of drugs that are used to treat postmenopausal patients with hormone receptor-positive breast cancer. Several studies have recently shown that treatment of hormone receptor-positive breast cancer in postmenopausal women with either aromatase inhibitors (AIs) alone or after Tamoxifen gives a clear advantage in comparison with treatment using Tamoxifen alone [70, 71].
In this study, we found that 86.1% of patients with HR+ breast cancer were given hormone therapy. Tamoxifen was used to treat the majority of our premenopausal (100% of cases) and postmenopausal (79.3% of cases) patients. Only 15.2% of postmenopausal patients received AIs alone, and 5.5% of cases were treated with AIs after Tamoxifen. Together, these population-based estimates of the HR status in Eastern Morocco can aid treatment decisions. These data indicate that since in Eastern Morocco the majority of patients showed hormone receptor-positive breast cancer, hormone therapy should be applied even for patients in whom HR status has not been conducted. Moreover, therapy with AIs should be used more often in the case of postmenopausal patients with hormone receptor-positive breast cancer.
HER2 status and targeted therapy in Eastern Morocco
In this study, we found that 28.6% of tumors were HER2+. This result is similar to those reported in other North African countries, Saudi Arabia, but higher than the figure reported in Europe, the United States and most countries in Sub-Saharan Africa [13, 18, 28, 30, 60, 62, 63, 65, 72, 73]. Women whose breast cancers test positive for HER2 can be given targeted therapy. Herceptin is a monoclonal antibody that directly targets the HER2 protein. In 2006, this drug has been approved by the FDA (US Food and Drug Administration) for the treatment of all HER2+ breast cancers [74]. It is currently the standard treatment for HER2+ tumor, and it is used in combination with other treatment [75–77]. In this study, we found that only 68.9% of patients with HER2+ breast cancer received targeted therapy with Herceptin. Together, these data indicate that in Eastern Morocco, tumors overexpressing HER2 protein are frequent and thereby should benefit from targeted therapy. Thus, affordable treatment for HER2-positive tumors with targeted therapy aimed at HER2 is needed in Eastern Morocco.
Distribution of molecular breast cancer subtypes in Eastern Morocco
As mentioned earlier, only two studies have been reported on molecular breast cancer subtypes among Moroccan women [18]. Although these studies were conducted in the same laboratory and during overlapping time periods these showed very discrepant results: Luminal B was the most frequent molecular subtype in El Fatemi et al., (2012), while Luminal A was the predominant subtype in Bennis et al., (2012). In this study, Luminal A was the commonest molecular subtype with 61.1%. This result is similar to that reported in white American population (62%) (Table 3) [78]. However, a lower frequency of Luminal A has been reported in other North African countries (30.5–53.6%), Sub-Saharan countries (25.6–53.5%), China (48.6%), black, Hispanic and Asian American (47–55%) (Table 3) [42, 45, 60, 62, 65, 79–81]. A higher prevalence of Luminal A than our series has been reported in European countries (68.7–75%) (Table 3) [45, 60, 62, 65, 79, 80]. The proportion of Luminal B in this study (16.1%) is similar to that found in other North African countries (13.4–19.7%), and China (16.7%) (Table 3) [45, 60, 62, 65, 79, 80]. However, a lower frequency of Luminal B than our series has been reported in Sub-Saharan African countries (12.2–14.6%), European countries (6–12.5%), and American population (9–12%) (Table 3) [45, 60, 62, 65, 79, 80].
The HER2 subtype in this study accounted for 8.6% of all breast cancer cases, which is similar to that reported in Algeria (8.9%), but lower than in other North African countries (9.2–14.5%), and China (13.7%) (Table 3) [45, 60, 62, 65, 79, 80]. A lower prevalence of HER2 than our series has been reported in American population (4–8%) and European countries (3–8%) (Table 3) [45, 60, 62, 65, 79, 80]. The prevalence of Triple Negative in this study (14.2%) is slightly higher than in European countries (11.8–12%), China (12.9%), and the white, Hispanic and Asian ethnic groups of the US population (9–13%) (Table 3) [45, 60, 62, 65, 79, 80]. A higher proportion of Triple Negative than our series has been reported in other North African countries (18–22.5%), Sub-Saharan African patients (20.5–49.4%) and black American (20%) (Table 3) [45, 60, 62, 65, 79, 80].
Together, these data suggest that the distribution of molecular subtypes among Moroccan women is similar to that reported in most studies over the world, with Luminal A being the most common subtype, followed by Luminal B, Triple Negative and HER2. The most likely explanation for the discrepancies among the two previous studies carried out in Fez in Morocco seems to be differences in sensitivity of the method of HR status assessment and/or in the criteria for classifying molecular breast cancer subtypes.
Molecular breast cancer subtypes associations with clinico-pathological factors
The molecular subtype showed no statically significant difference according to mean size of tumors at diagnosis, vascular emboli status, lymph node status or metastasis status. However, molecular subtype differed significantly with regards to age at diagnosis. We found that the Triple Negative subtype was associated with a younger age at diagnosis compared with the other subtypes, similar to previous reports on different populations [13, 42, 63, 82, 83]. The molecular subtypes have also shown a very significant difference by menopause status. The highest prevalence of premenopausal patients was observed in Triple Negative subtype, while Luminal A was associated with the lowest prevalence of premenopausal patients, consistent with previous studies [13, 84–86].
Regarding the histological grade, a significant difference was noted among the molecular subtypes. Luminal A was associated with the lowest proportion of histological grade III, association that has been noted by other studies [4, 13, 41, 42, 45, 83, 85, 87]. Luminal A had also the lowest proportion of tumors with diameter larger than 5 cm. These findings are consistent with previous studies that have shown that Luminal A tumors tend to be slow-growing and are associated with a good prognosis [4, 88]. In this study, Luminal A subtype had a better prognosis than Luminal B subtype. Indeed, in comparison with Luminal A, Luminal B had a higher percentage of tumors with a large diameter (>5.0 cm), a larger proportion of histological grade III, and a higher percentage of vascular emboli and lymph node involvement. These data are consistent with previous studies [89, 90].
In comparison with the other subtype, Triple Negative was associated with the highest proportion of histological grade III, the lowest median age at diagnosis, and the highest prevalence of premenopausal patients. These are consistent with several previous studies that have shown that Triple Negative is more common in premenopausal women and it is an aggressive subtype [13]. In this study, we found also that Triple Negative subtype had the lowest prevalence of positive lymph nodes and the lowest proportion of positive vascular emboli. These results are in accordance with previous studies that have shown that Triple Negative is less likely to demonstrate positive lymph nodes and positive vascular emboli when compared with the other subtypes [91, 92]. In our series, Triple Negative subtype showed the highest prevalence of medullary carcinoma. Previous studies have shown that this histological type is characterized by a high histological grade and rare lymph node metastasis [91, 92]. Interestingly, these clinico-pathologic features of medullary carcinoma are consistent with those observed for Triple Negative subtype in this study.
In comparison with Triple Negative subtype, HER2 had similar percentage of tumors with a large diameter (>5 cm) (34.6% versus 34%), but a higher percentage of lymph-node positive tumors (71.4% versus 59.2%), a larger proportion of positive vascular emboli (72% versus 61.9%), and a higher level of distant metastases (41.9% versus 30.1%). Together, these data indicate that in Eastern Morocco, HER2 breast cancers tend to grow and spread more aggressively than Triple Negative subtype breast cancers and are associated with poorer prognosis, and thus highlight the need to the use of targeted therapies for HER2 cancers in this region.
Conclusions
This study revealed alarming features of breast cancer in Eastern Morocco, with a large tumor size, a high histological grade, a significant percentage of vascular emboli, a large percentage of lymph node involvement, and distant metastases. Thus, our finding highlights the importance to strengthen the breast cancer screening program in Eastern Morocco. Moreover, the observed occurrence of breast cancer at a younger age in Eastern Morocco justifies the need to establish a screening program at an earlier age in this region. Our results indicate that in Eastern Morocco, hormone receptor-positive and HER2+ tumors are predominant and so the majority of breast cancer cases in this population may benefit from hormone therapy and/or targeted therapy. Molecular subtype analyses revealed that Luminal A was the commonest molecular subtype, followed by Luminal B, Triple Negative and HER2. Luminal B subtype in our study had a poorer prognosis than Luminal group A. Compared with the Triple Negative subtype, the HER2 subtype in our study tends to spread more aggressively and has a poorer prognosis, suggesting the importance of anti-HER2 therapy. This study will contribute in developing appropriate screening and cancer management strategies in Eastern Morocco.
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–86. doi:10.1002/ijc.29210.
Bray F, Ren JS, Masuyer E, Ferlay J. Global estimates of cancer prevalence for 27 sites in the adult population in 2008. Int J Cancer. 2013;132(5):1133–45.
Rouzier R, Perou CM, Symmans WF, Ibrahim N, Cristofanilli M, Anderson K, et al. Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res. 2005;11(16):5678–85. doi:10.1158/1078-0432.ccr-04-2421.
Blows FM, Driver KE, Schmidt MK, Broeks A, Van Leeuwen FE, Wesseling J, et al. Subtyping of breast cancer by immunohistochemistry to investigate a relationship between subtype and short and long term survival: a collaborative analysis of data for 10,159 cases from 12 studies. PLoS Med. 2010;7(5), e1000279.
de Ruijter TC, Veeck J, de Hoon JP, van Engeland M, Tjan-Heijnen VC. Characteristics of triple-negative breast cancer. J Cancer Res Clin Oncol. 2011;137(2):183–92.
Pusztai L, Mazouni C, Anderson K, Wu Y, Symmans WF. Molecular classification of breast cancer: limitations and potential. Oncologist. 2006;11(8):868–77.
Perou CM, Sørlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000;406(6797):747–52.
Van't Veer LJ, Dai H, Van De Vijver MJ, He YD, Hart AA, Mao M, et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature. 2002;415(6871):530–36.
Sørlie T, Tibshirani R, Parker J, Hastie T, Marron J, Nobel A, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci U S A. 2003;100(14):8418–23.
Sotiriou C, Neo S-Y, McShane LM, Korn EL, Long PM, Jazaeri A, et al. Breast cancer classification and prognosis based on gene expression profiles from a population-based study. Proc Natl Acad Sci U S A. 2003;100(18):10393–98. doi:10.1073/pnas.1732912100.
Soerjomataram I, Louwman MW, Ribot JG, Roukema JA, Coebergh JWW. An overview of prognostic factors for long-term survivors of breast cancer. Breast Cancer Res Treat. 2008;107(3):309–30.
Nielsen TO, Hsu FD, Jensen K, Cheang M, Karaca G, Hu Z, et al. Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res. 2004;10(16):5367–74.
Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295(21):2492–502.
Hu Z, Fan C, Oh DS, Marron J, He X, Qaqish BF, et al. The molecular portraits of breast tumors are conserved across microarray platforms. BMC Genomics. 2006;7(1):96.
Cheang MC, Chia SK, Voduc D, Gao D, Leung S, Snider J, et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst. 2009;101(10):736–50.
Cheang MC, Voduc D, Bajdik C, Leung S, McKinney S, Chia SK, et al. Basal-like breast cancer defined by five biomarkers has superior prognostic value than triple-negative phenotype. Clin Cancer Res. 2008;14(5):1368–76.
Elidrissi Errahhali M, Elidrissi Errahhali M, Abda N, Bellaoui M. Exploring Geographic Variability in Cancer Prevalence in Eastern Morocco: A Retrospective Study over Eight Years. PLoS One. 2016;11(3), e0151987. doi:10.1371/journal.pone.0151987.
Bennis S, Abbass F, Akasbi Y, Znati K, Joutei KA, El Mesbahi O, et al. Prevalence of molecular subtypes and prognosis of invasive breast cancer in north-east of Morocco: retrospective study. BMC Res Notes. 2012;5(1):436.
El Fatemi H, Chahbouni S, Jayi S, Moumna K, Melhouf MA, Bannani A, et al. Luminal B tumors are the most frequent molecular subtype in breast cancer of North African women: an immunohistochemical profile study from Morocco. Diagn Pathol. 2012;7(1):170.
Goldhirsch A, Winer EP, Coates A, Gelber R, Piccart-Gebhart M, Thürlimann B, et al. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol. 2013;24(9):2206–23.
Prat A, Cheang MCU, Martín M, Parker JS, Carrasco E, Caballero R, et al. Prognostic significance of progesterone receptor–positive tumor cells within immunohistochemically defined luminal A breast cancer. J Clin Oncol. 2012;31(2):203–9. doi:10.1200/JCO.2012.43.4134.
Soerjomataram I, Lortet-Tieulent J, Parkin DM, Ferlay J, Mathers C, Forman D, et al. Global burden of cancer in 2008: a systematic analysis of disability-adjusted life-years in 12 world regions. Lancet. 2012;380(9856):1840–50.
Ferlay J, Shin H-R, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893–917.
Almasri NM, Al HM. Immunohistochemical evaluation of human epidermal growth factor receptor 2 and estrogen and progesterone receptors in breast carcinoma in Jordan. Breast Cancer Res. 2005;7(5):R598–604.
Park S, Han W, Kim J, Kim MK, Lee E, Yoo T-K, et al. Risk factors associated with distant metastasis and survival outcomes in breast cancer patients with locoregional recurrence. J Breast Cancer. 2015;18(2):160–66. doi:10.4048/jbc.2015.18.2.160.
Runnak AM, Mohammed HA, Hassan HA, Abdulmahdi WA, Rashid RM, Hughson MD. A population-based study of Kurdish breast cancer in northern Iraq: hormone receptor and HER2 status. A comparison with Arabic women and United States SEER data. BMC Women's Health. 2012;12(1):16.
Kallel I, Khabir A, Boujelbene N, Abdennadher R, Daoud J, Frikha M, et al. EGFR overexpression relates to triple negative profile and poor prognosis in breast cancer patients in Tunisia. J Recept Sig Transduct. 2012;32(3):142–49.
Salhia B, Tapia C, Ishak EA, Gaber S, Berghuis B, Hussain KH, et al. Molecular subtype analysis determines the association of advanced breast cancer in Egypt with favorable biology. BMC Women's Health. 2011;11(1):44.
Missaoui N, Jaidene L, Abdelkrim SB, Abdelkader AB, Beizig N, Yaacoub LB, et al. Breast cancer in Tunisia: clinical and pathological findings. Asian Pac J Cancer Prev. 2011;12(1):169–72.
Cherbal F, Gaceb H, Mehemmai C, Saiah I, Bakour R, Rouis AO, et al. Distribution of molecular breast cancer subtypes among Algerian women and correlation with clinical and tumor characteristics: A population-based study. Breast Dis. 2015;35(2):95–102.
Abdelkrim SB, Trabelsi A, Missaoui N, Beizig N, Bdioui A, Anjorin A, et al. Distribution of molecular breast cancer subtypes among Tunisian women and correlation with histopathological parameters: a study of 194 patients. Pathol Res Pract. 2010;206(11):772–75.
Fregene A, Newman LA. Breast cancer in sub-Saharan Africa: How does it relate to breast cancer in African-American women? Cancer. 2005;103(8):1540–50.
Blamey R, Hornmark-Stenstam B, Ball G, Blichert-Toft M, Cataliotti L, Fourquet A, et al. ONCOPOOL–a European database for 16,944 cases of breast cancer. Eur J Cancer. 2010;46(1):56–71.
Parise C, Caggiano V. Disparities in the risk of the ER/PR/HER2 breast cancer subtypes among Asian Americans in California. Cancer Epidemiol. 2014;38(5):556–62.
Aiad HA, Wahed MM, Asaad NY, El‐Tahmody M, Elhosary E. Immunohistochemical expression of GPR30 in breast carcinoma of Egyptian patients: an association with immunohistochemical subtypes. APMIS. 2014;122(10):976–84.
Khabaz MN. Immunohistochemistry Subtypes (ER/PR/HER) of Breast Cancer: Where Do We Stand in the West of Saudi Arabia? Asian Pac J Cancer Prev. 2013;15(19):8395–400.
Kheirelseid EA, Boggs JM, Curran C, Glynn RW, Dooley C, Sweeney KJ, et al. Younger age as a prognostic indicator in breast cancer: a cohort study. BMC Cancer. 2011;11(1):383.
Fredholm H, Eaker S, Frisell J, Holmberg L, Fredriksson I, Lindman H. Breast cancer in young women: poor survival despite intensive treatment. PLoS One. 2009;4(11), e7695.
Gnerlich JL, Deshpande AD, Jeffe DB, Sweet A, White N, Margenthaler JA. Elevated breast cancer mortality in women younger than age 40 years compared with older women is attributed to poorer survival in early-stage disease. J Am Coll Surg. 2009;208(3):341–47.
HCP. Monograph of the region of Eastern Morocco 2012 (In French). Oujda Regional Direction. http://www.hcp.ma/region-oriental/docs/monographieFr2012/monographie%202012.pdf.
Su Y, Zheng Y, Zheng W, Gu K, Chen Z, Li G, et al. Distinct distribution and prognostic significance of molecular subtypes of breast cancer in Chinese women: a population-based cohort study. BMC Cancer. 2011;11(1):292. doi:10.1186/1471-2407-11-292.
McCormack VA, Joffe M, van den Berg E, Broeze N, dos Santos SI, Romieu I, et al. Breast cancer receptor status and stage at diagnosis in over 1,200 consecutive public hospital patients in Soweto, South Africa: a case series. Breast Cancer Res. 2013;15(5):R84. doi:10.1186/bcr3478.
Mahyari HM, Khosravi A, Mahyari ZM, Monfared ZE, Khosravi N. Overexpression of HER2/neu as a Prognostic Value in Iranian Women With Early Stage Breast Cancer; A Single Institute Study. Iran Red Crescent Med J. 2014; 16(11). doi: 10.5812/ircmj. 16005. eCollection 2014.
Banegas MP, Tao L, Altekruse S, Anderson WF, John EM, Clarke CA, et al. Heterogeneity of breast cancer subtypes and survival among Hispanic women with invasive breast cancer in California. Breast Cancer Res Treat. 2014;144(3):625–34.
Puig-Vives M, Sánchez M, Sánchez-Cantalejo J, Torrella-Ramos A, Martos C, Ardanaz E, et al. Distribution and prognosis of molecular breast cancer subtypes defined by immunohistochemical biomarkers in a Spanish population-based study. Gynecol Oncol. 2013;130(3):609–14.
Singh M, Ding Y, Zhang L-Y, Song D, Gong Y, Adams S, et al. Distinct breast cancer subtypes in women with early-onset disease across races. Am J Cancer Res. 2014;4(4):337–52. eCollection 2014.
El-Zaemey S, Nagi N, Fritschi L, Heyworth J. Breast cancer among Yemeni women using the National Oncology Centre Registry 2004–2010. Cancer Epidemiol. 2012;36(3):249–53.
Ayadi L, Khabir A, Amouri H, Karray S, Dammak A, Guermazi M, et al. Correlation of HER-2 over-expression with clinico-pathological parameters in Tunisian breast carcinoma. World J Surg Oncol. 2008;6(1):112–19.
Parise CA, Bauer KR, Caggiano V. Variation in breast cancer subtypes with age and race/ethnicity. Crit Rev Oncol Hematol. 2010;76(1):44–52.
Taucher S, Rudas M, Mader RM, Gnant M, Dubsky P, Bachleitner T, et al. Do we need HER-2/neu testing for all patients with primary breast carcinoma? Cancer. 2003;98(12):2547–53.
Duffy SW, Tabar L, Vitak B, Warwick J. Tumor size and breast cancer detection: what might be the effect of a less sensitive screening tool than mammography? Breast J. 2006;12(s1):S91–5.
Aryandono T, Harijadi S. Hormone receptor status of operable breast cancers in Indonesia: Correlation with other prognostic factors and survival. Asian Pac J Cancer Prev. 2006;7(2):321–4.
Azizun-Nisa BY, Raza F, Kayani N. Comparison of ER, PR and HER-2/neu (C-erb B 2) reactivity pattern with histologic grade, tumor size and lymph node status in breast cancer. Asian Pac J Cancer Prev. 2008;9(4):553–6.
Vaidyanathan K, Kumar P, Reddy C, Deshmane V, Somasundaram K, Mukherjee G. ErbB-2 expression and its association with other biological parameters of breast cancer among Indian women. Indian J Cancer. 2010;47(1):8.
Ambroise M, Ghosh M, Mallikarjuna V, Kurian A. Immunohistochemical profile of breast cancer patients at a tertiary care hospital in South India. Asian Pac J Cancer Prev. 2011;12(3):625–9.
Stead LA, Lash TL, Sobieraj JE, Chi DD, Westrup JL, Charlot M, et al. Triple-negative breast cancers are increased in black women regardless of age or body mass index. Breast Cancer Res. 2009;11(2):R18.
Huang H, Neven P, Drijkoningen M, Paridaens R, Wildiers H, Van Limbergen E, et al. Association between tumour characteristics and HER-2/neu by immunohistochemistry in 1362 women with primary operable breast cancer. J Clin Pathol. 2005;58(6):611–16.
Ernst MF, Roukema JA, Coebergh J-WW, van Driel OJR, van Beek MW, van der Sangen MJ, et al. Breast cancers found by screening: earlier detection, lower malignant potential or both? Breast Cancer Res Treat. 2002;76(1):19–25.
Gill P, Farshid G, Luke C, Roder D. Detection by screening mammography is a powerful independent predictor of survival in women diagnosed with breast cancer. Breast. 2004;13(1):15–22.
Awadelkarim KD, Arizzi C, Elamin EO, Hamad HM, De Blasio P, Mekki SO, et al. Pathological, clinical and prognostic characteristics of breast cancer in Central Sudan versus Northern Italy: implications for breast cancer in Africa. Histopathology. 2008;52(4):445–56.
Lin C-H, Liau J-Y, Lu Y-S, Huang C-S, Lee W-C, Kuo K-T, et al. Molecular Subtypes of Breast Cancer Emerging in Young Women in Taiwan: Evidence for More Than Just Westernization as a Reason for the Disease in Asia. Cancer Epidemiol Biomark Prev. 2009;18(6):1807–14. doi:10.1158/1055-9965.epi-09-0096.
Spitale A, Mazzola P, Soldini D, Mazzucchelli L, Bordoni A. Breast cancer classification according to immunohistochemical markers: clinicopathologic features and short-term survival analysis in a population-based study from the South of Switzerland. Ann Oncol. 2009;20(4):628–35.
Fourati A, Boussen H, El May MV, Goucha A, Dabbabi B, Gamoudi A, et al. Descriptive analysis of molecular subtypes in Tunisian breast cancer. Asia Pac J Clin Oncol. 2012;10(2):e69–74.
Xue C, Wang X, Peng R, Shi Y, Qin T, Liu D, et al. Distribution, clinicopathologic features and survival of breast cancer subtypes in Southern China. Cancer Sci. 2012;103(9):1679–87. doi:10.1111/j.1349-7006.2012.02339.x.
Rudat V, El-Sweilmeen H, Brune-Erber I, Nour AA, Almasri N, Altuwaijri S, et al. Identification of breast cancer patients with a high risk of developing brain metastases: a single-institutional retrospective analysis. BMC Cancer. 2014;14(1):289. doi:10.1186/1471-2407-14-289.
Kantelhardt EJ, Mathewos A, Aynalem A, Wondemagegnehu T, Jemal A, Vetter M, et al. The prevalence of estrogen receptor-negative breast cancer in Ethiopia. BMC Cancer. 2014;14:895. doi:10.1186/1471-2407-14-895.
Adjei EK, Owusu-Afriyie O, Awuah B, Stalsberg H. Hormone Receptors and Her2 Expression in Breast Cancer in Sub-Saharan Africa. A Comparative Study of Biopsies from Ghana and Norway. Breast J. 2014;20(3):308–11. doi:10.1111/tbj.12261.
Davies C, Pan H, Godwin J, Gray R, Arriagada R, Raina V, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381(9869):805–16.
EBCTC Group. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet. 2011;378(9793):771–84.
Dowsett M, Cuzick J, Ingle J, Coates A, Forbes J, Bliss J, et al. Meta-analysis of breast cancer outcomes in adjuvant trials of aromatase inhibitors versus tamoxifen. J Clin Oncol. 2010;28(3):509–18.
Group EBCTC. Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. Lancet. 2015;386(10001):1341–52.
Adebamowo CA, Famooto A, Ogundiran TO, Aniagwu T, Nkwodimmah C, Akang EE. Immunohistochemical and molecular subtypes of breast cancer in Nigeria. Breast Cancer Res Treat. 2008;110(1):183–88.
Ly M, Antoine M, Dembélé AK, Levy P, Rodenas A, Touré BA, et al. High incidence of triple-negative tumors in sub-saharan Africa: a prospective study of breast cancer characteristics and risk factors in Malian women seen in a Bamako university hospital. Oncology. 2012;83(5):257–63.
Wolff AC, Hammond MEH, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, et al. American Society of Clinical Oncology/College of American Pathologists Guideline Recommendations for Human Epidermal Growth Factor Receptor 2 Testing in Breast Cancer. Arch Pathol Lab Med. 2007;131(1):18–43.
von Minckwitz G, Du Bois A, Schmidt M, Maass N, Cufer T, de Jongh FE, et al. Trastuzumab beyond progression in human epidermal growth factor receptor 2–positive advanced breast cancer: A German Breast Group 26/Breast International Group 03–05 study. J Clin Oncol. 2009;27(12):1999–2006. doi:10.1200/JCO.2008.19.6618.
Horton J. Trastuzumab use in breast cancer: clinical issues. Cancer Control. 2002;9(6):499–07.
Giordano SH, Temin S, Kirshner JJ, Chandarlapaty S, Crews JR, Davidson NE, et al. Systemic therapy for patients with advanced human epidermal growth factor receptor 2–positive breast cancer: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2014;32(19):2078–99. doi:10.1200/JCO.2013.54.0948.
Clarke CA, Keegan TH, Yang J, Press DJ, Kurian AW, Patel AH, et al. Age-specific incidence of breast cancer subtypes: understanding the black–white crossover. J Natl Cancer Inst. 2012;104(14):1094–101.
Yang XR, Sherman ME, Rimm DL, Lissowska J, Brinton LA, Peplonska B, et al. Differences in Risk Factors for Breast Cancer Molecular Subtypes in a Population-Based Study. Cancer Epidemiol Biomarkers Prev. 2007;16(3):439–43.
Shomaf M, Masad J, Najjar S, Faydi D. Distribution of breast cancer subtypes among Jordanian women and correlation with histopathological grade: molecular subclassification study. JRSM Short Rep. 2013;4(10):2042533313490516.
Seshie B, Adu-Aryee NA, Dedey F, Calys-Tagoe B, Clegg-Lamptey J-N. A retrospective analysis of breast cancer subtype based on ER/PR and HER2 status in Ghanaian patients at the Korle Bu Teaching Hospital, Ghana. BMC Clin Pathol. 2015;15:14. doi:10.1186/s12907-015-0014-4. eCollection 2015.
El Saghir NS, Assi HA, Jaber SM, Khoury KE, Nachef Z, Mikdashi HF, et al. Outcome of Breast Cancer Patients Treated outside of Clinical Trials. J Cancer. 2014;5(6):491–8.
Ihemelandu CU, Leffall LD, Dewitty RL, Naab TJ, Mezghebe HM, Makambi KH, et al. Molecular breast cancer subtypes in premenopausal and postmenopausal African-American women: age-specific prevalence and survival. J Surg Res. 2007;143(1):109–18.
Kurebayashi J, Moriya T, Ishida T, Hirakawa H, Kurosumi M, Akiyama F, et al. The prevalence of intrinsic subtypes and prognosis in breast cancer patients of different races. Breast. 2007;16:72–7.
Al Tamimi DM, Shawarby MA, Ahmed A, Hassan AK, AlOdaini AA. Protein expression profile and prevalence pattern of the molecular classes of breast cancer-a Saudi population based study. BMC Cancer. 2010;10(1):223.
Turkoz FP, Solak M, Petekkaya I, Keskin O, Kertmen N, Sarici F, et al. Association between common risk factors and molecular subtypes in breast cancer patients. Breast. 2013;22(3):344–50.
Belkacemi Y, Penault-Llorcac F, Gligorovd J, Azriaf D. The use of breast cancer subtype classification to predict local and distant recurrence. A review. Cancer Radiother. 2008;12(6–7):577–83. doi:10.1016/j.canrad.2008.08.272.
Bhargava R, Striebel J, Beriwal S, Flickinger JC, Onisko A, Ahrendt G, et al. Prevalence, morphologic features and proliferation indices of breast carcinoma molecular classes using immunohistochemical surrogate markers. Int J Clin Exp Pathol. 2009;2(5):444–55.
Colombo PE, Milanezi F, Weigelt B, Reis-Filho JS. Microarrays in the 2010s: the contribution of microarray-based gene expression profiling to breast cancer classification, prognostication and prediction. Breast Cancer Res. 2011;13(3):212. doi:10.1186/bcr2890.
Reis-Filho JS, Pusztai L. Gene expression profiling in breast cancer: classification, prognostication, and prediction. Lancet. 2011;378(9805):1812–23.
Park I, Kim J, Kim M, Bae SY, Lee SK, Kil WH, et al. Comparison of the characteristics of medullary breast carcinoma and invasive ductal carcinoma. J Breast Cancer. 2013;16(4):417–25.
Foulkes WD, Smith IE, Reis-Filho JS. Triple-negative breast cancer. N Engl J Med. 2010;363(20):1938–48.
Acknowledgments
We are grateful to the clinical team and to all administrative staff at Hassan II Regional Oncology Center of Oujda for their support. We thank Dr. N. Abda for her support. We also thank the Regional Director of the Ministry of Health in Eastern Morocco for his support. We are grateful to Dr. A. Azzouzi and all the administrative staff of the Faculty of Medicine and Pharmacy of Oujda for heir valuable support and encouragement throughout the entire work.
Funding
No funding was received for this study.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
MEE, MEE, MO, TEH, SA and MB conceived the study. MEE, MEE, MO and MB designed the study. MEE and MEE collected the data. MEE, MEE, and MB, carried out the analysis. MEE and MB wrote the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
In this retrospective study, obtaining consent for publication was not possible. Therefore, we were granted a waiver by the Ethical Review Committee and the National Commission of control of Personal Data Protection.
Ethics approval and consent to participate
Our study protocol was ethically approved by the Ethical Review Committee for Biomedical Research of the Faculty of Medicine and Pharmacy of Casablanca under the number 41/14. In this study, because obtaining informed consent was not possible, we were granted a waiver of consent by the Ethical Review Committee. Patient records/information was anonymized and de-identified prior to analysis. The authorization for personal data processing was obtained from the National Commission of control of Personal Data Protection under the number A-RS-280/2014).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Elidrissi Errahhali, M., Elidrissi Errahhali, M., Ouarzane, M. et al. First report on molecular breast cancer subtypes and their clinico-pathological characteristics in Eastern Morocco: series of 2260 cases. BMC Women's Health 17, 3 (2017). https://doi.org/10.1186/s12905-016-0361-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-016-0361-z