Abstract
Background
Controversial results have been reported regarding the impact of photobiomodulation (PBM) on orthodontically induced inflammatory root resorption (OIIRR). The aim of this study was to evaluate the influence of two PBM protocols, one of them requiring a high application frequency (on days 0, 3, 7, 14, then every 2 weeks), while the second requires less frequent applications (every 3 weeks), on OIIRR accompanying orthodontic treatment.
Methods
Twenty female patients were recruited for this randomized controlled trial, requiring the therapeutic extraction of maxillary first premolars, and they were randomly divided into 2 equal groups. In Group A, one side of the maxillary arch randomly received PBM on days 0, 3, 7, 14, and every 2 weeks thereafter, while in Group B, one side was randomly chosen to receive PBM every 3 weeks. The laser applied was a Diode laser with a wavelength of 980 nm, in a continuous mode. Canine retraction in both groups was carried out using closed-coil springs, delivering 150 g of force, and the force level was checked every 3 weeks, over a 12-week study period. Pre-retraction and post-retraction cone-beam computed tomography (CBCT) was done for the evaluation of OIIRR.
Results
No significant differences in the amount of OIIRR have been reported between the laser and control sides in both groups A and B. Also, no significant differences have been reported between the laser sides in both groups.
Conclusions
Photobiomodulation does not affect OIIRR, whether by increasing or decreasing its occurrence, with both laser application protocols. Therefore, it can be stated that PBM does not result in root resorption less than the commonly observed range elicited with conventional orthodontic treatment, and that it has no effect on OIIRR.
Trial registration Two Low-level Laser Irradiation Protocols on the Rate of Canine Retraction (NCT04926389), 15/06/2021—retrospectively registered. https://clinicaltrials.gov/ct2/show/NCT04926389.
Similar content being viewed by others
Background
Orthodontically induced inflammatory root resorption (OIIRR) is known to be a common iatrogenic outcome of orthodontic treatment. However, despite its relative mildness in most of the cases, it is very frustrating when perceived radiographically. It has been agreed that orthodontic force application brings about a local inflammatory response in the surrounding periodontium, and this inflammation is considered the main reason behind the root resorption process [1]. Several authors proposed that OIIRR could be a side-effect of the cellular response accompanying the elimination of the hyalinized zone of the PDL, and simultaneously the removal of the anti-resorptive cementoid layer [2, 3].
The etiologic or risk factors contributing to OIIRR are multifactorial, caused by a blend of biological factors, in addition to the mechanical characteristics of the employed orthodontic forces [4]. Biological factors include genetic predisposition [5], age [6], root morphology [6], and pre-existing root resorption [7]. Factors related to orthodontic treatment mechanics include the force magnitude [8, 9], the overall treatment duration [10, 11], and the manner of force application [8].
Different procedures have been suggested, aiming to reduce the occurrence of OIIRR, or to potentially repair it. These suggestions included several drugs, such as steroidal and non-steroidal drugs [12], fluoride [13], calcitonin [14], and tetracycline [15]. However, other non-invasive adjuncts that were also clinically suitable, have been proposed for the same purpose, such as Photobiomodulation (PBM) [16, 17].
In contrast to the injected chemicals or the orally ingested drugs, PBM does not generate any systemic consequences, which might influence the general health of the patient [18]. PBM is also known to have a biostimulatory effect when applied to the target tissue areas, characterized by the enhancement of the bone remodelling process [16]. Moreover, as a consequence to the reparative and anti-inflammatory effects of PBM [19], it has been suggested that it may help in the reduction, the prevention, or the repair of root resorption [16, 17, 20, 21]. However, several studies opposed this reported effect for PBM, and according to their results, laser administration had no perceivable effect on OIIRR [22,23,24]. This divergence in the documented outcomes is probably attributed to the different laser application protocols, wavelength, output power, irradiation time, energy density, treatment interval, and so on, making direct comparisons between different studies rather difficult.
Several PBM application protocols have been reported in the literature, and some of them were found to require a high frequency of patient recall which is considered a major downside, such as that involving laser exposures on days 0, 3, 7, 14, and then every 2 weeks [25,26,27]. On the other hand, other protocols have been proposed with laser irradiations performed less frequently, making it more convenient to patients, such as that involving LLLT application every 3 weeks [28,29,30].
Therefore, the purpose of this study was to evaluate the influence of two different PBM protocols on OIIRR accompanying orthodontic tooth movement (OTM), one of them requiring a high laser application frequency (on days 0, 3, 7, 14, and every 2 weeks thereafter), while the second protocol requires less frequent applications (every 3 weeks), and thus less patient recall visits.
Materials and methods
Study design
The study was a randomized controlled clinical trial, involving two parallel groups, each evaluating one of the tested PBM application protocols. Each group employed the split-mouth design, with one side serving as the control group, and the other side serving as the study group.
Study subjects
Twenty female patients requiring the extraction of maxillary first premolars as a part of their orthodontic treatment with subsequent canine retraction have been recruited for the study, with an age range from 15 to 20 years. The sample size was calculated based on an alpha error of 5%, and an 80% study power. This calculation was based on the mean and standard deviation of canine retraction in the study by Doshi-Mehta and Bhad-Patil [31], regarding LLLT application on days 0, 3, 7, 14, and then every 2 weeks (Group A), and those in the study by Qamruddin et al. [28] regarding LLLT application every 3 weeks (Group B). Ethical approval was attained from the Institutional Review Board of the Faculty of Dentistry, Alexandria University, Alexandria, Egypt (IRB: 00010556-IORG: 0008839). Manuscript Ethics Committee number 0111-01/2020. Patient recruitment was done from the outpatient clinic, Department of Orthodontics, Faculty of Dentistry, Alexandria University. Subjects were examined and screened, with the following eligibility criteria being considered: healthy systemic condition with no chronic diseases, no previous orthodontic treatment, adequate oral hygiene, and a healthy periodontium. All patients were informed of the procedure and signed informed consents accordingly. All research procedures were performed in accordance with the relevant guidelines and regulations, as stated in the Declaration of Helsinki.
Patient preparation
The enrolled subjects were prepared for fixed orthodontic treatment by recording their medical and dental history, in addition to taking routine orthodontic records (intra-oral and extra-oral photographs, X-rays, and dental models). Reinforcement of oral hygiene measures was also ensured before the onset of orthodontic treatment. Maxillary and mandibular straight wire fixed Roth appliances were bonded, with 0.022 \(\times\) 0.028 inch slots (Mini 2000; Ormco, USA) in all patients, followed by their referral for maxillary first premolars’ extraction. Leveling and alignment was then started and was considered complete when a 0.016 \(\times\) 0.022 inch stainless steel arch wire could be placed passively in all the maxillary teeth.
Randomization and patient allocation
Before the onset of canine retraction, all 20 patients were randomly assigned to either Group A or Group B (10 in each group), for laser administration. Randomization was done using a simple randomization process with an allocation ratio of 1:1. A box was arranged containing 20 folded pieces of paper, 10 of which had the word “Group A” written on them, while the other 10 papers had the word “Group B”. Each participant was asked to choose one of the folded pieces of paper from the box, and accordingly was assigned to one of the two groups. The same procedure was repeated once again within each group to assign one side of the maxillary arch to be the “study”, with the contralateral side serving as the “control” in the split-mouth design. Canine retraction in groups A and B, on both the experimental and the control sides was performed using nickel-titanium (NiTi) closed-coil springs, stretched between the canine bracket hook and the hook on the molar tube, delivering a force of 150 g as measured by a force gauge. The applied force was checked every 3 weeks, with each follow-up visit. Pre-retraction and post-retraction cone beam computed tomography (CBCT) was performed by all the enrolled subjects.
Laser application
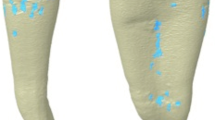
The administered PBM was a Diode laser (Wiser; Doctor Smile-Lambda Spa, Brendola, Italy), emitting infrared radiation at a wavelength of 980 nm, and a power output of 100 mW, in a continuous mode. The plane wave optical fiber (AB 2799; Doctor Smile-Lambda Spa, Brendola, Italy) dispensed a beam spot size of 1 cm2 using the flat top handpiece, and the irradiation was performed on the experimental side by placing the optical fiber tip along the maxillary arch against the middle third of the canine root, where the irradiation would also reach the apical and the cervical thirds. The flat top handpiece was held at a distance of 1.5 cm as minimum on defocalization, as per manufacturer instructions, for 8 s (Fig. 1). The total energy density conducted per episode was 8 J/cm2 (1 J/cm2 per second). Precautions were taken prior to laser application, where both the patient and the operator used protective eyeglasses supplied by the manufacturer, specific for the employed wavelength.
In Group A, subjects received PBM on days 0, 3, 7, 14, and every 2 weeks thereafter, whereas in Group B, PBM was applied every 3 weeks on the experimental sides throughout the study period, which was 12 weeks. The laser beam was also held passively on the control sides of both groups, providing a placebo effect, as a part of the blinding process for the enrolled patients. A research design flowchart is represented in Fig. 2, summarizing the study procedures.
Canine root resorption measurement
Root resorption of the maxillary canines was evaluated and measured on the acquired pre-retraction and post-retraction CBCT scans, that were performed using the same + CBCT machine (J. Morita R100 Cone beam 3D Imaging System; MFG Corp., Kyoto, Japan). The scan was done with a Field of View (FOV) of 100 × 50 mm (Width × Height). The volumes were reconstructed with a 0.160 mm isometric voxel size. Also, the tube voltage was 90 kVp and 8 mA, whereas the exposure time was 20 s.
For the assessment of root resorption, the index suggested by Malmgren et al. [32] was used, where they constructed a classification for the evaluation of root resorption consisting of 5 grades; 0: No root resorption. 1: Mild resorption, normal root length but irregular contour. 2: Moderate resorption, apical root resorption (under 2 mm of the initial root length). 3: Severe resorption, apical root resorption (2 mm to one third of the initial root length). 4: Extreme resorption (exceeding one third of the root length).
Using the software OnDemand3DTM (Cybermed Inc., South Korea), the pre- and post-retraction CBCTs obtained for each of the enrolled patients were utilized to assess the effect of the suggested two PBM protocols on canine root resorption, as follows:
-
1.
The maxillary canines on the right and left sides were individually assessed in each CBCT.
-
2.
Utilizing the arch section module, the focal trough was adjusted twice for each canine (Fig. 3). The first adjustment was to permit the labiolingual slicing/sectioning of the canine parallel to the long axis of its root (Fig. 4), whereas the second adjustment was to enable the mesiodistal slicing/sectioning of the canine, also parallel to the long axis of its root (Fig. 5). The least slice thickness interval was chosen, which was 0.1 mm.
-
3.
The two perpendicular cross-sections showing the maximum length of the canine root were then selected for assessment using Malmgren index [32].
-
4.
The right and left maxillary canines in each patient were operated upon as previously described, and each canine was given two scores from (0–4) in accordance with the degree of root resorption detected from the labiolingual as well as the mesiodistal cross-sections. These steps were performed for the pre- and post-retraction CBCTs.
-
5.
The pre- and post-retraction scores for each canine were measured and evaluated statistically. The clinician was blinded to the experimental and control sides during measurement to avoid unwarranted bias. Measurements were also repeated by the same person one week later to check if there were measurement errors. Calibration of the root resorption measurements was performed, and intra-examiner reliability was calculated (Kappa = 0.96) [33], indicating excellent reliability.
Statistical analysis
Frequencies and percentages were calculated for the root resorption scores. Comparisons of root resorption pre- and post-retraction scores between the two study groups were done using Mann–Whitney U test, while comparisons between the laser and control sides were done using Wilcoxon signed rank test. Comparisons between the root resorption scores pre- and post-retraction, within each group, were done using Wilcoxon signed rank test. Significance was set at p value < 0.05. Data were analyzed using IBM SPSS for Windows version 23.0 (IBM; Armonk, NY, USA).
Results
Over the course of the study, there were no subject dropouts in the pre-intervention period, nor throughout the rest of the study. All the twenty initially recruited subjects completed the entire 12-week study period (10 subjects per group). Also, all the required CBCTs whether pre-retraction or post-retraction were accounted for. Demographic data and clinical characteristics of the enrolled subjects in both groups A and B, are presented in Table 1.
The effect of PBM on OIIRR
Root resorption scores of the maxillary canines in groups A and B, on both the laser and control sides, are presented in Table 2. The roots of the maxillary canines were given scores according to Malmgren index as previously explained. In Group A, no changes in the pre-retraction and post-retraction root resorption scores have been recorded on the laser side. As for the control side, no patients were given a score of 2 in the pre-retraction records, but in the post-retraction numbers, two subjects were given a score of 2, comprising 20% of the group sample. However, this percentage change was not statistically significant.
In Group B, on the laser side, two patients were given a score of 1 in the pre-retraction measurements, comprising 20% of the group sample, but in the post-retraction records three patients were given a score of 1, thus accounting for 30% of the group sample. However, this change was insignificant statistically. For the control side, two patients were given a score of 1 pre-retraction (20% of the sample), while three patients were scored 1 in the post-retraction scores, accounting for 30% of the study sample, nevertheless this change was not statistically significant. Furthermore, no patients were given the score 2 in the pre-retraction measurements, yet one patient was given a score of 2 in the post-retraction records, representing 10% of the study sample, but this change also was not significant.
Comparison between the root resorption scores on the laser sides in groups A and B
The difference in the canine root resorption pre- and post-retraction scores, on the laser sides of both groups A and B, is represented in Fig. 6. Between both study groups, no statistically significant differences have been recorded. In Group A, the laser side did not demonstrate any changes regarding the root resorption scores, pre- and post-retraction. As for Group B, a change of 10% was noted, where only two patients were given a score of 1 pre-retraction, and this changed to three patients with a score of 1 in the post-retraction records, which was an insignificant difference.
Discussion
The aim of this study was to compare the effect of PBM on the OIIRR, using both the high frequency application protocol where laser has been applied on days 0, 3, 7, 14, and every 2 weeks thereafter (Group A), and the protocol with less patient recall, where laser application has been done at 3-week intervals (Group B). Both protocols have been documented in the literature [25, 26, 28, 30].
The current study design was a clinical randomized controlled trial (RCT). RCTs are contemplated as the gold standard for the evaluation of intervention efficacy [34]. The split-mouth technique also has been implemented, with its main advantage being the elimination of the inter-subject variability, as the patient acts and his/her own control, thus reducing the number of participants required.
One of the crucial factors influencing the therapeutic and biostimulatory effect of PBM is the dosage or energy density. In the current study, an energy density of 8 J/cm2 has been used, which is similar to that employed by Yousry et al. [35], as well as Goymen and Gulec [24]. By reviewing the literature, a wide range of energy density values have been documented with laser administration, where several authors used lower energy doses such as 3.6 J/cm2 [22], and 4.8 J/cm2 [16, 21], and others used higher doses such as 54 J/cm2 [36], and 75 J/cm2 [20]. In the present work, the administered laser energy dose was 8 J/cm2, delivered through a single application of 8 s against the maxillary canine root, dispensing a beam spot size of 1 cm2 using the flat top handpiece. A direct correlation has been documented between the beam size and the laser penetration depth, which in turn justifies the use of the flat top handpiece in this study [37, 38]. The same single application protocol with a large beam spot size was performed by Caccianiga et al. [39], and Abd El-Ghafour et al. [40].
The laser type employed in this study was a Diode laser semiconductor (Doctor Smile-Lambda Spa, Italy), used at a wavelength of 980 nm, as per manufacturer recommendation, in order to obtain the desirable bio-stimulatory effect. Generally, in the ultraviolet (UV) to the near infrared (IR) spectrum, the shorter wavelengths (200–600 nm) have more superficial penetration, in contrast to the longer absorption wavelengths (650–1200 nm) that have deeper tissue penetration [37]. The least penetrating wavelengths are in the far UV (excimer) and in the far IR (CO2) spectra, due to their high affinity to water [37]. Moreover, wavelengths in the 600–700 nm range are usually chosen for treating superficial tissues [41], whereas diode lasers in the near infrared ranges (810–980 nm) are selected for deeper-seated tissues, due to their longer optical penetration distances through the target tissues [41,42,43]. It has been also found that the near infrared diode lasers routinely used in dentistry, can reach a penetration depth of 4–5 mm into the target tissues, due to their poor absorption by water [43]. The 980 nm wavelength employed in the current study, has been used in several other studies where its biostimulatory effect has been advocated, such as that by Yassin et al. [21], where it has been reported that laser application can be effective in preventing, reducing, and repairing OIIRR. Also, in the study by Caccianiga et al. [39], the same laser device as that employed in our trial has been used, with the same 980 nm wavelength, and positive biostimulation has been reported. Effective biostimulation with the 980 nm wavelength has been also reported by Jivrajani and Bhad-Patil [44], as well as Abtahi et al. [45].
CBCT images were mandatory to investigate the effect of PBM on root resorption, thus pre- and post-retraction CBCTs (12-week interval) were performed by the patients enlisted in the study. Regarding CBCT measurements, high intra-observer and inter-observer reliability have been endorsed by El-Beialy et al. [46], and Tarazona-Àlvarez et al. [47]. Also, in comparison to periapical and panoramic X-rays, CBCT images have shown superior diagnostic precision in the detection of root resorption [48, 49]. Moreover, Malmgren index [32] was selected as a reliable scoring system for the assessment of root resorption. This assessment protocol has been adopted by other authors, such as Nimeri et al. [50], and Aboalnaga et al. [51].
Regarding the influence of PBM on OIIRR, according to the results of this study, no significant differences have been registered between the laser and control sides in both Group A and Group B. On comparing the root resorption values between the laser sides in both groups, using the different application protocols, also no significant differences have been reported. Therefore, it can be stated that according to our study results, PBM did not result in root resorption less than the commonly observed range, elicited with conventional orthodontic treatment, and that it has no effect on OIIRR.
However, controversial effects have been documented in the existent literature, regarding the impact of PBM on OIIRR. Similar results to those reported in the current study have been documented by Yousry et al. [35], and by Goymen and Gulec [24], and their results can be comparable to those of our study since they both also used an energy density of 8 J/cm2. Contrastingly, some researchers advocated the beneficial effects of employing PBM with OTM in reducing the expected associated root resorption, such as Ng et al. [52]. In the investigation by Ng et al. [52], four point laser irradiations have been conducted over the entire root length, starting from the root apex, followed by the middle centre of the root, and finally reaching the cervical third (on the mesial and distal sides), whereas in our study, the flat top handpiece was only held against the mid-root of the maxillary canine. The flat top handpiece employed in our study dispensed a large beam size of 1 cm2, and by holding it against the middle third of the root, the irradiation should reach the apical as well as the cervical parts. However, the apical third of the root did not receive direct laser irradiation, and this might explain the lack of a preventive or a reparative effect for PBM on OIIRR in the current study. Nevertheless, till now, the influence of PBM on root resorption is a rather disputable issue [53,54,55].
Conclusions
With the parameters employed in this study, photobiomodulation does not affect orthodontically induced inflammatory root resorption, whether by increasing or decreasing its occurrence, with both laser application protocols. Therefore, it can be stated that PBM does not result in root resorption less than the commonly observed range elicited with conventional orthodontic treatment, and that it has no effect on OIIRR.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bosshardt D, Masseredjian V, Nanci A. Root resorption and tissue repair in orthodontically treated human premolars. Biological mechanisms of tooth eruption, resorption and replacement by implants. Boston: Harvard Society for the Advancement of Orthodontics; 1998. p. 425–37.
Rygh P. Orthodontic root resorption studied by electron microscopy. Angle Orthod. 1977;47:1–16.
Brudvik P, Rygh P. The initial phase of orthodontic root resorption incident to local compression of the periodontal ligament. Eur J Orthod. 1993;15:249–63.
Lopatiene K, Dumbravaite A. Risk factors of root resorption after orthodontic treatment. Stomatologija. 2008;10:89–95.
Hartsfield J Jr, Everett ET, Al-Qawasmi R. Genetic factors in external apical root resorption and orthodontic treatment. Crit Rev Oral Biol Med. 2004;15:115–22.
Brezniak N, Wasserstein A. Root resorption after orthodontic treatment: part 2. Literature review. Am J Orthod Dentofacial Orthop. 1993;103:138–46.
Nigul K, Jagomagi T. Factors related to apical root resorption of maxillary incisors in orthodontic patients. Stomatologija. 2006;8:76–9.
Casa MA, Faltin RM, Faltin K, Arana-Chavez VE. Root resorption on torqued human premolars shown by tartrate-resistant acid phosphatase histochemistry and transmission electron microscopy. Angle Orthod. 2006;76:1015–21.
Paetyangkul A, Türk T, Elekdağ-Türk S, Jones AS, Petocz P, Cheng LL, et al. Physical properties of root cementum: part 16. Comparisons of root resorption and resorption craters after the application of light and heavy continuous and controlled orthodontic forces for 4, 8, and 12 weeks. Am J Orthod Dentofacial Orthop. 2011;139:e279–84.
Roscoe MG, Meira JB, Cattaneo PM. Association of orthodontic force system and root resorption: a systematic review. Am J Orthod Dentofacial Orthop. 2015;147:610–26.
Weltman B, Vig KW, Fields HW, Shanker S, Kaizar EE. Root resorption associated with orthodontic tooth movement: a systematic review. Am J Orthod Dentofacial Orthop. 2010;137:462–76.
Gonzales C, Hotokezaka H, Matsuo K-I, Shibazaki T, Yozgatian JH, Darendeliler MA, et al. Effects of steroidal and nonsteroidal drugs on tooth movement and root resorption in the rat molar. Angle Orthod. 2009;79:715–26.
Gonzales C, Hotokezaka H, Karadeniz EI, Miyazaki T, Kobayashi E, Darendeliler MA, et al. Effects of fluoride intake on orthodontic tooth movement and orthodontically induced root resorption. Am J Orthod Dentofacial Orthop. 2011;139:196–205.
Guan L, Lin S, Yan W, Chen L, Wang X. Effects of calcitonin on orthodontic tooth movement and associated root resorption in rats. Acta Odontol Scand. 2017;75:595–602.
Baysal A, Uysal T, Ozdamar S, Kurt B, Kurt G, Gunhan O. Comparisons of the effects of systemic administration of l-thyroxine and doxycycline on orthodontically induced root resorption in rats. Eur J Orthod. 2010;32:496–504.
Altan AB, Bicakci AA, Mutaf HI, Ozkut M, Inan VS. The effects of low-level laser therapy on orthodontically induced root resorption. Lasers Med Sci. 2015;30:2067–76.
Suzuki SS, Garcez AS, Suzuki H, Ervolino E, Moon W, Ribeiro MS. Low-level laser therapy stimulates bone metabolism and inhibits root resorption during tooth movement in a rodent model. J Biophotonics. 2016;9:1222–35.
Seifi M, Atri F, Yazdani MM. Effects of low-level laser therapy on orthodontic tooth movement and root resorption after artificial socket preservation. Dent Res J. 2014;11:61.
Fonseca PDA, de Lima FM, Higashi DT, Koyama DFV, de Oliveira Toginho Filho D, Dias IFL, et al. Effects of light emitting diode (LED) therapy at 940 nm on inflammatory root resorption in rats. Lasers Med Sci. 2013;28:49–55.
de Melo CC, Suzuki H, Garcez AS, Suzuki SS. Effects of photobiomodulation on root resorption induced by orthodontic tooth movement and RANKL/OPG expression in rats. Photochem Photobiol. 2019;95:1249–57.
Yassin AM, Shehata FI, Al-Sawa AA, Karam SS. Effect of low-level laser therapy on orthodontic induced inflamatory root resorption in rats. Alex Dent J. 2020;45:62–7.
Khaw CMA, Dalci O, Foley M, Petocz P, Darendeliler MA, Papadopoulou AK. Physical properties of root cementum: part 27. Effect of low-level laser therapy on the repair of orthodontically induced inflammatory root resorption: a double-blind, split-mouth, randomized controlled clinical trial. Am J Orthod Dentofacial Orthop. 2018;154:326–36.
Vasconcelos EC, Henriques JFC, Sousa MVS, de Oliveira RC, Consolaro A, Pinzan A, et al. Low-level laser action on orthodontically induced root resorption: histological and histomorphometric evaluation. J Lasers Med Sci. 2016;7:146–51.
Goymen M, Gulec A. Effect of photobiomodulation therapies on the root resorption associated with orthodontic forces: a pilot study using micro computed tomography. Clin Oral Investig. 2020;24:1431–8.
Isola G, Matarese M, Briguglio F, Grassia V, Picciolo G, Fiorillo L, et al. Effectiveness of low-level laser therapy during tooth movement: a randomized clinical trial. Materials (Basel). 2019;12:2187.
Lalnunpuii H, Batra P, Sharma K, Srivastava A, Raghavan S. Comparison of rate of orthodontic tooth movement in adolescent patients undergoing treatment by first bicuspid extraction and en-mass retraction, associated with low level laser therapy in passive self-ligating and conventional brackets: a randomized controlled trial. Int Orthod. 2020;18:412–23.
Abdelhameed AN, Refai WMM. Evaluation of the effect of combined low energy laser application and micro-osteoperforations versus the effect of application of each technique separately on the rate of orthodontic tooth movement. Open Access Maced J Med Sci. 2018;6:2180–5.
Qamruddin I, Alam MK, Mahroof V, Fida M, Khamis MF, Husein A. Effects of low-level laser irradiation on the rate of orthodontic tooth movement and associated pain with self-ligating brackets. Am J Orthod Dentofacial Orthop. 2017;152:622–30.
Qamruddin I, Alam MK, Mahroof V, Fida M, Khamis MF, Husein A. Photobiostimulatory effect of a single dose of low-level laser on orthodontic tooth movement and pain. Pain Res Manag. 2021;2021:6690542.
Garg NJ, Singh G, Kannan S, Rai D, Kaul A, Gupta A, et al. Effect of 810 nm diode laser therapy on the rate of extraction space closure. J Indian Orthod Soc. 2014;48:143–8.
Doshi-Mehta G, Bhad-Patil WA. Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofacial Orthop. 2012;141:289–97.
Malmgren O, Goldson L, Hill C, Orwin A, Petrini L, Lundberg M. Root resorption after orthodontic treatment of traumatized teeth. Am J Orthod. 1982;82:487–91.
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med. 2012;22:276–82.
Stang A. Randomized controlled trials—an indispensible part of clinical research. Dtsch Ärztebl Int. 2011;108:661–2.
Yousry T, El-Harouni N, Enany N. Effect of low level laser on root resorption with en masse maxillary anterior retraction: a randomized clinical trial. Egypt Orthod J. 2015;48:23–36.
Keklikci HB, Yagci A. Effects of different wavelengths of low-level laser therapy on orthodontically induced inflammatory root resorption in rats investigated with micro-computerized tomography. Am J Orthod Dentofacial Orthop. 2021;159:e245–51.
Farkas JP, Hoopman JE, Kenkel JM. Five parameters you must understand to master control of your laser/light-based devices. Aesthet Surg J. 2013;33:1059–64.
Ash C, Dubec M, Donne K, Bashford T. Effect of wavelength and beam width on penetration in light-tissue interaction using computational methods. Lasers Med Sci. 2017;32:1909–18.
Caccianiga G, Paiusco A, Perillo L, Nucera R, Pinsino A, Maddalone M, et al. Does low-level laser therapy enhance the efficiency of orthodontic dental alignment? Results from a randomized pilot study. Photomed Laser Surg. 2017;35:421–6.
Abd El-Ghafour M, El-Ashmawi NA, El-Beialy AR, Fayed MMS, Hussein F. Effect of low level laser therapy on the rate of canine retraction in orthodontic patients: a split-mouth randomized controlled trial. Orthod Pract. 2017;8:18–24.
Coluzzi DJ, Parker SP. Lasers in dentistry—current concepts. Berlin: Springer; 2017.
Desiate A, Cantore S, Tullo D, Profeta G, Grassi FR, Ballini A. 980 nm diode lasers in oral and facial practice: current state of the science and art. Int J Med Sci. 2009;6:358–64.
Fornaini C, Merigo E, Sozzi M, Rocca J-P, Poli F, Selleri S, et al. Four different diode lasers comparison on soft tissues surgery: a preliminary ex vivo study. Laser Ther. 2016;25:105–14.
Jivrajani SJ, Bhad WA. Effect of low intensity laser therapy (LILT) on MMP-9 expression in gingival crevicular fluid and rate of orthodontic tooth movement in patients undergoing canine retraction: a randomized controlled trial. Int Orthod. 2020;18:330–9.
Abtahi M, Saghravanian N, Poosti M, Shafaee H. Histological evaluation of orthodontic tooth movement following low level laser irradiation in rabbits. Electron Phys. 2018;10:6219–22.
El-Beialy AR, Fayed MS, El-Bialy AM, Mostafa YA. Accuracy and reliability of cone-beam computed tomography measurements: influence of head orientation. Am J Orthod Dentofacial Orthop. 2011;140:157–65.
Tarazona-Álvarez P, Romero-Millán J, Peñarrocha-Oltra D, Fuster-Torres MÁ, Tarazona B, Peñarrocha-Diago M. Comparative study of mandibular linear measurements obtained by cone beam computed tomography and digital calipers. J Clin Exp Dent. 2014;6:e271–4.
Dudic A, Giannopoulou C, Leuzinger M, Kiliaridis S. Detection of apical root resorption after orthodontic treatment by using panoramic radiography and cone-beam computed tomography of super-high resolution. Am J Orthod Dentofacial Orthop. 2009;135:434–7.
Yi J, Sun Y, Li Y, Li C, Li X, Zhao Z. Cone-beam computed tomography versus periapical radiograph for diagnosing external root resorption: a systematic review and meta-analysis. Angle Orthod. 2017;87:328–37.
Nimeri G, Kau CH, Corona R, Shelly J. The effect of photobiomodulation on root resorption during orthodontic treatment. Clin Cosmet Investig Dent. 2014;6:1–8.
Aboalnaga AA, Fayed MMS, El-Ashmawi NA, Soliman SA. Effect of micro-osteoperforation on the rate of canine retraction: a split-mouth randomized controlled trial. Prog Orthod. 2019;20:1–9.
Ng D, Chan AK, Papadopoulou AK, Dalci O, Petocz P, Darendeliler MA. The effect of low-level laser therapy on orthodontically induced root resorption: a pilot double blind randomized controlled trial. Eur J Orthod. 2018;40:317–25.
Michelogiannakis D, Al-Shammery D, Akram Z, Rossouw PE, Javed F, Romanos GE. Influence of low-level laser therapy on orthodontically-induced inflammatory root resorption. A systematic review Arch Oral Biol. 2019;100:1–13.
Nayyer N, Tripathi T, Rai P, Gopal R. Effect of photobiomodulation on external root resorption during orthodontic tooth movement—a scoping review. Lasers Dent Sci. 2019;3:219–26.
Shin K. No clear evidence for the effect of low-level laser treatment on orthodontically induced inflammatory root resorption: more human clinical studies are needed. J Evid Based Dent Pract. 2020;20: 101463.
Acknowledgements
Not applicable.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This study received no external fund from any institute or authority.
Author information
Authors and Affiliations
Contributions
FE: conceptualization, performing all the clinical procedures, data curation, writing preparing the original manuscript, visualization, and investigation. WE: supervision, conceptualization, revising the written manuscript, and helping in drawing out the final study conclusions. MM: supervision of the clinical procedures, reviewing and editing, aiding in the analysis and interpretation of the obtained results. AE: supervision of the clinical procedures, reviewing and editing, aiding in the analysis and interpretation of the obtained results, and drawing the final conclusions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board at the Faculty of Dentistry, Alexandria University (IRB: 00010556-IORG: 0008839). All CBCT scans had a patient-waiver consenting for the use of records for diagnostic and research purposes. All patients were informed of the procedure and signed informed consents accordingly. All research procedures were performed in accordance with the Declaration of Helsinki.
Consent for publication
Written informed consents were signed by patients whose scans were used in the study for publication purposes.
Competing interests
The authors declare that they have no competing interests as defined by BMC Oral Health, or other interests that might be perceived to influence the results and/or discussion reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Eid, F.Y., El-Kenany, W.A., Mowafy, M.I. et al. The influence of two photobiomodulation protocols on orthodontically induced inflammatory root resorption (a randomized controlled clinical trial). BMC Oral Health 22, 221 (2022). https://doi.org/10.1186/s12903-022-02251-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-022-02251-w