Abstract
Background
There is limited population-level research on end-of-life care in Australia that considers health care use and costs across hospital and community sectors. The aim of this study was to quantify health care use and costs in the last 6 months of life in a cohort of elderly Australian decedents and to examine the factors associated with end-of-life resource use and costs.
Methods
A retrospective cohort study using routinely collected health data from Australian Government Department of Veterans’ Affairs clients. The study included two cohorts of elderly Australians who died between 2005 and 2009; one cohort with a recorded cancer diagnosis and a comparison cohort with no evidence of a cancer history. We examined hospitalisations, emergency department (ED) visits, prescription drugs, clinician visits, pathology, and procedures and associated costs in the last 6 months of life. We used negative binominal regression to explore factors associated with health service use and costs.
Results
The cancer cohort had significantly higher rates of health service use and 27% higher total health care costs than the comparison cohort; in both cohorts, costs were driven primarily by hospitalisations. Older age was associated with lower costs and those who died in residential aged care incurred half the costs of those who died in hospital.
Conclusions
The results suggest differences in end-of-life care pathways dependent on patient factors, with younger, community-dwelling patients and those with a history of cancer incurring significantly greater costs. There is a need to examine whether the investment in end-of-life care meets patient and societal needs.
Similar content being viewed by others
Background
Elderly populations continue to grow, with estimates that in Organisation for Economic Co-operation and Development (OECD) countries one in five people will be 65 years and older by 2030 [1] and, in developed countries, at least half of the population over 65 have more than one chronic condition [2,3,4,5]. As populations become sicker, they have increasing health care needs and it is not surprising that per capita health care costs increase with age [4]. However, the health care costs associated with ageing are low compared with costs incurred in the 6–12 months prior to death; some estimates show that per capita health care costs are up to four times higher in those at the end of life compared with age-matched persons who are not at life’s end. For example, Neuman et al. [4] found that in the USA, average Medicare per capita spending for beneficiaries age 96 ($US16,145) was more than double that for beneficiaries age 70 ($US7,566) [4, 6].
There is a growing literature dedicated to understanding patterns of health care use and costs at the end of life, much of which has been conducted using routinely collected health care data [6,7,8,9]. The research highlights the extensive array of health care services delivered at the end of life and the high costs associated with care. However, significant variability is reported in end-of-life health care and costs which is dependent on a range of patient and health system factors; one of the most consistently important factors is age at death [8]. Several studies show that the chance of receiving intensive or life-sustaining treatments such as chemotherapy, emergency department (ED) visits, and admission to intensive care units and hospitals decreases with age [10,11,12,13,14,15,16]. As such, it is not surprising that corresponding health care costs decrease steadily with age, particularly in those aged 85 years and older [4, 14, 15, 17, 18]. To date, the majority of research on end-of-life care has been undertaken in Europe or North America. Given the complexities and jurisdiction-specific features of end-of-life care for elderly patients, there is a need to conduct studies that account for local health system characteristics such as the relationship between primary and hospital-based care, level of subsidisation of services and the availability of hospice and palliative care services.
The aim of this study is to quantify health care use and costs in the last 6 months of life in the Australian setting and to examine the factors associated with end-of-life care in an elderly decedent population. We compare total health care use and costs in two elderly decedent cohorts; a cohort with a history of cancer and a cohort without a cancer history. We focused on comparing cohorts with and without a previous cancer diagnosis as cancer is the leading cause of death in Australia and other similar countries and cancer patients represent a significant proportion of patients receiving end-of-life care [19, 20]. Additionally, patterns of end-of-life cancer care are more extensively studied and understood than other terminal diseases which provides an important context within which to interpret our findings [21].
Methods
Setting
The Australian Government Department of Veterans’ Affairs (DVA) funds the health care of eligible veterans, war widows, war widowers and their dependents. DVA clients have access to the universal health care arrangements provided to Australian permanent residents and citizens plus additional DVA-approved services and pharmaceutical items not subsidised for the general population; the types of services subsidised depends on the level of entitlement.
Study design and population
This study used data from the cancer and comparison cohorts developed for the End of Life in Cancer Care (EOL-CC) study, the details of which have been published elsewhere [22]. Briefly, this is a retrospective study of two decedent cohorts of Australian DVA clients with full health care entitlements during the last 12 months of life to ensure near-complete capture of health-related resource use and costs. Clients were eligible for the study if they: resided in New South Wales (Australia’s most populous state) in the 18 months prior to death; were aged 65 years or older at death; died between June 30 2005 and December 31 2009; and received at least one health service in the last 12 months of life. The cancer cohort had a notifiable cancer diagnosis recorded in the NSW Central Cancer Registry between 1994 and 2009. The comparison cohort comprised the remaining eligible clients with no evidence of a cancer notification or any cancer related health service use or cancer medicine; for more information, see our study protocol [22].
Data sources and linkage
The data infrastructure comprises DVA data holdings linked with NSW Ministry of Health data collections. Data were linked by a third party under the custodianship of the DVA, the NSW Ministry of Health and the Cancer Institute NSW, using best practice, probabilistic, privacy preserving protocols [23]. The linked datasets capture information on DVA client characteristics, residence in an aged care facility, cancer notification history and cause of death. However, we did not present information on cause of death for the two cohorts because information was only available to 2007. For those who died in the period 2005–2007, the most common causes of death in the cancer cohort were cancer (59%) and diseases of the circulatory system (21%). For the comparison cohort, the most common causes of death were diseases of the circulatory system (48%), lung disease (7%) and dementia (9%); for more information see our study protocol [23].
The linked datasets also include information about all subsidised health services including hospital admissions, emergency department (ED) presentations and dispensed prescription medicines. Clinical consultations, pathology services and procedures; procedures include diagnostic services (e.g., ultrasound, CT, MRI), therapeutic services (e.g., radiotherapy) and surgery are also captured; unit costs were available for all these services, while costs for the hospital admissions and ED presentations were calculated per admission or presentation using the methodology described in the NSW Costs of Care Standards Report 2009/10. Full details of the costing methods are described elsewhere [22].
Statistical analyses
Outcomes were health service use and associated costs in the last 6 months of life based on six constructed ‘months’ consisting of 30 days each; all individuals are observed for exactly 180 days to the date of death.
We calculated person-level mean (with 95% confidence interval (CIs)) and median (with inter quartile range (IQR)) service use and costs for the entire six-month period, and by month until death.
We allocated unit costs to each item of resource use to calculate mean (95% CI) and median (IQR) costs in 2009/10 Australian dollars. Total costs were calculated as the sum of costs of health services (excluding any services received during a hospitalisation which are captured in hospital costs), pharmacy, ED and hospital costs (excluding the pharmacy component of hospital costs for private hospital patients which is captured in the prescribing database); more details are reported elsewhere [22, 24].
Factors associated with resource use and costs
We used negative binomial regression to determine factors associated with health service use and costs. The cost data can be thought of as counts (of dollars and cents). Cost data are non-negative and skewed so count data models can be applied to these data, and in our case this makes sense because it is consistent with the method used for utilization [25]. Factors included: age, sex, comorbidity burden, location of residence (remoteness, areas of socioeconomic disadvantage), year of death, residence in an aged care facility and place of death. These variables were selected based on common factors found to predict patterns of health service use as death approaches [22]. Comorbidity burden was estimated in the periods prior to the last 6 months of life using hospitalisation codes (Charlson index [26]) and prescription dispensing history (RxRisk [27]); while the Charlson is likely to under ascertain morbidity burden it is more likely to capture people with severe morbidity, e.g. those needing admission to hospital for the condition. Two indices were used to capture a more complete morbidity history [22, 28].
Separate models were estimated for utilisation and costs of each type of health service (i.e., clinician visits, pathology and procedures; prescription medicines dispensed; ED visits and hospitalisations) and total health care costs. The strength of associations was represented by adjusted incident rate ratios with 95% CIs, and two-tailed p < 0.05 were used as a criterion for statistical significance.
We used SAS version 9.3 (SAS Institute) for data manipulation and performed statistical analyses using STATA version 12 (StataCorp).
Results
Cohort characteristics [Table 1]
A total of 9862 decedents met the eligibility criteria for the cancer cohort and 15,483 for the comparison cohort. The cohorts were similar in relation to age, socioeconomic status and geographical location of residence. Comorbidity burden (based on hospitalisations) was higher in the cancer cohort; 17% of cancer decedents versus 10% of the comparison cohort had a comorbidity score of three or more. However, comorbidity burden was similar for both cohorts when calculated based on prescription medicines dispensed [Table 1].
Resource use and costs in the last 6 months of life
On average, decedents in the cancer cohort were dispensed 41 medicines (vs. 38 medicines in the comparison cohort), received 90 clinician visits/procedures (vs. 66 in the comparison cohort) and had approximately three hospital admissions (vs. two in the comparison cohort). The mean number of ED visits was similar in both cohorts at about one visit/decedent in the last 6 months of life [Additional file 1: Table S1].
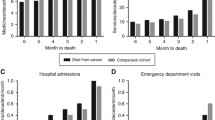
The mean total cost associated with health care in the last 6 months of life was higher in the cancer cohort ($28,091 per decedent) than the comparison cohort ($19,696 per decedent). Costs were driven primarily by hospitalisations, accounting for about 80% of total costs in both cohorts [Fig. 1].
Prescription medicines
The mean cost of medicines per person in the cancer cohort was $1840 compared with $1234 for the comparison cohort. [Additional file 1: Table S1] The difference was driven by the costs of antineoplastic and immunomodulation agents (mean of $469 per person in the cancer cohort vs. $5 in the comparison cohort).
Clinician visits and procedures
Differences in utilisation can be attributed mainly to higher numbers of medical specialist visits and pathology services in the cancer cohort. The greatest difference in health service costs related to diagnostic procedures at a mean cost of $1041 per person in the cancer cohort compared to $568 for the comparison cohort. The cost of therapeutic procedures also differed substantially between cohorts, with mean costs of $877 and $464 per person in the cancer and comparison cohorts respectively [Additional file 1: Table S1].
Hospitalisations
The difference in hospitalisation costs was driven by the higher number of admissions in the cancer cohort (mean of three episodes per person costing $22,852 in total) than the comparison cohort (two episodes per person costing $15,893 in total). [Additional file 1: Table S1] Only 15% of the cancer cohort and 3% of the comparison cohort received a palliative service while in hospital; and 4% of the cancer cohort and <1% of the comparison cohort were admitted to a hospice [Additional file 1: Table S2].
Resource use and costs by month, during the last 6 months of life [Figs. 2 and 3]
Rates of health service use and associated costs increased over the last 6 months of life and peaked in the last month of life. Total costs for both cohorts and in each month to death are driven by the cost of hospitalisations [Fig. 1].
Factors associated with resource use and costs
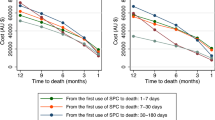
Multivariable analyses demonstrate that cancer decedents had significantly higher rates of prescription medicines (adjusted IRR: 1.09; 95% CI: 1.08–1.11, p < 0.001); clinician visits and procedures (adjusted IRR: 1.23; 95% CI: 1.20–1.25, p < 0.001); hospitalisations (adjusted IRR: 1.26; 95% CI: 1.23–1.30, p < 0.001) and ED visits (adjusted IRR: 1.05; 95% CI: 1.02–1.08, p < 0.001) than the comparison cohort. Decedents aged over 90 at death had lower rates of prescription medicines (adjusted IRR: 0.92; 95% CI: 0.90–0.93, p < 0.001); clinician visits and procedures (adjusted IRR: 0.81; 95% CI: 0.79–0.84, p < 0.001); hospitalisations (adjusted IRR: 0.76; 95% CI: 0.74–0.79, p < 0.001) and ED visits (adjusted IRR: 0.91; 95% CI: 0.88–0.95, p < 0.001) than younger decedents [Fig. 4].
Overall, cancer decedents incurred 27% higher health care costs than non-cancer decedents, (adjusted IRR: 1.27; 95% CI: 1.24–1.30, p < 0.001) [Fig. 5]. The cancer cohort had 42% higher costs for prescribed medicines (adjusted IRR: 1.42; 95% CI: 1.39–1.46, p < 0.001), 32% higher costs for clinician visits and procedures (adjusted IRR: 1.32; 95% CI: 1.29–1.35, p < 0.001) and 28% higher costs for hospitalisations (adjusted IRR: 1.28; 95% CI: 1.21–1.35, p < 0.001) than the comparison cohort. There was no significant difference in costs associated with ED visits (adjusted IRR: 1.05; 95% CI: 0.98–1.12, p = 0.166) [Fig. 5]. A number of factors were associated with lower health care costs: decedents aged over 90 at death had 20% lower health care costs than decedents aged 80–84 (adjusted IRR: 0.80; 95% CI: 0.77–0.82); decedents residing in residential aged facilities incurred 9% lower total costs (adjusted IRR: 0.91; 95% CI: 0.88–0.95); and those who died in residential aged care incurred less than half the costs of those who died in hospital (adjusted IRR: 0.47; 95% CI: 0.45–0.49) [Fig. 5].
Discussion
This study used routine health care data collections to quantify and characterise factors associated with health care use and costs at the end of life in elderly decedents. Our results suggest wide variation in end-of-life care, particularly when comparing decedents with and without a cancer history. Decedents with a cancer history had higher rates health services use and higher associated costs than non-cancer decedents. Age at death was also a determinant of end-of-life care, with older decedents in both cohorts using fewer health care services than younger decedents. This is the first study of its kind in Australia, yet the results align with studies conducted internationally in terms of the impact of age on health services use and distribution of health care costs, with hospitals being the main driver of end-of-life costs [8].
Our results suggest systematic differences in the care received by elderly populations, particularly those aged 85 years and over. The patterns of care received by this group may suggest a different attitude towards active or intensive treatment for this group compared with their younger counterparts. Our finding that older decedents were less likely to use hospital and ED services are similar to another study examining the entire NSW population which reported that decedents aged 90 and older were 60% less likely to have more than three hospital episodes and 85% less likely to spend time in the ICU than those aged 60–79 years at death [29]. Our results show that not only were elderly decedents (both cancer and non-cancer) less likely to be admitted to hospital, but also received fewer clinician visits and prescription medicines at the end of life. The reduced services in elderly decedents may be compounded by the fact that this group are more likely to live in residential aged care settings; those who died in residential aged care incurred half the health care costs of those who died in hospital. While some literature suggests that lower rates of hospital and ED use at the end of life may represent quality care, [30] there is a need to further investigate whether the reductions in end-of-life health service use in elderly decedents translate into appropriate treatment that is consistent with patient preferences [31, 32]. We suggest that the differences in care observed in this and other studies does not necessarily represent inequities in treatment. Rather, the very elderly may have their end-of-life needs met with other sources of care [33, 34].
Services such as palliative hospital admissions and use of hospice care are regarded as important for delivering quality end-of-life care [7]. The proportion of people receiving palliative services in hospital in the last 6 months of life was low (14.7% in the cancer cohort and 3.1% for the comparison cohort); hospice admissions were also low (4.1% and 0.5% respectively, for the same cohorts).While our findings are consistent with other studies reporting the challenges of elderly patients accessing palliative services in acute care settings, [35] a limitation of our study is that rates of palliative care services delivered may be underestimated due to coding practices in Australia not being tied to hospital payment [36]. Nevertheless, the low rates of palliative services in this study are important from a health care planning perspective and warrant further examination. National data demonstrate that less than half of all patients who die in hospital receive any palliative care service [36].
Our findings have important policy implications within the broader social and economic context of end-of-life care. For instance, international studies and surveys of the Australian population indicate that most people with a terminal condition would prefer to die at home and prefer a symptom management approach rather than intensive treatment or heroic life-saving measures [37,38,39]. However, we found that hospital was the most common place of death and also placed the greatest burden on the health system in terms of costs. This indicates the need for more widespread discussion between patients, providers, caregivers, and health system managers about end-of-life planning (e.g., measures such as advanced care directives). Indeed, patients’ awareness that their condition is terminal and end-of-life discussions with clinicians have been demonstrated to result in the delivery of care in-line with patient preferences [31, 40]. There is also evidence that suggests there is merit in increasing resources for community-based palliative care services [41, 42]. While our study is comprehensive in that it captures nearly all health services from a health payer perspective, recent studies considering costs more broadly found that between one-fifth and one-third of overall end-of-life care costs can be attributed to informal care givers [43]. Costs of informal caregiving and patient preferences are not captured in routinely collected data holdings but this information is needed to fully understand how to maximise the value of end-of-life care services at a population-level in a health care environment with limited resources.
There are a number of strengths of our study, including our comprehensive patient-level analysis using multiple linked routine data collections. Our findings relating to DVA clients may not be generalisable to the elderly Australian cancer population. However, there is evidence that DVA clients have similar rates of health service use when compared with Australians of a similar age [44, 45] and comparison with recent studies on end-of-life hospital care in the general population suggest similar rates of hospital admissions and ED visits [29, 46].
A study limitation is that we do not provide information on patterns of end-of-life care in people under 65 years of age, a group that represents about 20% of all deaths in Australia [47] and up to one third of cancer deaths [20, 48]. Also there may have been changes in practice in Australia since our study period ended in 2009; however, the data reflect the most recent available at the time this research was undertaken. Another potential limitation of our study is the retrospective study design that does not necessarily reflect the challenges associated with predicting survival time in real world clinical practice [49]. However, some research comparing prospective and retrospective designs found similar patterns of end-of-life health care [13, 50].
Conclusion
Decedents with a history of cancer used more services and incurred higher costs in the last 6 months of life than decedents without a cancer history. We also found evidence of a shift in treatment patterns by age with decedents aged 65–84 years receiving a greater number and range of services (particularly hospital based services) than those aged85 years and older. Future research is required to understand which patterns of care are associated with improved patient-reported care and to understand which patterns of care represent the best value in terms of appropriateness, quality and patient preferences.
Change history
10 October 2017
An erratum to this article has been published.
Abbreviations
- CT:
-
Computed tomography
- DVA:
-
Department of Veterans Affairs
- ED:
-
Emergency Department
- EOL-CC:
-
End-of-life cancer care study
- ICU:
-
Intensive care unit
- MRI:
-
Magnetic resonance imaging
- NSW:
-
New South Wales
References
OECD. Economic, environmental and social statistics. Paris: OECD; 2009.
Barnett K, Mercer SW, Norbury M. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43.
Fortin M, Stewart M, Poitras M. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med. 2012;10:142–51.
Neuman P, Cubanski J, Damico A. Medicare per capita spending by age and service: new data highlights oldest beneficiaries. Health Aff. 2014;34:335–9.
Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition-multimorbidity. JAMA. 2012;307:2493–4.
Yabroff KR, Warren JL, Brown ML. Costs of cancer care in the USA: a descriptive review. Nat Clin Pract Oncol. 2007;4:643–56.
Barbera L, Seow H, Sutradhar R, Chu A, Burge F, Fassbender K, et al. Quality indicators of end-of-life care in patients with cancer: What rate is right? J Oncol Pract. 2015;11(3):e279–87.
Langton JM, Blanch B, Drew AK. Retrospective studies of end-of-life resource utilization and costs in cancer care using health administrative data: a systematic review. Palliat Med. 2014;28:1167–96.
Luta X, Maessen M, Egger M. A., S. Measuring intensity of end of life care: review. PLoS One. 2015;10:e0123764.
Burge FI, Lawson BJ, Johnston GM. A population-based study of age inequalities in access to palliative care among cancer patients. Med Care. 2008;46(12):1203–11.
Gagnon B, Mayo NE, Hanley J. Pattern of care at the end of life: does age make a difference in what happens to women with breast cancer? J Clin Oncol. 2004;22(17):3458–65.
Ho TH, Barbera L, Saskin R. Trends in the aggressiveness of end-of-life cancer care in the universal health care system of Ontario, Canada Oncol. J Clin Oncol 2011, 29:1587-1591.
Setoguchi S, Earle CC, Glynn R. Comparison of prospective and retrospective indicators of the quality of end-of-life cancer care. J Clin Oncol. 2008;26:5671–8.
Shugarman LR, Bird CE, Schuster CR. Age and gender differences in Medicare expenditures at the end of life for colorectal cancer decedents. J Women’s Health. 2007;16:214–27.
Shugarman LR, Bird CE, Schuster CR. Age and gender differences in medicare expenditures and service utilization at the end of life for lung cancer decedents. Womens Heal Issues. 2008;18:199–209.
Virnig BA, McBean A, Kind S. Marshall hospice use before death: variability across cancer diagnoses. Med Care. 2002;40:73–8.
Kaul P, McAlister FA, Ezekowitz JA. Resource use in the last 6 months of life among patients with heart failure in Canada. Arch Intern Med. 2011;171:211–7.
Unroe KT, Greiner MA, Hernandez AF. Resource use in the last 6 months of life among medicare beneficiaries with heart failure, 2006-2007. Arch Intern Med. 2011;171:196–203.
Australian Institute of Health and Welfare (AIHW). Cancer survival and prevalence in Australia: period estimates from 1982 to 2010. Canberra: AIHW; 2013.
Australian Institute of Health and Welfare (AIHW). Cancer in Australia: an overview. Canberra: AIHW; 2014.
Lunney JR, Lynn J, Hogan C. Profiles of older medicare decedents. J Am Geriatr Soc. 2002;50:1108–12.
Langton JM, Srasuebkul P, Reeve R, Parkinson B, Gu Y, Buckley NA, et al. Resource use, costs and quality of end of life care: observations in a cohort of elderly Australian cancer decedents. Implement Sci. 2015;10:25.
Centre for Health Record Linkage (CHeReL). http://www.cherel.org.au/.
Reeve R, Haas M. Estimating the cost of emergency department presentations in NSW. CHERE working paper 2014/01. In. Sydney: CHERE; 2014.
Jones A. Models for health care. HEDG working paper 10/01. York: University of York; 2010.
Sundararajan V, Henderson T, Perry C. New ICD 10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004, 57 SRC - GoogleScholar:1288–1294.
Sloan KL, Sales AE, Liu C. Construction and characteristics of the RxRisk-V: a VA-adapted pharmacy-based case-mix instrument. Med Care. 2003;41:761–74.
Lu CY, Barratt J, Vitry A. Charlson and Rx-risk comorbidity indices were predictive of mortality in the Australian health care setting. J Clin Epidemiol. 2011;64:223–8.
Goldsbury DE, Connell DL, Girgis A, C. BM. O’ Acute hospital-based services used by adults during the last year of life in New South Wales, Australia: a population-based retrospective cohort study. Health Serv Res. 2015; 15:537.
Earle CC, Neville BA, Landrum MB. Evaluating claims-based indicators of the intensity of end-of-life cancer care. Int J Qual Health Care. 2005;17:505–9.
Mack JW, Cronin A, Taback N. End-of-life care discussions among patients with advanced cancer: a cohort study. Ann Intern Med. 2012;156:204–10.
You JJ, Dodek P, Lamontagne F. What really matters in end-of-life discussions? Perspectives of patients in hospital with serious illness and their families. Can Med Assoc J. 2014;186:E679–87.
Burt J, Plant H, Omar R, Raine R. Equity of use of specialist palliative care by age: cross-sectional study of lung cancer patients. Palliat Med. 2010;24(6):641–50.
Burt J, Raine R. The effect of age on referral to and use of specialist palliative care services in adult cancer patients: a systematic review. Age Ageing. 2006;35(5):469–76.
Gardiner C, Cobb M, Gott M, Ingleton C. Barriers to providing palliative care for older people in acute hospitals. Age Ageing. 2011;40(2):233–8.
Australian Institute of Health and Welfare (AIHW). Palliative care services in Australia. Canberra: AIHW; 2014.
The National Palliative Care Strategy 2010. Supporting Australians to live well at the end of life. Canbera: Commonwealth of Australia; 2010.
Gomes B, Calanzani N, Gysels M, C BM. Heterogeneity and changes in preferences for dying at home: a systematic review. BMC Palliat Care. 2013; 12:7.
Gomes B, Higginson IJ, Calanzani N. Preferences for place of death if faced with advanced cancer: a population survey in England, Flanders, Germany, Italy, the Netherlands, Portugal and Spain. Ann Oncol. 2012;23:2006–15.
Zhang B, Wright AA, Huskamp HA. Health care costs in the last week of life associations with end-of-life conversations. Arch Intern Med. 2009;169:480–8.
Abernethy AP, Currow DC, Shelby-James T, Rowett D, May F, Samsa GP, et al. Delivery strategies to optimize resource utilization and performance status for patients with advanced life-limiting illness: results from the “palliative care trial” [ISRCTN 81117481]. J Pain Symptom Manag. 2013;45(3):488–505.
Almaawiy U, Pond GR, Sussman J. Are family physician visits and continuity of care associated with acute care use at end-of-life? A population-based cohort study of homecare cancer patients. Palliat Med. 2014;28:176–83.
McCaffrey N, Cassel JB, Coast J. Bringing the economic cost of informal caregiving into focus. Palliat Med. 2015;29:866–7.
Australian Institute of Health and Welfare (AIHW). Health care usage and costs: A comparison of veterans and war widows and widowers with the rest of the community Canberra Australia. Canberra: AIHW; 2002.
Tooth LR, Hockey R, Treloar S. Does government subsidy for costs of medical and pharmaceutical services result in higher service utilization by older widowed women in Australia? BMC Health Serv Res. 2012;12:179.
Rosenwax LK, McNamara BA, Murray K. Hospital and emergency department use in the last year of life: a baseline for future modifications to end-of-life care. Med J Aust. 2011;194:570–3.
Age at death (AIHW). http://www.aihw.gov.au/deaths/age-at-death/. Accessed 19 Mar 2015.
Australian Cancer Incidence and Mortality (ACIM) books. http://www.aihw.gov.au/acim-books/. Accessed 19 Mar 2015.
Bach PB, Schrag D, Begg CB. Resurrecting treatment histories of dead patients: a study design that should be laid to rest. JAMA. 2004;292:2765–70.
Pyenson B, Connor S, Fitch K. Medicare cost in matched hospice and non-hospice cohorts. J Pain Symptom Manag. 2004;28:200–10.
Acknowledgements
The authors would like to thank the Centre for Health Record Linkage for undertaking the data linkage process.
Funding
This research is supported, in part, by a National Health and Medical Research Council Health (NHMRC) Services Research Capacity Building Grant (ID: 571,926), NHMRC Centre of Research Excellence in Medicines and Ageing (ID: 1,060,407), Cancer Australia Grant (ID: 568,773) and a University of Sydney, Faculty of Pharmacy Small Project Grant. SP is supported by a Cancer Institute New South Wales Career Development Fellowship (ID: 12/CDF/2–25).
Availability of data and materials
Our service agreement with the Australian Department of Veterans’ Affairs does not permit the authors to share the data with other parties.
Authors’ contributions
RV, MH and SP designed the research and supervised the analysis. RR and PS performed the statistical and econometric analyses. All authors reviewed the results and helped to draft the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors report no actual, potential, or perceived competing interests with regard to the submission of this manuscript.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The NSW Population and Health Services Ethics Committee (approval number 2013/11/494) and the Department of Veterans’ Affairs Human Research Ethics Committee (E013/015) approved this project.
Disclaimer
The Australian Government Department of Veterans’ Affairs is the copyright owner of the data presented in this manuscript including all tables, figures and supplementary content. The authors have obtained permission from the Australian Government Department of Veterans’ Affairs to publish this manuscript. The views expressed in this version of the work do not necessarily represent the views of the Minister for Veterans’ Affairs or the Department of Veterans’ Affairs. The Commonwealth of Australia does not give any warranty nor accept any liability in relation to the contents of this work.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
An erratum to this article is available at https://doi.org/10.1186/s12904-017-0233-9.
Additional file
Additional file 1: Table S1.
Mean and median health service use and costs in the last 6 months of life, by health service type, and cohort. Table S2. Mean and median health service use and costs in the last 6 months of life, by health service type, and cohort. (DOCX 24 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons 4.0 Attribution License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Reeve, R., Srasuebkul, P., Langton, J.M. et al. Health care use and costs at the end of life: a comparison of elderly Australian decedents with and without a cancer history. BMC Palliat Care 17, 1 (2018). https://doi.org/10.1186/s12904-017-0213-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-017-0213-0