Abstract
Background
This retrospective study investigated the effect of breathing pattern, skeletal class (Class I, Class II), and age on the hyoid bone position (HBP) in normodivergent subjects.
Methods
A total of 126 subjects (61 males, 65 females) aged 7–9 years and 10–12 years were scanned using cone-beam computed tomography (CBCT). All participants were classified according to the anteroposterior skeletal pattern into (Class I, Class II). Each skeletal group was further divided according to the breathing mode into mouth breathers (MB) and nasal breathers (NB). The HBP was measured accordingly. Independent sample t-test and Mann Whitney U test were used to detect significant differences between the groups, and binary logistic regression was used to identify MB predictive indicators.
Results
The breathing mode and skeletal class affected the vertical HBP in subjects with 7–9 years, while they affected the anteroposterior HBP in subjects with 10–12 years. Regarding the age effect, hyoid bone was located more anteriorly in the older NB subjects, and hyoid bone was more inferiorly in the older age group. A regression equation of the significant variables was formulated, C3-Me (P: 001, OR: 2.27), and H-EB (P: 0.046, OR: 1.16) were positively correlated with occurrence of MB.
Conclusion
There were significantly different HBPs among subjects with different anteroposterior skeletal classes, breathing modes, and age cohorts. Moreover, C3-Me, and H-EB were significant predictors and correlated with increased likelihood of being MB subject.
Similar content being viewed by others
Background
The respiratory function has been linked to craniofacial development and occlusion. Poor nasal respiratory function is related to low airway capacity, which might lead to mouth breathing [1].
Multiple etiologies have been associated with mouth breathing: adenoid hypertrophy is considered the most common cause of mouth breathing in children [2]; other etiologies include tonsillar hypertrophy, nasal septum deviation, hypertrophied turbinate, and allergic rhinitis [3]. According functional matrix theory, in which he stated that development of the Moss who proposed nasal resistance caused by adenoid or skeletal tissues is guided by the soft tissues, therefore [4] of the craniofacial structures tonsillar hypertrohy are thought to affect the development.
Mouth breathing was considered a predisposing factor of obstructive sleep apnea syndrome [5]. A previous study [6] posited that a brachyfacial vertical skeletal pattern with a lower position of hyoid bone was a characteristic feature of OSAS patients.
Hyoid bone was described as a floating bone since it has no articulation with any other bone. It is linked to the pharynx, cranium, and mandible by muscles and ligaments, forming the oropharyngeal complex. It has three primary functions: deglutition, phonation, and breathing [7].
Many factors are related to HBP, changes in the position of the mandible whether skeletally, surgically, or after orthodontic treatment might result in a change in HBP and pharyngeal airway volume [8,9,10,11]. Because of the tight relationship between hyoid bone and pharyngeal airway, a better knowledge of the impact of the breathing pattern, skeletal class, and age on HBP would improve orthodontic diagnosis and treatment planning.
CBCT offered more precise information than lateral cephalogram (LC) [12]. Most previous studies used LC to determine HBP, and few of them used CBCT [13,14,15,16,17,18]. However, the effect of breathing mode on HBP using CBCT has never been studied previously. Hence, this study evaluated HBP in normodivergent children aged 7–12 years old with skeletal Class I and Class II and different breathing modes.
Methods
Ethical approval
This retrospective study was approved by the Ethics Review Committee of Xi'an Jiaotong University with protocol number Xjkqll [2018] No.17.
Sample size calculation
Sample size was calculated using a formula proposed by Pandis [19] with power = 80%, level of significance = 0.05, to detect a difference of 4.44 mm in H–V distance between MB and NB and standard deviation = 4.2 mm [13]. We found that 14 subjects on each subgroup would be sufficient.
CBCT process
Each patient was requested to sit straight and maintain maximal intercuspation of their jaws; their lips and tongue were assured to be in a resting condition. The Frankfort horizontal plane of the patients was maintained parallel to the ground, and patients were advised to breathe adequately via their nose, without swallowing or moving their head or tongue. All pictures were taken using (i-Cat, Imaging Sciences International, Hatfield, PA, USA) cone beam machine at 120 kV, 5 mA, 14 × 17 cm FOV, 0.4 mm voxel, and scan time of 8.9 s. After that, the CBCT pictures were stored as DICOM (digital imaging and communications in medicine) files.
Subjects
In this study, 126 CBCT scans were collected from 61 males and 65 females. Eligible CBCT scans were obtained as a diagnostic record of children aged 7–12 years who first attended the Department of Orthodontics at Xi'an Jiaotong University from 2017 to 2021. Furthermore, prior to CBCT scanning, all patients' parents provided informed and written consent. CBCT scans with non-obvious hyoid bone and landmarks were excluded from the study, regarding the medical history, patients who had previously undergone orthodontic treatment, had enlarged tongue, or any syndromes in the head and neck area were also excluded from the study. The sample distribution of this study is illustrated in Fig. 1.
To identify the skeletal classes: ANB° from the cephalometric analysis of Steiner was used. Class I patients (1 ≤ ANB° ≤ 4.9), Class II patients (ANB° ≥ 5). All the patients were normodivergent growers (27 < FMA° < 37) [20], with (18.5 < BMI < 24) [8].
Breathing pattern diagnostic criteria
Respiratory function was assessed by a multidisciplinary approach consisting of an expert orthodontist and an otolaryngologist. The orthodontist initially took a history from the children's parents about their children's sleeping habits, such as sleeping with their mouth open, drooling in pillow, and snoring, then performed a clinical examination of the children's habitual lip posture, nostril size and shape, and the Glatzel mirror test to identify mouth breathers [21].
Furthermore, all subjects were checked by an otolaryngologist, who confirmed the mouth breathers. A full examination by an otolaryngologist comprised a nasopharyngeal x-ray, rhinoscopy, and flexible nasopharyngoscopy. Mouth breathers were diagnosed based on the existence of nasopharyngeal airway obstruction caused by adenoid or tonsillar hypertrophy [22].
CBCT orientation and measurements
The DICOM files were imported into Dolphin Imaging software (version 11.7) (Dolphin Imaging & Management Solutions®, Chatsworth, CA, USA). All measurements were taken by a single investigator who was unaware of the participants' demographics. CBCT images were oriented, the axial plane was aligned with the Frankfort plane (FHP), and the midsagittal plane was aligned with the patient's midline, which is described as a vertical plane running across Nasion point (N), and the coronal plane was adjusted to be perpendicular to the axial plane and passing through Porion point (Fig. 2).
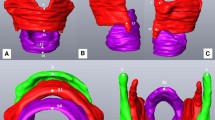
Hyoid bone measurements include eight linear measurements: H-Me, H-EB, C3-H, C3-Me, H-C3-Me, H-PNS, H–H, and H-V [14] (Table 1), (Fig. 3).
Statistical analysis
All measurements were analyzed with SPSS software (version 25.0, Chicago, Ill).
Shapiro–Wilk test was used to check the normality of variables. Among the total CBCT images, 30 images were randomly selected; Two investigators repeated all the measurements two weeks after the first measurement. The intra-investigator and inter-investigator errors were assessed by intraclass correlation coefficient. And Dahlberg’s formula \((\sqrt{\sum \frac{{D}^{2}}{2N}}\)) was used to calculate the measurements error [23].
Independent sample t-test and Mann–Whitney U test were used for multiple comparisons between the groups, and logistic regression was used to identify MB predictive indicators; a P < 0.05 was considered significant.
Results
The concordance index was ranged between 0.92 and 0.99 for the intra-investigator, and from 0.86 to 0.96 for the inter-investigator in the ICC test revealing high intra and inter-examiner reliability. Furthermore, the measurements errors ranged between 0.73 and 1.2 mm, so the errors were considered negligible.
After performing the Shapiro–Wilk test, some variables revealed non-normal distribution, so Mann Whitney U test was used for the non-normally distributed variables (H-EB, C3-H, C3-Me, H–H, H-V), and Independent sample t-test was performed for the normally distributed variables (H-Me, H-C3Me, H-PNS) to identify differences between the groups.
In the current study, the groups showed no significant difference in the demographic variables (Table 2).
Class I and Class II patients with the same age group and breathing mode were compared. In 7–9 years group, there was significance related to the vertical parameters of hyoid bone between anteroposterior skeletal groups (H-C3Me, P = 0.0001; H-PNS, P = 0.0003; H-V, P = 0.002), indicating downward HBP in the Class I MB compared to class II MB. In contrast, Class I NB appeared with an upward HBP in relation to Class II NB group (H-V, P = 0.00007). For 10–12 years group significance was accompanied with the horizontal parameters of hyoid bone; class II patients had a backward HBP in both breathing patterns with weak significance for MB group (C3-H, P = 0.045 for MB, and C3H, P = 0.001 for NB) (Table 3).
In 7–9 years group, Class I MB presented with a downward HBP compared to their matched NB participants (H-C3Me, P = 0.006; H-PNS, P = 0.010; H-V, P = 0.0001). While class II MB patients were characterized by an upward HBP compared to their NB counterparts (H-C3Me, P = 0.007; H-PNS, P = 0.006; H-V, P = 0.007) (Table 4).
For the 10–12 years group, Class I MB compared to the control NB group displayed a backward HBP in relation to S point and the 3rd cervical vertebrae (C3-H, P = 0.002; H–H, P = 0.036). Class II MB group showed a backward HBP in relation to the 3rd cervical vertebrae (C3-H, P = 0.011). No significant difference between MB and NB was detected regarding the vertical HBP for this age group (Table 4).
On the other hand, the effect of age on the HBP was considerably detected. After controlling the effect of the antero-posterior skeletal Class and breathing mode, hyoid bone vertical distance (H-V) was significantly increased in 10–12 years group than 7–9 years group in all skeletal classes and breathing mode categories (Table 5).
Additionally, Class I MB group showed significantly increased C3-Me distance in 10–12 years group compared to 7–9 years group (P = 0.017). While Class I NB group had significantly increased H-EB, C3-H, and C3-Me distances (P = 0.007, 0.00008, 0.003), respectively. Class II MB showed significantly increased differences in 10–12 years group in H-C3Me (P = 0.001) and H-PNS (P = 0.0001). While Class II NB showed significance in H-EB, and H-PNS (P = 0.026, 0.007) (Table 5).
The regression equation was formulated as Y = 0.11 − 0.769 * X1 + 0.151 * X2 − 0.969 * X3 + 0.823 * X4 − 0.064 * X7 (Y: Breathing pattern Nasal breathing or Mouth breathing; X1: H-Me; X2: H-EB; X3: C3-H; X4: C3-Me; X7: H–H). According to the equation, C3-H was the most influencing factor, followed by C3-Me, H-Me, H–H, and H-EB (P value: 0.0001, 0.001, 0.001, 0.046, and 0.020 respectively); considering that the negative β value indicated decreased likelihood of falling into MB group, while the positive β value indicated increased likelihood of falling into MB group. (Table 6).
Discussion
Our findings asserted that there were differences in HBP between MB and NB children, in addition antero-posterior skeletal Class (Class I and Class II), and age affected HBP.
Different methodologies had been used to evaluate the HBP; Lateral cephalometric was more predominant for determination of HBP [5, 24, 25]. As reported previously, the CBCT scan obtained before orthodontic diagnosis and treatment planning can help in gaining a clear clinical judgement of hyoid bone position and its surrounding structures [14]. Numerous CBCT studies [17, 18] had evaluated HBP in nasal breathing subjects. The current study used CBCT to evaluate the effect of different breathing patterns on HBP.
All CBCT images were taken when only CBCT was expected to add additional information which would aid in orthodontic diagnosis and treatment planning. The authors’ institution follows the ALARA principle “as low as reasonably achievable” [26] ensuring not to expose the patients to unnecessary ionizing radiation.
We believe that recognition of mouth breathing patients should be conducted through a multidisciplinary approach by orthodontists and otolaryngologists as recommended by Costa et al. [3] Previous literature relied on visual and clinical examination only to diagnose mouth breathing, which in fact could lead to improper mouth breathing recognition protocol [27]. This might clarify the different findings and contradictions between various researchers.
Few studies relied on otolaryngologists' diagnosis of mouth breathing [22, 28]. However, previous literature found that orthodontists can accurately diagnose nasal breathing and advised collaboration between orthodontists and otolaryngologists regarding mouth breathing diagnosis [3]. Lymphoid tissue develops fast after birth, reaches its peak size in childhood, begins to regress around the age of 8–10 years, and usually entirely diminishes around 12–14 years [29]. Hence, in our study: the history taking and clinical tests were used as preliminary screening tests for detection of mouth breathing, and the otolaryngologists confirmed the diagnosis, cooperation between the two disciplines led to a better diagnosis and treatment planning [3].
It has been documented that the HBP could be influenced by the anteroposterior sagittal skeletal patterns [9], vertical skeletal patterns [30], and age [31]. In our study, patients with similar age cohorts and skeletal patterns were compared to detect the differences in HBP between MB and NB, given that all of our participants were normal vertical growers.
Chung et al. [32] compared mouth breathing and nasal breathing children, concluded that mouth breathing patients had elevated HBP compared to the nasal breathing children, although they didn't classify their participants into different antero-posterior sagittal classes, but they found that most of mouth breathing participants had a tendency toward having Class II malocclusion, this concurred with our finding that Class II MB children aged 7–9 years exhibited an upward HBP compared to Class II NB with similar age group. Furthermore, this finding was also corroborated by Chaves et al. [33] who emphasized that asthmatic patients with mouth breathing had an elevated HBP in relation to the mandible and 3rd cervical vertebrae.
However, Cuccia et al. [24] and Behlfelt et al. [34] claimed that mouth breathing children showed extended head posture as well as a lower HBP. Our study found that in 7–9 years group, MB children with skeletal Class I displayed a lower HBP than their matched NB group. A recent study by Vuong and Kang [16] found a positive correlation between the superior HBP and the constricted airway. Furthermore, skeletal class II pattern and mouth breathing habit have been stated to predispose to a constricted airway [22, 35]. This could explain our finding that MB patients with Class II pattern exhibited more superior HBP than Class I MB patients.
Behlfelt et al. [34] suspected that the lower HBP in mouth breathers was attributed to lower position of the tongue and to allow for more airway patency as the airway volume might be decreased in the mouth breathers [29], whereas, Chaves et al. [33] suggested that the upward HBP is a compensatory mechanism; as mouth breathing is accompanied with clockwise rotation of the mandible, which might release the tension applied by suprahyoid muscle to hyoid bone, thus led to an inferior HBP and constricted pharynx as well, then mouth breathers tended to extend their heads to allow for more airway patency, this posture exaggerated the tension applied by suprahyoid muscle, which consequently pulled hyoid bone to a superior position. Moreover, in our study, we also used Sella point to determine HBP as it is a more stable reference point than cervical vertebrae and mandible [32].
According to Janicka and Halczy-Kowalik [36] who assessed the different HBP in mouth and nasal breathers, their sample ranged between 9 and 35 years old; they presumed that mouth breathers had a backward HBP described by the parameter (C3-H). This finding was consistent with our findings in 10–12 years group, in which MB in both skeletal classes demonstrated a backward HBP. However, this finding is contradicted with other findings expressed by Juliano et al. [5], who assumed an anterior HBP for mouth breathers which is attributed to their head extension to enhance breathing capacity. However, it is worthy to note that previously mentioned studies used varied study designs and methodologies to evaluate HBP.
In the current study, hyoid bone descent in the older age group. Pae et al. [6] conducted a longitudinal study and described the early descent of hyoid bone as a physiological phenomenon related to speech development, while late descent is associated with increased resistance of airway with aging which usually seen on OSAS patients.
Mouth breathing habit was reported to cause alteration in the normal growth of the craniofacial complex and could be a risk factor for developing OSAS [5]. Our regression model was capable of predicting mouth breathers based on hyoid bone measurements with 76.2% overall accuracy. Moreover, C3-Me and H-EB were found to be significant predictors, for each one-unit increase in the previously mentioned predictors the odds of being mouth breather increase by 2.27 and 1.16, respectively. Increased values of these parameters speculate that MB subjects had extended head posture and hyoid bone modifies its position to enhance breathing capacity [34].
Previous studies have shown an association between HBP and the severity of OSAS. Chang and Shiao [37] reported that the distance from the hyoid bone to the mandibular plane (MP-H) was positively correlated to the Apnea Hypopnea Index (AHI), and subjects with longer MP-H distance suffered from more daytime sleepiness. A recent review by Haskell et al. [38] discussed the favorability of AHI response to oral appliances. Treatment favorability was linked to the anatomical position and angulation of hyoid bone beside maxillofacial and pharyngeal parameters. Moreover, several studies reported hyoid bone positional changes after orthodontic treatment with functional appliances [39, 40]. Such findings highlight the need of gaining a better knowledge of HBP to permit early intervention and a better prognosis.
Our study demonstrated in-depth grouping for age and anteroposterior skeletal classes to detect the differences in HBP between NB and MB, but one limitation is we didn't include Class III patients and we didn’t consider gender differences due to the lack of samples; another limitation is our cross-sectional retrospective study is not capable to assess the causality principle; the differences between NB and MB were detected on one-time point, However, this study adopted a cross-sectional design because of the ethical concerns associated with possibility of increased radiation doses accompanying longitudinal studies; also we didn't include subjects less than 7 years old or older than 12 years old, and this study only included Chinese participants.
Conclusion
-
1.
The current study found that individuals with different anteroposterior skeletal classes, breathing mode, and age showed significantly different HBPs.
-
2.
C3- Me and H-EB were significant predictors and positively correlated with increased probability of impaired breathing function.
Availability of data and materials
Data used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- OSAS:
-
Obstructive sleep apnea syndrome
- LC:
-
Lateral cephalogram
- MB:
-
Mouth breathing
- NB:
-
Nasal breathing
- CBCT:
-
Cone-beam computed tomography
- HBP:
-
Hyoid bone position
- 3D:
-
Three dimensional
- DICOM:
-
Digital imaging and communication
- ICC:
-
Intra-class correlation coefficient
References
de Freitas MR, Alcazar NMPV, Janson G, de Freitas KMS, Henriques JFC. Upper and lower pharyngeal airways in subjects with Class I and Class II malocclusions and different growth patterns. Am J Orthod Dentofac Orthop. 2006;130(6):742–5.
Vilella BDS, Vilella ODV, Koch HA. Growth of the nasopharynx and adenoidal development in Brazilian subjects. Braz Oral Res. 2006;20(1):70–5.
Costa JG, Costa GS, Costa C, de Vasconcellos VO, Mattos CT, de Alcantara C-S. Clinical recognition of mouth breathers by orthodontists: a preliminary study. Am J Orthod Dentofac Orthop. 2017;152(5):646–53.
Moss ML. The functional matrix hypothesis revisited, 2: the role of an osseous connected cellular network. Am J Orthod Dentofac Orthopedics. 1997;112(2):221–6.
Juliano ML, Machado MAC, Carvalho LBC, Prado LBF, Prado GF. Mouth breathing children have cephalometric patterns similar to those of adult patients with obstructive sleep apnea syndrome. Arquivos de Neuro-psiquiatria. 2009;67(3B):860–5.
Pae E-K, Quas C, Quas J, Garrett N. Can facial type be used to predict changes in hyoid bone position with age? A perspective based on longitudinal data. Am J Orthod Dentofac Orthop. 2008;134(6):792–7.
Bibby R. Pres ton CB. The hyoid triangle. Am J Orthod. 1981;80:92–7.
Wu S, Wang T, Kang X, Wang X, Jiao Y, Du X, et al. Hyoid bone position in subjects with different facial growth patterns of different dental ages. CRANIO®. 2021:1–7.
Adamidis IP, Spyropoulos MN. Hyoid bone position and orientation in Class I and Class III malocclusions. Am J Orthod Dentofac Orthop. 1992;101(4):308–12.
Shin J-H, Kim M-A, Park I-Y, Park Y-H. A 2-year follow-up of changes after bimaxillary surgery in patients with mandibular prognathism: 3-dimensional analysis of pharyngeal airway volume and hyoid bone position. J Oral Maxillofac Surg. 2015;73(2):340.e1-e9.
Wang Q, Jia P, Anderson NK, Wang L, Lin J. Changes of pharyngeal airway size and hyoid bone position following orthodontic treatment of Class I bimaxillary protrusion. Angle Orthod. 2012;82(1):115–21.
Fernandes TMF, Adamczyk J, Poleti ML, Henriques JFC, Friedland B, Garib DG. Comparison between 3D volumetric rendering and multiplanar slices on the reliability of linear measurements on CBCT images: an in vitro study. J Appl Oral Sci. 2014;23:56–63.
Chen W, Mou H, Qian Y, Qian L. Evaluation of the position and morphology of tongue and hyoid bone in skeletal Class II malocclusion based on cone beam computed tomography. BMC Oral Health. 2021;21(1):1–7.
Jiang Y-Y. Correlation between hyoid bone position and airway dimensions in Chinese adolescents by cone beam computed tomography analysis. Int J Oral Maxillofac Surg. 2016;45(7):914–21.
Yamashita AL, Iwaki Filho L, Leite PCC, de Lima NR, Ramos AL, Previdelli ITS, et al. Three-dimensional analysis of the pharyngeal airway space and hyoid bone position after orthognathic surgery. J Cranio-Maxillofac Surg. 2017;45(9):1408–14.
Vuong L, Kang HK. A cross-sectional retrospective study of normal changes in the pharyngeal airway volume in white children with different skeletal patterns, part 2: cervical vertebral maturation method and hyoid bone. Am J Orthod Dentofac Orthopedics. 2021;159(4):e377–88.
Di Carlo G, Polimeni A, Melsen B, Cattaneo PM. The relationship between upper airways and craniofacial morphology studied in 3D. A CBCT study. Orthod Craniofac Res. 2015;18(1):1–11.
Iwasaki T, Suga H, Yanagisawa-Minami A, Sato H, Sato-Hashiguchi M, Shirazawa Y, et al. Relationships among tongue volume, hyoid position, airway volume and maxillofacial form in paediatric patients with Class-I, Class-II and Class-III malocclusions. Orthod Craniofac Res. 2019;22(1):9–15.
Pandis N. Sample calculations for comparison of 2 means. Am J Orthod Dentofacial Orthop. 2012;141(4):519–21.
Han M, Wang R, Liu H, Zhu X, Wei F, Lv T, et al. Association between mandibular posterior alveolar morphology and growth pattern in a Chinese population with normal occlusion. J Zhejiang Univ Sci B. 2013;14(1):25–32.
Pacheco MCT, Casagrande CF, Teixeira LP, Finck NS, Araújo MTM. Guidelines proposal for clinical recognition of mouth breathing children. Dental Press J Orthod. 2015;20:39–44.
Alves M Jr, Baratieri C, Nojima LI, Nojima MC, Ruellas AC. Three-dimensional assessment of pharyngeal airway in nasal-and mouth-breathing children. Int J Pediatr Otorhinolaryngol. 2011;75(9):1195–9.
Dahlberg G. Statistical methods for medical and biological students. In: Statistical methods for medical and biological students. 1940.
Cuccia AM, Lotti M, Caradonna D. Oral breathing and head posture. Angle Orthod. 2008;78(1):77–82.
Chung Leng Munoz I, Beltri Orta P. Comparison of cephalometric patterns in mouth breathing and nose breathing children. Int J Pediatr Otorhinolaryngol. 2014;78(7):1167–72.
De Grauwe A, Ayaz I, Shujaat S, Dimitrov S, Gbadegbegnon L, Vande Vannet B, et al. CBCT in orthodontics: a systematic review on justification of CBCT in a paediatric population prior to orthodontic treatment. Eur J Orthod. 2019;41(4):381–9.
Kluemper GT, Vig PS, Vig KW. Nasorespiratory characteristics and craniofacial morphology. Eur J Orthod. 1995;17(6):491–5.
Parikh SR, Coronel M, Lee JJ, Brown SM. Validation of a new grading system for endoscopic examination of adenoid hypertrophy. Otolaryngol Head Neck Surg. 2006;135(5):684–7.
Kawashima S, Ueda K, Shinohara M, Mano M, Kanegae H, Namaki S. Relationship between growth of facial morphology and chronologic age in preschool children with obstructive sleep apnea. J Oral Biol Craniofac Res. 2012;2(1):20–4.
Jena AK, Duggal R. Hyoid bone position in subjects with different vertical jaw dysplasias. Angle Orthod. 2011;81(1):81–5.
Sheng C-M, Lin L-H, Su Y, Tsai H-H. Developmental changes in pharyngeal airway depth and hyoid bone position from childhood to young adulthood. Angle Orthod. 2009;79(3):484–90.
Muñoz ICL, Orta PB. Comparison of cephalometric patterns in mouth breathing and nose breathing children. Int J Pediatr Otorhinolaryngol. 2014;78(7):1167–72.
Chaves T, deAndrade e Silva TS, Monteiro SA, Watanabe PC, Oliveira AS, Grossi DB. Craniocervical posture and hyoid bone position in children with mild and moderate asthma and mouth breathing. Int J Pediatr Otorhinolaryngol. 2010;74(9):1021–7.
Behlfelt K, Linder-Aronson S, Neander P. Posture of the head, the hyoid bone, and the tongue in children with and without enlarged tonsils. Eur J Orthod. 1990;12(4):458–67.
Nath M, Ahmed J, Ongole R, Denny C, Shenoy N. CBCT analysis of pharyngeal airway volume and comparison of airway volume among patients with skeletal Class I, Class II, and Class III malocclusion: a retrospective study. CRANIO®. 2021;39(5):379–90.
Janicka A, Halczy-Kowalik L, editors. Hyoid bone position and tongue size and patency of upper airway structures. Annales Academiae Medicae Stetinensis; 2006.
Chang E-T, Shiao G-M. Craniofacial abnormalities in Chinese patients with obstructive and positional sleep apnea. Sleep Med. 2008;9(4):403–10.
Haskell BS, Voor MJ, Roberts AM. A consideration of factors affecting palliative oral appliance effectiveness for obstructive sleep apnea: a scoping review. J Clin Sleep Med. 2021;17(4):833–48.
Baka ZM, Fidanboy M. Pharyngeal airway, hyoid bone, and soft palate changes after Class II treatment with Twin-block and Forsus appliances during the postpeak growth period. Am J Orthod Dentofac Orthop. 2021;159(2):148–57.
Ulusoy C, Canigur Bavbek N, Tuncer BB, Tuncer C, Turkoz C, Gencturk Z. Evaluation of airway dimensions and changes in hyoid bone position following class II functional therapy with activator. Acta Odontol Scand. 2014;72(8):917–25.
Acknowledgements
Not applicable.
Funding
General project from the field of social Development, in Department of Science and Technology of Shaanxi Province, Grant/Award Number: 2019SF-081. Science and Technology Project of Xi 'an, Grant/Award Number: 20YXYJ0010. Clinical New Technology from Stomatological Hospital of Xi’an Jiaotong University in 2018.
Author information
Authors and Affiliations
Contributions
ASM: methodology, data collection, and writing manuscript; JH: statistical analysis, and result interpretation; BC: resources, and interpretation; MZ: statistical analysis; YG: draft review and editing; RZ: Conception; FW: supervision, methodology, draft review and editing, and project administration. All authors reviewed the results and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Stomatological Hospital of Xi’an Jiaotong University, Ethics approval number: Xjkqll [2018] No. 17. All patients' parents or guardians were informed and signed written consent forms to participate in the research. All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Not applicable.
Competing interests
The authors report no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mohamed, A.S., Habumugisha, J., Cheng, B. et al. Three-dimensional evaluation of hyoid bone position in nasal and mouth breathing subjects with skeletal Class I, and Class II. BMC Oral Health 22, 228 (2022). https://doi.org/10.1186/s12903-022-02257-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-022-02257-4