Abstract
Background
Several studies have demonstrated the benefits of early initiation of end-of-life care, particularly homecare nursing services. However, there is little research on variations in the timing of when end-of-life homecare nursing is initiated and no established benchmarks.
Methods
This is a retrospective cohort study of patients with a cancer-confirmed cause of death between 2004 and 2009, from three Canadian provinces (British Columbia, Nova Scotia, and Ontario). We linked multiple administrative health databases within each province to examine homecare use in the last 6 months of life. Our primary outcome was mean time (in days) to first end-of-life homecare nursing visit, starting from 6 months before death, by region. We developed an empiric benchmark for this outcome using a funnel plot, controlling for region size.
Results
Of the 28 regions, large variations in the outcome were observed, with the longest mean time (97 days) being two-fold longer than the shortest (55 days). On average, British Columbia and Nova Scotia had the first and second shortest mean times, respectively. The province of Ontario consistently had longer mean times. The empiric benchmark mean based on best-performing regions was 57 mean days.
Conclusions
Significant variation exists for the time to initiation of end-of-life homecare nursing across regions. Understanding regional variation and developing an empiric benchmark for homecare nursing can support health system planners to set achievable targets for earlier initiation of end-of-life care.
Similar content being viewed by others
Background
Providing end-of-life care in the home is an important policy issue because it can support many patients’ preferences to die at home [1, 2], and has the potential for cost-savings by avoided hospitalizations [3,4,5]. In particular, homecare nursing is critical at end-of-life since it provides complex symptom management, education, and support, which can then help to avoid often unnecessary and expensive hospitalizations. Yet policymakers have little information or quality benchmarks about the delivery of end-of-life homecare nursing.
Research has shown that the use and intensity of end-of-life homecare nursing is strongly associated with a home death [6], and reduced hospitalizations near death [7]. Moreover, several studies have demonstrated that early initiation of palliative and end-of-life care in cancer patients has benefits, such as reduced symptoms, improved quality of life, and even longer survival [8,9,10]. Earlier initiation and more intensity of end-of-life homecare nursing specifically, has also been associated with reduced hospitalizations and hospital deaths [7, 11, 12]. Yet despite the growing evidence of the benefits of early initiation of end-of-life care by homecare nurses, little research describes the timing in when such care is initiated. This hinders health system planners from understanding regional variation in end-of-life home care access. Furthermore, there are no established benchmarks to compare or target against.
The purpose of this study is three-fold: i) to describe the regional variation in the mean time to first end-of-life homecare visit starting from 6 months before death among health regions across British Columbia (BC), Nova Scotia (NS), and Ontario (ON); ii) establish the three-province average with confidence limits for this outcome; and iii) determine a national empiric benchmark based on the best regional performers. Ultimately these data can be used by Canadian policy makers to set achievable targets and improve end-of-life home care access. The methods can be applied by other countries to determine their own benchmarks.
Methods
Study design
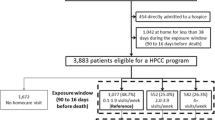
We conducted a retrospective cohort study of cancer decedents who received homecare nursing in the Canadian provinces of ON, NS and BC, which contain a total of 28 health regions. Our inclusion criteria were adult decedents (19 years or older) with a valid provincial health insurance number, who had at least one record of homecare nursing following their cancer diagnosis and within 6 months of their date of death during the study period between April 1, 2004 and March 31, 2009. Due to a time lag in capturing cancer-confirmed cause of death in cancer registries, these were the most recent data available at the time of study inception.
Data sources
To derive our cohort, we used a unique encrypted patient identifier within each province to link with multiple administrative databases. Starting with a provincial cancer registry for cancer type, cancer diagnosis, and confirmed cause of death from cancer, we then linked with the: provincial homecare database for homecare nursing use with standard or end-of-life intent; Canadian Institute for Health Information’s Discharge Abstract Database for Charlson-Deyo score for comorbidity; and the provincial health insurance databases for demographics of age at death, sex, and postal code for both region and income quintile [13,14,15,16]. Individual level data were not merged across provinces.
Outcome
Our main outcome was mean number of days to first end-of-life homecare nursing visit, starting from 6 months (182 days) before death. Homecare nursing intent is recorded in each provincial homecare database. Standard intent nursing is provided to patients with service goals ranging from providing “short-term care” with a predictable recovery (e.g., wound care) to “preserving the client’s level of function and autonomy” with a prognosis of very gradual decline (e.g., early onset of frailty) [17]. Whereas end-of-life nursing intent is provided to patients classified as “not responsive to curative treatment and are dying,” with service goals being “to alleviate distressing symptoms to achieve the best quality of life by providing complex support in the last stages of their illness,” and a typical prognosis of an “expected death within six months” [17]. Given this standardized homecare eligibility criteria, we aligned our outcome definition to start from 6 months from death; thus, a shorter mean time would represent earlier initiation, and the outcome has a maximum of 182 days representing death date. At each week, the number of patients receiving standard or end-of-life homecare nursing was identified. After first end-of-life homecare nursing visit, all subsequent nursing visits were considered end-of-life. Nursing visits were measured as time (hours/day) in ON, as nursing visits received in BC, and as authorized in NS over a month.
Statistical analyses
Through the use of descriptive statistics, baseline characteristics of each population under study were compared by province. The outcome was compared across health regions through the use of a bar chart graph and a X2 test with P < .05 considered as statistically significant. The benchmark mean for the outcome of interest was determined using the pared-mean method, which derives benchmarks from the top decile of performers [18]. Five criteria are included for this method of benchmark development: 1) the level of the benchmark signifies excellence, that is, it is always better than the mean; 2) the benchmark is achievable and realistic; 3) high performers should be selected from all performers in a pre-defined way; 4) all high performers should contribute to the benchmark; and 5) high performers with a low number of cases should not excessively impact the benchmark level (but should contribute).
In order to construct benchmark levels, health regions were first ranked according to descending order of performance. Starting with the best performing health region (i.e. shortest mean time), the eligible population sizes in each region were summed sequentially until the combined population size of this subset of regions was at least 10% of the combined size of all health regions. Combining the number of patients from these best-performing regions, the benchmark mean was calculated as the weighted average of the mean time to initiation of end-of-life nursing among the best performing regions.
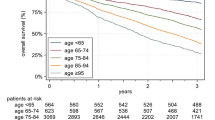
A funnel plot was created for the outcome, controlling for age and sex. The funnel plot displays the number that received end-of-life homecare in each region on the horizontal axis and the corresponding mean days to initiation of end-of-life homecare nursing on the vertical axis (as seen by the dots). This funnel plot also illustrates the overall mean of the outcome across all regions (as seen by the thick black line) and the expected 95% and 99.8% CIs (as seen by the curved black lines) calculated based on normal distribution control limits [19]. The benchmark mean calculated above was overlaid on the funnel plot, as indicated by the red line. Statistical analyses were performed using SAS 9.3 (SAS Institute, Cary, North Carolina, USA), R 3.0.1, and Microsoft Excel 2010.
Results
The study identified 85,339 cancer decedents who used any homecare nursing in the last 6 months of life, of which 61,903 of those used end-of-life care nursing (73%) to form our final cohort: 28% were from BC, 65% from ON, and 7% from NS. Table 1 shows the size and demographic information for the 28 regions examined in the three provinces. The average age was 71 years old, 48% were female, and approximately 20% had a comorbidity other than cancer.
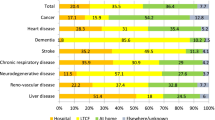
Figure 1 displays the unadjusted mean number of days to initial end-of-life homecare visit (starting from 6 months before death) by the 28 regions, color-coded by province (shorter number of days to initiation equates to earlier access to end-of-life care). Large regional variations were observed. The longest mean time, 97 days, (ON- Mississauga Halton) is nearly twice as long as the shortest, 55 days (BC- Vancouver Coastal, and NS- South West). The majority of ON regions have the longest mean time to initial visit. BC and NS had the first and second shortest times, respectively.
Figure 2 displays a funnel plot for the mean days to initial end-of-life homecare nursing visit, from 6 months before death, across the 28 regions controlling for age, sex, and region size. The funnel plot includes the following information: 1) the overall mean (straight black line), 2) the expected 95% Confidence Intervals (narrows as the number that received end-of-life care in each region increases), 3) the benchmark mean (straight red line), and 4) the mean of each region (dots, color-coded according to province). The overall three-province outcome average was 76 days after the six-month point (i.e. 106 days or 3.5 months before death). The empiric benchmark value based on best-performing regions was 57 days after the six-month point (i.e. 125 days or 4.2 months before death). The best-performing regions belong to BC and NS. Most regions of ON are worse than the benchmark and overall mean. This contrasts with most regions of NS and BC, which are better than the overall mean. Regions with both small and large population sizes performed worse than the benchmark and worse than the overall indicator mean. Similarly, there were large and small regions at or near the benchmark.
Discussion
This population-based, end-of-life cancer study displays variations in timing of end-of-life homecare nursing among 28 regions across three Canadian provinces (BC, NS, ON). While past research has demonstrated the important benefits of early end-of-life homecare, this is the first study that compares the time to initiation of end-of-life homecare visits and establishes an empiric benchmark: 57 days after the six-month point (i.e. 125 days or 4.2 months before death). We found a nearly two-fold difference in the timing of when end-of-life homecare nursing was initiated among select regions. Starting from 6 months before death, BC generally has regions with the shortest times to initiation and ON has regions with the longest times to initiation (i.e. initiated closest to death) of end-of-life homecare. Ultimately this information is useful for health system planners aiming to monitor health system performance and improve policies related to end-of-life homecare access.
Prior cancer-based randomized controlled trials demonstrating the benefits of early palliative care (i.e. at late-stage diagnosis [9] or 8–12 weeks from diagnosis [8]) were conducted in hospital-based programs: Intervention patients received early palliative care and survived for a median of 11.6 months [9] and 14 months [8], respectively. In comparison, our patients received home-based end-of-life care for a far shorter period, ranging from 125 to 83 days before death. The variation in timing may reflect the differences between palliative approach to care versus end-of-life care and/or the differences between implementing a resource-intensive home-nursing program versus a hospital program.
Past research has also used similar benchmark methods to establish quality indicators for end-of-life cancer care, such as Emergency Department visits, physician visits, Intensive Care Unit admissions, and deaths in hospital [20]. This study extends those indicators by establishing “time to initiation of end-of-life homecare nursing” as an additional quality indicator, and is related to early initiation of supportive care rather than over-aggressive acute care. In prior research, BC was identified as having the lowest hospital death rate; our study corroborates this trend as the BC regions had among the shortest mean times to first end-of-life homecare nursing. Further research is required to understand differences in provincial policies that may explain variation. Other countries could apply these methods to determine their own regional variation and benchmarks and compare against Canadian rates.
The presentation of benchmark data using a funnel plot allows health system planners to observe their performance among regions of similar, smaller, or larger sizes. It is worth noting that the two regions better than the benchmark mean are very different in size (n = 372 and n = 3663), suggesting that region size is not necessarily the most important factor in early initiation of end-of-life homecare nursing. In fact, several small, medium, and large sized regions are near the benchmark. Another advantage of this approach is that often times, benchmark values are set by larger regions or based on crude unadjusted rates. As such smaller regions find it difficult to compare themselves to larger regions. Using this approach, other regions near to or worse than the overall mean can identify a realistic comparator mean, such as a region of similar size. As a result, this supports quality improvement by setting realistic targets that regions and/or provinces can aim to achieve and may help to reduce overall variation, particularly when using recent data and monitoring over time. Moreover, health system planners can compare against better performing regions and identify what policies they have that facilitate improved access.
This study is limited by including only cancer decedents in the analysis. Using a population-based decedent cohort prevents us from examining if and when individual patients ought to have received end-of-life home care nursing [21]. However, using retrospective decedent cohorts have been shown to be an efficient way to monitor performance at a population level [22], particularly as palliative care continues to be advocated earlier in the disease trajectory [9]. The quality of end-of-life homecare nursing is not described in administrative data. Additionally, we are unable to take other factors into account that may play a role in our results. For instance, patient preferences, level of need, refusal of services, or level of caregiver support or burnout are not available in our databases. As a result, we are not able to determine appropriateness of timing at an individual-level (more clinically relevant at a patient level), but rather we can only look at variation in timing at regional population level (more relevant for health system policy planner level). Further research should explore timing of homecare services based on comprehensive patient-level factors. Strengths of the study include using a population-based cohort from three provinces, comprising approximately 54% of the population in Canada. Hence, the results possess high external validity, which likely can be generalized to the entire Canadian population. Computing benchmark values through the use of real-world data gives insight into what is required for a practical and realistic target goal. Furthermore, the methods to explore regional variation and determine benchmarks would be relevant to other countries, particularly those with publicly-funded home care systems, though the actual benchmark values might differ.
Conclusions
In conclusion, we identified regional variation and empiric benchmarks for time to initiation of end-of-life homecare nursing using administrative health care data from three provinces. Identifying a benchmark using the best-performing regions is a beginning step. Understanding the reasons for variation, particularly provincial variation, could enable more equitable care. Exploring health system processes within best-performing regions could provide insights for other regions trying to initiate homecare services earlier. Ongoing surveillance efforts are essential to enable timely and realistic targets. National-level data sharing arrangements will allow more rapid access to regional and provincial comparisons and system performance measures.
Abbreviations
- BC:
-
British Columbia
- NS:
-
Nova Scotia
- ON:
-
Ontario
References
Brazil K, Howell D, Bedard M, Krueger P, Heidebrecht C. Preferences for place of care and place of death among informal caregivers of the terminally ill. Palliat Med. 2005;19(6):492–9.
Quality End-of-Life Care Coalition of Canada. Hospice Palliative Home Care in Canada: A Progress Report. Ottawa: Quality End-of-Life Care Coalition of Canada; 2008.
Kelley AS, Deb P, Du Q, Carlson MDA, Morrison RS. Hospice enrollment saves money for Medicare and improves care quality across a number of different lengths-of-stay. Health Aff. 2013;32(3):552–61.
Kerr CW, Donohue KA, Tangeman JC, Serehali AM, Knodel SM, Grant PC, Luczkiewicz DL, Mylotte K, Marien MJ. Cost savings and enhanced hospice enrollment with a home-based palliative care program implemented as a hospice–private payer partnership. J Palliat Med. 2014;17(12):1328–35.
Taylor DH, Ostermann J, Van Houtven CH, Tulsky JA, Steinhauser K. What length of hospice use maximizes reduction in medical expenditures near death in the US Medicare program? Soc Sci Med. 2007;65(7):1466–78.
Gomes B, Higginson IJ. Factors influencing death at home in terminally ill patients with cancer: systematic review. BMJ. 2006;332(7540):515–21.
Seow H, Barbera L, Howell D, Dy SM. Using more end-of-life homecare services is associated with using fewer acute care services: a population-based cohort study. Med Care. 2010;48(2):118–24.
Bakitas MA, Tosteson TD, Li Z, Lyons KD, Hull JG, Li Z, Dionne-Odom JN, Frost J, Dragnev KH, Hegel MT. Early versus delayed initiation of concurrent palliative oncology care: patient outcomes in the ENABLE III randomized controlled trial. J Clin Oncol. 2015;33(13):1438–45.
Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, Dahlin CM, Blinderman CD, Jacobsen J, Pirl WF. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2010;363(8):733–42.
Zimmermann C, Swami N, Krzyzanowska M, Hannon B, Leighl N, Oza A, Moore M, Rydall A, Rodin G, Tannock I. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet. 2014;383(9930):1721–30.
Chitnis X, Georghiou T, Steventon A, Bardsley M. Effect of a home-based end-of-life nursing service on hospital use at the end of life and place of death: a study using administrative data and matched controls. BMJ Support Palliat Care. 2013;3(4):422–30.
Seow H, Sutradhar R, McGrail K, Fassbender K, Pataky R, Lawson B, Sussman J, Burge F, Barbera L. End-of-life cancer care: temporal association between homecare nursing and hospitalizations. J Palliat Med. 2016;19(3):263–70.
Statistics Canada. Annual demographic estimates: Subprovincial areas 2005 to 2010. Ottawa: Statistics Canada; 2011. pp. 91–214.
British Columbia Ministry of Health. Home and Community Care (Continuing Care). Victoria: Ministry of Health; 2012.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9.
Wilkins R. PCCF+ version 3J User’s guide (Geocodes/PCCF). Automated geographic coding based on the statistics Canada postal code conversion files, including postal codes to May 2002. Ottawa: Health Analysis and Measurement Group, Statistics Canada; 2002.
Canadian Institute for Health Information (CIHI). Development of National Indicators and Reports for Home Care: Phase 2 Indicator Descriptions. Ottawa: CIHI; 2002.
Kiefe CI, Weissman NW, Allison JJ, Farmer R, Weaver M, Williams OD. Methodology matters-XII. Identifying achievable benchmarks of care: concepts and methodology. Int J Qual Health Care. 1998;10(5):443–7.
Dover DC, Schopflocher DP. Using funnel plots in public health surveillance. Popul Health Metrics. 2011;9(1):58.
Barbera L, Seow H, Sutradhar R, Chu A, Burge F, Fassbender K, McGrail K, Lawson B, Liu Y, Pataky R. Quality indicators of end-of-life care in patients with cancer: what rate is right? J Oncol Pract. 2015;11(3):e279-e287.
Bach PB, Schrag D, Begg CB. Resurrecting treatment histories of dead patients: a study design that should be laid to rest. JAMA. 2004;292(22):2765–70.
Earle CC, Ayanian JZ. Looking back from death: the value of retrospective studies of end-of-life care. J Clin Oncol. 2006;24(6):838–40.
Acknowledgements
The authors would like to acknowledge the following people for their feedback during the preparation of this manuscript: Reka Pataky, Erin O’Leary, Ying Liu, and Konrad Fassbender.
Funding
This study was funded by the Canadian Cancer Society Research Institute (grant number 700689) and also supported by the Canadian Partnership Against Cancer’s Applied Research in Cancer Control (grant number 019789). This study used databases maintained by the Institute for Clinical Evaluative Sciences, which receives funding from the ON Ministry of Health and Long Term Care. The British Columbia Cancer Agency and the BC Ministry of Health approved access to and use of the data facilitated by Population Data BC for this study. Portions of the data used in this report were made available by the NS Department of Health and Wellness and the Population Health Research Unit (now known as Health Data NS) of Dalhousie University. The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding and data providing sources.
Availability of data and materials
The datasets used in this study are held in securely coded format at the Institute for Clinical Evaluative Sciences (ICES). Data sharing restrictions apply, which prohibit ICES from making the datasets publically available. However, access may be granted to those who meet the conditions for confidential access, available at www.ices.on.ca/DAS.
Author information
Authors and Affiliations
Contributions
HS and LB designed the study and were responsible for the acquisition of data. HS, LB, and RS conducted the statistical analysis of the data, with all authors making important contributions to its interpretation. HS and DQ drafted the initial manuscript. LB, KM, BL, FB, and RS critically revised each draft of the manuscript and made significant contributions to its intellectual content. HS and DQ reviewed and approved the final draft of the manuscript. All authors read and approved the final manuscript.
Ethics declarations
Ethics approval and consent to participate
The study was approved by research ethics boards at McMaster University (ON), Capital Health (NS), and BC Cancer Agency (BC).
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Seow, H., Qureshi, D., Barbera, L. et al. Benchmarking time to initiation of end-of-life homecare nursing: a population-based cancer cohort study in regions across Canada. BMC Palliat Care 17, 70 (2018). https://doi.org/10.1186/s12904-018-0321-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-018-0321-5