Abstract
Background
After reparation of root perforations with calcium silicate-based cements (CSBC), the surface of the material is expected to be exposed to root canal irrigants (RCI) while resuming the root canal treatment.
Methods
The aim of this study was to compare the effect of exposure to a mixture of sodium hypochlorite (NaOCl) and etidronic acid (HEBP) or other irrigants on the Push Out Bond Strength (POBS) of CSBC after two different setting times. 240 root slices 1 mm thick were obtained from single-rooted human teeth. A 1.4 mm diameter perforation was performed on each slice and filled with Biodentine (BD) or ProRoot MTA (PMTA). After 1 or 21 days they were exposed to 17% ethylenediaminetetraacetic acid, 5.25% NaOCl, a mixture of 5.25% NaOCl and 9% HEBP (NaOCl + HEBP) or saline (n = 15) and submitted to a push-out test. POBS results were analysed with ANOVA and Tukey tests.
Results
BD showed higher POBS than PMTA after 1 day (p < .05). After 21 days no differences were found between materials. After 1 day exposure to NaOCl + HEBP resulted in higher POBS, compared to the other irrigants (p < .05).
Conclusion
POBS results are influenced by the cement, the setting time and the exposure to irrigants.
Similar content being viewed by others
Background
Immediate root perforation repair is critical to avoid the contamination of the periodontal ligament, or the extrusion of root canal irrigants (RCI) [1] or root canal filling materials, which could cause an endodontic-periodontal lesion through damage to the epithelial attachment and bone loss [2]. For this reason, it is recommended to repair the perforation even before performing the root canal treatment [3].
An ideal repair material should, amongst other requirements, provide a suitable seal and have an adequate resistance to dislodgement under pressure caused by condensation forces applied to the restorative materials placed above it, or by occlusion loads [4].
Calcium silicate-based cements (CSBC) are commonly used to repair perforations [3, 5]. Mineral trioxide aggregate (MTA), and in particular ProRoot MTA (PMTA; Dentsply-Sirona, Ballaigues, Switzerland), was the first CSBC developed. Despite its widespread use, several drawbacks have been attributed to this cement, such as an extended setting time or discoloration of the tooth, among others [6]. To overcome these limitations, other materials have been developed. Biodentine (BD; Septodont, Saint-Maur-des-Fossés, France) is a CSBC that has shown a good performance in vitro and in vivo due to its biocompatibility, lower risk of tooth discoloration, shorter setting time and a similar ability to promote periradicular bone healing compared with PMTA [7,8,9]. The improved properties of BD in comparison to PMTA have been attributed to the differences in the composition of the two materials. The presence of bismuth oxide as a radiopacifier in MTA causes dentinal staining due to the reaction with collagen present in the organic dentin matrix [10] and it has also been reported to actively take part in the hydration reaction [11]. To prevent this problem, an inert component, zirconium oxide, has been added as a radiopacifier in BD [12, 13]. The PMTA powder is mixed with distilled water whereas the Biodentine liquid consists of an aqueous solution of calcium chloride (CaCl2), which acts as an accelerator of the hardening process, and a hydrosoluble polymer (water reducing agent) that allows good flowability with a low water/powder ratio [12, 14]. All these differences in the composition of the two cements may have an influence in their chemical reaction with other substances and, subsequently, in their physical properties.
After sealing the perforation, during cleaning and shaping of the root canal, the surface of the repairing material is expected to be exposed to different RCI, such as sodium hypochlorite (NaOCl), ethylenediaminetetraacetic acid (EDTA), or the recently introduced etidronic acid (also known as 1-hydroxyethylidene-1, 1-bisphosphonate, HEBP). HEBP is a biocompatible chelator that can be used in combination with NaOCl while maintaining the properties of both compounds [15]. Dual Rinse HEDP (MedCem, Vienna, Austria) has been developed as a HEBP powder to be mixed with sodium hypochlorite, which creates a stable solution to be used during the whole root canal treatment as a single irrigant [16, 17].
It has been established that contact with different RCI during setting time may influence the push-out bond strength (POBS) of CSBC [18,19,20], and this has been attributed to a variety of factors related to the compositions of the cements, or the properties of the RCI [19,20,21]. A number of studies have reported the deleterious effect of certain chelating agents on the properties of CSBC, and have attributed this to the interference of these substances with the setting reaction of the cements and with their chemical adhesion to dentine [19, 22,23,24]. However, until now, it has not been well established whether the exposure to the NaOCl + HEBP solution may affect the POBS. To our knowledge, only one study has recently tested the effect of exposure to NaOCl + HEBP on the POBS of several CSBC after 7 days of setting, concluding that after exposure to NaOCl + HEBP, BD obtained higher POBS values than with other RCI [25]. In addition, it has been observed that the POBS results of CSBC are conditioned by the time during which the cement is allowed to set before performing the pushout test [4, 26]. This influence of time may differ among cements as their setting times have been shown to be different [7]. Therefore, the clinical outcome of root perforations may be affected by the composition of the repairing materials, the properties of the RCI to which they are exposed during root canal treatment and the time elapsed between the placement of the material and the exposure.
The purpose of this study is to compare the effect of EDTA, NaOCl and NaOCl + HEBP on POBS of PMTA and BD in simulated root perforations after two different setting times (1 or 21 days). The following null hypotheses were tested:
-
There is no difference in the POBS between cements, after exposure to different RCI or after different setting times.
-
There is no difference in the failure pattern distribution among subgroups.
Methods
Specimen preparation
A total of 240 single-rooted freshly extracted human teeth were selected to be included in this study. All of them were evaluated by radiograph and under 10 × magnification (Leica MZ12 Leica Microsystem, Wetzlar, Germany). The selected teeth had single, non-calcified canals, and absence of radicular caries, resorptions or visible cracks. The soft tissue and the calcified debris of the radicular surface were removed with a manual scaler and then the teeth were stored in saline solution (0.9% Sodium Chloride Injection USP, B. Braun Medical S.A., Rubí, Barcelona, Spain) at 4ºC until further preparation.
All the specimens were prepared as previously described [4, 25]. Shortly after the removal of the crown, a slice of 1 mm thickness was cut from the coronal end of every root. In the centre of the slice, a circular perforation of 1.4 mm diameter was drilled with a cylindrical diamond bur (Kerr C837-014, Bioggio, Switzerland). The slices were inserted into a circular metal frame, securing them through their perforation to a stem located in the centre of the frame to be embedded in resin (Activated Chronolite 1019, Plastiform, Cronolab, Madrid, Spain) (Fig. 1a). Once the resin had cured, the created specimens were extracted from the frames (Fig. 1b), obtaining cylindrical pieces with the tooth slice surrounded by chronolite, with the upper surface uncovered, and a lower perforation in the axis of the resin cylinder of 2.5 mm diameter and 5 mm height, aligned with the perforation of the root slice.
Sample preparation and POBS device. a Circular steel frame with a stem (1) to centre the dentin disc. b Schematic view of a specimen, consisting of a resin cylinder with the tooth slice on the upper surface and with the perforation centred and aligned with the axis. c Lateral view of the specimen with a metal cylinder (2) to prevent extrusion while filling the perforation. d Specimen with perforation filled with CSBC and covered with the RCI (3). e POBS device 4: upper piece holding the cylindrical punch (5), 6: lower piece—specimen holder, 7: cover, 8: hole to centre the punch during the test). f POBS device located in the testing machine (9: alignment device)
Experimental groups
The specimens were randomly divided into 2 groups (n = 120), according to the repairing material used to fill the perforation: BD or PMTA. The cements were used following manufacturers’ instructions and placed inside the perforation of the specimens. To prevent the extrusion of the material, below the lower surface of the tooth a 2.5 mm diameter steel cylinder was inserted inside the lower perforation of the specimen (Fig. 1c). The excess material was removed from the upper surface with a scalpel. The specimens in each group were further divided into 2 subgroups according to the different setting times: 1 day, or 21 days. During setting, the specimens were stored at 37ºC and 95% humidity. Afterwards, the specimens were randomly divided to be exposed to 17% EDTA (EDTA, ENDO-SOLution, Cerkamed, Stalowa Wola, Poland), to 5.25% NaOCl (NaOCl, Chloraxid 5.25%, Cerkamed, Stalowa Wola, Poland), to a mixture of 5.25% NaOCl and 9% HEBP (NaOCl + HEBP, Dual Rinse HEDP) or remain stored in contact with a gauze wrapped in saline. An amount of 0.2 ml of RCI was applied on the coronal surface of the repairing material. The RCI was discarded and renewed every 5 min until the exposure time of 30 min was completed (Fig. 1d). The exposure time for EDTA was 5 min, and therefore no renewal was needed. In all, with this experimental design, we obtained a total of 16 groups (n = 15), based on the CSBC, the setting time and the RCI used. (See Table 1, in the results section).
Push out bond strength test
The specimens were attached to an aligning device that held them centred below a 1.2 mm diameter cylindrical stainless-steel punch (Fig. 1e, f). Using a universal material testing machine (Hounsfield H-5000 M, Metrotec, Lezo, Spain), the punch was moved towards the repairing material at a constant crosshead speed of 1 mm/min. The maximal force (F) needed for the punch to dislodge the material was registered in Newtons, and the POBS was calculated in Megapascals using the following formula: POBS (MPa) = F(N) / S(mm2), where S is the contact surface between dentin and material, obtained as follows: S = 2 × r (mm) × π × h (mm) (where r is the radius of the perforation, π is the constant 3.14, and h is the thickness of the slice).
Failure pattern analysis
The samples were assessed under 40 × magnification to record the pattern of failure: adhesive (between dentin and cement), cohesive (within the cement) or mixed failure (both patterns).
Statistical analysis
For the POBS data, three-way ANOVA was used to detect interactions amongst the three independent factors (cement, setting time and exposure to RCI). Afterwards, the CSBC were compared and studied separately at each setting time, to explore the effect of the different RCI with one-way ANOVA. All the analyses were followed by applying Tukey’s multiple comparisons test. The failure patterns were analysed using a Chi-square test. The level of statistical significance was set at 0.05.
Results
During the experimental process, 3 of the 240 specimens were discarded (PMTA-Saline-1D, BD-EDTA-1D and BD-Saline-21D groups) due to the friction of the punch against the dentin wall caused by an error in the location of the dentin slice in the aligning device.
The mean and standard deviation (SD) values (in MPa) of all experimental groups are shown in Table 1. Three-way ANOVA revealed that the POBS was significantly affected by cements (p < 0.001), setting time (p < 0.001) and exposure to RCI (p < 0.001). All double interactions were statistically significant (p < 0.001 for cement*setting time and cement*exposure to RCI, and p = 0.005 for setting time*exposure to RCI). BD showed higher POBS than PMTA after 1 day (p < 0.001). At 21 days, no differences were found between these cements. There were no statistically significant differences in BD POBS between 1 and 21 days of setting while PMTA showed higher POBS values after 21 days than after 1 day (p < 0.001). When separately analysing the effect of exposure to RCI on BD and PMTA after the two setting times, both BD and PMTA obtained higher POBS values when exposed to NaOCl + HEBP, compared to the other RCI after 1 day of setting (p < 0.001). No statistically significant differences among RCI were detected at 21 days for both BD and PMTA (Fig. 2).
Bar Graph showing the mean POBS in MPa of each experimental subgroup. Error lines are calculated with a 95% confidence interval. BD, Biodentine; PMTA, ProRoot MTA; EDTA, Ethylenediaminetetraacetic acid; NaOCl, Sodium hypochlorite; HEBP, Etidronic Acid. Significant differences are represented as resulted from the Three-way ANOVA test among setting times (*), cements (**) and root canal irrigants (***)
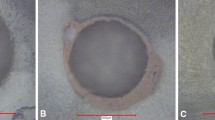
The total distribution of the different failure patterns in all the specimens was as follows: 35.4% cohesive, 38.8% mixed and 25.7% adhesive. A Chi-square test revealed no differences in the distribution of failure patterns among groups. The count and percentage of all the experimental groups are presented in Table 2. Examples of different failure patterns are shown in Fig. 3.
Representative stereomicroscope views at × 40 showing the different failure patterns. Cohesive failures in samples of BD-1 day-saline (a.1) and PMTA-21 days-NaOCl (a.2) groups; Mixed failures in samples of PMTA-1 day-NaOCl + HEBP (b.1) and BD-21 days-EDTA (b.2) groups; Adhesive failures in samples of BD-21 days-saline (c.1) and PMTA-1 day-NaOCl (c.2) groups
Discussion
This research has reproduced the most frequently used parameters in POBS studies (i.e. the thickness of the slice, the size of the perforation or the incubation conditions of the specimens) with the aim of avoiding bias and allowing direct comparisons of the results among studies [27]. In order to create an accurate anatomical reproduction, Nagas et al. used a furcal perforation model [28], given that many of these perforations occur at the furcal level. Another design has been proposed to increase the reliability of the pushout test, which consists in placing different materials in perforations performed in the same dentin slice, to avoid the influence of individual variables of each tooth [29]. However, the use of radicular coronal third slices of uniradicular teeth with a single centred perforation may provide a more reproducible model and a more comparable situation among the tested materials. Decentred perforations may cause exposure to the tubules at different angles along the perimeter, which may have an influence on the penetration of CSBC in the dentinal tubules. Performance of the perforation centred in the root canal provides a homogeneous exposure of the dentinal tubules around the whole perimeter of the perforation.
Two setting times were established in order to compare the effect of RCI on the POBS values at different moments during the hydration process. The 21-day period of setting was selected to allow the complete maturation before testing, based on the results of a previously published research. In that study an increase in POBS of PMTA was observed between 1 and 21 days of setting when kept under wet conditions, suggesting a prolonged hydration process of this material [4].
Since our goal was to evaluate the effect of the tested irrigants on the POBS of repairing materials used to seal root perforations in simulated clinical conditions, exposure to the RCI was performed once the CSBC were placed in the perforation sites, instead of previously treating the dentin and then filling the perforations. Moreover, to extrapolate the results to clinical practice, the specimens were exposed to the RCI only on one side as previously described in the literature [30]. The exposure time for NaOCl was 30 min based on average reported clinical time of root canal preparation [18, 31]. A solution of 5.25% NaOCl was chosen for being one of the most commonly used in the clinical practice given that high concentrations have shown to be superior in terms of disinfection when compared to lower concentrations such as 1 or 2% [32, 33]. For NaOCl + HEBP the same exposure time as NaOCl was used as the authors that tested the properties of HEBP established that it can be used in combination with NaOCl as a single irrigating solution during the whole course of root canal preparation [15, 16]. EDTA was applied for a shorter time to reproduce usual protocols where it is used as a final rinse to remove the smear layer.
Our results showed that the POBS of BD was higher than that of PMTA. These findings agree with previous POBS studies [18, 26, 34]. Nevertheless, other authors have reported no differences between these repairing cements [35, 36]. The discrepancies in the results could be explained by the differences in the methodology among studies [27]. One of the differences in the study designs is the time elapsed between placement of the cement and the push-out test. In fact, when analysing the POBS results of the different subgroups of our study, we observed that the difference between BD and PMTA was only noticeable after 1 day of setting, while after 21 days, no difference between cements was detected. It has been reported that the POBS of MTA increases progressively with time, showing higher values after 21 or 28 days than after shorter times [4, 26], while BD has shown a much faster increase of its POBS, reaching high values after only 24 h [26]. This fact is in accordance with the results obtained after the two setting times in the present study. The rapid improvement of the mechanical properties of BD has been explained by the shorter setting time after mixing, due to the calcium carbonate contained in the BD powder that acts as a nucleation site for calcium carbonate hydrate and the addition of CaCl2 to the liquid as a setting reaction accelerator [12].
Regarding the role of RCI on the performance of the CSBC, the results of this study showed that contact with the tested RCI has different effects on the POBS of BD and PMTA. After 1 day, the exposure of BD and PMTA to NaOCl + HEBP solution obtained a higher POBS, compared to the exposure to the other RCI. After 21 days, no differences were found among RCI for any of the cements. Previous studies have reported that prior conditioning of dentin with a mixture of NaOCl and HEBP increased the POBS of calcium silicate-based materials [37, 38]. A recent study conducted with the same methodology as the present one tested the effect of exposure to NaOCl + HEBP and other RCI on the POBS of several CSBC after 7 days of setting, concluding that HEBP + NaOCl may improve the POBS values of BD and not those of PMTA [25]. This finding is in agreement with the results obtained in the present study after 1 day of setting for BD, however not with those obtained after 21 days. Another study has reported the high reactivity observed in a CSBC when exposed immediately after mixing to a mixture of NaOCl and HEBP for 30 min and described the formation of a highly crystalline surface [31]. All these observations suggest that the effect of this RCI on POBS could be related to the hydration process and the time that the cement needs to complete this process. It could also be associated with the specific chemical composition of each cement, such as the water soluble polymer or the CaCl2 added to the liquid of BD, which have been shown to improve the physical characteristics and the hydration process [39]. It has been hypothesised that the different radiopacifiers may play a role in the chemical reactions of the cements and therefore in their ultimate physical properties [11, 21, 40]. However, a clear explanation for the effect of NaOCl + HEBP on the CSBC has not been well established yet, as there is lack of knowledge about the actual chemical reaction of these substances.
In our study, exposure of the CSBC to different RCI did not influence their failure patterns. This is in accordance with other studies [18]. The higher prevalence of cohesive failure for BD has been widely reported in the literature [18, 37] while adhesive failure has been described as the most frequent type of failure for PMTA [30, 41]. In this study, no differences were found between cements.
Deeper understanding of the effect of RCI such as HEBP on the performance of CSBC is needed to establish treatment protocols and improve the outcome of perforation treatment in clinical situations. The present study was designed to test the POBS immediately after the exposure of the cements to RCI at two different setting times. Our results suggest that NaOCl + HEBP may be a suitable irrigant to be used shortly after repairing a perforation with CSBC as it has no detrimental effect on the bond strength of these materials. In fact, it seems to be beneficial when used after 24 h of setting. Nevertheless, further research focused on the effect of exposure time or on the role of the composition of CSBC or RCI could provide useful evidence for better handling of these materials.
Conclusions
Based on the results of this study, it may be concluded that the POBS results are influenced by the cement, the setting time and the exposure to RCI. BD and PMTA exposed to NaOCl + HEBP after 1 day of setting obtained higher POBS than when exposed to other irrigants.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BD:
-
Biodentine
- CSBC:
-
Calcium silicate-based cements
- EDTA:
-
Ethylenediaminetetraacetic acid
- HEBP:
-
Etidronic acid (1-hydroxyethylidene-1, 1-bisphosphonate)
- MTA:
-
Mineral trioxide aggregate
- NaOCl:
-
Sodium hypochlorite
- PMTA:
-
ProRoot MTA
- POBS:
-
Push-out bond strength
- RCI:
-
Root canal irrigants
References
Sinai IH. Endodontic perforations: their prognosis and treatment. J Am Dent Assoc. 1977;95(1):90–5. https://doi.org/10.14219/jada.archive.1977.0531.
Jew RC, Weine FS, Keene JJ Jr, Smulson MH. A histologic evaluation of periodontal tissues adjacent to root perforations filled with cavit. Oral Surg Oral Med Oral Pathol. 1982;54(1):124–35. https://doi.org/10.1016/0030-4220(82)90427-3.
Holland R, Filho JA, de Souza V, Nery MJ, Bernabé PF, Junior ED. Mineral trioxide aggregate repair of lateral root perforations. J Endod. 2001;27(4):281–4. https://doi.org/10.1097/00004770-200104000-00011.
Gancedo-Caravia L, Garcia-Barbero E. Influence of humidity and setting time on the push-out strength of mineral trioxide aggregate obturations. J Endod. 2006;32(9):894–6. https://doi.org/10.1016/j.joen.2006.03.004.
Torabinejad M, Chivian N. Clinical applications of mineral trioxide aggregate. J Endod. 1999;25(3):197–205. https://doi.org/10.1016/s0099-2399(99)80142-3.
Torabinejad M, Parirokh M, Dummer PMH. Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview—part II: other clinical applications and complications. Int Endod J. 2018;51(3):284–317. https://doi.org/10.1111/iej.12843.
Prati C, Gandolfi MG. Calcium silicate bioactive cements: biological perspectives and clinical applications. Dent Mater. 2015;31(4):351–70. https://doi.org/10.1016/j.dental.2015.01.004.
Shokouhinejad N, Nekoofar MH, Pirmoazen S, Shamshiri AR, Dummer PM. Evaluation and comparison of occurrence of tooth discoloration after the application of various calcium silicate-based cements: an ex vivo study. J Endod. 2016;42(1):140–4. https://doi.org/10.1016/j.joen.2015.08.034.
Tang JJ, Shen ZS, Qin W, Lin Z. A comparison of the sealing abilities between Biodentine and MTA as root-end filling materials and their effects on bone healing in dogs after periradicular surgery. J Appl Oral Sci. 2019;27:e20180693. https://doi.org/10.1590/1678-7757-2018-0693.
Marciano MA, Costa RM, Camilleri J, Mondelli RF, Guimarães BM, Duarte MA. Assessment of color stability of white mineral trioxide aggregate angelus and bismuth oxide in contact with tooth structure. J Endod. 2014;40(8):1235–40. https://doi.org/10.1016/j.joen.2014.01.044.
Camilleri J. Characterization of hydration products of mineral trioxide aggregate. Int Endod J. 2008;41(5):408–17. https://doi.org/10.1111/j.1365-2591.2007.01370.x.
Camilleri J, Sorrentino F, Damidot D. Investigation of the hydration and bioactivity of radiopacified tricalcium silicate cement, biodentine and MTA angelus. Dent Mater. 2013;29(5):580–93. https://doi.org/10.1016/j.dental.2013.03.007.
Ochoa-Rodríguez VM, Tanomaru-Filho M, Rodrigues EM, Guerreiro-Tanomaru JM, Spin-Neto R, Faria G. Addition of zirconium oxide to biodentine increases radiopacity and does not alter its physicochemical and biological properties. J Appl Oral Sci. 2019;27: e20180429. https://doi.org/10.1590/1678-7757-2018-0429.
Pelepenko LE, Saavedra F, Antunes TBM, Bombarda GF, Gomes B, Zaia AA, et al. Physicochemical, antimicrobial, and biological properties of White-MTAFlow. Clin Oral Investig. 2021;25(2):663–72. https://doi.org/10.1007/s00784-020-03543-7.
Zehnder M, Schmidlin P, Sener B, Waltimo T. Chelation in root canal therapy reconsidered. J Endod. 2005;31(11):817–20. https://doi.org/10.1097/01.don.0000158233.59316.fe.
Zollinger A, Mohn D, Zeltner M, Zehnder M. Short-term storage stability of NaOCl solutions when combined with dual rinse HEDP. Int Endod J. 2018;51(6):691–6. https://doi.org/10.1111/iej.12875.
Tartari T, Guimarães BM, Amoras LS, Duarte MA, Silva e Souza PA, Bramante CM. Etidronate causes minimal changes in the ability of sodium hypochlorite to dissolve organic matter. Int Endod J. 2015;48(4):399–404. https://doi.org/10.1111/iej.12329.
Guneser MB, Akbulut MB, Eldeniz AU. Effect of various endodontic irrigants on the push-out bond strength of biodentine and conventional root perforation repair materials. J Endod. 2013;39(3):380–4. https://doi.org/10.1016/j.joen.2012.11.033.
Ballal V, Marques JN, Campos CN, Lima CO, Simão RA, Prado M. Effects of chelating agent and acids on biodentine. Aust Dent J. 2018;63(2):170–6. https://doi.org/10.1111/adj.12609.
do Prado M, de Lima CO, Marques JD, Ballal V, Simao RA, Campos CN. Effect of different irrigation regimens on the bond strength of biodentine used for furcal perforation repair. Endo-Endodontic Pract Today. 2019;13(1):49–59.
Shokouhinejad N, Yazdi KA, Nekoofar MH, Matmir S, Khoshkhounejad M. Effect of acidic environment on dislocation resistance of endosequence root repair material and mineral trioxide aggregate. J Dent (Tehran). 2014;11(2):161–6.
Lee YL, Lin FH, Wang WH, Ritchie HH, Lan WH, Lin CP. Effects of EDTA on the hydration mechanism of mineral trioxide aggregate. J Dent Res. 2007;86(6):534–8. https://doi.org/10.1177/154405910708600609.
Uyanik MO, Nagas E, Sahin C, Dagli F, Cehreli ZC. Effects of different irrigation regimens on the sealing properties of repaired furcal perforations. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2009;107(3):e91–5. https://doi.org/10.1016/j.tripleo.2008.10.024.
Prasanthi P, Garlapati R, Nagesh B, Sujana V, Kiran Naik KM, Yamini B. Effect of 17% ethylenediaminetetraacetic acid and 0.2% chitosan on pushout bond strength of biodentine and ProRoot mineral trioxide aggregate: an in vitro study. J Conserv Dent. 2019;22(4):387–90. https://doi.org/10.4103/jcd.Jcd_56_19.
Rebolloso de Barrio E, Gancedo-Caravia L, García-Barbero E, Pérez-Higueras JJ. Effect of exposure to root canal irrigants on the push-out bond strength of calcium silicate-based cements. Clin Oral Invest. 2021;25(5):3267–74. https://doi.org/10.1007/s00784-020-03658-x.
Marquezan FK, Kopper PMP, Dullius A, Ardenghi DM, Grazziotin-Soares R. Effect of blood contamination on the push-out bond strength of calcium silicate cements. Braz Dent J. 2018;29(2):189–94. https://doi.org/10.1590/0103-6440201801766.
Brichko J, Burrow MF, Parashos P. Design variability of the push-out bond test in endodontic research: a systematic review. J Endod. 2018;44(8):1237–45. https://doi.org/10.1016/j.joen.2018.05.003.
Nagas E, Kucukkaya S, Eymirli A, Uyanik MO, Cehreli ZC. Effect of laser-activated irrigation on the push-out bond strength of proroot mineral trioxide aggregate and biodentine in furcal perforations. Photomed Laser Surg. 2017;35(4):231–5. https://doi.org/10.1089/pho.2016.4171.
Scelza MZ, da Silva D, Scelza P, de Noronha F, Barbosa IB, Souza E, et al. Influence of a new push-out test method on the bond strength of three resin-based sealers. Int Endod J. 2015;48(8):801–6. https://doi.org/10.1111/iej.12378.
Nagas E, Cehreli ZC, Uyanik MO, Durmaz V, Vallittu PK, Lassila LVJ. Bond strength of mineral trioxide aggregate to root dentin after exposure to different irrigation solutions. Dent Traumatol. 2014;30(3):246–9. https://doi.org/10.1111/edt.12070.
Neelakantan P, Berger T, Primus C, Shemesh H, Wesselink PR. Acidic and alkaline chemicals’ influence on a tricalcium silicate-based dental biomaterial. J Biomed Mater Res B Appl Biomater. 2019;107(2):377–87. https://doi.org/10.1002/jbm.b.34129.
Ma J, Wang Z, Shen Y, Haapasalo M. A new noninvasive model to study the effectiveness of dentin disinfection by using confocal laser scanning microscopy. J Endod. 2011;37(10):1380–5.
Wang Z, Shen Y, Haapasalo M. Effectiveness of endodontic disinfecting solutions against young and old Enterococcus faecalis biofilms in dentin canals. J Endod. 2012;38(10):1376–9.
Nagas E, Cehreli ZC, Uyanik MO, Vallittu PK, Lassila LV. Effect of several intracanal medicaments on the push-out bond strength of ProRoot MTA and Biodentine. Int Endod J. 2016;49(2):184–8. https://doi.org/10.1111/iej.12433.
Stefaneli Marques JH, Silva-Sousa YTC, Rached FJA, de Macedo LMD, Mazzi-Chaves JF, Camilleri J, et al. Push-out bond strength of different tricalcium silicate-based filling materials to root dentin. Braz Oral Res. 2018;32(6):e18. https://doi.org/10.1590/1807-3107bor-2018.vol32.0018.
Aguiar BA, Frota LMA, Taguatinga DT, Vivan RR, Camilleri J, Duarte MAH, et al. Influence of ultrasonic agitation on bond strength, marginal adaptation, and tooth discoloration provided by three coronary barrier endodontic materials. Clin Oral Invest. 2019;23(11):4113–22. https://doi.org/10.1007/s00784-019-02850-y.
Paulson L, Ballal NV, Bhagat A. Effect of root dentin conditioning on the pushout bond strength of biodentine. J Endod. 2018;44(7):1186–90. https://doi.org/10.1016/j.joen.2018.04.009.
Neelakantan P, Nandagopal M, Shemesh H, Wesselink P. The effect of root dentin conditioning protocols on the push-out bond strength of three calcium silicate sealers. Int J Adhes Adhes. 2015;60:104–8. https://doi.org/10.1016/j.ijadhadh.2015.04.006.
Grech L, Mallia B, Camilleri J. Investigation of the physical properties of tricalcium silicate cement-based root-end filling materials. Dent Mater. 2013;29(2):e20–8. https://doi.org/10.1016/j.dental.2012.11.007.
Govindaraju L, Neelakantan P, Gutmann JL. Effect of root canal irrigating solutions on the compressive strength of tricalcium silicate cements. Clin Oral Investig. 2017;21(2):567–71. https://doi.org/10.1007/s00784-016-1922-0.
Shokouhinejad N, Nekoofar MH, Iravani A, Kharrazifard MJ, Dummer PM. Effect of acidic environment on the push-out bond strength of mineral trioxide aggregate. J Endod. 2010;36(5):871–4. https://doi.org/10.1016/j.joen.2009.12.025.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
LGC, JJPH and EGB: conceived and designed the experiment. ERB carried out the experiment and wrote the first version of the manuscript. JJPH and LGC analysed the data and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and with the approval of the Ethics Committee of Clinical Research of San Carlos Hospital (Madrid) (C.I. 16/335-E). Informed consents were obtained from all subjects or their legal guardian(s).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rebolloso de Barrio, E., Pérez-Higueras, J.J., García-Barbero, E. et al. Effect of exposure to etidronic acid on the bond strength of calcium silicate-based cements after 1 and 21 days: an in vitro study. BMC Oral Health 21, 591 (2021). https://doi.org/10.1186/s12903-021-01959-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-021-01959-5