Abstract
Background
There is growing recognition of the difficult reproductive decisions faced by HIV-positive women. Studies in both resource-constrained and developed countries have suggested that many HIV-positive women continue to desire children in spite of their understanding of the possible risks that HIV poses. This study investigates the factors associated with fertility desire among HIV-positive women in Tigray region, Ethiopia.
Methods
A cross-sectional survey was conducted among 964 HIV-positive women receiving HIV care in 12 health centers of Tigray region. In each health center, the number of study participants was allocated proportionally to the load of HIV-positive women in the chronic care clinics. A descriptive summary of the data and a logistic regression model were used to identify factors associated with fertility desire using odds ratios with a 95% confidence interval and P-value of 0.05.
Results
Four hundred and thirty nine (45.5%) of the participants reported a desire to have children in the future. Eighty six percent of the women had given birth to at least one live baby at the time of study, with the median number of live births being 2 (Inter quartile range = 1,3). Women in the age group of 15-24 years [AOR = 2.64(95% CI: 1.44, 4.83)] and 25-34 years [AOR = 2.37 (95% CI: 1.60, 2.4 3.50)] had higher fertility desire as compared to women in the age group of 35-49 years. Having no children [AOR = 25.76 (95% CI: 13.66, 48.56)], having one to two children [AOR = 5.14 (95% CI: 3.37, 7.84)] and disclosing HIV status to husband/sexual partner [AOR = 1.74 (95% CI: 1.11, 2.72)] were all independently associated with fertility desire.
Conclusions
Age, HIV disclosure status to husband/sexual partner, and relatively few live children were all found to influence HIV-positive women’s fertility desire. Programmers and policy makers should consider the effects of these factors for HIV-positive women as they develop HIV/AIDS interventions.
Similar content being viewed by others
Background
Globally, studies estimate that 75% of all HIV-positive people are of reproductive age. Sub-Saharan Africa is home to60% of all people living with HIV/AIDS, and more than half of these are females [1]. In Ethiopia, for example, the prevalence of HIV/AIDS among women of reproductive age (1.9%) is higher than men (1.0%) in the same age [2]. Thus, interventions to meet the reproductive health needs, and specifically the needs relating to a desire to have children of this population group need to be prioritized as many HIV-positive women continue to want to have babies despite knowledge of their HIV status [3]-[7].
Evidence indicates that HIV-positive women continue to desire more children in the future, though to differing degrees in different contexts. In two studies conducted in Canada and Malawi, for example, the proportions of HIV-positive women who wanted to have children in the future were 69% and 17%, respectively [4],[5]. In Ethiopia, different studies have indicated different levels of fertility desire among HIV-positive women. A study in North Wollo, Ethiopia, demonstrated that 15.7% of HIV-positive women had fertility desire [8]. By contrast, 44% of HIV-positive women in Addis Ababa wanted more children [6], as compared to 53% of women in Harari region [7], and 92% of women in Oromia region, Ethiopia [3]. Studies in a number of settings have pointed to different factors which determine the fertility desire of HIV-positive women. For example, young age of HIV-infected individuals is significantly associated with increased fertility desire [4],[9]-[13]. Decreased fertility desire is associated with divorce or separation, as well as having at least one child [4],[12]-[14]. HIV disclosure to a woman’s sexual partner has also been associated with her having increased fertility desire [11],[14]. Sero-discordance could also affect fertility desire of couples [15]. A further study indicated that educational status was not significantly associated with fertility desire among HIV-positive women [13], while good perceived health status, and CD4 count more than or equal to 200 cells/mm3 were found to be significantly associated with increased fertility desire [14],[16].
Evidence about the association between Antiretroviral Therapy (ART) use and fertility desire is mixed, however, with some studies indicating that there is no association between the two [8],[13],[14],[16],[17], and others suggesting that commencement of ART was one of the reasons for women’s increased fertility desire, due to an improved quality of life [6],[10].
In Ethiopia, a number of studies have been conducted to investigate fertility desire of people living with HIV/AIDS [3],[6]-[8],[15],[18],[19]. However, none of these studies has been conducted on a large scale, incorporating a number of health facilities covering large demographic areas with socio-cultural diversity. The present study addresses this gap in the knowledge base by incorporating a number of health facilities covering all zones of the region, and with a large sample size.
The main aim of this study is to assess the extent of, and the factors associated with fertility desire among HIV-positive women in Tigray region, Ethiopia. This is necessary in order to help stakeholders engaged in Sexual and Reproductive Health programs and policies, such as regional health bureaus and non-governmental organizations working on HIV/AIDS and family planning, to make evidence-based decisions about the interventions they are running. Specifically, it is important to ensure that the necessary resources and programs for improved reproductive health services, such as Prevention of Mother-to-Child Transmission (PMTCT) of HIV and family planning services for HIV-positive women, are in place, and that they are as integrated into AIDS care services as current Regional health policy requires them to be. It is hoped that this will lead to a better quality of life for HIV-positive women, decrease levels of vertical HIV transmission to children, and ultimately reduce maternal and child mortality.
Methods
Study setting and design
Tigray region has an estimated total population of just over 4.6 million, of whom 50.7% are female. More than 80% of the population lives in rural areas of the region [20]. In 2012, Tigray had 14 hospitals, 220 health centers and 671 health posts [21].
The 2011 Ethiopian Demographic and Health Survey (EDHS) estimated that overall HIV adult prevalence (15-49 years) in Tigray was 1.8% (2.2% for women and 1.3% for men) [2]. HIV prevalence in Tigray varies considerably across zones, from 0.4% (Central zone) to 2.2% (Western zone) [22].
In 2013, there were 60 health centers in Tigray region which were supported by the Ethiopian Network of HIV/AIDS Treatment, Care and Support (ENHAT-CS). Each of these health centers provided a number of free services, including Voluntary HIV Counseling and Testing (VCT), HIV treatment and care (including ART and PMTCT), and family planning.
This study was conducted at chronic follow-up care clinics (providing both pre-ART support and ART) in 12 ENHAT-CS supported health centers in Tigray region from May to June 2013. The study area is also described elsewhere [23].
The analysis is based on cross-sectional survey data collected from HIV-positive women (including those who are on ART and those who have not yet started treatment) receiving services at ENHAT-CS supported health centers in the region. A medical chart review was also conducted to confirm HIV serology, ART history, and other medical characteristics of the women.
Eligibility criteria
To be eligible to participate in the study, women were required to be 15-49 years of age, attending a chronic follow-up care ENHAT-CS-supported center, competent to give informed consent, and willing to allow medical record review for the purposes of confirming HIV sero-status and other aspects of their medical history. We considered women to be ART users if they were taking ART at the time of interview. We considered women to be pre-ART (not using ART) if they were not taking ART at the time of survey, or if they were taking ART purely for prophylactic purposes within the context of PMTCT.
Sample selection
Twenty percent of ENHAT-CS supported health centers in Tigray region were selected with a simple random sampling technique. Around 20% of the health centers in each administrative zone with Tigray (there are 6 zones in the Region) were selected based on the total number of ENHAT-CS supported health centers in each zone. The numbers of study participants in each health center were determined using proportion to population size (HIV-positive women registered in the health centers). To select woman to participate in each health center, a systematic random sampling technique was used. In each health center, every fourth eligible woman was invited to join the study (Figure 1).
Data collection procedures and tools
After confirming eligibility and obtaining written informed consent, randomly selected participants were asked to complete a 25-35 minute, interviewer-administered questionnaire in the local Tigrenga language.
The questionnaire assessed socio-demographic characteristics, fertility desire, fertility, and sexual history. Questions were adapted from previously conducted studies [4],[24]-[27]. Medical records of HIV-positive women were reviewed to confirm HIV status and other relevant medical history, including date of HIV diagnosis, current WHO stage of disease, most recent CD4 count, ART status, as well as date of ART start, type of ART drugs and other medications/prophylaxis.
Measures and operational definitions
The explanatory variables included current ART status, age, education, employment, current sexual partnership, number of living children, and HIV-related clinical outcomes. We define HIV-positive women receiving chronic care as women who had engaged in care at least once to the selected pre-ART or ART units, whether they were receiving ART or not.
The primary outcome was self-reported fertility desire at the time of the survey. Based on previous similar studies [5],[27], the fertility desire variable was investigated using the question “Would you like to have children in the future?”, and, the variable was dichotomized into “had no desire” if a woman answered “No”, and “had fertility desire” if she answered “Yes”. If the answer was “Yes”, the respondent was asked “How many children would you like to give birth to in the future?”.
Data quality control, management and analysis
The data were entered into an Epidata version 3.1 database and transferred to STATA version 11.1 (Stata Corporation, College Station, TX, USA) statistical package for analysis.
A pretest of the questionnaire was conducted in two health facilities which had similar services to the selected study health centers. Supervisors checked each completed questionnaire and the data extraction tool (which collected the clinical data listed above) for consistency, completeness and accuracy. Support supervision was also provided by the investigators for data collectors and supervisors.
Frequencies, proportions and summary statistics were used to describe the study population in relation to relevant variables. Person’s χ 2, trend χ 2 and Fisher’s exact test were used to estimate crude differences among women by different backgrounds in terms of fertility desire. Both bivariate and multivariate logistic regression models were used to identify significant factors associated with fertility desire. The degree of association between independent and dependent variables was assessed using odds ratios with a 95% confidence interval. After testing for co-linearity [28] and interaction [29], all covariates with statistically significant associations in the bivariate analysis were included in multivariate logistic regression model to obtain adjusted estimates of the association between covariates and fertility desire. All statistical tests were two-sided and considered statistically significant at P-value of 0.05.
Ethics statement
Ethical clearance was obtained from the Institutional Review Board of Mekelle University, College of Health Sciences. Permission letters were gained from Tigray regional Health Bureau, respective district health offices, and the in-charges of the participating health centers. After explaining the objective and contents of the study, written consent was obtained from each respondent, or from the adult next-of-kin when the respondent was under 18 years of age. The information collected was purely used for research works and all respondents have remained anonymous.
Results
Socio demographic, clinical and fertility characteristics of the study participants
All 964 eligible study participants gave responses during the interview, and allowed their medical records to be reviewed - this gave a response rate of 100%. The median age was 30 years (Inter Quartile Range (IQR) = 27, 36). More than two-thirds (68.8%) of the participants were from urban areas. A large majority, 92.6% and 91.8%, of the participants were ethnic “Tigrie” and orthodox Christians, respectively. Three-fifths (59.1%) of the women were illiterate. Housewives, daily laborers and farmers collectively accounted for more than three-fifths (20.1%, 21.7% and 20.2%, respectively) of all the occupations of the study participants. Exactly two-fifths (40%) of the participants were married at the time of survey. More than 69% and 57%, respectively, of the participants had no functional television and radio in their house (Table 1).
The level of HIV disclosure among the women was high, with 822 (85.3%) reporting they had informed at least one person of their HIV-positive status. However, almost half of these women, 414 (49.1%), had not disclosed to their husband/sexual partner. A large majority, 897 (93.1%), of the women reported that their health status was improving. Of these, 789 (88%) were on ART. In all, 822 (85.3%) of the women were on ART at the time of survey (Table 1).
More than half of the women, 558 (57.9%), were in WHO clinical stage I, and more than four-fifths of them, 767 (82.5%), had greater than or equal to 200 cells/mm3 CD4 count in their latest laboratory result. Of those who were married or partnered at the time of survey, 92(19.9%) did not know their husband’s/partner’s HIV status. Nearly four-fifths, 286 (77%), of the women who knew their partner’s/husband’s HIV status, reported that he is HIV-positive. The majority, 508 (52.7%), of women had one or two living children with the median number of children being 2 (IQR = 1, 3) (Table 1).
Fertility desire was crudely associated with age and women’s education status (P < 0.0001). There was also association between marital status and women’s fertility desire (P < 0.0001). Associations were detected between fertility desire of women and the presence of television and radio. Disclosure of HIV status and total number of living children a mother had were found to be significantly associated with fertility desire (P < 0.0001) (Table 1).
Thirty nine (3.5%) of the women reported that they were pregnant, and of these, five (14.7%) said that their pregnancy was unplanned and unwanted. Four hundred thirty nine (45.5%) of all the HIV-positive women expressed a desire to have more children in the future. Of the women who did not desire to have children and who were sexually active at the time of the survey (n = 453), 182 (40.2%) were not using any contraceptive methods.
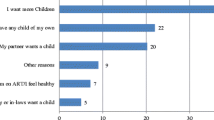
Half (49.7%) of the women who did not report any desire to have children (n = 525; 54.5%) reported that this was because they did not have enough income to support more children. The other reasons given were the presence of enough children (44.2%), fear of further deterioration of health (24.2%), fear of transmission of HIV to the child (14.1%), and advice from health professionals (6.7%). Partner objection (0.8%) and other reasons (5.3%) were also mentioned.
Factors associated with fertility desire
Of all the variables modeled in a bivariate logistic regression, marital status, age, education level, occupation, presence of functional television and radio, total number of living children, HIV status disclosure to husband/sexual partner, perceived health status, and being on Cotrimoxazole prophylaxis or non-ART medication were found to be significantly associated with fertility desire at P-value of 0.05% (Table 2).
In a multivariate analysis, women in the age groups of 15-24 and 25-34 years had 2.6 [AOR = 2.64 (95% CI: 1.44, 4.83)] and 2.4 [AOR = 2.37 (95% CI: 1.60, 3.50)] higher odds of fertility desire compared to women in the age group of 35-49 years, respectively. Women who has disclosed their HIV status had almost two times [AOR = 1.74 (95% CI: 1.11, 2.72)] higher odds of fertility desire compared to women who had not. Women who had no children had 26 times [AOR = 25.76 (95% CI: 13.66, 48.56)] higher odds of desiring children as compared to women who already had three or more children; and women who already had one or two children had five times [AOR = 5.14 (95% CI: 3.37, 7.84)] higher odds of desiring more children (Table 2).
Discussion
In this study, 45% of the HIV-positive women we surveyed desired to have children in the future. This finding is lower than findings from similar studies in Swaziland, 60% [24]; Uganda, 59% [9] and 72% [30]; and Canada, 69% [4]; while it is higher than the figures derived from studies conducted in Tanzania, 36% [14]; Uganda, 10% [12], 19% [31], and 29% [11] and Malawi, 17% [5]. In Ethiopia, various studies have reported different level of fertility desire. A similar level was reported in Addis Ababa (44%) [6]; a lower level was reported in Northern Ethiopia (24%) [18] and South Wollo (15.7%) [8]. Higher rate of fertility intention (92.3%) was also reported in Oromia region [3]. A study in Harari region indicated that 52.9% of women had fertility desire [7]. The reasons for these differences are not clear, but they are likely to be the products of specific socio-cultural and/or economic factors - or the differential expressions of these - in each setting.
Our findings indicated that ART use was not significantly associated with fertility desire, and neither was CD4 count, even though both of these would have led to or indicated improved health. These findings were consistent with studies (including a meta-analysis) conducted in Tanzania, Ethiopia, Malawi [8],[13],[14],[16],[17]. The important issue, therefore, may not have been the women’s clinical status, but rather, perhaps, their socio-demographic characteristics and fertility history.
Other studies have found the factors predicting fertility desire to include, for example, the desire to have children of both sexes, the desire for a large family, pressure from family or partner to have children [32], and a child being thought of as a prerequisite for a fulfilled and happy life [33]. The most important factors predicting fertility desire in our study population, by contrast, included age, disclosing HIV status to husband/sexual partner, and having no or few living children.
After adjusting for other variables, we found that age of women was significantly associated with fertility desire. Women of younger age had higher odds fertility desire compared to older women. This finding is similar from those of a methodologically diverse series of studies from Uganda and Canada, which indicate that young, HIV-infected women experience significantly more fertility desire than HIV-infected, older women [4],[9]-[12]. In Ethiopia, some studies demonstrated the presence of an association between age and fertility desire [6],[7], while another study reported that such an association was not present [8].
In the current study, women who disclosed their HIV status to their husband/sexual partner had higher odds of having fertility desire. HIV disclosure to a woman’s sexual partner has also been associated with her having increased fertility desire [11],[14]. A study in Ethiopia has reported the same finding [8], probably because communication between partners may play an important role in pre-conception planning behaviors [34]. Additionally, it is important to understand the positive impact of communication on partner participation in PMTCT programmes [35],[36]. Thus, interventions to promote the reproductive health of HIV-positive women in Ethiopia should continue to promote positive couple communication about HIV status.
Our finding that women who had no children, or who had one or two children, were much more likely to desire babies than women who had more than two children, was also expected: similar findings have been reported in a number of different countries [4],[12]-[14],[17],[37], including in Ethiopia [6],[7],[16],[19]. This could be that in some communities, such as Ethiopia, a child is thought of as a prerequisite for a fulfilled and happy life [33].In some African communities, satisfying desired family size, desire for biological children, maintaining stability of the union, and socio-cultural pressures were important reasons for continuing fertility desire among HIV-positive women [38].
An important finding of our study was that slightly more than half of these HIV-positive women reported that they did not want to have children in the future. Several reasons were given for this, with two of the most important being insufficient financial security and a fear of further deterioration in their health [10]. In other words, these women may have wanted children had their financial and health circumstances been better, a finding which may also be reflected in the wider HIV-negative female population in the region. Counseling on safer contraceptive methods for these women will have important reproductive health implications.
The current study found that 40.2% of HIV-positive women had an unmet need for contraceptives. This represents a potentially serious public health problem. It is essential that the contraceptive needs of these women are met, so that they may avoid the anxieties and possible health risks associated with an unwanted pregnancy. The health workers providing their chronic AIDS care must be made aware of this, and a range of contraceptive options should be made available, as well as all the associated information about these options.
Study limitations
It is important to note some limitations of this study. First, men were not included in the study, in spite of the essential role they can play in deciding about the size of their family. Second, health service providers, whose attitudes and perceptions could have a direct or indirect influence on fertility desire in this population, were not also included. Structural components of the health system and service provision quality would also be important considerations in future studies on this topic.
This study is also limited to women who are receiving chronic, long term care for their HIV infection. Fertility desire among these women could be very different from women who are not receiving such care. In addition, small numbers of HIV-positive women who are not ART users were not specifically powered to detect differences in terms of their fertility desire. Lack of comparison to HIV-negative women may also be seen as a limitation.
Conclusions
This study has identified two discrete groups of HIV-positive women in Tigray region, Ethiopia, with very clear and differing requirements from the health services. One of these groups, constituting 45% of the 964 women surveyed, report that they want to have children in the future; while the other group, made up of the remaining 55% of the women, say that they do not want to have children. The factors associated with fertility desire in the former group included being young, having no children, and disclosing HIV status to their husband/sexual partner; while the primary reasons for the women in the latter group not wanting to have children were insufficient financial security, having `enough’ children already, and a fear of deteriorating health.
These findings have important implications for sexual and reproductive health policy and practice in Tigray. Tigray regional SRH policy stipulates that services should be fully integrated into existing HIV/ART care and it is important that this integration is maintained and strengthened in practice. This strengthening could include ensuring that health workers are well informed about the possible effect of the factors identified in this study that are associated with HIV-positive women’s desire either to have children or not. Full information about the possible risks of having a baby should be provided to all HIV-positive women, but in a way that protects their reproductive rights, and ensures that any decision to conceive is supported all the way through the pregnancy, birth, and post-natal period. Meanwhile, for those HIV-positive women who do not desire to have children, a range of family planning method options should be made accessible from all HIV/AIDS care units.
Further research on this topic should include qualitative studies that would provide a deeper understanding of HIV-positive women’s fertility desires. One important aspect of this would be the possible role of health care workers in ensuring that the rights of HIV-positive women are protected, and that their desires and decisions to have children, or not to have children, are supported. In addition, further studies should consider including a comparison with HIV-negative women.
References
AIDS Epidemic update. In united nation joint programme on HIV/AIDS. 2011, WHO/UNAIDS, Geneva, Switzerland
Central Statistical Agency [Ethiopia] and ORC Macro: Ethiopia Demographic and Health Survey 2011.Addis Ababa, Ethiopia and Calverton, Maryland, USA, 2012
Bonnenfant YT, Hindin MJ, Gillespie D: HIV diagnosis and fertility intentions among couple VCT clients in Ethiopia. AIDS Care. 2012, 24 (11): 1407-1415. 10.1080/09540121.2011.650679.
Loufy MR, Hart TA, Mohammed SS, Su D, Ralph ED, Loufy MR, Hart TA, Mohammed SS, Su D, Ralph ED, Walmsley SL, Soje LC, Muchenje M, Rachlis AR, Smaill FM, Angel JB, Raboud JM, Silverman MS, Tharao WE, Gough K, Yudin MH: Fertility desires and intentions of HIV-positive women of reproductive age in Ontario, Canada: a cross-sectional study. PLoS One. 2009, 4 (12): e7925-10.1371/journal.pone.0007925.
Dube ALN, Baschieri A, Cleland J, Floyd S, Molesworth A, Parrott F, French N, Glynn JR: Fertility intentions and use of contraception among monogamous couples in Northern Malawi in the context of HIV testing: a cross-sectional analysis. PLoS One. 2012, 7 (12): e51861-10.1371/journal.pone.0051861. doi:10.1371/journal.pone.0051861
Asfaw HM, Gashe FE: Fertility intentions among HIV-positive women aged 18-49 years in Addis Ababa Ethiopia: a cross sectional study. Reprod Health. 2014, 11: 36-10.1186/1742-4755-11-36.
Haile F, Isahak N, Dessie A: Fertility desire and associated factors among people living with HIV on ART, in Harari Regional State, Eastern Ethiopia. J Trop Dis. 2014, 2: 3.
Getachew M, Alemseged F, Abera M, Deribew A: Factors affecting fertility decisions of married men and women living with HIV in South Wollo Zone, Northeast Ethiopia. Ethiop J Health Dev. 2010, 24 (3): 214-220.
Beyeza-Kashesya J, Ekstrom MA, Kaharuza F, Mirembe F, Neema S, Kulane A: My partner wants a child: a cross-sectional study of the determinants of the desire for children among mutually disclosed sero-discordant couples receiving care in Uganda. BMC Public Health. 2010, 10: 247-10.1186/1471-2458-10-247.
King R, Khana K, Nakayiw S, Katuntu D, Homsy J, Lindkvist P, Johansson E, Bunnell R: Pregnancy comes accidentally - like it did with me-: reproductive decisions among women on ART and their partners in rural Uganda. BMC Public Health. 2011, 11: 530-10.1186/1471-2458-11-530.
Kakaire O, Osinde OM, Kaye KD: Factors that predict fertility desires for people living with HIV infection at a support and treatment centre in Kabale, Uganda. Reprod Health. 2010, 7: 27-10.1186/1742-4755-7-27.
Kipp W, Heys J, Jhangri GS, Alibhai A, Rubaale T: Impact of antiretroviral therapy on fertility desires among HIV-infected persons in rural Uganda. Reprod Health. 2011, 8: 27-10.1186/1742-4755-8-27.
Berhan Y, Berhan A: Meta-analyses of fertility desires of people living with HIV. BMC Public Health. 2013, 13: 409-10.1186/1471-2458-13-409.
Mmbaga EJ, Leyna GH, Ezekiel MJ, Kakoko DC: Fertility desire and intention of people living with HIV/AIDS in Tanzania: a call for restructuring care and treatment services. BMC Public Health. 2013, 13: 86-10.1186/1471-2458-13-86.
Hailemariam TG, Kassie GM, Sisay MM: Sexual life and fertility desire in long-term HIV serodiscordant couples in Addis Ababa, Ethiopia: a grounded theory study. BMC Public Health. 2012, 12: 900-10.1186/1471-2458-12-900.
Negash S, Yusuf L, Tefera M: Fertility desires predictors among people living with HIV/AIDS at art care centers of two teaching hospitals in Addis Ababa. Ethiop Med J. 2013, 51 (1): 1-11.
Kawale P, Mindry D, Stramotas S, Chilikoh P, Phoya A, Henry K, Elashoff D, Jansen P, Hoffman R: Factors associated with desire for children among HIV-infected women and men: A quantitative and qualitative analysis from Malawi and implications for the delivery of safer conception counseling. AIDS Care. 2014, 26 (6): 769-776. 10.1080/09540121.2013.855294. http://dx.doi.org/10.1080/09540121.2013.855294
Alemayehu B, Aregay A: Desire to procreate among people living with HIV/AIDS: Determinants in Ethiopia: a cross-sectional study. J AIDS HIV Res. 2012, 4 (5): 128-135. 10.5897/JAHR11.042.
Tesfaye L, Admasu M, Getachew A, Sharma HR: Fertility desires and family planning demand among HIV-positive clients in follow-up care at antiretroviral treatment unit in Gondar University hospital, Ethiopia. Vulnerable Child Youth Stud. 2012, 7 (1): 20-35. 10.1080/09540121.2011.647114.
Ethiopian Central Statistics Agency, Central Statistical Agency [Ethiopia]: Ethiopia Census report 2007. Addis Ababa, Ethiopia; 2007.
Tigray Health Bureau: Tigray Health Profile 2010. Mekelle: Tigray Health Bureau, Tigray, Ethiopia; 2012.
USAID, Tigray Health Bureau: Tigray Regional State Synthesis of the HIV Epidemic and Response p3-4. 2012.
Melaku YA, Zeleke EG: Contraceptive Utilization and Associated Factors among HIV-positive Women on Chronic Follow Up Care in Tigray Region, Northern Ethiopia: A Cross Sectional Study. PLoS One. 2014, 9 (4): e94682-10.1371/journal.pone.0094682. doi:10.1371/journal.pone.0094682
Warren EC, Abuya T, Askew I: Family planning practices and pregnancy intentions among HIV-positive and HIV-negative postpartum women in Swaziland: a cross sectional survey. BMC Pregnancy Childbirth. 2013, 13: 150-10.1186/1471-2393-13-150.
Kaida A, Gray G, Bastos FI, Andia I, Maier M, Kaida A, Gray G, Bastos FI, Andia I, Maier M, McIntyre J, Grinsztejn B, Strathdee SA, Bangsberg DR, Hogg R: The relationship between HAART use and sexual activity among HIV-positive women of reproductive age in Brazil, South Africa, and Uganda. AIDS Care. 2008, 20: 21-25. 10.1080/09540120701426540.
Kaida A, Laher F, Strathdee SA, Money D, Janssen PA, Hogg RS, Glenda Gray G: Contraceptive use and method preference among women in Soweto, South Africa: the influence of expanding access to HIV care and treatment services. PLoS ONE. 2010, 5: 11-10.1371/journal.pone.0013868. e13868. doi:10.1371/journal.pone.0013868
Ogilvie GS, Palepu A, Remple VP, Maan E, Health K, MacDonald G, Christilaw J, Berkowitz J, Fisher WA, Burdge DR: Fertility intentions of women of reproductive age living with HIV in British Columbia, Canada. AIDS. 2007, 21: S83-S88. 10.1097/01.aids.0000255090.51921.60.
Pagano M, Gauvreau K: Principles of biostatistics. 2000, Duxbury, Pacific Grove, CA, 2
Van Ness PH, Allore HG: Using SAS to investigate effect modification. Paper 105-31. SUGI 31. 2007
Beyeza-Kashesya J, Kaharuza F, Ekström AM, Neema S, Kulane A, Mirembe F: To use or not to use a condom: a prospective cohort study comparing contraceptive practices among HIV-infected and HIV-negative youth in Uganda. BMC Infect Dis. 2011, 11: 144-10.1186/1471-2334-11-144.
Wanyenze RK, Tumwesigye NM, Kindyomunda R, Beyeza-Kashesya J, Atuyambe L, Kansiime A, Neema S, Ssali F, Akol Z, Mirembe F: Uptake of family planning methods and unplanned pregnancies among HIV-infected individuals: a cross sectional survey among clients at HIV clinics in Uganda. J Int AIDS Soc. 2011, 14: 35-10.1186/1758-2652-14-35.
Wanyenze RK, Wagner JG, Tumwesigye NM, Nannyonga M, Wabwire-Mangen F, Kamya MR: Fertility and contraceptive decision making and support for HIV infected individuals: client and provider experiences and perceptions at two HIV clinics in Uganda. BMC Public Health. 2013, 13: 98-10.1186/1471-2458-13-98.
Ujiji AO, Ekstrom MA, Ilako F, Indalo D, Rubenson B: I will not let my HIV status stand in the way. Decisions on motherhood among women on ART in a slum in Kenya- a qualitative study. BMC Womens Health. 2010, 10: 13-10.1186/1472-6874-10-13.
Stern E, Buikema R: The relational dynamics of hegemonic masculinity among South African men and women in the context of HIV. Culture, Health & Sexuality. 2013, 15 (9): 1040-1054. 10.1080/13691058.2013.805817.
Orne-Gliemann J, Tchendjou PT, Miric M, Gadgil M, Butsashvili M, Eboko F, Perez-Then E, Darak S, Kulkarni S, Kamkamidze G, Balestre E, du Loû AD, Dabis F: Couple-oriented prenatal HIV counseling for HIV primary prevention: an acceptability study. BMC Public Health. 2010, 10 (1): 197-10.1186/1471-2458-10-197.
Villar-Loubet OM, Bruscantini L, Shikwane ME, Weiss S, Peltzer K, Jones DL: HIV disclosure, sexual negotiation and male involvement in prevention-of-mother-to-child transmission in South Africa. Cult Health Sex. 2013, 15 (3): 253-268. 10.1080/13691058.2012.716166.
Tamene W, Fantahun M: Fertility desire and family-planning demand among HIV-positive women and men undergoing antiretroviral treatment in Addis Ababa. Afr J AIDS Res. 2007, 6 (3): 223-227. 10.2989/16085900709490418.
Ngure K, Baeten JM, Mugo K, Curran K, Vusha S, Heffron R, Celum C, Shell-Duncan B: My intention was a child but I was very afraid: fertility intentions and HIV risk perceptions among HIV sero-discordant couples experiencing pregnancy in Kenya. AIDS Care. 2014, 26 (10): 1283-1287. 10.1080/09540121.2014.911808. http://dx.doi.org/10.1080/09540121.2014.911808
Acknowledgements
The study was financially supported by the United States Agency for International Development (USAID) through Management Science for Health (MSH) for which the investigators are grateful. The authors also want to express their gratitude for Mekelle University, Tigray regional Health Bureau, study participants, data collectors and supervisors.
Funding
The study was funded by the United States Agency for International Development (USAID) under cooperative agreement No. AID-663-A-11-00006.
Disclaimer
This study is made possible by the generous support of the United States Agency for International Development (USAID) under cooperative agreement No. AID-663-A-11-00006. The contents are the responsibility of the authors and do not necessarily reflect the views of USAID or the United States Government.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
YAM was involved in designing the study, data collection, supervision, data processing, cleaning, analysis and interpretation of the results, as well as drafting the manuscript. EGZ was involved in designing of the study and reviewing the manuscript. JK participated in drafting, reviewing and commenting on the manuscript. AKA has reviewed the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Melaku, Y.A., Zeleke, E.G., Kinsman, J. et al. Fertility desire among HIV-positive women in Tigray region, Ethiopia: implications for the provision of reproductive health and prevention of mother-to-child HIV transmission services. BMC Women's Health 14, 137 (2014). https://doi.org/10.1186/s12905-014-0137-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-014-0137-2