Abstract
Background
Several studies have assessed the relationship between type 2 diabetes (T2D) and tooth loss; however, results have been inconsistent. Therefore, the present systematic review and meta-analysis of observational studies was designed to examine the association between T2D and tooth loss.
Methods
This systematic review and meta-analysis was conducted based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Guideline. We searched all the relevant studies in international databases of Scopus, PubMed, ProQuest, Web of Science, Cochrane Library, and Google scholar search engine until February 2022. The heterogeneity of the studies was calculated using the I2 index. Measure of effect and 95% confidence interval (CI) were extracted from each study. The results of the study were analyzed using the random effects model.
Results
In the present study, 22 eligible studies were included. Meta-analysis of unadjusted and adjusted results showed that T2D significantly increased the risk of tooth loss, and Odds Ratio (OR) unadjusted was 1.87 (95% CI: 1.62–2.13, p < 0.001), and OR adjusted was 1.20 (95% CI: 1.10–1.30, p < 0.001), respectively. Subgroup analysis based on study design for adjusted OR indicated that in the cohort study (OR: 1.29, 95% CI: 1.07–1.51), in the cross-sectional study (OR: 1.15, 95% CI: 1.06–1.23), and in the case-control study (OR: 5.10, 95% CI: 1.01–9.18) there was a significant association between T2D and tooth loss. Other subgroups analyses showed consistent results and no publication bias existed.
Conclusions
The findings suggest that T2D is associated with increased risk of tooth loss. This conclusion may provide useful evidence for correlated clinical researches.
Similar content being viewed by others
Introduction
Diabetes mellitus is a chronic metabolic disease characterized by hyperglycemia caused by defects in insulin secretion, insulin function, or both. It is divided into two types: type 1 and type 2 diabetes [1, 2]. Diabetes mellitus is a global health problem affecting 463 million people aged 20–79 years in 2019, projected to rise to 700 million by 2045 [3]. The estimated global direct health expenditure on diabetes in 2019 is United States dollar (USD) 760 billion and is expected to grow to a projected USD 825 billion by 2030 and USD 845 billion by 2045. There is a wide variation in annual health expenditures on diabetes [4]. About one-third of people with diabetes are unaware of their illness, and many go undiagnosed until the onset of symptoms [5]. Diabetes has complications such as retinopathy, neuropathy, microvascular and macrovascular changes, and oral complications such as tooth decay, periodontal disease, dry mouth, and tooth loss [2, 6]. Diabetes increases the risk of oral disease directly (e.g., gingival inflammatory response) and indirectly (e.g., decreased saliva production due to medication) [7]. About one-third of people with diabetes have severe periodontal disease (periodontitis) or severe gum disease In people with diabetes, periodontal disease eventually leads to the loss of one or more teeth [8]. Indeed, periodontitis, also known as gum disease, is a serious infection of the gums that can damage soft tissue and, if left untreated, the bone that supports your teeth. Periodontitis can cause teeth to loosen or cause teeth loss [9]. In fact, the American Dental Association has published a new study that believes that one in five cases of tooth loss is related to diabetes [10]. In addition, most of these studies [11,12,13] showed that very few patients diagnosed with diabetes visit their dentist regularly for periodontal exams, and many patients are unaware of the impact of diabetes on oral health. They do not even know that diabetes can cause tooth loss [14]. Severe tooth decay and chronic periodontal disease are the main causes of tooth loss in adults [15, 16]. The severity and prevalence of tooth loss is still a major problem in many countries around the world [17]. According to the National Health and Nutrition Examination Survey (NHANES), the prevalence of edentulous among people aged 60 and older was 31 and 25% between 1988 and 1994 and 1999–2002, respectively. In addition, the average number of teeth in the mouth of people aged 60 and over during these years was 18.4 and 19.4, respectively [18]. Although the prevalence of tooth loss has decreased over the past few decades, it is still a major public health problem [7]. Tooth loss and complete edentulous are both poor health outcomes that negatively affect a person’s quality of life [18, 19]. Elderly people with diabetes have more teeth lost and a lower quality of life than non-diabetics [20].
Oral health is a very important factor in increasing the quality of life despite increasing attention and dental care, various risk factors such as: age, socioeconomic status [7, 18, 21], gender, race and ethnicity [19], level of education, family income, geographical location, access to care, history of smoking, insurance [18, 22], lifestyle, oral hygiene habits and regular visits to the dentist [21]. Adverse effects of tooth loss include: difficulty chewing, difficulty speaking, difficulty smiling, cosmetic problems, negative social points such as interacting with others, and social isolation [7, 18]. Absence of fiber and vegetables and eating more cholesterol and fatty foods [6, 23] or high-carbohydrate diets [19], can reduce cognitive function and increase vulnerability to serious and fatal infections [7, 24]. The findings suggest that tooth loss is independently associated with chronic diseases such as cardiovascular disease, hypertension, stroke, cancer and other systemic diseases [19, 25]. The increased incidence of oral health problems may be due to the rapid increase in T2D and obesity in adults, especially in African Americans [7]. Several studies have evaluated the relationship between T2D and tooth loss; however, the results have been inconsistent [26,27,28,29,30]. Although there have been meta-analyses on the relationship between T2D and periodontitis that have evaluated predictors of tooth loss in patients with periodontitis, including Diabetes Mellitus (DM) [31]. In addition, another meta-analysis of tooth loss and diabetes risk was conducted in recent years with a limited number of studies [32]. Therefore, we conducted the meta-analysis on the number of further studies and subgroup analyses including study type, continent, method of diagnosing diabetes, quality of studies, number of missing teeth, adjusted and unadjusted for confounding factors in calculating effect size in assessing of association between T2D with tooth loss.
Methods
This systematic review and meta-analysis was reported in according to referred reporting items for systematic reviews and meta-analyses (PRISMA) guideline [33]. This review is not part of a registry for systematic reviews and the protocol has not been published.
Search strategy and data sources
Literature search were conducted for English evidences in PubMed/Medline, Scopus, ProQuest and Web of Sciences up to February 2022. The following keywords were used: ‘Tooth’ OR ‘teeth’ AND ‘Loss’ AND ‘diabet*’ OR ‘Prediabet*’ OR ‘Glucose Intolerance’. No restriction for publication date was applied. Full search strategies for all sources are listed in Appendix 1. We also performed a manual search of related articles’ references to avoid missing any relevant published papers. Two reviewers independently screened the output of the search to identify potentially eligible studies (M. GH and A.J). Any disagreements between the two reviewers were resolved by the consultation with the principal investigator (A.R).
Study selection and definition
Each title and abstract were reviewed to identify relevant studies by two individual researchers (M.GH and MM). The full texts of publications were reviewed if the abstract suggested that diabetics had been examined in relation to tooth loss. Studies met the inclusion criteria if: a) had observational design, b) reported odds ratio (OR), prevalence ratio (PR), risk ratio (RR) or hazard ratio (HR) with 95% confidence interval (95% CI) for the category of diabetic or provided number of tooth loss subjects and without tooth loss subjects in each category of diabetic or without diabetic to calculate OR and 95% CI. Studies were excluded if: a) had randomized clinical trial (RCT) design, b) insufficient data studies, animal experiments, letters, case reports and review b) reporting mean (SD), correlation, or regression coefficient as the effect size, and c) were conducted on the same population.
Data extraction
The following data were extracted from each study: first author’s last name, date of publication, country, study design, duration of follow-up for cohort studies, sex, age, definition of diabetics, type of outcome and its definition, number of total subjects and cases in each category of diabetics, OR, RR, and HR (95% CI) in each category of exposure diabetics and adjusted variables.
Assessment of the risk of bias and quality of the evidence
Risk of bias of included observational studies were assessed using the Newcastle-Ottawa Scale (NOS) [34, 35]. NOS tool is comprised of three items including: selection, comparability, and outcome. A maximum score of 9 can be awarded to each study. In the current study, the quality of the studies was divided into three categories: low (less than 5 points), moderate (5–6 points) and high (7–8 points).
Statistical analysis
Stata software version 16 (StataCrop, College Station, Texas, USA) was used to conduct meta-analysis. The ORs (95% CI) were used to calculate summary effect size. Pooled odds ratios were summarized using the Der Simonian and Laird method for random effects models. The reported HRs or RRs and PRs by cohort studies were considered the same as OR. For studies that did not report ORs, HRs, or PRs, we calculated ORs and 95% CIs using relevant formula: OR = (odds of being tooth loss if diabetics / odds of being tooth loss if not diabetics) and 95% CI = exp. [ln (OR) ± 1.96 SE (ln (OR))] [36]. Heterogeneity was assessed based on I2. Subgroup analysis was conducted based on type of study, location, exposure definition, outcome definition, quality of study and adjustment for confounders. Publication bias among included studies was assessed using the visual inspection of funnel plots, Bgge’s and Egger’s regression test. Also, a trim and fill analysis was performed to assess the stability of overall relative risk when the results suggested obvious publication bias.
Results
Identification and selections of studies
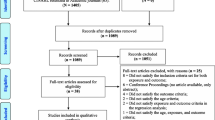
In the first step of our search, a total of 3121 articles were retrieved using PubMed/Medline, Scopus, Web of Science, ProQuest, and Cochrane library, Google and Google Scholar. Of these articles, 494 articles were removed due to duplication and other 2175 articles were excluded after their title and abstract evaluation. The remaining 121 primary studies were considered for further eligibility assessment through careful reading of their full texts. After full-text evaluation, a further 99 articles were excluded due to inability to calculate effect sizes, study settings, and outcome interest (Table 1). Finally, 22 articles were found to be eligible and included in the systematic review and meta-analysis. The flow chart of study selection process is presented in Fig. 1.
Characteristics of included articles
The articles included in the meta-analysis comprised 13 cross-sectional study, six cohort studies and three case– control studies. Eight studies were conducted in American countries, seven studies in European and four studies in Asian countries. The publication year of all included articles range from 2007 to 2021. In primary studies, 11 studies the self-report and medical records was used to diagnose of the diabetes and 11 primary studies used glucose level or HbA1c to diagnose of diabetes among participants. In four studies ORs, PRs, RRs (95% CI) were not reported, therefore, we calculated ORs (95% CI) based on relevant formula. In addition, 16 studies have considered the any tooth loss for calculation of the effect sizes, and in six studies tooth loss at least 5 and more considered for calculation of the effect sizes. There were 677,532 participants in the included studies, with the number of participants per study ranging from 60 to 379,021. The characteristics of the included studies are summarized in Table 2. The NOS scores ranged from 3 to 8, with a mean score of 5.81. According to the NOS tool, 17 studies (77.27%) were of moderate or high quality. Tables 3, 4 and 5 provide a detailed summary of the risk of bias for included cohort, case-control and cross-sectional studies using NOS [34, 35].
Meta-analysis
In the overall summary, in unadjusted and adjusted results indicated that T2D significantly increased the risk of tooth loss, and OR unadjusted was 1.87 (95% CI: 1.62–2.13, p < 0.001), and OR adjusted was 1.20 (95% CI: 1.10–1.30, p < 0.001), respectively. The forest plot is displayed in Fig. 2.
Subgroup analysis was performed based on the study type, continent, method of diagnosis T2D, category of tooth loss, and quality of study. In the sub-group analysis for unadjusted OR by study type only in the cross-sectional study T2D significantly was associated with tooth loss (OR: 2.01, 95% CI: 1.62–2.39), but in the case-control study (OR: 2.38, 95% CI: 0.25–4.51) and cohort study (OR: 1.73, 95% CI: 0.89–2.57) T2D not significantly was associated with tooth loss. Also, Subgroup analysis based on study design for adjusted OR indicated that in the cohort study (OR: 1.29, 95% CI: 1.07–1.51), in the cross-sectional study (OR: 1.15, 95% CI: 1.06–1.23), and in the case-control study (OR: 5.10, 95% CI: 1.01–9.18) there was a significant association between T2D and tooth loss (Fig. 3).
In addition, in the sub-group analysis for unadjusted OR by continent, were found the T2D associated with tooth loss in North America (OR: 2.22, 95% CI: 1.65–2.79), in South America (OR: 1.64, 95% CI: 1.49–1.79), and in Europe (OR: 2.29, 95% CI: 1.22–3.37), but in Asia, T2D was not significantly associated with tooth loss (OR: 1.23, 95% CI: 0.98–1.47). Also, Subgroup analysis based on the continent for adjusted OR indicated that in North America (OR: 1.34, 95% CI: 1.10–1.59), in South America (OR: 1.11, 95% CI: 1.01–1.21), and in Asia (OR: 1.35, 95% CI: 1.27–1.43) there was a significant association between T2D and tooth loss (Fig. 4).
In the subgroup analysis based on the method of diagnosing T2D, we found both in the self-reporting method and in the blood sample detection method a significant association between T2D and tooth loss in unadjusted and adjusted OR. That results showed the association T2D and tooth loss were stronger in the blood sample assessment (Fig. 5).
The subgroup analysis for unadjusted OR on quality of studies for those revealed an estimated low quality with an OR of 2.16 and a 95% CI (1.40–2.92), an OR of 1.70 with a 95% CI (1.31–2.09) for those with moderate quality and an OR of 2.32 at a 95% CI (1.34–3.29) for those with high quality. Also, subgroup analysis based on quality of studies for adjusted OR indicated that in the low quality (OR: 3.13, 95% CI: 1.83–4.43), and high quality (OR: 1.18, 95% CI: 1.07–1.30) there was a significant association between T2D and tooth loss, but in moderate quality, T2D was not significantly associated with tooth loss (OR:1.21, 95% CI: 0.99–1.44) (Fig. 6).
A subgroup analysis for unadjusted OR, on the number of tooth loss was indicated for the category of tooth loss at least 5 teeth and more OR: 1.93 at a 95% CI (1.22–2.63), and any tooth loss OR: 1.77 at a 95% CI (1.50–2.04) Also, subgroup analysis based on the number of tooth loss for adjusted OR indicated that in the category of tooth loss at least 5 teeth and more (OR: 1.19, 95% CI: 1.03–1.36), and for any tooth loss category (OR: 1.20, 95% CI: 1.07–1.32) there was a significant association between T2D and tooth loss (Fig. 7).
Publication bias
Testing for publication bias was possible for the overall analysis, which is presented in Fig. 8. There seemed to be some publication bias when funnel plots for odds estimates were considered in ORs studies and the p-values in the Begg’s test and Egger’s test were p = 0.99 and p = 0.0001 for unadjusted and the Begg’s test and Egger’s test were p = 0.16 and p = 0.0005 for adjusted (Fig. 8). However, the trim and fill method for calibration of publication bias was performed because an asymmetry was observed in the visual inspection of the funnel plot. However missing study was not identified by trim and fill method.
Discussion
The present study summarizes a collection of articles in the field of dentistry and medicine with respect to an important question that examines the relationship between T2D and tooth loss. This systematic review and meta-analysis were conducted on 22 observational studies involving 677,532 participants. The overall summary, indicated that T2D increases the risk of tooth loss by> 1.87 times in unadjusted data and 1.20 times in adjusted data. In addition, this association was also present in other subgroups, including study design, method of diagnosing T2D, continent, study quality, and number of tooth loss. This event seems to be in line with what has been reported in other epidemiologic studies, as several cases have supported the link between diabetes, periodontal disease, and tooth decay [49, 50]. These are two common reasons for the endpoint of the tooth loss parameter. Therefore, the general conclusion for this section is that diabetes maybe can increase the risk of tooth loss.
Review of other meta-analysis studies conducted by Hilal et al. [31] in seven studies that examined the association between diabetes and tooth loss, they found that diabetes was significantly associated with tooth loss (OR: 1.76, 95% CI: 1.21–2.55). Our study with more studies (22 studies) confirmed these findings. In addition, Weijdijk’s et al. [32], which examined the risk of tooth loss in diabetic patients on 10 studies, found that diabetes was significantly associated with the risk of tooth loss (OR: 1.63, 95% CI:1.33–2.00). Our study also confirmed the findings of this study. It should be noted, however, that other studies have not addressed the issue of confounding control in examining the association between diabetes and tooth loss. This is why our adjusted odds ratio (OR:1.20, 95% CI: 1.10–1.30) for association between diabetes and tooth loss is lower than other studies. This indicates an independent association (adjusted for confounders) between diabetes with tooth loss.
Previous observational studies investigating the association between T2D and tooth loss have reported conflicting results. In a cohort study of 15,113 participants, Greenblatt et al. [20] showed that the odds of tooth loss were more than doubled in T2D cases (OR: 2.69, 95% CI: 2.45–2.97). In another cohort study, T2D increased the odds of tooth loss by 29% (OR: 1.29; 95% CI: 1.23–1.36) [15]. However, another cohort study showed no association between T2D and risk of tooth loss [26]. Such findings have also been reported in other types of studies [27,28,29,30]. Differences in study design, general characteristics of participants, methodological approach to data collection, diagnosis of T2D, and lack of adjustment for potential confounders may explain the different findings. In a systematic review of 53 observational studies, Wu et al. [51] showed consistent results for the association between T2D and periodontitis. They reported that the prevalence of T2D was significantly higher in patients with periodontitis (OR = 4.04, 95% CI 2.48–6.59, p < 0.001) and vice versa (OR = 1.58, 95% CI 1.38–1.81, p < 0.001). The findings of this study are consistent with previous evidence that there is a significant association between T2D and tooth loss.
The relationship between diabetes and oral diseases such as tooth loss, gingivitis, periodontal disease, and soft tissue damage has been investigated in various studies [1, 17]. Periodontal disease is the sixth most common complication of diabetes [6, 52]. Patients with T2D have a significantly higher rate of tooth loss. Roughly 22% of diabetics suffer from periodontal disease, which increases with age. Poor blood sugar control can increase the risk of gum problems [10]. There is a two-way relationship between diabetes and periodontitis [17]. Periodontal disease causes high blood sugar, which makes diabetes more difficult to control and makes the patient more susceptible to gum disease [10]. Various studies have shown an association between T2D and periodontal disease [1]. As a result, periodontal disease in diabetics can lead to tooth loss, so diabetics have 15% more tooth loss than non-diabetics [7, 53, 54]. A study showed that the risk of periodontitis in diabetic patients is three times that of non-diabetic patients, and tooth loss is usually caused by periodontal problems. In diabetes, the growth of anaerobic Gram-negative bacteria under the gums is increased [53]. Bacteria in the mouth can form plaques around the teeth and gums. If this plaque is not removed by personal hygiene, the bacteria in the plaque will break down food and produce toxins that cause inflammation of the gums. At this stage, symptoms of gum disease (redness, swelling, bleeding of the gums) appear. If gum disease is not treated, more plaque builds up on the teeth, gums, and under the gums, and this plaque becomes calculus. As a result of the activity of more bacteria, this inflammation can lead to the formation of a gum connection between the tooth and the periodontal pocket. Periodontitis is a stage of the disease that eventually results in the loss of the bone and ligaments surrounding the teeth and loosening as the teeth lose their support, eventually leading to tooth loss [10, 21].
Tooth loss as a proxy for severe periodontitis might play an epidemiologically confusing role in the evaluation of a systemic disease hypothesis [43, 55]. How diabetes leads to periodontal disease and subsequent tooth loss can be explained by various physiological processes, such as immune responses, microflora, cytokines, and glycosylation products. Poorly controlled diabetes can lead to elevated glucose levels in the crevice fluid of the gums in people with diabetes. Therefore, it increases the growth of microaerophilic anaerobic gram-negative bacteria in the areas under the gums [53]. They also impair the function of polymorphonuclear leukocytes (PMNs) and monocytes/macrophages, thereby reducing host defenses against periodontal pathogens and increasing bacterial proliferation. Fat metabolism in diabetics also increases the production of proinflammatory cytokines such as tumor necrosis factor-α (TNF-α) and interleukin-1β (IL-1β) by multinucleated leukocytes and decreases the production of essential polypeptide growth factors such as platelet-derived growth factor (PDGF), transforming growth factor-beta 1 (TGF-β1) and fibroblast growth factor (bFGF) by tissue macrophages [6]. On the other hand, these individuals produce more glycosylation products, which lead to collagen cross-linking, which in addition to reducing collagen solubility, reduces the likelihood of collagen repair and replacement. All of these processes lead to gingivitis, which then progresses to adjacent periodontal tissue, leading to increased tooth loss through increased bone, cement, and ligament damage [15, 54]. Diabetes mellitus (DM) is a chronic inflammatory disease. Evidence supports an increased risk of periodontal disease and the incidence / severity of caries in diabetic patients. Both are major sources of tooth loss.
Between-study heterogeneity is common in meta-analyses, and different characteristics between studies such as year of publication, study location, diagnostic testing, design, and quality of original articles may be sources of between-study heterogeneity [56, 57]. Our meta-analysis revealed significant heterogeneity among studies on T2D and tooth loss risk. Therefore, subgroup analyses did not identify potential factors for heterogeneity between studies.
Risk of bias
Assessment of risk of bias is a key step in conducting SRs and informs many other steps and decisions within the review. It also plays an important role in the final assessment of the strength of the evidence [58]. Based on the risk of bias of the results, it indicated that all cohort studies included in the selection section met the NOS criteria. However, two of the studies [42, 43] did not adjust for confounders to report results, and results and effect sizes were reported crudely. Among the case-control studies, none of them are representative of cases and the rate of non-response has not been reported. In all cross-sectional studies, tooth loss was assessed using the clinical assessment method, which is the standard method for outcome assessment. Seven [7, 29, 38,39,40, 48] cross-sectional studies used the self-report method to diagnose diabetes, which increases the risk of bias. Sub-analysis based on the estimated quality of study of the selected studies shows that for low quality, a smaller OR (2.16 and 95% CI [1.40–2.90]) was found than for those with high quality (OR = 2.32 at a 95% CI [1.34–3.29]). Both low-quality and high-quality confidence intervals are small, indicating that the estimates are not flawed by imprecision.
The current systematic reviews and meta-analyses have some strengths and limitations. The study advantages; firstly, our study is the first comprehensive meta-analysis about the association between T2D and tooth loss. Second, in the current study, there was no publication bias between studies, and we performed several subgroup analyses. Third, in the diagnosis of diabetes, the self-report method and the blood sample diagnosis method were evaluated, and the results were reported separately.
There are limitations in our present meta-analysis. First, our study only included articles published in English and the limited number of studies included in this study may lead to false or unstable results. Second, most of the studies included were cross-sectional, so it is difficult to determine the causal relationship between T2D and tooth loss. The results of this study should be interpreted with caution.
Conclusions
In conclusion, the results of our study showed a positive association between T2D and tooth loss in cross-sectional studies. No significant association between T2D and tooth loss was found in cohort studies. Undoubtedly, large-scale prospective studies are needed to validate the current results in the future.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- T2D:
-
Type 2 Diabetes
- CI:
-
Confidence Interval
- OR:
-
Odds Ratio
- NOS:
-
Newcastle-Ottawa Scale
- RR:
-
Relative Ratio
- HR:
-
Hazard Ratio
- HbA1c:
-
Hemoglobin A1c
- PR:
-
Prevalence Ratio
- SD:
-
Standard Deviation
References
Kaur G, Holtfreter B, Rathmann WG, Schwahn C, Wallaschofski H, Schipf S, et al. Association between type 1 and type 2 diabetes with periodontal disease and tooth loss. J Clin Periodontol. 2009;36(9):765–74.
Patiño MN, Loyola R, Medina S, Pontigo L, Reyes M, Ortega R, et al. Caries, periodontal disease and tooth loss in patients with diabetes mellitus types 1 and 2. Acta Odontol Latinoam. 2007;21(2):127–33.
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas. Diabetes Res Clin Pract. 2019;157:107843.
Williams R, Karuranga S, Malanda B, Saeedi P, Basit A, Besançon S, et al. Global and regional estimates and projections of diabetes-related health expenditure: results from the international diabetes federation diabetes atlas. Diabetes Res Clin Pract. 2020;162:108072.
Kapp JM, Boren SA, Yun S, LeMaster J. Peer reviewed: diabetes and tooth loss in a national sample of dentate adults reporting annual dental visits. Prev Chronic Dis. 2007;4(3):A59.
Furukawa T, Wakai K, Yamanouchi K, Oshida Y, Miyao M, Watanabe T, et al. Associations of periodontal damage and tooth loss with atherogenic factors among patients with type 2 diabetes mellitus. Intern Med. 2007;46(17):1359–64.
Hastings JF, Vasquez E. Diabetes and tooth loss among working-age African Americans: a national perspective. Social Work in Public Health. 2017;32(7):443–51.
Vidone L. A healthy mouth: an important part of a diabetes management plan. AADE Pract. 2018;6(3):22–7.
Wilder RS, Moretti AJ. Overview of gingivitis and periodontitis in adults. Waltham: UpToDate; 2021.
Manish K, Raman N, Gautam A, Jain S, Jha PC, Kumar A. A study on association 0f tooth loss & periodontal disease in patients suffering from diabetes from bihar region. Int J Med Biomed Stud. 2020;4(2):220–6.
Al Habashneh R, Khader Y, Hammad MM, Almuradi M. Knowledge and awareness about diabetes and periodontal health among Jordanians. J Diabetes Complicat. 2010;24(6):409–14.
Control CfD, Prevention. Dental visits among dentate adults with diabetes--United States, 1999 and 2004. MMWR Morb Mortal Wkly Rep. 2005;54(46):1181–3.
Jansson H, Lindholm E, Lindh C, Groop L, Bratthall G. Type 2 diabetes and risk for periodontal disease: a role for dental health awareness. J Clin Periodontol. 2006;33(6):408–14.
Ogunbodede E, Fatusi O, Akintomide A, Kolawole K, Ajayi A. Oral health status in a population of Nigerian diabetics. J Contemp Dent Pract. 2005;6(4):75–84.
Yoo JJ, Kim DW, Kim MY, Kim YT, Yoon JH. The effect of diabetes on tooth loss caused by periodontal disease: a nationwide population-based cohort study in South Korea. J Periodontol. 2019;90(6):576–83.
Thorstensson H, Johansson B. Why do some people lose teeth across their lifespan whereas others retain a functional dentition into very old age? Gerodontology. 2010;27(1):19–25.
Sensorn W, Chatrchaiwiwatana S, Bumrerraj S. Relationship between diabetes mellitus and tooth loss in adults residing in Ubonratchathani province, Thailand. J Med Assoc Thai. 2012;95(12):1593–605.
Patel MH, Kumar JV, Moss ME. Diabetes and tooth loss: an analysis of data from the National Health and nutrition examination survey, 2003–2004. J Am Dent Assoc. 2013;144(5):478–85.
Wiener RC, Shen C, Findley PA, Sambamoorthi U, Tan X. The association between diabetes mellitus, sugar-sweetened beverages, and tooth loss in adults: evidence from 18 states. J Am Dent Assoc. 2017;148(7):500–9. e4.
Greenblatt AP, Salazar CR, Northridge ME, Kaplan RC, Taylor GW, Finlayson TL, et al. Association of diabetes with tooth loss in Hispanic/Latino adults: findings from the Hispanic Community Health Study/Study of Latinos. BMJ Open Diabetes Res Care. 2016;4(1):e000211.
Broadbent J, Thomson W, Poulton R. Progression of dental caries and tooth loss between the third and fourth decades of life: a birth cohort study. Caries Res. 2006;40(6):459–65.
Deguchi M, Mau MKLM, Davis J, Niederman R. Peer reviewed: preventable tooth loss in Hawai ‘i: the role of socioeconomic status, diabetes, and dental visits. Prev Chronic Dis. 2017;14:E115.
Felton DA. Edentulism and comorbid factors. J Prosthodont. 2009;18(2):88–96.
Harada K, Morino K, Ishikawa M, Miyazawa I, Yasuda T, Hayashi M, et al. Impact of glycaemic control on the number of teeth remaining: a cross-sectional analysis using a database containing japanese employment-based health insurance and check-up data. Available at SSRN 3557999. 2020.
Joshipura KJ, Ritchie C. Can the relation between tooth loss and chronic disease be explained by socio-economic status? Eur J Epidemiol. 2005;20(3):203.
Oluwagbemigun K, Dietrich T, Pischon N, Bergmann M, Boeing H. Association between number of teeth and chronic systemic diseases: a cohort study followed for 13 years. Plos One. 2015;10(5):e0123879.
Shamala A, Al-Hajri M, Al-Wesabi MA. Risk factors for periodontal diseases among yemeni type II diabetic patients. A case-control study. J Oral Res. 2017;6(7):176–81.
Frias-Bulhosa J, Manso MC, Mota CL, Melo P. Self-rated health and oral health in type 2 diabetic patients - a case-control study. Revista Portuguesa De Estomatologia Medicina Dentaria E Cirurgia Maxilofacial. 2018;59(4):181–90.
Delgado-Pérez VJ, De La Rosa-Santillana R, Márquez-Corona ML, Ávila-Burgos L, Islas-Granillo H, Minaya-Sánchez M, et al. Diabetes or hypertension as risk indicators for missing teeth experience: an exploratory study in a sample of Mexican adults. Niger J Clin Pract. 2017;20(10):1335–41.
Buysschaert M, Muhindo CT, Alexopoulou O, Rahelic D, Reychler H, Preumont V. Oral hygiene behaviours and tooth-loss assessment in patients with diabetes: a report from a diabetology Centre in Belgium. Diabetes Metab. 2017;43(3):272–4.
Helal O, Goestemeyer G, Krois J, Fawzy El Sayed K, Graetz C, Schwendicke F. Predictors for tooth loss in periodontitis patients: systematic review and meta-analysis. J Clin Periodontol. 2019;46(7):699–712.
Weijdijk LP, Ziukaite L, Van der Weijden G, Bakker EW, Slot DE. The risk of tooth loss in patients with diabetes: a systematic review and meta-analysis. Int J Dent Hyg. 2022;20(1):145–66.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J Clin Epidemiol. 2021;134:103–12.
Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute. 2011, 2 (1): 1-12.
Modesti PA, Reboldi G, Cappuccio FP, Agyemang C, Remuzzi G, Rapi S, et al. Panethnic differences in blood pressure in Europe: a systematic review and Meta-analysis. Plos One. 2016;11(1):e0147601.
Hamling J, Lee P, Weitkunat R, Ambühl M. Facilitating meta-analyses by deriving relative effect and precision estimates for alternative comparisons from a set of estimates presented by exposure level or disease category. Stat Med. 2008;27(7):954–70.
Costa FO, Santuchi CC, Lages EJP, Cota LOM, Cortelli SC, Cortelli JR, et al. Prospective study in periodontal maintenance therapy: comparative analysis between academic and private practices. J Periodontol. 2012;83(3):301–11.
Huang DL, Chan KCG, Young BA. Poor oral health and quality of life in older U.S. adults with diabetes mellitus. J Am Geriatr Soc. 2013;61(10):1782–8.
Dar-Odeh N, Borzangy S, Babkair H, Farghal L, Shahin G, Fadhlalmawla S, et al. Association of dental caries, retained roots, and missing teeth with physical status, diabetes mellitus and hypertension in women of the reproductive age. Int J Environ Res Public Health. 2019;16(14):2565.
Rai NK, Carey C, Brunson D, Tiwari T. Increasing dental Students’understanding of population surveillance through data mining. J Dent Educ. 2019;83(3):281–6.
Simila T, Auvinen J, Puukka K, Keinanen-Kiukaanniemi S, Virtanen JI. Impaired glucose metabolism is associated with tooth loss in middle-aged adults: the Northern Finland birth cohort study 1966. Diabetes Res Clin Pract. 2018;142:110–9.
Joshipura KJ, Munoz-Torres FJ, Dye BA, Leroux BG, Ramirez-Vick M, Perez CM. Longitudinal association between periodontitis and development of diabetes. Diabetes Res Clin Pract. 2018;141:284–93.
Liljestrand JM, Havulinna AS, Paju S, Männistö S, Salomaa V, Pussinen PJ. Missing teeth predict incident cardiovascular events, diabetes, and death. J Dent Res. 2015;94(8):1055–62.
Kowall B, Holtfreter B, Volzke H, Schipf S, Mundt T, Rathmann W, et al. Pre-diabetes and well-controlled diabetes are not associated with periodontal disease: the SHIP trend study. J Clin Periodontol. 2015;42(5):422–30.
de Medeiros TCC, Areas E, Souza A, Prates RC, Chapple I, Steffens JP. Association between tooth loss, chronic conditions, and common risk factors—results from the 2019 Brazilian health survey. J Periodontol. 2021; Online ahead of print.
Zhang S, Philips KH, Moss K, Wu D, Adam HS, Selvin E, et al. Periodontitis and risk of diabetes in the atherosclerosis risk in communities (ARIC) study: A BMI-modified association. J Clin Endocrinol Metab. 2021;106(9):E3546–E58.
Fatima del Carmen AD, Aída BYS, Javier DLFH. Risk indicators of tooth loss among Mexican adult population: A cross-sectional study. Int Dent J. 2021;71(5):414–9.
Laouali N, El Fatouhi D, Aguayo G, Balkau B, Boutron-Ruault MC, Bonnet F, et al. Type 2 diabetes and its characteristics are associated with poor oral health: findings from 60,590 senior women from the E3N study. BMC Oral Health. 2021;21(1):315.
Chapple IL, Genco R, workshop* wgotjEA. Diabetes and periodontal diseases: consensus report of the joint EFP/AAP workshop on periodontitis and systemic diseases. J Periodontol. 2013;84:S106–S12.
Chapple IL, Bouchard P, Cagetti MG, Campus G, Carra MC, Cocco F, et al. Interaction of lifestyle, behaviour or systemic diseases with dental caries and periodontal diseases: consensus report of group 2 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol. 2017;44:S39–51.
Wu CZ, Yuan YH, Liu HH, Li SS, Zhang BW, Chen W, et al. Epidemiologic relationship between periodontitis and type 2 diabetes mellitus. BMC Oral Health. 2020;20(1):204.
Malviya M, Trivedi M, Chourasia PK, Tote JV. A study of association between diabetes mellitus and tooth loss among diabetic patients. Glob J Res Analysis (GJRA). 2019;8(11):2277–8160.
Singh AK, Mishra R. A prospective study establishing correlation between diabetes and tooth loss. J Adv Med Dent Sci Res. 2017;5(12):119A–23A.
Preshaw P, Alba A, Herrera D, Jepsen S, Konstantinidis A, Makrilakis K, et al. Periodontitis and diabetes: a two-way relationship. Diabetologia. 2012;55(1):21–31.
Desvarieux M, Demmer RT, Rundek T, Boden-Albala B, Jacobs DR Jr, Papapanou PN, et al. Relationship between periodontal disease, tooth loss, and carotid artery plaque: the Oral infections and vascular disease epidemiology study (INVEST). Stroke. 2003;34(9):2120–5.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Higgins J, Thompson S, Deeks J, Altman D. Statistical heterogeneity in systematic reviews of clinical trials: a critical appraisal of guidelines and practice. J Health Serv Res Policy. 2002;7(1):51–61.
Viswanathan M, Ansari M, Berkman N, Chang S, Hartling L, McPheeters M, et al. Assessing the risk of bias of individual studies in systematic reviews of health care interventions. Agency for healthcare research and quality methods guide for comparative effectiveness reviews. US: AHRQ Methods for Effective Health Care; 2012.
Acknowledgements
Not applicable.
Funding
This study was not funded.
Author information
Authors and Affiliations
Contributions
AR and ARA designed the study protocol. MM, AJ, and MG independently performed the literature searches and extraction of data. AR and DR conducted the statistical analyses, and drafted the manuscript. ARA and FE made substantial contributions to interpretation of data, and were involved in drafting the manuscript or revising it critically for important intellectual content. All authors confirmed that they meet the ICMJE criteria for authorship. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This systematic review was ethical approved by Golestan University of Medical Sciences (Ethical code: IR.GOUMS.REC.1400.036).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ahmadinia, A.R., Rahebi, D., Mohammadi, M. et al. Association between type 2 diabetes (T2D) and tooth loss: a systematic review and meta-analysis. BMC Endocr Disord 22, 100 (2022). https://doi.org/10.1186/s12902-022-01012-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-022-01012-8