Abstract
Background
Due to the multifactorial aetiology and unpredictable long-term stability, skeletal anterior open bite (SAOB) is one of the most intractable conditions for orthodontists. The abnormal orofacial myofunctional status (OMS) may be a major risk factor contributing to the development and relapse of SAOB. This study is aimed at evaluating the OMS and the efficacy of orofacial myofunctional therapy (OMT) alone for SAOB subjects.
Methods
Eighteen adolescents with SAOB (4 males, 14 females; age: 12–18 years) and eighteen adolescents with normal occlusion (2 males, 16 females; age: 12–18 years) were selected. The electromyographic activity (EMGA) associated with mastication and closed mouth state was measured. Lateral cephalography was used to evaluate craniofacial morphology. Wilcoxon signed rank tests and t-tests were performed to evaluate myofunctional and morphological differences. Pearson or Spearman correlation analysis was used to investigate the correlations between EMGA and morphological characteristics. SAOB subjects were given OMT for 3 months, and the EMGA was compared between before and after OMT.
Results
During rest, anterior temporalis activity (TAA) and mentalis muscle activity (MEA) increased in SAOB subjects, but TAA and masseter muscle activity (MMA) decreased in the intercuspal position (ICP); and upper orbicularis activity (UOA) and MEA significantly increased during lip sealing and swallowing (P < 0.05). Morphological evaluation revealed increases in the FMA, GoGn-SN, ANS-Me, N-Me, L1-MP, U6-PP, and L6-MP and decreases in the angle of the axis of the upper and lower central incisors and OB in SAOB subjects (P < 0.05). TAA, MMA and anterior digastric activity (DAA) in the ICP were negatively correlated with vertical height and positively correlated to incisor protrusion. MEA was positively correlated with vertical height and negatively correlated with incisor protrusion; and the UOA showed a similar correlation in ICP, during sealing lip and swallowing. After SAOB subjects received OMT, MEA during rest and TAA, MMA and DAA in the ICP increased, while UOA and MEA decreased (P < 0.05).
Conclusion
SAOB subjects showed abnormal OMS features including aberrant swallowing patterns and weak masticatory muscles, which were interrelated with the craniofacial dysmorphology features including a greater anterior facial height and incisor protrusion. Furthermore, OMT contributes to OMS harmonization, indicating its therapeutic prospect in SAOB.
Similar content being viewed by others
Background
Anterior open bite malocclusion is defined as the lack of vertical overlap or contact between the upper and lower incisors with occlusion of the posterior teeth. It can be classified as dentoalveolar or skeletal malocclusion. Certain morphological features, such as increased gonial and steep occlusal plane angles and increased anterior facial height, are usually present in individuals with skeletal anterior open bite (SAOB) [1,2,3,4]. Due to the multifactorial aetiology and unpredictable long-term stability of SAOB, it is considered one of the most intractable conditions to treat by many orthodontists.
Recent research has demonstrated the high prevalence of harmful oral habits, such as thumb or dummy sucking, mouth breathing, and tongue-thrust swallowing, among children with open bite [5,6,7,8], mainly ranging in age from 0 to 3 years old. One school of thought believes that, druing the long process of oromaxillofacial muscle development, harmful oral habits contribute to the development of an abnormal orofacial myofunctional status (OMS) [9, 10]. Several cross-sectional studies found that the abnormal OMS, in which inappropriate and uneven muscular pressure on facial bones can influence directional growth over time and eventually result in open bite [11,12,13]. Furthermore, a ten-year follow-up research showed that the dysfunctional neuromuscular pattern formed in long-term development could also lead to unfavourable results and relapse after treatment [14]. These facts suggest that the abnormal OMS of SAOB is a potential major risk factor that contributes to the development, treatment and relapse of open bite. Others support the opinion that the existence of harmful oral habits in the developing craniofacial structures is the consequence of the existing malocclusion of open bite, which is the form that determines OMS [15, 16].
Orofacial myofunctional therapy (OMT), which is often considered as an adjunct to conventional orthodontic treatment, has been shown to be effective in harmonizing the OMS based on its improvement of musculature and orofacial function. Degan VV [17] highlighted that myofunctional therapy associated with the removal of sucking habits contributed to a better and faster amelioration of the swallowing pattern and the tongue rest position. Korbmacher [18] demonstrated that an appliance-based orofacial muscle training protocol exhibited 65% effectiveness in altering habitual mouth breathing to nasal breathing. However, a recent systematic review and meta-analysis found that although myofunctional treatment in the deciduous and mixed dentition children appeared to be promising to correct anterior open bite, the quality of the existing evidence was questionable [19]. Moreover, inadequate attention has been paid to the correlation between the OMS and morphological features in SAOB and the potential benefits of OMT regarding the myofunctional status and orthodontic treatment.
In the present study, we compared the EMGA of different muscles under four conditions between adolescents with SAOB or normal occlusion, and we performed an analysis of correlations between the EMGA and morphological features of adolescents with SAOB. In addition, we compared the myofunctional status of oromaxillofacial muscles in SAOB subjects before and after receiving OMT. The aim of this study was to obtain a better understanding of the OMS and its relationship with craniofacial dysmorphology in SAOB subjects and to propose preliminary treatment strategies targeting early intervention, thereby facilitating orthodontic treatment.
Methods
Subjects
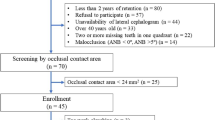
Eighteen adolescents with SAOB (4 males, 14 females; age: 12–18 years) and eighteen adolescents with normal occlusion (2 males, 16 females; age: 12–18 years) were selected for comparison of the OMS. Three female adolescents with SAOB were lost to follow-up during OMT, so a total of fifteen adolescents with SAOB (4 males, 11 females; age: 12–18 years) finished the OMT regimen. All of the subjects were diagnosed at the orthodontic department of the Hospital of Stomatology, Sun Yat-sen University. This study was performed in accordance with the Declaration of Helsinki, and the Medical Ethics Committee of the Hospital of Stomatology, Sun Yat-sen University, approved the study (Protocol Title: The Electromyographic Activity Of Oromaxillofacial Muscles In Adolescents With Skeletal Anterior Open Bite, No. KQEC-2020-53-01). The purpose and methods of the study were explained to all subjects, each of whom provided informed consent to participate.
The selection criteria for the experimental group were as follows: (1) age from 12–18 years; (2) full permanent dentition with second molar occlusion; (3) lack of contact between the lower incisors and the upper incisors or palate, and a vertical distance between the lower and upper incisal edge of at least 0.5 mm; (4) hyperdivergent facial type: SN-MP ≥ 40°; and (5) no missing teeth. The selection criteria for the control group were as follows: (1) age from 12 to 18 years; (2) full permanent dentition with second molar occlusion; (3) normal overbite: vertical distance between the lower and upper incisal edge of 1–4 mm; (4) normodivergent facial type: 30° < SN-MP < 40°; (5) no missing teeth; and (6) bilateral neutral molar relationship. The exclusion criteria for both groups were as follows: (1) previous orthodontic treatment or orthognathic surgery; (2) symptoms of temporomandibular joint disorder; (3) severe skeletal facial asymmetry; and (4) unilateral masticatory habit.
EMG examination
EMG recordings of the oromaxillofacial muscles were made using a BioEMG electromyographic amplifier (BioEMG, Bioresearch, Inc., Milwaukee, WI, USA) and BioPAC software (BioPAC Systems, Inc., Santa Barbara, CA, USA) (Fig. 1). The EMG examinations were conducted in the EMG laboratory of the orthodontic department of the Hospital of Stomatology, Sun Yat-sen University. Data were recorded with each subject seated in a dental chair; the head was supported with the Frankfort horizontal plane parallel to the ground. The position of differential active electrodes, determined by palpation and anatomical location, was parallel with the muscle fibres’ main direction, and skin impedance was reduced by wiping the skin with alcohol. In every case, a ground electrode was placed near the 7th vertebra to assist the bipolar electrode configuration. In this way, EMGA associated with mastication, including the activity of anterior temporalis, masseter muscle, and anterior digastric, and EMGA associated with the closed mouth state, including the activity of upper orbicularis and mentalis muscle, were recorded (Fig. 2).
The EMG recordings were carried out under the following clinical conditions: mandibular rest (REST), maximum voluntary contraction in the intercuspal position (ICP), lip sealing (LIP), and swallowing (SWA). The protocols were as follows: REST: Subjects were asked to relax facial muscles for 5 min with the mandible in the rest position and the lips and teeth not in contact. ICP: The teeth were clenched in the ICP as tightly as possible for 2 s. LIP: Before testing, the lips were ensured to be moist and the mandible was in the rest position; then, the lips were slightly closed lips to achieve natural contact for 2 s while receiving instruction. SWA: First, 20 ml of water was held in the mouth and the facial muscles were relaxed for at least 5 s; then, the water was swallowed in one gulp while receiving instruction. EMGA under each condition was obtained three times, resting EMGA was measured for 5 s each time, EMGA under the other three conditions was assessed 2 s each time, with an interval of 1 min in order to prevent muscular fatigue. The mean values of EMGA of those muscles under each condition were calculated and recorded.
Morphological characteristic evaluation
Before orthodontic treatment, the craniofacial morphological characteristics of all 36 subjects were measured using lateral cephalograms. Radiographs were obtained when the upper and lower dentition were in the centric occlusion position and the Frankfort horizontal plane was parallel to the ground. The radiographs were digitally traced using Quick Ceph Studio software (Quick Ceph Systems, San Diego, CA, USA).
The following cephalometric measurements were traced and measured to express different anatomic relationships: anteroposterior jaw relationships: SNA, SNB, and ANB; protrusion of incisors: Mx1-SN, Md1-MP, and angle of the axis of the upper and lower central incisors; mandibular plane inclination: FMA and GoGn-SN; facial height: N-Me, ANS-Me, Go-S, and Go-Ar; positional relations between the upper and lower incisors: overbite and overjet; and alveolar height: U1-PP, L1-MP, U6-PP, and L6-MP.
OMT
According to the myofunctional and morphological characteristics of the SAOB subjects, the perioral muscles, tongue and masticatory muscles were specially trained to achieve a better myofunctional status. The protocol was as follows: The perioral muscles were strengthened by pressing the lips tightly together for nasal breathing for at least 0.5 h a day (Fig. 3a). The masticatory muscles and tongue were trained for 2 h a day by chewing gum vigorously with posterior teeth and shaping the softened chewing gum into a ball on the front of the tongue, lifting the tip of the tongue and sticking the gum to the hard palate, pressing the tongue against the hard palate and flattening the gum, swallowing saliva while simultaneously pressing the tongue against the gum, and repeating the above steps (Fig. 3b).
OMT, OMT of perioral muscles (a), OMT of masticatory muscles and tongue: including chewing gum vigorously with posterior teeth and shaping the softened chewing gum into a ball on the front of the tongue (b), lifting the tip of the tongue and sticking the gum to the hard palate (c), pressing the tongue against the hard palate and flattening the gum (d)
The OMT regimen lasted for 3 months and subjects received follow-up contact by telephone every 2 weeks and paid a return visit every month. Each subject received an EMGA record before and after the 3-month OMT treatment.
Statistical analysis
Wilcoxon signed rank tests and t-tests were performed to evaluate myofunctional and morphological differences between the normal and SAOB subjects. In order to select representative items, factor analysis was performed for 18 cephalometric measurements and 20 EMG measurements; then, the main factors from each group were extracted. Furthermore, we investigated the correlations between muscle activity and morphological characteristics by performing Pearson or Spearman correlation analysis of the main factors from among the cephalometric and EMG measurements. The OMS of SAOB subjects before and after receiving OMT was compared using a Wilcoxon signed rank test or t-test to investigate the effect of OMT. Wilcoxon signed rank tests were used for data with a skewed distribution, and t-tests were used for data with a normal distribution; α = 0.05. Data are presented as the median (25%, 75%) or mean ± standard deviation. A P value less than 0.05 was considered statistically significant. All tests were conducted using SPSS 19 software (SPSS, Chicago, IL, USA).
Results
OMS features and morphological characteristics of SAOB
At rest, the activity of anterior temporalis and mentalis muscle significantly increased in SAOB subjects compared to normal subjects, but the activity of anterior temporalis and masseter muscle decreased in the ICP. Furthermore, upper orbicularis activity and mentalis muscle activity significantly increased during lip sealing and swallowing, indicating that the OMS features of SAOB mainly include aberrant swallowing patterns and weak masticatory muscles (Table 1).
Morphological evaluation of SAOB subjects compared to normal subjects revealed significant (P < 0.05) increases in the FMA, GoGn-SN, ANS-Me, N-Me, L1-MP, U6-PP, and L6-MP and significant (P < 0.05) decreases in the angle of the axis of the upper and lower central incisors and overbite. These findings indicate that the morphological features of SAOB mainly reflect a greater anterior facial height and greater degree of incisor protrusion (Table 2).
Correlations between EMGA and morphological characteristics of SAOB
Factor analysis was carried for 18 cephalometric measurements, and 5 main factors were extracted (Table 3). In the same way, factor analysis was carried for 20 EMG measurements, including the EMGA of 5 kinds of muscles under 4 different conditions, and 6 main factors were extracted (Table 4). The correlation analysis between the morphological factors and EMGA factors showed that factor 1 and factor 5 from the cephalometric measurements and factor 1 from the EMGA measurements were positively correlated (Table 5). Factor 1 from the cephalometric measurements corresponds to vertical height, including the ANS-Me, N-Me, U1-PP, U6-PP, L1-MP, FMA, GoGn-SN, L6-MP, and overbite, while factor 5 corresponds to incisor protrusion, including the Mx1-SN and angle of the axis of the upper and lower central incisors (Table 3). Factor 1 from the EMGA measurements corresponds to the high EMGA of perioral muscles and low EMGA of muscles associated with mastication in the ICP (Table 4).
Table 6 shows the results of a further correlation analysis of the corresponding measurements of the main factors. The activity of anterior temporalis, masseter muscle and anterior digastric in the ICP were negatively correlated with measurements of vertical height, such as the ANS-Me, FMA, GoGn-SN, and Mx1-SN, while positively correlated with measurements of incisor protrusion, such as the angle of the axis of the upper and lower central incisors. Mentalis muscle activity and upper orbicularis activity were positively correlated with vertical height and negatively correlated with incisor protrusion during sealing lip and swallowing. At rest, mentalis muscle activity showed a positive correlation with vertical height and a negative correlation with incisor protrusion. These results suggest that the craniofacial dysmorphology of SAOB is associated with the orofacial myofunctional disorder. EMGA associated with mastication in the ICP was negatively correlated with vertical height and positively correlated with incisor protrusion, while EMGA associated with the closed mouth state was positively correlated with vertical height and negatively correlated with incisor protrusion.
Influence of OMT on EMGA in SAOB
By comparing the measurements, it was found that mentalis muscle activity at rest, and the activity of anterior temporalis, masseter muscle and anterior digastric in the ICP increased significantly (P < 0.05) after OMT; however upper orbicularis activity and mentalis muscle activity decreased significantly (P < 0.05) after OMT, suggesting that OMT might contribute to normalization of the OMS by strengthening the muscles associated with mastication in the ICP and relaxing the perioral muscles during lip sealing (Table 7).
Discussion
A general agreement has been reached that orofacial myofunctional disorder has strong ties to malocclusion and the craniofacial dysmorphology of SAOB. Among various methods to estimate the neuromuscular status, EMG has become the most common method because of the higher sensitivity of the myoelectric amplitude than indicators of morphology and function in reflecting myofunctional changes. In this research, by comparing the EMGA of different muscles under four conditions between adolescents with SAOB or normal occlusion, we found that the OMS features of SAOB mainly include aberrant swallowing patterns and weak masticatory muscles. Furthermore, the morphological features of SAOB were found to mainly involve the anterior facial height and degree of incisor protrusion, and the correlation analysis revealed that the craniofacial dysmorphology of SAOB is associated with orofacial myofunctional disorder.
In this research, orofacial EMGA was classified into EMGA associated with mastication, including the activity of anterior temporalis, masseter muscle, and anterior digastric, and EMGA associated with the closed mouth state, including activity of upper orbicularis and mentalis muscle, since mastication and the closed mouth state are common and important states during orofacial function. Mastication is a complex functional movement integrating the jaw bones, masticatory muscles and soft tissues, such as the cheeks, lips and tongue. The temporal muscle, masseter muscle, and anterior digastric muscle play important roles in mastication by contracting or relaxing muscle fibres to lift or lower the mandible and close or open the mouth. Regarding perioral muscles, the upper orbicularis and mentalis muscle are essential for maintaining the closed mouth state at rest and during functions such as swallowing and lip sealing.
The ICP is the most important functional position during mastication. In this research, we observed that in the ICP, the activity of anterior temporalis, masseter muscle and anterior digastric were significantly lower in adolescents with SAOB, which is in agreement with the findings of previous studies [20,21,22]; additionally, there were significant negative correlations between vertical morphology factors with the activity of all three of these muscles in the ICP. It is widely accepted that a large proportion of subjects with SAOB suffer from mouth breathing [6, 8]. Breathing is the primary requirement, so the oral cavity needs to make room for air circulation, and then food often cannot be chewed fully. As masticatory force and nasal breathing can both influence the three-dimensional development of the jaws during growth, the low mastication efficiency and lack of chewing stimulation in the molar area can lead to an increase in the occlusal height and eventually the formation of hyperdivergent facial pattern [20]. In this research, subjects in the experimental group had already formed steep occlusal plane angles. The reason for this finding may lie in that some morphological features of SAOB, such as a higher gonial angle and greater maxillary height, can shift the position of the load application point posteriorly, which leads to an increase in the loading moment arm and eventually results in weakening of the mechanical force of the stomatognathic system. Furthermore, the cross-sectional area and muscular force of the masseter muscle and temporal muscle tend to be smaller in those with a hyperdivergent facial type [23], which results in lower EMGA.
The clinical rest position is also called the mandibular postural position, in which the mandible stretches masticatory muscle fibres by the effect of gravity to maintain the mandibular position. Subjects with SAOB usually show a well-developed and clockwise-rotated mandibular body, which imposes a greater stretching force through the masticatory muscles. In the present study, the anterior temporalis activity in the experimental group was markedly higher than that in the control group in the resting posture, while the difference in masseter muscle activity was not significant; Cha [24] reported similar findings in a previous study. This result might be explained by the different functions of the temporal muscle and masseter muscle in the resting position and ICP potentially providing different stimuli to the corresponding neuromuscular spindles.
In turns of perioral muscles, harmful habits, such as mouth breathing and tongue-thrust swallowing, during development can disrupt the balance between perioral muscles and other muscles, resulting in malocclusion. In this research, the EMGA in SAOB patients was significantly higher at rest and during lip pressing and swallowing and was positively correlated with the anterior facial height but negatively correlated with incisor protrusion. The reason for this finding may be that the high prevalence of harmful oral habits, such as mouth breathing, tongue-thrust swallowing and thumb sucking, during development results in lip incompetence as a common phenomenon in subjects with SAOB [25,26,27]. In the normal stomatognathic system, the muscular forces of perioral muscles and the tongue maintain a balance to achieve passive lip contact and eventually a closed oral environment, which means that achieving a normal lip sealing state does not require greater contraction of the perioral muscle fibres. Tomiyama [28] found that subjects with incompetent lips showed higher EMGA in the clinical rest position or during chewing when they were told to close their mouth. Gamboa [27] found that the EMGA of perioral muscles was significantly higher in subjects without competent lips during swallowing. Thus, subjects with SAOB tend to exert greater perioral muscular effort due to the requirement of lip sealing during functional activities. Furthermore, incompetent lips contribute to harmful oral habits, such as chronic mouth breathing and tongue thrusting, which could be risk factors for open bite and are associated with the adaptive change of the hyperdivergent facial pattern during development [29, 30].
On this basis, the OMS feature of the SAOB facial pattern was found to mainly include passive lip contact with extra perioral muscle contraction, aberrant swallowing patterns, and weak masticatory muscles. According to these features, well-directed OMT was given to adolescents with SAOB, and the OMT phase of the intervention lasted 3 months. After the treatment, the EMGA of masticatory muscles was significantly increased, while that of perioral muscles was decreased, indicating that the OMT contributed to an improvement in the orofacial myofunctional disorder. As development of the masticatory system is influenced by functional needs, gum chewing exercise was designed to improve masticatory function in this research. Previous studies have shown that chewing exercise contributes to improvements in masticatory disturbances and deficiencies by influencing the functional capacity and increasing the strength of the masticatory muscles [31,32,33], which is consistent with our results. Furthermore, according to the high prevalence of harmful oral habits, such as mouth breathing and tongue-thrust swallowing, among subjects with SAOB and the relationship of these habits with orofacial myofunctional disorder, lip-pressing training and tongue training were designed to correct the harmful oral habits and abnormal tongue forces by establishing patterns of nasal breathing and physiological swallowing. Former studies have demonstrated that OMT can significantly change the tongue posture by establishing patterns of nasal breathing and physiological swallowing [30, 34]. Our results support the efficacy of OMT in altering the OMS. Combined with the findings discussed above, OMT is effective in correcting harmful habits and harmonizing OMS abnormalities, indicating that OMT as one of adjuvant orthodontic therapies is beneficial to the treatment of SAOB patients. For patients in the growth and development stage, in whom the malocclusion or craniofacial deformities has not yet formed, it is important to raise awareness of harmful oral habits and provide early intervention with well-directed OMT to help rebalance the OMS for facial bone growth. For patients in whom malocclusion or craniofacial deformities has already developed, combining OMT with conventional orthodontic treatment may help reduce the difficulty of treatment by harmonizing abnormal OMS. However, there have been few studies on the effects of OMT on the improvement of craniofacial morphology in SAOB patients. Further research is needed to evaluate the morphological changes of SAOB patients after OMT and confirm the long-term effects of OMT as an adjunct to conventional orthodontic treatment. It is worth noting that genetic factors should also be taken into account.
Conclusion
In summary, the OMS features of SAOB mainly include aberrant swallowing patterns and weak masticatory muscles, while the morphological features mainly reflect a greater anterior facial height and greater degree of incisor protrusion, demonstrating that the craniofacial dysmorphology of SAOB is associated with orofacial myofunctional disorder. Furthermore, OMT contributes to OMS harmonization by normalizing abnormal EMGA, indicating that taking OMT as one of adjuvant orthodontic therapies is beneficial to the development and treatment of SAOB.
Availability of data and materials
Data used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SAOB:
-
Skeletal anterior open bite
- OMS:
-
Orofacial myofunctional status
- OMT:
-
Orofacial myofunctional therapy
- EMGA:
-
Electromyographic activity
- TAA:
-
Anterior temporalis activity
- MMA:
-
Masseter muscle activity
- DAA:
-
Anterior digastric activity
- UOA:
-
Upper orbicularis activity
- MEA:
-
Mentalis muscle activity
- AOB:
-
Anterior open bite
- EMG:
-
Electromyography
- TA:
-
Temporal muscle
- MM:
-
Masseter muscle
- OMT:
-
Orofacial myofunctional therapy
- REST:
-
Mandibular rest
- ICP:
-
Maximum voluntary contraction in the intercuspal position
- LIP:
-
Lip sealing
- SWA:
-
Swallowing
- DA:
-
Anterior digastric
- UO:
-
Upper orbicularis
- ME:
-
Mentalis muscle
References
Krey KF, Dannhauer KH, Hierl T. Morphology of open bite. J Orofac Orthop. 2015;76(3):213–24.
Taibah SM, Feteih RM. Cephalometric features of anterior open bite. World J Orthod. 2007;8(2):145–52.
Perillo L, Isola G, Esercizio D, Iovane M, Triolo G, Matarese G. Differences in craniofacial characteristics in Southern Italian children from Naples: a retrospective study by cephalometric analysis. Eur J Paediatr Dent. 2013;14(3):195–8.
Perillo L, Padricelli G, Isola G, Femiano F, Chiodini P, Matarese G. Class II malocclusion division 1: a new classification method by cephalometric analysis. Eur J Paediatr Dent. 2012;13(3):192–6.
Kasparaviciene K, Sidlauskas A, Zasciurinskiene E, Vasiliauskas A, Juodzbalys G, Sidlauskas M, Marmaite U. The prevalence of malocclusion and oral habits among 5-7-year-old children. Med Sci Monit. 2014;20:2036–42.
Oliveira AC, Paiva SM, Martins MT, Torres CS, Pordeus IA. Prevalence and determinant factors of malocclusion in children with special needs. Eur J Orthod. 2011;33(4):413–8.
Mistry P, Moles DR, O’Neill J, Noar J. The occlusal effects of digit sucking habits amongst school children in Northamptonshire (UK). J Orthod. 2010;37(2):87–92.
Paolantonio EG, Ludovici N, Saccomanno S, La Torre G, Grippaudo C. Association between oral habits, mouth breathing and malocclusion in Italian preschoolers. Eur J Paediatr Dent. 2019;20(3):204–8.
Grabowski R, Kundt G, Stahl F. Interrelation between occlusal findings and orofacial myofunctional status in primary and mixed dentition: Part III: interrelation between malocclusions and orofacial dysfunctions. J Orofac Orthop. 2007;68(6):462–76.
Moimaz SA, Garbin AJ, Lima AM, Lolli LF, Saliba O, Garbin CA. Longitudinal study of habits leading to malocclusion development in childhood. BMC Oral Health. 2014;14:96.
Gomes MC, Neves E, Perazzo MF, Martins CC, Paiva SM, Granville-Garcia AF. Association between psychological factors, socio-demographic conditions, oral habits and anterior open bite in five-year-old children. Acta Odontol Scand. 2018;76(8):553–8.
Silvestrini-Biavati A, Salamone S, Silvestrini-Biavati F, Agostino P, Ugolini A. Anterior open-bite and sucking habits in Italian preschool children. Eur J Paediatr Dent. 2016;17(1):43–6.
Grippaudo C, Paolantonio EG, Antonini G, Saulle R, La Torre G, Deli R. Association between oral habits, mouth breathing and malocclusion. Acta Otorhinolaryngol Ital. 2016;36(5):386–94.
Zuroff JP, Chen SH, Shapiro PA, Little RM, Joondeph DR, Huang GJ. Orthodontic treatment of anterior open-bite malocclusion: stability years postretention. Am J Orthod Dentofacial Orthop. 2010;137(3):301–2.
Tulley WJ. A critical appraisal of tongue-thrusting. Am J Orthod. 1969;55(6):640–50.
Subtelny J, Sakuda A. Open-bite: diagnosis and treatment. Am J Orthod. 1964;50:337–58.
Degan VV, Puppin-Rontani RM. Removal of sucking habits and myofunctional therapy: establishing swallowing and tongue rest position. Pro Fono. 2005;17(3):375–82.
Korbmacher HM, Schwan M, Berndsen S, Bull J, Kahl-Nieke B. Evaluation of a new concept of myofunctional therapy in children. Int J Orofacial Myology. 2004;30:39–52.
Koletsi D, Makou M, Pandis N. Effect of orthodontic management and orofacial muscle training protocols on the correction of myofunctional and myoskeletal problems in developing dentition. A systematic review and meta-analysis. Orthod Craniofac Res. 2018;21(4):202–15.
Alabdullah M, Saltaji H, Abou-Hamed H, Youssef M. Association between facial growth pattern and facial muscle activity: a prospective cross-sectional study. Int Orthod. 2015;13(2):181–94.
Gomes SG, Custodio W, Jufer JS, Del BC, Garcia RC. Mastication, EMG activity and occlusal contact area in subjects with different facial types. Cranio. 2010;28(4):274–9.
Custodio W, Gomes SG, Faot F, Garcia RC, Del BCA. Occlusal force, electromyographic activity of masticatory muscles and mandibular flexure of subjects with different facial types. J Appl Oral Sci. 2011;19(4):343–9.
Charalampidou M, Kjellberg H, Georgiakaki I, Kiliaridis S. Masseter muscle thickness and mechanical advantage in relation to vertical craniofacial morphology in children. ACTA Odontol Scand. 2008;66(1):23–30.
Cha BK, Kim CH, Baek SH. Skeletal sagittal and vertical facial types and electromyographic activity of the masticatory muscle. Angle Orthod. 2007;77(3):463–70.
Baroni M, Ballanti F, Franchi L, Cozza P. Craniofacial features of subjects with adenoid, tonsillar, or adenotonsillar hypertrophy. Prog Orthod. 2011;12(1):38–44.
Nicolet C, Munoz D, Marino A, Werner A, Argandona J. Lip competence in Class III patients undergoing orthognathic surgery: an electromyographic study. J Oral Maxillofac Surg. 2012;70(5):e331–6.
Gamboa NA, Miralles R, Valenzuela S, Santander H, Cordova R, Bull R, Espinoza DA, Martinez CA. Comparison of muscle activity between subjects with or without lip competence: Electromyographic activity of lips, supra- and infrahyoid muscles. Cranio. 2017;35(6):385–91.
Tomiyama N, Ichida T, Yamaguchi K. Electromyographic activity of lower lip muscles when chewing with the lips in contact and apart. Angle Orthod. 2004;74(1):31–6.
Saitoh I, Inada E, Kaihara Y, Nogami Y, Murakami D, Kubota N, Sakurai K, Shirazawa Y, Sawami T, Goto M, et al. An exploratory study of the factors related to mouth breathing syndrome in primary school children. Arch Oral Biol. 2018;92:57–61.
Kurihara K, Fukui T, Sakaue K, Hori K, Ono T, Saito I. The effect of tongue thrusting on tongue pressure production during swallowing in adult anterior open bite cases. J Oral Rehabil. 2019;46(10):895–902.
Maki K, Nishioka T, Morimoto A, Naito M, Kimura M. A study on the measurement of occlusal force and masticatory efficiency in school age Japanese children. Int J Paediatr Dent. 2001;11(4):281–5.
Ohira A, Ono Y, Yano N, Takagi Y. The effect of chewing exercise in preschool children on maximum bite force and masticatory performance. Int J Paediatr Dent. 2012;22(2):146–53.
Nakagawa K, Matsuo K, Takagi D, Morita Y, Ooka T, Hironaka S, Mukai Y. Effects of gum chewing exercises on saliva secretion and occlusal force in community-dwelling elderly individuals: a pilot study. Geriatr Gerontol Int. 2017;17(1):48–53.
Van Dyck C, Dekeyser A, Vantricht E, Manders E, Goeleven A, Fieuws S, Willems G. The effect of orofacial myofunctional treatment in children with anterior open bite and tongue dysfunction: a pilot study. Eur J Orthod. 2016;38(3):227–34.
Acknowledgements
We would like to thank Department of Orthodontic, Hospital of Stomatology, Sun Yat-sen University, for providing all experimental equipment.
Funding
This study was supported by grants of Medical Scientific Research Foundation of Guangdong Province of China (A2018418).
Author information
Authors and Affiliations
Contributions
HH and YZ performed the clinical investigations and drafted the manuscript. CP, JD, XZ, LD contributed to the data collection. XC and YX were responsible for the data analysis. LW were responsible for the study design, manuscript revising, and financial support. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study followed the Declaration of Helsinki on medical protocol and ethics and the Medical Ethics Committee of Hospital of Stomatology, Sun Yat-sen University, has approved the study (Protocol Title: The Electromyographic Activity Of Oromaxillofacial Muscles In Adolescents With Skeletal Anterior Open Bite. No. KQEC-2020-53-01). Informed consent was obtained from each child’s parent and/or legal guardian.
Consent for publication
Written informed consent for publication were obtained from the parents of the patients.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hong, H., Zeng, Y., Chen, X. et al. Electromyographic features and efficacy of orofacial myofunctional treatment for skeletal anterior open bite in adolescents: an exploratory study. BMC Oral Health 21, 242 (2021). https://doi.org/10.1186/s12903-021-01605-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-021-01605-0