Abstract
Background
This study aimed to investigate the association between sleep duration and bone mineral density (BMD) and determine whether vitamin D (VD) status influenced the association between sleep duration and BMD.
Methods
National Health and Nutrition Examination Survey 2007–2014 participants aged ≥ 40 years were included in this study. BMD testing was conducted with dual-energy X-ray absorptiometry examinations. Moreover, all individuals were divided into four groups according to self-reported nocturnal sleep duration (7–8 h; 6 h; < 6 h; and > 8 h). In addition, the differences in BMD between the normal sleep duration group and other groups were calculated using multiple linear regression models.
Results
Overall, the median age of the overall study population was 55.00 years old, with 46.97% of men distributed. Participants sleeping > 8 h/night had lower BMDs than those sleeping 7–8 h/night. Moreover, the association between unhealthy sleep duration (especially > 8 h/night) and low BMD was more pronounced in older individuals, men, postmenopausal women, and subjects with inadequate VD intakes (< 15.00 µg/day) or deficient/insufficient serum 25-hydroxyvitamin D (< 75.00 nmol/L).
Conclusions
In conclusion, unhealthy sleep duration, especially long sleep duration, was associated with decreased BMD, particularly among individuals aged > 60 years, men, or postmenopausal women. Moreover, VD status might influence the association between sleep duration and BMD, especially in the context of inadequate VD intake or deficient/insufficient serum 25-hydroxyvitamin D levels. However, given the limitations of the present study, further investigation is warranted to confirm this association and to explore potential mechanisms.
Similar content being viewed by others
Background
Osteoporosis, which is characterized by low bone mineral density (BMD) and microarchitectural deterioration of bone tissue, is a common chronic disease among the middle-age and elderly individuals [1]. According to the International Osteoporosis Foundation (IOF), one-third of females and one-fifth of males aged over 50 years worldwide are at risk of osteoporosis, and the prevalence of osteoporosis is still increasing annually in the middle-age and elderly population [2,3,4]. Moreover, osteoporotic fracture, which is one of the most severe complications of osteoporosis, is an important cause of morbidity among older adults [5, 6]. In addition to placing an economic burden on healthcare systems, osteoporosis also drastically impacts the quality of life of patients [1]. Osteoporosis is a complex disease determined by numerous genes and environmental factors from the standpoint of pathogenesis [1]. In addition to essential nonmodifiable risk factors, such as aging, menopausal status, and genetic factors, many modifiable risk factors, such as dietary and lifestyle habits, also play essential roles in the pathogenesis of osteoporosis [1]. Therefore, exploration of the potentially modifiable risk factors for osteoporosis is receiving increasing attention and is expected to open new preventive avenues.
Although several previous studies reported that long or short sleep duration might be associated with lower BMD or a high risk of osteoporosis [7, 8]. Fu et al. observed that Chinese women who slept 6 h or less per night showed lower BMD than those who slept 8 h per night [7]. Wang et al. found that post-menopausal women with long sleep duration (> 10 h/day) showed a higher risk of osteoporosis than those with normal sleep duration (8–9 h/day) [8]. However, it should be noted that there is still no reliable conclusion because some studies found that long or short sleep durations might not contribute to decreased BMD [9, 10]. For example, Swanson et al. observed that nocturnal sleep duration was not independently associated with hip BMD among postmenopausal women irrespective of the method of assessment of sleep duration (objective or subjective) [9]. Another study by Swanson et al. found that there were no significant differences in hip or spine BMD between older men with short sleep duration (< 6 h) or recommended sleep duration (7–8 h) [10]. These controversial findings (abnormal sleep duration might be associated with low BMD or it might not) indicate that more studies on the impact of sleep duration on bone health are needed and suggest that other potential factors might influence the association between sleep duration and BMD.
As previous studies have reported, vitamin D (VD) is an essential nutrient for human health [11, 12]. VD status usually involves two aspects: daily VD intake and serum 25-hydroxyvitamin D [25(OH)D] level. VD intake from dietary sources and supplements is essential for maintaining adequate VD levels in the body, especially for individuals with insufficient light exposure. Moreover, the serum level of 25(OH)D, a precursor of activated VD, reflects whole-body VD stores and is the most commonly used indicator to adjudicate whether VD deficiency is present. Several studies have demonstrated that VD plays an essential role in bone metabolism [11, 12]. Low daily VD intake or low serum 25(OH)D levels were associated with lower BMD [11, 12]. Moreover, many studies found that vitamin status was linked to sleep behaviors [13,14,15]. For example, Majid et al. observed that VD supplements improved sleep quality among individuals aged 20 to 50 years [16]. A meta-analysis by Gao et al. found that VD deficiency was associated with poor sleep quality, short sleep duration, and sleepiness [15]. In addition, de Oliveira et al. observed that short sleep duration (< 6 h/day) was independently associated with low serum 25(OH)D levels among men [17]. However, there was no definite evidence of whether VD status affected the association between sleep duration and BMD.
Based on the above reasons, this study aimed to investigate the association between sleep duration and BMD. Moreover, we also tried to determine whether VD status affected the association between sleep duration and BMD.
Methods
Study population
This was a cross-sectional study. The data of all participants were extracted from the National Health and Nutrition Examination Survey (NHANES) database [18]. The NHANES database, which is affiliated with the Centers for Disease Control and Prevention (USA) and updated biennially, was designed to assess the health and nutritional status of general United States (US) residents. We extracted data from the NHANES database (2007–2008, 2009–2010, 2013–2014; BMD data were not obtainable in the NHANES database for 2011–2012) [18]. The inclusion criteria were as follows: (i) participants aged ≥ 40 years; (ii) participants with complete BMD data; (iii) participants with available sleep duration data; and (iv) participants with complete VD status data (VD intake and serum 25(OH)D). Moreover, subjects with missing data on covariates (missing data; refused to answer; or answered “do not know”) were excluded from the present study. Finally, all individuals included in this study provided informed consent, and the ethics review board of the National Center for Health Statistics approved the study [19].
BMD testing
All participants included in the present study underwent BMD testing via dual-energy X-ray absorptiometry (DXA) examinations. The examinations were conducted by certified radiology technologists using Hologic QDR-4500A fan-beam densitometers (Hologic; Bedford, MA), and the data analysis was performed using Hologic APEX, version 4.0, software. Other details about the procedure of BMD testing are available on the NHANES website [20]. Moreover, this study analyzed the BMD data of the femoral regions [total femur BMD (TF-BMD) and femoral neck BMD (FN-BMD)] and spinal areas [total spine BMD (TS-BMD)].
Sleep duration
The sleep duration analyzed in the present study included only self-reported nocturnal sleep duration. Moreover, the present study did not include daytime sleep duration or daytime napping because they were not available on the NHANES database. All sleep duration data were collected by a questionnaire survey, which asked the participants, “How much sleep do you usually get at night on weekdays or workdays?” Moreover, all results collected for sleep duration were reported in integral numbers. Other details about the sleep duration data collection are available on the NHANES website [21]. Moreover, we divided all participants into four groups according to the frequency distribution of sleep duration among all individuals included in the final analysis (Supplementary Figure S1) and NIH sleep duration recommendations (7–8 h/day) [22]: (i) Group 1 (normal sleep duration, N = 2371): 7 to 8 h/day; (ii) Group 2 (N = 1106): 6 h/day; (3) Group 3 (N = 644): < 6 h/day; and (4) Group 4 (N = 278): > 8 h/day.
Vitamin D status
VD status included two aspects in this study: VD intake levels and serum 25(OH)D levels. For VD intake (D2 + D3), NHANES assessed the types and amounts of foods/beverages (including all types of water) consumed and dietary supplements used during the 24-h period prior to the interview and estimated the intakes of VD from those foods/beverages and dietary supplements. Information on VD intake was collected through in-person interviews and telephone surveys (3 to 10 days after the in-person interview). The dietary recall statuses were classified as (i) reliable and met the minimum criteria; (ii) not reliable or did not meet the minimum criteria; (iii) reported consuming breast milk (for infants); and (iv) not done. In the present study, we enrolled only participants with a dietary recall status that was “reliable and met the minimum criteria” in the final analysis. Moreover, to balance both methods (in person or by phone) of errors, we calculated the mean values between the two methods to investigate VD intake and used them as the final values of VD intake. Other details about the measurement of VD intake are available on the NHANES website [23]. Finally, according to the published Endocrine Society’s Practice Guidelines on Vitamin D [24], individuals were divided into two groups according to VD intake levels: (i) adequate VD intake: VD intake ≥ 15.00 μg/day; and (ii) inadequate VD intake: VD intake < 15.00 μg/day.
Serum 25(OH)D levels (D2 + D3) were detected in the serum of participants. Moreover, the quantitative detection of 25-hydroxyvitamin concentration was performed by ultra-high-performance liquid chromatography-tandem mass spectrometry. The lower limits of detection (LODs) for 25(OH)D2 and 25(OH)D3 were 2.05 nmol/L and 2.23 nmol/L, respectively. Serum 25(OH)D concentrations less than the LOD were imputed as LOD/√2. Other details about the detection of the serum 25(OH)D concentrations are available on the NHANES website [25]. Finally, the participants with different serum 25(OH)D levels were grouped into two categories according to the published Endocrine Society’s Practice Guidelines on Vitamin D [24]: (i) deficient/insufficient serum 25(OH)D levels: serum 25(OH)D < 75.00 nmol/L; (ii) sufficient serum 25(OH)D levels: serum 25(OH)D ≥ 75.00 nmol/L [individuals with ≥ 125 nmol/L serum 25(OH)D, which was considered to have potential toxic effects on human health [26], were also assigned to sufficient serum 25(OH)D levels group because the sample size was too small (N = 110)].
Covariates
Considering the impact of other factors on BMD, we controlled for potential variables to perform covariate-adjusted analyses. The selection of potential variables that might affect BMD was performed according to previous studies and accessibility data from the NHANES database [1, 27]. Finally, age, sex/menopause status (the definition and information extraction of menopause status referred to a previous study [28]), race, education level, income level, body mass index (BMI), smoking status, alcohol drinking status, physical activity level, sedentary activity, fracture history, glucocorticoid use, family history of osteoporosis, Charlson Comorbidity Index (CCI) (the definition and information extraction of CCI referred to a previous study [29]), calcium intake and caffeine intake were considered to be potential covariates in the present study. Other detailed information on the covariates is listed in Supplementary Table S1.
Statistical analysis
First, all analyses were based on participants with complete data; thus, the individuals with missing data on covariates were excluded from the final analysis. Second, the baseline characteristics were indicated by the mean/median (continuous variables) and proportion (categorical variable). Moreover, the normality of the continuous variables was tested with the Shapiro–Wilk normality test. If the data of the continuous variable were normally distributed, statistical significance was determined using Student’s t-test; if the data were nonnormally distributed, statistical significance was determined using the Kruskal–Wallis test. For categorical variables, statistical significance was determined using the chi-square test. Third, covariates associated with TF-BMD with a p-value of < 0.05 in univariate analysis were included in the multiple linear regression models. Finally, the differences in BMD between participants with normal sleep duration and any other group were also assessed using multiple linear regression models. All analyses were performed using R software (version 4.0.3; https://www.R-project.org) and EmpowerStats (version 2.0; http://www.empowerstats.com). P values < 0.05 were considered statistically significant.
Results
Participant selection and baseline characteristics
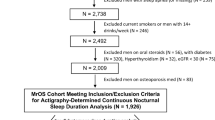
The flow chart of participant selection is displayed in Fig. 1. We extracted the information of 30,861 participants from the NHANES 2007–2014. First, we excluded subjects aged < 40 years of age (n = 18,886), subjects without complete BMD data (n = 5,365), subjects without SD data (n = 6), and subjects without VD status data (n = 1,356). Second, we excluded individuals with missing data on covariates (details on the missing covariate data are shown in Supplementary Fig. S2; n = 849), and a total of 4,399 participants were included in the final analysis.
The baseline characteristics of the individuals are listed in Table 1. Overall, the median age of the overall study population was 55.00 years old, with 46.97% of men and 53.03% of women distributed. Compared with individuals with 7–8 h of sleep per day, individuals with > 8 h of sleep per day showed lower TF-BMD and FN-BMD, while individuals with < 6 or > 8 h of sleep per day showed higher TF-BMD and FN-BMD than those with 7–8 h of sleep per day. Moreover, individuals sleeping < 6 h/ day showed lower vitamin D intakes than those sleeping 7–8 h/day. In addition, individuals with < 6 or 6 h of sleep per day showed lower serum 25(OH)D levels than those with 7–8 h of sleep per day. To make the results more intuitive, we also plotted the frequency histogram of the number of individuals with different VD intake and serum 25(OH)D. The frequency histogram is shown in Fig. 2.
Selection of covariates
We included fifteen candidate covariates in the univariate analysis and then selected covariates with a p-value of < 0.05 for association with TF-BMD. The results of the univariate analysis are presented in Supplementary Table S2. Finally, we included age, sex/menopause status, race, income level, BMI, smoking status, alcohol drinking status, physical activity level, fracture history, glucocorticoid use, family history of osteoporosis, CCI, calcium intake in the multiple linear regression models.
Association between sleep duration and BMD
Overall, individuals with > 8 h of sleep per day showed lower TF-BMD and FN-BMD than those with 7–8 h of sleep per day, while higher TF-BMD and FN-BMD were observed among individuals sleeping six or < 6 h/day in Model 1 (unadjusted model). Moreover, when age, sex/menopause status, race, and BMI were adjusted (Model 2), significant differences in TF-BMD and FN-BMD between individuals sleeping > 8 h/day and 7–8 h/day were observed. In addition, when all covariates, VD intakes, and serum 25(OH)D levels were adjusted (Model 3), the results suggested that participants with > 8 h of sleep per day had significantly lower TF-BMD and FN-BMD than those with 7–8 h of sleep per day. The specific results are listed in Fig. 3, Supplementary Tables S3 and S4.
Association between sleep duration and BMD. A overall population; B individuals aged < 60 years; C individuals aged ≥ 60 years; D men; E non-postmenopausal women; F postmenopausal women. Model 1: unadjusted model; Model 2: age, sex/menopause status, race, and BMI were adjusted; Model 3: age, sex/menopause status, race, income level, BMI, smoking status, alcohol drinking status, physical activity level, fractures history, glucocorticoid use, family history of osteoporosis, CCI, calcium intake, vitamin D intake, and serum 25-hydroxyvitamin D were adjusted. Group 1: SD = 7–8 h/day; Group 2: SD = 6 h/day; Group3: SD < 6 h/day; Group 4: SD > 8 h/day. BMD, bone mineral density; BMI, body mass index; CCI, Charlson Comorbidity Index; FN, femoral neck; SD, sleep duration; TF, total femur; TS, total spine. * p < 0.05; ** p < 0.01
When stratified by age, individuals (aged < 60 years) sleeping six h/night showed higher TF-BMD and FN-BMD, and individuals sleeping < 6 h/night showed higher FN-BMD than those with 7–8 h of sleep per day in Model 1. However, no significant differences in BMDs were observed in any abnormal sleep duration group (< 6, 6, or > 8 h/day) compared with the normal sleep duration group (7–8 h/day) in Model 2 and Model 3. Moreover, individuals (aged ≥ 60 years) sleeping > 8 h/day showed lower TF-BMD and FN-BMD than those sleeping 7–8 h/day, regardless of adjustment. The details are listed in Fig. 3, Supplementary Tables S3, and S4.
When stratified by sex/menopause status, men sleeping > 8 h/day showed lower TF-BMD and FN-BMD than those with 7–8 h of sleep per day in Model 1. Moreover, men sleeping > 8 h/day still showed lower TF-BMD, FN-BMD, and TS-BMD, and men sleeping < 6 h/day showed lower TF-BMD compared with those sleeping 7–8 h/day in Model 2. In addition, men sleeping > 8 h/night still showed lower TS-BMD than those sleeping 7–8 h/day in Model 3. Non-postmenopausal women sleeping < 6 h/day showed higher TF-BMD and FN-BMD than those sleeping 7–8 h/night in Model 1. Moreover, postmenopausal women sleeping > 8 h/day showed significantly lower TF-BMD and FN-BMD than those sleeping 7–8 h/day, regardless of adjustment. The details are listed in Fig. 3, Supplementary Tables S3 and S4.
Association between sleep duration and BMD in different vitamin D intake levels
Overall, in the inadequate VD intake group (< 15.00 µg/day), individuals sleeping > 8 h/day showed lower TF-BMD and FN-BMD than those sleeping 7–8 h/day in Model 1 (unadjusted model) and Model 2 (age, sex/ menopause status, race, and BMI were adjusted). Moreover, individuals sleeping > 8 h/night showed lower TF-BMD than those sleeping 7–8 h/day in Model 3 [all covariates and serum 25(OH)D levels were adjusted]. In the adequate VD intake group (≥ 15.00 µg/day), individuals sleeping six h/night showed higher FN-BMD, and individuals sleeping < 6 h/day showed higher TF-BMD and FN-BMD than those sleeping 7–8 h/day in Model 1. Moreover, individuals sleeping > 8 h/day showed lower TF-BMD than those sleeping 7–8 h/day in Model 2. However, no significant differences in BMDs were observed in any abnormal sleep duration group (< 6, 6, or > 8 h/day) compared with the normal sleep duration group (7–8 h/day) in Model 3. The details are listed in Fig. 4, Supplementary Tables S3 and S5.
Association between sleep duration and BMD in different vitamin D intake levels. A overall population; B individuals aged < 60 years; C individuals aged ≥ 60 years; D men; E non-postmenopausal women; F postmenopausal women. Model 1: unadjusted model; Model 2: age, sex/menopause status, race, and BMI were adjusted; Model 3: age, sex/menopause status, race, income level, BMI, smoking status, alcohol drinking status, physical activity level, fractures history, glucocorticoid use, family history of osteoporosis, CCI, calcium intake, and serum 25-hydroxyvitamin D were adjusted. Group 1: SD = 7–8 h/day; Group 2: SD = 6 h/day; Group3: SD < 6 h/day; Group 4: SD > 8 h/day. BMD, bone mineral density; BMI, body mass index; CCI, Charlson Comorbidity Index; FN, femoral neck; SD, sleep duration; TF, total femur; TS, total spine. * p < 0.05; ** p < 0.01
When stratified by age, among subjects with inadequate VD intake, individuals (aged ≥ 60 years) sleeping > 8 h/day showed significantly lower TF-BMD (Model 1–3), FN-BMD (Model 1–3), and TS-BMD (Model 2) than those sleeping 7–8 h/day. In the adequate VD intake group, individuals (aged < 60 years) sleeping < 6 h/ day showed higher TF-BMD and FN-BMD than the control group in Model 1. Moreover, individuals (aged ≥ 60 years) sleeping > 8 h/day showed lower TF-BMD and FN-BMD than those sleeping 7–8 h/night in Model 2. The details are listed in Fig. 4, Supplementary Tables S3 and S5.
When stratified by sex/menopause status, in the inadequate VD intake group, non-postmenopausal women sleeping < 6 h/day showed higher TF-BMD (Model 1) than those sleeping 7–8 h/day. Moreover, men sleeping > 8 h/day showed significantly lower TF-BMD (Model 1–2), FN-BMD (Model 1–3), and TS-BMD (Model 1–3) than those sleeping 7–8 h/day. In addition, postmenopausal women sleeping > 8 h/day showed significantly lower TF-BMD (Model 1–3) and FN-BMD (Model 1–2) than those sleeping 7–8 h/day. In the adequate VD intake group, non-postmenopausal women sleeping < 6 h/day showed higher FN-BMD (Model 1) than those sleeping 7–8 h/day. Moreover, postmenopausal women sleeping > 8 h/day showed lower FN-BMD (Model 2–3) than those sleeping 7–8 h/day. The details are listed in Fig. 4, Supplementary Tables S3 and S5.
Association between sleep duration and BMD in different serum 25(OH) levels
Overall, in the deficient/insufficient serum 25(OH)D group (0.00 ≤ serum 25(OH)D < 75.00 nmol/L), individuals with > 8 h of sleep per day showed lower TF-BMD and FN-BMD than those with 7–8 h of sleep per night in Model 1 (unadjusted model) and Model 2 ((age, sex/menopause, race, and BMI were adjusted). Moreover, individuals sleeping > 8 h/day showed lower TF-BMD than those sleeping 7–8 h/day in Model 3 (all covariates and VD intakes were adjusted). In the sufficient serum 25(OH)D group (serum 25(OH)D ≥ 75.00 nmol/L), individuals sleeping < 6 h/day showed higher TF-BMD and FN-BMD than those sleeping 7–8 h/day in Model 1. Moreover, individuals sleeping > 8 h/day showed lower TF-BMD than those sleeping 7–8 h/day in Model 2. In addition, individuals sleeping six h/day showed lower TS-BMD than those sleeping 7–8 h/day in Model 2 and Model 3. The details are listed in Fig. 5, Supplementary Tables S3 and S6.
Association between sleep duration and BMD in different serum 25(OH) levels. A overall population; B individuals aged < 60 years; C individuals aged ≥ 60 years; D men; E non-postmenopausal women; F postmenopausal women. Model 1: unadjusted model; Model 2: age, sex/menopause status, race, and BMI were adjusted; Model 3: age, sex/menopause status, race, income level, BMI, smoking status, alcohol drinking status, physical activity level, fractures history, glucocorticoid use, family history of osteoporosis, CCI, calcium intake, and vitamin D intake were adjusted. Group 1: SD = 7–8 h/day; Group 2: SD = 6 h/day; Group3: SD < 6 h/day; Group 4: SD > 8 h/day. BMD, bone mineral density; BMI, body mass index; CCI, Charlson Comorbidity Index; FN, femoral neck; SD, sleep duration; TF, total femur; TS, total spine; 25(OH)D, 25-hydroxyvitamin D. * p < 0.05; ** p < 0.01
When stratified by age, in the deficient/insufficient serum 25(OH)D group, individuals (aged < 60 years) sleeping six h/night had higher TF-BMD, FN-BMD, and TS-BMD than the control group (7–8 h/night) in Model 1. Moreover, individuals (aged ≥ 60 years) sleeping > 8 h/night showed lower TF-BMD (Model 1–3) and FN-BMD (Model 1–2) than the control group. In the sufficient serum 25(OH)D group, individuals (aged ≥ 60 years) sleeping > 8 h/night showed lower TF-BMD and FN-BMD than those sleeping 7–8 h/night (Model 2), while no significant differences were observed among individuals aged < 60 years. The details are listed in Fig. 5, Supplementary Tables S3 and S6.
When stratified by sex, in the deficient/insufficient serum 25(OH)D group, men sleeping < 6 h/day showed lower TF-BMD (Model 2), and men sleeping > 8 h/day showed significantly lower TF-BMD (Model 2) and TS-BMD (Model 2–3) than those sleeping 7–8 h/day. Moreover, non-postmenopausal women sleeping < 6 h/day showed higher TF-BMD and FN-BMD, and non-postmenopausal women sleeping six h/day showed higher TS-BMD than those sleeping 7–8 h/day in Model 1. In addition, postmenopausal women sleeping > 8 h/day showed significantly lower TF-BMD and FN-BMD than those sleeping 7–8 h/day in Model 2 and Model 3. In the sufficient serum 25(OH)D group, men sleeping > 8 h/night showed lower FN-BMD than the control group in Model 1, and postmenopausal women sleeping > 8 h/day showed significantly lower TF-BMD than those sleeping 7–8 h/day in Model 1. The details are listed in Fig. 5, Supplementary Tables S3 and S6.
Discussion
Osteoporosis in middle-aged and older individuals has become a global issue in the past decade. Currently, there is an increasing awareness that dietary changes and lifestyle modification might be effective means to prevent osteoporosis. Our study found that unhealthy sleep duration (especially > 8 h/night) was associated with reduced BMD. Moreover, the negative effect of unhealthy sleep duration on BMD was more salient among older individuals (aged ≥ 60 years), men, postmenopausal women, and subjects with inadequate VD intake or deficient/insufficient serum 25(OH)D levels.
Some previous studies demonstrated that unhealthy sleep duration was associated with decreased BMD or increased risk of osteoporosis [9, 10, 30,31,32]. For example, Ochs-Balcom et al. observed that women with short sleep duration (≤ 5 h/per night) showed lower BMD and higher risk of low bone mass and osteoporosis than individuals with a 7-h sleep duration [30]. Tian et al. found that participants with a long sleep duration (≥ 9 h) had a higher risk of osteoporosis than those with sleep durations of 7–8 h regardless of sex [31]. A meta-analysis conducted by Wang et al. demonstrated that each one-hour reduction in sleep duration increased the risk of osteoporosis 1.03-fold, while a one-hour increment in sleep duration increased the risk of osteoporosis 1.01-fold [32]. The negative effect of unhealthy sleep duration on bone metabolism might involve the following mechanisms. First, unhealthy sleep duration might lead to reduced bone mass by affecting mechanical stress. As previously reported, mechanical stress plays an important role in maintaining bone mass [33, 34]. Moreover, mechanical stress is reduced during sleep, and long sleep duration might decrease the effect of mechanical stress on bone formation, which might be a possible explanation for the negative effect of long sleep duration on reduced bone mass. Second, unhealthy sleep duration might lead to reduced bone mass by affecting hormone levels in the body. For example, estrogen is considered the chief regulator of the balance between bone formation and resorption [35]. Michels et al. found that a one-hour increase in sleep duration was associated with a 0.039-fold increase in mean estradiol concentrations among women [36]. However, more studies to investigate whether unhealthy sleep duration leads to low BMD by affecting estrogen levels are needed because the number of related studies is limited. Moreover, melatonin has been shown to have an inhibitory effect on bone resorption and a promoting effect on bone formation. which received increasing attention in recent years because it is one of the most important factors in circadian regulation and plays a role in bone metabolism [37, 38]. Wu et al. observed that women with sleep durations ≥ 9 h showed 42% higher melatonin levels than those with sleep durations ≤ 6 h [39]. These results suggested that unhealthy sleep duration might influence BMD by affecting melatonin levels.
VD, a pro-hormone, is considered to play an essential role in bone metabolism [11, 12, 40]. On the one hand, VD could facilitate the intestinal absorption of calcium, which is an important metal ion in bone formation [11, 12, 40]. On the other hand, VD levels are closely related to parathyroid hormone (PTH) levels [12, 40]. PTH plays a crucial role in bone metabolism and calcium homeostasis. PTH is a major stimulator of VD synthesis in the kidney, and the levels of PTH are also regulated in a negative-feedback manner by VD [40]. Moreover, several studies demonstrated that there existed an intrinsic circadian rhythm of PTH secretion (two peaks: early morning and late evening) [41,42,43,44], which was affected by age and menopause status [41]. In addition, sleep duration might influence the rhythm of PTH and lead to a change in PTH levels. For example, Staab et al. observed a non-significant, but numerically, reduction in PTH levels caused by a short-term sleep restriction [45]. Therefore, long or short sleep duration might lead to decreased BMD by affecting the rhythm or levels of PTH, which is also a possible reason for the observed results that the negative effect of unhealthy sleep duration on BMD was more salient among individuals with inadequate VD status. Unfortunately, the information on PTH levels was not obtainable from the NHANES database. Therefore, we could not evaluate the level of PTH of the study population in the present study. However, this point mentioned above might be a topic worth pursuing in the future. Serum 25(OH)D, a precursor of activated VD, was considered an ideal indicator to reflect the storage of VD in the body [11, 12]. In the present study, we observed that the negative effects of unhealthy sleep duration on BMD were more obvious among individuals with inadequate VD intake or deficient/insufficient serum 25(OH)D levels, which suggested that VD status might influence the association between sleep duration and BMD or that sleep duration affects BMD by influencing VD levels in the body. In addition to bone metabolism, VD has also been associated with sleep, which is a complex concept including sleep duration and sleep quality, bedtime, and other aspects. A meta-analysis by Gao et al. found that VD deficiency was associated with poor sleep quality and sleepiness but not short sleep duration [15]. Similarly, Cheng et al. observed that women with plasma 25(OH)D deficiency showed a high risk of poor sleep quality [46]. Likewise, sleep behaviors might also affect the VD status. For example, de Oliveira et al. observed that short sleep duration (< 6 h/day) was independently associated with low serum 25(OH)D levels among men [17]. Moreover, some studies demonstrated that other factors involved in sleep were also associated with the risk of bone loss or osteoporosis. For example, Tang et al. found that some unhealthy sleep patterns (defined by sleep duration and bedtime) were associated with low femur BMD and a high risk of osteoporosis [47]. Similarly, Tian et al. found that individuals with long sleep duration (≥ 9 h) and early bedtime (sleep before 21:00 h) showed a high risk of osteoporosis [31]. In addition, Bevilacqua et al. found that self-reported sleep quality was associated with BMD in older adults [48]. Therefore, reduced BMD might be caused by low VD intake or low serum 25(OH)D levels, which affect sleep duration or other sleep-related behaviors or parameters. In comparison, sleep duration might affect BMD by influencing VD levels in the body, which might also be a plausible explanation for the negative effects of unhealthy sleep duration, especially long sleep duration, on BMD. Adequate VD intake is obviously important, but sun exposure also plays an essential role in maintaining adequate levels of activated VD [49]. On the one hand, long sleep duration might reduce the time of sun exposure, thus leading to VD deficiency. On the other hand, we speculate that unhealthy sleep duration might diminish the ability of the skin to produce VD, but this postulation needs further examination. Conversely, we also observed that postmenopausal women sleeping > 8 h/night showed lower FN-BMD than the control group (7–8 h/night) in those with adequate VD intake, which suggested that the complexity of the interaction between VD status and sleep duration. However, no significant differences were observed among female individuals with sufficient serum 25(OH)D levels. Moreover, the published Endocrine Society’s Practice Guidelines on Vitamin D also recommended that raising the blood level of 25(OH)D above 75 nmol/L may require at least 1500–2000 IU/d (37.5–50.0 µg/day) of supplemental VD [24]. These findings above suggested that 15 µg/day of VD intake might be inadequate, especially for women. In addition, because of the cross-sectional design of the present study, the causality requires further investigation.
In the present study, we observed that the adverse effects of abnormal sleep duration on BMD were more pronounced in individuals aged ≥ 60 years. On the one hand, it was consistently shown that aging was an important factor in bone loss [1], and individuals who were older appeared to have lower BMDs than those who were younger. On the other hand, aging was also associated with reduced hormone levels, especially sex hormones [50, 51], and older subjects seemed to have worse adaptability to the changes in metabolic or hormone levels caused by other factors. Moreover, we observed that the association between VD status and the negative effect of unhealthy sleep duration on BMD was different between men and women. On the one hand, the sex differences might result from the small sample size of the included population. On the other hand, the sex differences might suggest differences in VD requirements to maintain normal bone metabolism for men and women. The leading cause of bone loss among women is natural menopause [52]. Estrogen levels gradually decrease in older women after menopause, which disturbs the balance of bone metabolism and leads to diminished bone mass [52]. In comparison, the most important reason for bone loss or osteoporosis among men is aging, and the rate of disease progression among men was slower than that among women [1, 53]. Therefore, the theory presented above might explain the sex differences. Interestingly, we also observed differences in affected sites (femur or spine). Although there was no clear evidence to explain the differences in affected sites, several reasonable explanations can be put forth to account for this observation. For example, the biomechanical features of the femur and spine are different. Although the mechanical stimulus or stress on the femur and spine is lower during sleep, the mechanical stimulus or stress on the femur and spine generated by different physical activities might be different, which might be a reason for the differences in affected sites. For example, Hind et al. found that participants who participated in > 2 weeks of resistance training had significantly higher lumbar spine but not hip BMD than those who participated in < 2 weeks of resistance training [54]. However, considering that the type of physical activity could not be assessed among the individuals included, the differences in affected sites might result from the small sample size. Therefore, more studies will be needed to determine whether differences in affected sites exist and the detailed mechanism.
The findings of the present study might provide some valuable suggestions for clinical practice. First, our study revealed that unhealthy sleep duration might contribute to reduced bone mass. Therefore, maintaining a healthy sleep duration might be an effective approach to prevent bone loss. Moreover, this study revealed that the negative effect of unhealthy sleep duration on BMD might be affected by VD status, especially among individuals with inadequate VD intake or deficient/insufficient serum 25(OH)D levels. Therefore, adequate VD intake to maintain sufficient serum 25(OH)D levels might be a potential means to prevent the adverse effects of abnormal sleep duration on BMD. However, given the limitations of the present study (such as the cross-sectional study design), the causality between sleep duration and BMD and the specific role played by VD still need further investigation.
This study also had some limitations. First, only individuals with complete data were included, and subjects with missing data were excluded from the present study, which might produce bias. Second, sleep duration and dietary data were collected based on self-reports, which might not accurately reflect the actual situation and introduce recall bias. Third, the participants included in the final analysis were based on the general US population. Considering the differences in culture, lifestyle, and diet among different countries and regions, more studies are needed to investigate whether the conclusion of the present study is generally applicable. Fourth, the VD intake and sleep duration data were collected based on short-term intake, using short-term dietary intake as usual intake to assess whether VD intakes influenced the association between sleep duration and BMD, which might lead to a biased estimate. Fifth, some unmeasured confounding variables (such as medication use, PTH levels, bone turnover markers, sleep onset, and daylight hours), which are also considered important factors for bone metabolism and sleep behaviors, were not assessed in the present study because these variables were not available in the NHANES database, and the lack of adjustment for these potential factors may bias the results. Finally, the causality between sleep duration and BMD could not be established because this study was represented by a cross-sectional design.
Conclusions
In conclusion, unhealthy sleep duration, especially long sleep duration, was associated with decreased BMD, particularly among individuals aged > 60 years, men, or postmenopausal women. Moreover, VD status might influence the association between sleep duration and BMD, especially in the context of inadequate VD intake or deficient/insufficient serum 25(OH)D levels. However, given the limitations of the present study, further investigation is warranted to confirm this association and to explore potential mechanisms.
Availability of data and materials
The datasets obtained and analysed during the current study are available on the NHANES database [https://www.cdc.gov/nchs/nhanes/index.htm].
References
Compston JE, McClung MR, Leslie WD. Osteoporosis. Lancet. 2019;393:364–76.
Kanis JA, Johnell O, Oden A, Sembo I, Redlund-Johnell I, Dawson A, De Laet C, Jonsson B. Long-term risk of osteoporotic fracture in Malmö. Osteoporos Int. 2000;11:669–74.
Melton LJ 3rd, Atkinson EJ, O’Connor MK, O’Fallon WM, Riggs BL. Bone density and fracture risk in men. J Bone Miner Res. 1998;13:1915–23.
IOF. Epidemiology of osteoporosis. 2021. https://www.osteoporosis.foundation/health-professionals/about-osteoporosis/epidemiology. Accessed 1 Dec 2021.
Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005;16(Suppl 2):S3-7.
Lu J, Ren Z, Liu X, Xu YJ, Liu Q. Osteoporotic fracture guidelines and medical education related to the clinical practices: a nationwide survey in China. Orthop Surg. 2019;11:569–77.
Fu X, Zhao X, Lu H, Jiang F, Ma X, Zhu S. Association between sleep duration and bone mineral density in Chinese women. Bone. 2011;49:1062–6.
Wang K, Wu Y, Yang Y, Chen J, Zhang D, Hu Y, Liu Z, Xu J, Shen Q, Zhang N, et al. The associations of bedtime, nocturnal, and daytime sleep duration with bone mineral density in pre- and post-menopausal women. Endocrine. 2015;49:538–48.
Swanson CM, Blatchford PJ, Orwoll ES, Cauley JA, LeBlanc ES, Fink HA, Wright KP Jr, Wierman ME, Kohrt WM, Stone KL. Association between objective sleep duration and bone mineral density in older postmenopausal women from the Study of Osteoporotic Fractures (SOF). Osteoporos Int. 2019;30:2087–98.
Swanson CM, Blatchford PJ, Stone KL, Cauley JA, Lane NE, Rogers-Soeder TS, Redline S, Bauer DC, Wright KP Jr, Wierman ME, et al. Sleep duration and bone health measures in older men. Osteoporos Int. 2021;32:515–27.
Anderson PH. Vitamin D Activity and Metabolism in Bone. Curr Osteoporos Rep. 2017;15:443–9.
Lips P, van Schoor NM. The effect of vitamin D on bone and osteoporosis. Best Pract Res Clin Endocrinol Metab. 2011;25:585–91.
McCarty DE, Chesson AL Jr, Jain SK, Marino AA. The link between vitamin D metabolism and sleep medicine. Sleep Med Rev. 2014;18:311–9.
Huiberts LM, Smolders K. Effects of vitamin D on mood and sleep in the healthy population: interpretations from the serotonergic pathway. Sleep Med Rev. 2021;55: 101379.
Gao Q, Kou T, Zhuang B, Ren Y, Dong X, Wang Q. The association between Vitamin D deficiency and sleep disorders: a systematic review and meta-analysis. Nutrients. 2018;10(10):1395.
Majid MS, Ahmad HS, Bizhan H, Hosein HZM, Mohammad A. The effect of vitamin D supplement on the score and quality of sleep in 20–50 year-old people with sleep disorders compared with control group. Nutr Neurosci. 2018;21:511–9.
de Oliveira DL, Dokkedal-Silva V, Fernandes GL, Kim LJ, Tufik S, Andersen ML. Sleep duration as an independent factor associated with vitamin D levels in the EPISONO cohort. J Clin Sleep Med. 2021;17:2439–49.
CDC. National Health and Nutrition Examination Survey. 2021. https://wwwn.cdc.gov/nchs/nhanes/. Accessed 1 Dec 2021.
CDC. NCHS Research Ethics Review Board (ERB) Approval. 2021. https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2007. Accessed 1 Dec 2021.
CDC. Body Composition Procedures Manual. 2021. https://wwwn.cdc.gov/nchs/data/nhanes/2013-2014/manuals/2013_Body_Composition_DXA.pdf. Accessed 1 Dec 2021.
CDC. Sleep Disorders. 2021. https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/SLQ_H.htm. Accessed 1 Dec 2021.
National Heart L, and Blood Institute. Explore sleep deprivation and deficiency: How much sleep is enough? 2012. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency. Accessed 1 Dec 2021.
CDC. Dietary Interview - Total Nutrient Intakes. 2021. https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/DR1TOT_H.htm. Accessed 1 Dec 2021.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–30.
CDC. Vitamin D. 2021. https://wwwn.cdc.gov/nchs/nhanes/2013-2014/VID_H.htm. Accessed 1 Dec 2021.
Institute of Medicine Committee to Review Dietary Reference Intakes for Vitamin D, Calcium: The National Academies Collection: Reports funded by National Institutes of Health. In Dietary Reference Intakes for Calcium and Vitamin D. Edited by Ross AC, Taylor CL, Yaktine AL, Del Valle HB. Washington (DC): National Academies Press (US) Copyright © 2011, National Academy of Sciences.; 2011
Weaver CM, Gordon CM, Janz KF, Kalkwarf HJ, Lappe JM, Lewis R, O’Karma M, Wallace TC, Zemel BS. The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations. Osteoporos Int. 2016;27:1281–386.
Tang Y, Peng B, Liu J, Liu Z, Xia Y, Geng B. Systemic immune-inflammation index and bone mineral density in postmenopausal women: a cross-sectional study of the national health and nutrition examination survey (NHANES) 2007–2018. Front Immunol. 2022;13: 975400.
Zhao H, Pan Y, Wang C, Guo Y, Yao N, Wang H, Li B. The effects of metal exposures on charlson comorbidity index using zero-inflated negative binomial regression model: NHANES 2011–2016. Biol Trace Elem Res. 2021;199:2104–11.
Ochs-Balcom HM, Hovey KM, Andrews C, Cauley JA, Hale L, Li W, Bea JW, Sarto GE, Stefanick ML, Stone KL, et al. Short sleep is associated with low bone mineral density and osteoporosis in the women’s health initiative. J Bone Miner Res. 2020;35:261–8.
Tian Y, Shen L, Wu J, Xu G, Yang S, Song L, Zhang Y, Mandiwa C, Yang H, Liang Y, Wang Y. Sleep duration and timing in relation to osteoporosis in an elderly Chinese population: a cross-sectional analysis in the Dongfeng-Tongji cohort study. Osteoporos Int. 2015;26:2641–8.
Wang D, Ruan W, Peng Y, Li W. Sleep duration and the risk of osteoporosis among middle-aged and elderly adults: a dose-response meta-analysis. Osteoporos Int. 2018;29:1689–95.
Yuan Y, Zhang L, Tong X, Zhang M, Zhao Y, Guo J, Lei L, Chen X, Tickner J, Xu J, Zou J. Mechanical stress regulates bone metabolism through MicroRNAs. J Cell Physiol. 2017;232:1239–45.
Somemura S, Kumai T, Yatabe K, Sasaki C, Fujiya H, Niki H, Yudoh K. Physiologic mechanical stress directly induces bone formation by activating glucose Transporter 1 (Glut 1) in Osteoblasts, inducing signaling via NAD+-Dependent Deacetylase (Sirtuin 1) and Runt-Related transcription factor 2 (Runx2). Int J Mol Sci. 2021;22(16):9070.
Khosla S, Oursler MJ, Monroe DG. Estrogen and the skeleton. Trends Endocrinol Metab. 2012;23:576–81.
Michels KA, Mendola P, Schliep KC, Yeung EH, Ye A, Dunietz GL, Wactawski-Wende J, Kim K, Freeman JR, Schisterman EF, Mumford SL. The influences of sleep duration, chronotype, and nightwork on the ovarian cycle. Chronobiol Int. 2020;37:260–71.
Li T, Jiang S, Lu C, Yang W, Yang Z, Hu W, Xin Z, Yang Y. Melatonin: another avenue for treating osteoporosis? J Pineal Res. 2019;66: e12548.
Swanson CM, Kohrt WM, Buxton OM, Everson CA, Wright KP Jr, Orwoll ES, Shea SA. The importance of the circadian system & sleep for bone health. Metabolism. 2018;84:28–43.
Wu AH, Wang R, Koh WP, Stanczyk FZ, Lee HP, Yu MC. Sleep duration, melatonin and breast cancer among Chinese women in Singapore. Carcinogenesis. 2008;29:1244–8.
Khundmiri SJ, Murray RD, Lederer E. PTH and Vitamin D Compr Physiol. 2016;6:561–601.
Diemar SS, Dahl SS, West AS, Simonsen SA, Iversen HK, Jørgensen NR: A Systematic Review of the Circadian Rhythm of Bone Markers in Blood. Calcif Tissue Int. 2022.
Heshmati HM, Riggs BL, Burritt MF, McAlister CA, Wollan PC, Khosla S. Effects of the circadian variation in serum cortisol on markers of bone turnover and calcium homeostasis in normal postmenopausal women. J Clin Endocrinol Metab. 1998;83:751–6.
el-Hajj Fuleihan G, Klerman EB, Brown EN, Choe Y, Brown EM, Czeisler CA. The parathyroid hormone circadian rhythm is truly endogenous--a general clinical research center study. J Clin Endocrinol Metab. 1997;82:281–6.
Rejnmark L, Lauridsen AL, Vestergaard P, Heickendorff L, Andreasen F, Mosekilde L. Diurnal rhythm of plasma 1,25-dihydroxyvitamin D and vitamin D-binding protein in postmenopausal women: relationship to plasma parathyroid hormone and calcium and phosphate metabolism. Eur J Endocrinol. 2002;146:635–42.
Staab JS, Smith TJ, Wilson M, Montain SJ, Gaffney-Stomberg E. Bone turnover is altered during 72 h of sleep restriction: a controlled laboratory study. Endocrine. 2019;65:192–9.
Cheng TS, Loy SL, Cheung YB, Cai S, Colega MT, Godfrey KM, Chong YS, Tan KH, Shek LP, Lee YS, et al. Plasma Vitamin D deficiency is associated with poor sleep quality and night-time eating at mid-pregnancy in Singapore. Nutrients. 2017;9(4):340.
Tang Y, Wang S, Yi Q, Xia Y, Geng B. Sleep pattern and bone mineral density: a cross-sectional study of National Health and Nutrition Examination Survey (NHANES) 2017–2018. Arch Osteoporos. 2021;16:157.
Bevilacqua G, Denison HJ, Laskou F, Jameson KA, Ward KA, Cooper C, Dennison EM. Self-reported sleep quality and bone outcomes in older adults: findings from the hertfordshire cohort study. Calcif Tissue Int. 2020;106:455–64.
Saraff V, Shaw N. Sunshine and vitamin D. Arch Dis Child. 2016;101:190–2.
Horstman AM, Dillon EL, Urban RJ, Sheffield-Moore M. The role of androgens and estrogens on healthy aging and longevity. J Gerontol A Biol Sci Med Sci. 2012;67:1140–52.
Araujo AB, Wittert GA. Endocrinology of the aging male. Best Pract Res Clin Endocrinol Metab. 2011;25:303–19.
Eastell R, O’Neill TW, Hofbauer LC, Langdahl B, Reid IR, Gold DT, Cummings SR. Postmenopausal osteoporosis Nat Rev Dis Primers. 2016;2:16069.
Walsh JS, Eastell R. Osteoporosis in men. Nat Rev Endocrinol. 2013;9:637–45.
Hind K, Truscott JG, Evans JA. Low lumbar spine bone mineral density in both male and female endurance runners. Bone. 2006;39:880–5.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (81874017; 81960403; 82060405), Cuiying Scientific and Technological Innovation Program of Lanzhou University Second Hospital (CY2017-ZD02; CY2021-MS-A07), and Innovation Star Project for Excellent Graduate Students of the Education Department of Gansu Province (2021CXZX-143). At the same time, we would like to express our gratitude to American Journal Experts (https://www.aje.com/) for the language editing services provided.
Funding
This work was supported by the National Natural Science Foundation of China (81874017; 81960403; 82060405), Cuiying Scientific and Technological Innovation Program of Lanzhou University Second Hospital (CY2017-ZD02; CY2021-MS-A07), and Innovation Star Project for Excellent Graduate Students of the Education Department of Gansu Province (2021CXZX-143).
Author information
Authors and Affiliations
Contributions
YT and JL have contributed equally to this work. YT: Conceptualization, Methodology, Software, Formal analysis, Data Curation, Writing—Original Draft, Writing—Review & Editing, Funding acquisition; JL: Methodology, Validation, Investigation, Writing—Original Draft, Writing—Review & Editing; ZF: Software, Data Curation, Visualization; ZL: Validation, Writing—Review & Editing; SW: Formal analysis, Visualization; YX: Conceptualization, Writing—Review & Editing, Supervision, Funding acquisition; BG: Conceptualization, Methodology, Writing—Review & Editing, Supervision, Funding acquisition. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All analyses were based on data of the National Health and Nutrition Examination Survey (NHANES). The study was approved by the ethics review board of the National Center for Health Statistics. The National Center for Health Statistics Ethics Review Board protocol numbers are Continuation of Protocol #2005–06 (NHANES 2007–2008), Continuation of Protocol #2005–06 (NHANES 2009–2010), and Continuation of Protocol #2011–17 (NHANES 2013–2014), respectively. The detailed information located on the NHANES website. Written informed consent was obtained from each participant before their inclusion on the NHANES database. Detailed information on the ethics application and written informed consent are provided on the NHANES website.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Figure S1.
Frequency distribution of sleep duration among all individuals included in the final analysis. Supplementary Figure S2. Frequency distribution of sleep duration among all individuals included in the final analysis. Supplementary Table S1. Detailed information on covariates. Supplementary Table S2. Univariate analysis for the association between covariates and total femur BMD. Supplementary Table S3. Number of participants in each subgroup. Supplementary Table S4. Association between sleep duration and BMD. Supplementary Table S5. Association between sleep duration and BMD in different vitamin D intake levels. Supplementary Table S6. Association between sleep duration and BMD in different serum 25(OH) levels.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tang, Y., Liu, J., Feng, Z. et al. Nocturnal sleep duration and bone mineral density: a cross-sectional study of the National Health and Nutrition Examination Survey (NHANES) 2007–2014. BMC Endocr Disord 22, 333 (2022). https://doi.org/10.1186/s12902-022-01259-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-022-01259-1