Abstract
Background
Red cell distribution width (RDW) is a predicter of infections, cancer and diabetes. However, the relationship between RDW and β-cell function and insulin resistance remains unclear in patients with type 2 diabetes mellitus (T2DM). The aim of the study was to explore the relationship between RDW and β-cell function in patients with T2DM.
Methods
A total of 559 T2DM patients were enrolled in this cross-sectional study. Patients were divided into three groups according to RDW tertiles. Clinical and biochemical characteristics such as age, duration of diabetes, blood pressure, RDW, glycosylated hemoglobin A1c (HbA1c), C-peptide and lipid profiles were collected. Homeostasis model assessment of insulin resistance (HOMA2IR) and homeostasis model assessment of β-cell function (HOMA2%B) were assessed using homeostasis model assessment (HOMA) based on fasting blood glucose (FBG) and fasting C-peptide index (FCPI). Correlations and multiple linear regressions were performed to explore the association between RDW and islet function indexes in total population and in different gender subgroups.
Results
The HOMA2%B gradually increased according to RDW tertiles (lowest, second, highest RDW tertiles; 47.1(32.9–75.4), 54.05(34.1–81), and 57.9(38.65–95.4), respectively; P = 0.036). Correlation analysis indicated that there were significant correlations between RDW and age, diabetes duration, diastolic blood pressure (DBP), triglycerides (TG), aspartate transaminase (AST), FBG, HbA1c and HOMA2%B in all subjects. In male subjects, RDW correlated positively with age, high-density lipoprotein cholesterol (HDL) and AST, and it correlated negatively with body mass index (BMI), DBP and TG. In female subjects, RDW correlated positively with age, duration, serum creatinine (Cr), FCPI and HOMA2%B, and it correlated negatively with alanine transaminase (ALT), FBG and HbA1c. Multiple linear regressions indicated that RDW was significantly correlated with HOMA2%B and HbA1c in the total population in both unadjusted and adjusted analysis. This finding could be reproduced in the subgroup of men for HOMA2%B only and in women for HbA1c only.
Conclusions
RDW is associated with β-cell function assessed by HOMA2%B after adjusting for covariates in male T2DM patients.
Similar content being viewed by others
Background
Red blood cell distribution width (RDW) is not only a measure of the size variation of circulating red blood cells (RBC), but also an indicator of their heterogeneity [1]. Measurements of RDW are provided in routine hematological examinations in clinical practice. Multiple studies have shown that elevated RDW values are associated with many human diseases, such as cancer, cardiovascular disease and diabetes [2,3,4,5,6], and are also associated with disease activity or complications of diseases [7,8,9]. The relationship between RDW and type 2 diabetes mellitus (T2DM) has been studied for several years, and there are no consistent results. From the Malmo Diet and Cancer Study, researchers found that low RDW was independently associated with increased incidence of diabetes [6]. However, Gang L et al. reported that elevated RDW is associated with an increased incidence of DM [10]. A prospective cohort study reported a significant reduction in the risk of poor glycemic control in T2DM patients with higher RDW [11].
T2DM is currently one of the most common chronic diseases, affecting approximately 415 million adults in the world and more than 100 million adults in China, and its incidence has risen dramatically in recent years, especially in middle-aged and elderly [12, 13]. The progressive deterioration of islet β-cell function and insulin resistance are the main pathophysiological factors of adult type 2 diabetes mellitus. However, to the best of our knowledge, the relationship between RDW and islet β-cell function has not been studied. Therefore, we conducted a cross-sectional study to investigate the association of RDW with β-cell function indexes in T2DM patients.
Methods
Study subjects
From January 1, 2016 to December 31, 2018, 559 T2DM patients were enrolled in the Second Affiliated Hospital of Anhui Medical University in this study. The diagnosis of type 2 diabetes in this cross-sectional study was based on the standards of the American Diabetes Association. We excluded the following patients: 1) patients with severe diseases of the heart, liver, pancreas, kidney or hematological disorders; 2) patients with infection, tumor or immune diseases; 3) patients with recent acute complications of diabetes (such as ketoacidosis, hyperosmolar nonketotic diabetic coma or lactic acid acidosis, etc.); 4) patients with viral hepatitis, autoimmune hepatitis, acute infection, or nephritis; 5) patients who used of steroid hormones within 3 months; and 6) women in the follicular phase of their menstrual cycle. Written informed consent was obtained from all participating patients before enrollment. All procedures performed in this study were in accordance with the ethical guidelines of the Declaration of Helsinki and were approved by an Ethics Committee of the Second Affiliated Hospital of Anhui Medical University.
Measurements
Anthropometric measurements and fasting blood tests of every participant were performed during the patients’ visits to our institution. Study participants were inquired about their age and duration of diabetes, the duration of diabetes (in years) was calculated from the time for the patient to be diagnosed as T2DM. Height and weight were measured in the morning on an empty stomach, and the body mass index (BMI) was calculated by dividing weight (in kilograms) by square of the height (in meters). All the subjects were forbidden to smoke and rested for 30 min before the blood pressure of right upper limb was measured, each subject was measured twice with an interval of about 5 min, and systolic blood pressure was recorded by taking the average value. Overnight fasting blood samples were collected from each participant to test for RDW, glucose, serum total cholesterol (TC), triglycerides (TG), low-density lipoprotein cholesterol (LDL), high-density lipoprotein cholesterol (HDL), serum uric acid (SUA), liver/renal functions and glycosylated hemoglobin A1c (HbA1c).
After fasting blood samples were collected, the T2DM patients took a mixed noodle meal, which is a steamed bun made from 100 g of flour, and then blood samples were collected 2 h after the meal to measure the concentration of glucose and C-peptide. Homeostasis model assessment of insulin resistance (HOMA2IR) and homeostasis model assessment of β-cell function (HOMA2%B) were estimated using fasting blood glucose (FBG) and C-peptide by homeostasis model assessment (HOMA) (http://www.dtu.ox.ac.uk/homacalculator/) [14]. C-peptide index (CPI) and ΔC-peptide was used to evaluate insulin secretory capacity. The calculation of fasting CPI (FCPI) and postprandial CPI (PPCPI) are from the ratio of serum C peptide to blood glucose concentrations at baseline and 2 h postprandial, which was termed CPR (nmol /L) / FBG (mmol/L). ΔC peptide value is defined as serum C peptide level 2 h after meal minus the fasting C peptide level (nmol/L).
Complete blood count levels were measured using an automatic hematology analyzer (Sysmex, XE-2100). The RDW to Mean Corpuscular Volume (MCV) ratio was calculated using the following formula: RDW/MCVx100%. HbA1c was determined by high performance liquid chromatography. The glucose oxidase method was used to determine blood glucose. Standardized enzyme method was used to determine TC, TG, HDL, LDL, SUA and liver and kidney functions.
Statistical analysis
All statistical analyses were carried out using SPSS for Windows 22.0 (SPSS Inc., Chicago, IL, USA). Normally distributed data, expressed as the means ± standard deviations (SDs), were analyzed using the student’s t test or the one-way analysis of variance (ANOVA) with Bonferroni corrections for post hoc analysis. Non-normally distributed variables were presented as medians (range 25th–75th percentile) and analyzed using the Mann-Whitney test or the Kruskal-Wallis H test to identify statistical differences between groups, a post hoc analysis using Bonferroni corrections for paired comparisons was employed. All categorical variables were represented by numbers (proportions). A chi-square test or Fisher’s exact test were used to analyze the difference of frequencies between groups. The associations between RDW and various clinical factors were further analyzed by stratifying RDW into three tertiles. The Pearson’s or Spearman’s correlation tests were used to explore the simple correlations between RDW and various clinical factors. Multiple linear regression analysis was conducted to determine whether RDW was associated with HOMA2%B or HOMA2IR with or without adjusting for potential confounding factors. Model 1 for RDW was adjusted for age, BMI and diabetes duration. Model 2 was additionally adjusted for HbA1c. A two-tailed P values < 0.05 were considered as statistically significant.
Results
Clinical and biochemical characteristics of subjects
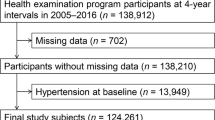
A total of 559 participants (343 men and 216 women) were included in the study. Clinical and laboratory data of the patients in the study are summarized in Table 1. The patients were categorized into three groups based on RDW tertiles. It appeared that age, proportion of male, duration of diabetes, diastolic blood pressure, TG, FBG, HbA1c, HOMA2%B and RDW were significantly different among the groups. HOMA2%B values were 47.1(32.9–75.4), 54.05(34.1–81), and 57.9(38.65–95.4), in the first, second, and third RDW tertiles, respectively, and Kruskal-Wallis H test showed significant difference between tertile 1 and tertile 3 of HOMA2%B values after Bonferroni correction(P = 0.030) (Fig. 1), but no statistical significance was demonstrated between tertile 1 and tertile 2(P = 0.437) or between tertile 2 and tertile 3(P = 0.763). There were no significant difference in the proportion of hypertention, poor glycemic control and hyperuricemia among RDW tertiles.
Clinical and biochemical characteristics of the patients in different gender subgroups
The clinical characteristics and islet function indexes of the study patients in different gender subgroups were shown in Table 2. Compared with female group, the male patients were younger and had higher diastolic blood pressure. The levels of TG, ALT, CR, SUA, HDL and RDW were statistically different between the male group and the female group. The levels of TG, ALT, CR, and SUA in the male group were higher than those in the female group, while the levels of HDL and RDW were lower than the female group. There were no significant difference in the proportion of hypertention, poor glycemic control and hyperuricemia between the male group and the female group.
Table 3 and Table 4 showed the distributions of clinical characteristics and islet function indexes of the patients according to gender-specific tertiles of RDW levels, respectively. In male participants, age, duration of diabetes, BMI, TG, HDL and RDW were significantly different among the RDW tertiles. The analysis of islet function indexes showed that there was no significant difference in HOMA2%B among the three tertiles; however, it did show a slightly increasing trend with RDW levels. Across female RDW tertiles, there was significant statistical difference with respect to age, ALT, Cr, FBG, HbA1c, HOMA2%B and RDW levels among the RDW tertiles while all other variables did not differed significantly. Specifically, paired comparisons showed significant difference between tertile 1 and tertile 3 of HOMA2%B values after Bonferroni correction (P = 0.009), but no statistical significance was demonstrated between tertile 1 and tertile 2 (P = 0.146) or between tertile 2 and tertile 3 (P = 0.909) .
Correlation between RDW and various metabolic parameters in total and different gender subgroups
The correlations between RDW and clinical characteristics and islet function indexes were shown in Table 5. In the total population, correlation analysis revealed that RDW significantly correlated with age, diabetes duration, DBP, TG, AST, FBG, HbA1c and HOMA2%B. In male subjects, RDW correlated positively with age, HDL and AST, and it correlated negatively with BMI, DBP and TG. In female subjects, RDW correlated positively with age, duration, Cr, FCPI and HOMA2%B, and it correlated negatively with ALT, FBG and HbA1c.
Multiple linear regression analysis of RDW and HOMA2%B, HOMA2IR or HbA1c
To further explore the association between RDW and HOMA2%B, multiple linear regressions were conducted using RDW as the dependent variable (see Table 6). In unadjusted analyses, the associations between RDW values and HOMA2%B were statistically significant in the total population and in male subjects, but not in females. After adjustments for potential confounders (model 1: age, BMI and diabetes duration; model 2: age, BMI, diabetes duration and HbA1c), RDW remained positively associated with HOMA2%B in the total population and in male subjects, yet in female subjects, RDW was not associated with HOMA2%B. We did similar analysis to define the association between RDW and HOMA2IR, as shown in Supplementary Table 1, the multiple linear regressions suggested that RDW was not associated with HOMA2IR in T2DM patients.
Multiple linear regressions were also carried out using RDW as the dependent variable to examine the relation between RDW and HbA1c (see Table 7). RDW levels were significantly associated with HbA1c in the total population and in female subjects in both unadjusted analyses and adjusted analysis (adjusted for age, BMI and diabetes duration), but the association was not found in male subjects in either unadjusted analyses or adjusted analysis.
Discussion
In the cross-sectional study, we demonstrated that RDW values are significantly associated with HOMA2%B and HbA1c. These associations persisted after adjustment for potential confounding factors. This finding could be reproduced in the subgroup of men for HOMA2%B only and in women for HbA1c only. However, we found a lack of correlation between RDW and HOMA2IR in T2DM patients. The results suggest that RDW may be more important in augmenting insulin secretion than in insulin resistance. To the best of our knowledge, this study is the first to investigate the relationship between RDW and β-cell function and insulin resistance in patients with T2DM.
RDW is a simple, inexpensive, routinely reported CBC inspection method. Its role in the differential diagnosis of anemia together with MCV has been recognized for a long time [15]. The increase of RDW reflects a deregulation of erythrocyte homeostasis. HOMA2%B is an index of basic insulin secretion, which represents the ability of islet β-cells to compensate against insulin resistance. We only found that RDW levels were significantly associated with HOMA2%B in male T2DM patients, but not in female patients with type 2 diabetes. This phenomenon may be explained that RDW was influenced by women’s menstrual period. Although we excluded women who were in the menstrual period, RDW changes with women’s menstrual cycle. A possible explanation of the association between RDW and HOMA2%B is that increased RDW might improve islet neogenesis and islet cell apoptosis, thereby, higher RDW decreased the risk of poor glycemic control in patients with type 2 diabetes, as Yin Y et al. reported [11]. However, the relationship between increased RDW and diseases is inconsistent. In contrast to our findings, some researchers have found that elevated RDW may reflect various potential pathological processes, such as impaired iron metabolism, which may lead to the development of diseases [16, 17]. Other researchers also reported that an increase in RDW is related to an impairment of erythropoiesis, which reflects chronic inflammation and oxidative stress, both of which are cornerstones in the pathogenesis of T2DM [18, 19]. Nevertheless, due to few published data, the biological mechanism of RDW and insulin secretion in T2DM patients is currently unclear. The target pathway of RDW for insulin production will provide a new direction for further research.
The HbA1c concentration represents the average blood glucose level over the previous 3 months, is free of short-term fluctuations, and can be monitored long term and controlled according to individual circumstances to an appropriate level to reduce the risk of serious complications [20]. Several studies found that the increase of RDW was related with the increase of HbA1c [6, 21, 22]. It was reported that hyperglycemia shortens the life span of RBCs, resulting in high variability of the red blood cell volume and an increase of RDW [23]. However, a few studies did not find a significant association between RDW and HbA1c [11, 24]. Compared with the above studies, we observed a negative correlation between RDW and HbA1c in female T2DM patients but not in male T2DM patients. In agreement with our findings, Sen-Yu et al. also observed that the level of RDW was in negative correlation with the levels of HbA1c in early diabetic nephropathy patients [25]. Unlike our study, Satilmis Bilgin et al. [26] found a strong correlation between RDW and HbA1c in type 2 diabetic men. However, owing to the controversial research results, it may be difficult to make a clear conclusion on the association between RDW and HbA1c.
Unfortunately, our research had a few limitations. First of all, because of the cross-sectional design, the causal relationship between RDW and HOMA2%B in T2DM patients was difficult to determine. Secondly, potential confounding factors that would affect islet function or RDW were not taken into consideration, such as exercise, diet, other complications, menopausal status and so on. Third, this study may have selection bias since the participants were enrolled in one institution. Despite these limitations, this is the first study to explore the relationship between RDW and HOMA2%B in T2DM patients. Well-designed cohort study is needed to verify these findings.
Conclusion
In conclusion, RDW was significantly correlated with HOMA2%B and HbA1c of the total T2DM patients in both unadjusted and adjusted analysis. The associations remained in the subgroup of men for HOMA2%B only and in women for HbA1c only. RDW could be taken into consideration as a marker of islet function in clinical practice.
Availability of data and materials
The data in this study are available only upon reasonable request from the corresponding authors.
Abbreviations
- RDW:
-
Red blood cell distribution width
- HOMA2IR:
-
Homeostasis model assessment of insulin resistance
- HOMA2%B:
-
Homeostasis model assessment of β-cell function
- RBCs:
-
Red blood cells
- T2DM:
-
Type 2 diabetes mellitus
- HbA1c:
-
Glycosylated hemoglobin A1c
- BMI:
-
Body mass index
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
- SUA:
-
Serum uric acid
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- Cr:
-
Serum creatinine
- FBG:
-
Fasting blood glucose
- AST:
-
Aspartate transaminase
- ALT:
-
Alanine transaminase
- MCV:
-
Mean corpuscular volume
- CPI:
-
C-peptide index
- FCPI:
-
Fasting C-peptide index
- PPCPI:
-
Postprandial C-peptide index
References
Montagnana M, Cervellin G, Meschi T, Lippi G. The role of red blood cell distribution width in cardiovascular and thrombotic disorders. Clin Chem Lab Med. 2011;50(4):635–41.
Lee H, Kong SY, Sohn JY, Shim H, Youn HS, Lee S, Kim HJ, Eom HS. Elevated red blood cell distribution width as a simple prognostic factor in patients with symptomatic multiple myeloma. Biomed Res Int. 2014;2014:145619.
Lippi G, Filippozzi L, Montagnana M, Salvagno GL, Franchini M, Guidi GC, Targher G. Clinical usefulness of measuring red blood cell distribution width on admission in patients with acute coronary syndromes. Clin Chem Lab Med. 2009;47(3):353–7.
Yao HM, Sun TW, Zhang XJ, Shen DL, Du YY, Wan YD, Zhang JY, Li L, Zhao LS. Red blood cell distribution width and long-term outcome in patients undergoing percutaneous coronary intervention in the drug-eluting stenting era: a two-year cohort study. PLoS One. 2014;9(4):e94887.
Nam JS, Ahn CW, Kang S, Kim KR, Park JS. Red blood cell distribution width is associated with carotid atherosclerosis in people with type 2 diabetes. J Diabetes Res. 2018;2018:1792760.
Engström G, Smith JG, Persson M, Nilsson PM, Melander O, Hedblad B. Red cell distribution width, haemoglobin A1c and incidence of diabetes mellitus. J Intern Med. 2014;276(2):174–83.
Arif MA, Syed F, Niazi R, Arif SA, Javed MU, Bashir A, Mansoor S. Assessment of red cell distribution width, glycaemic control and diabetes related complications - the ARDENT study. J Pak Med Assoc. 2019;69(4):483–8.
Malandrino N, Wu WC, Taveira TH, Whitlatch HB, Smith RJ. Association between red blood cell distribution width and macrovascular and microvascular complications in diabetes. DIABETOLOGIA. 2012;55(1):226–35.
Yunchun L, Yue W, Jun FZ, Qizhu S, Liumei D. Clinical significance of red blood cell distribution width and inflammatory factors for the disease activity in rheumatoid arthritis. Clin Lab. 2016;62(12):2327–31.
Gang L, Lifang W. Association of the Elevated red Blood Cell Distribution Width with the risk of developing diabetes mellitus. Intern Med. 2016;55(15):1959–65.
Yin Y, Ye S, Wang H, Li B, Wang A, Yan W, Dou J, Mu Y. Red blood cell distribution width and the risk of being in poor glycemic control among patients with established type 2 diabetes. Ther Clin Risk Manag. 2018;14:265–73.
Ogurtsova K, Da RFJ, Huang Y, Linnenkamp U, Guariguata L, Cho NH, Cavan D, Shaw JE, Makaroff LE. IDF diabetes atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50.
Xu Y, Wang L, He J, Bi Y, Li M, Wang T, Wang L, Jiang Y, Dai M, Lu J, et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310(9):948–59.
Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27(6):1487–95.
Xu L, Wang L, Huang X, Liu L, Ke W, He X, Huang Z, Liu J, Wan X, Cao X, et al. Baseline red blood cell distribution width predicts long-term glycemic remission in patients with type 2 diabetes. Diabetes Res Clin Pract. 2017;131:33–41.
Allen LA, Felker GM, Mehra MR, Chiong JR, Dunlap SH, Ghali JK, Lenihan DJ, Oren RM, Wagoner LE, Schwartz TA, et al. Validation and potential mechanisms of red cell distribution width as a prognostic marker in heart failure. J Card Fail. 2010;16(3):230–8.
Forhecz Z, Gombos T, Borgulya G, Pozsonyi Z, Prohaszka Z, Janoskuti L. Red cell distribution width in heart failure: prediction of clinical events and relationship with markers of ineffective erythropoiesis, inflammation, renal function, and nutritional state. Am Heart J. 2009;158(4):659–66.
Dada OA, Uche E, Akinbami A, Odesanya M, John-Olabode S, Adediran A, Oshinaike O, Ogbera AO, Okunoye O, Arogundade O: The relationship between red blood cell distribution width and blood pressure in patients with type 2 diabetes mellitus in Lagos, Nigeria. J Blood Med 2014, 5(default):185–189.
Horta-Baas G, Romero-Figueroa M. Clinical utility of red blood cell distribution width in inflammatory and non-inflammatory joint diseases. Int J Rheum Dis. 2019;22(1):47–54.
Heiskanen A. Standards of medical care in diabetes - 2013. Diabetes Care. 2013;33(Suppl 1):S11–61.
Giuseppe L, Giovanni T, Gian Luca S, Gian Cesare G. Increased red blood cell distribution width (RDW) is associated with higher glycosylated hemoglobin (HbA1c) in the elderly. Clin Lab. 2014;60(12):2095–8.
Veeranna V, Zalawadiya SK, Panaich SS, Ramesh K, Afonso L. The association of red cell distribution width with glycated hemoglobin among healthy adults without diabetes mellitus. CARDIOLOGY. 2012;122(2):129–32.
Cohen RM, Franco RS, Khera PK, Smith EP, Lindsell CJ, Ciraolo PJ, Palascak MB, Joiner CH. Red cell life span heterogeneity in hematologically normal people is sufficient to alter HbA1c. Blood. 2008;112(10):4284–91.
Sherif H, Ramadan N, Radwan M, Hamdy E, Reda R. Red cell distribution width as a marker of inflammation in type 2 diabetes mellitus. 2013;10(4):32–9.
Sen-Yu W, Chao X. Assessment of the relationship between red blood cell distribution width and preganecy hypertension disease. J Obstet Gynaecol Res. 2016;42(10):1258–62.
Bilgin S, Aktas G, Zahid Kocak M, Atak BM, Kurtkulagi O, Duman TT, Savli H. Association between novel inflammatory markers derived from hemogram indices and metabolic parameters in type 2 diabetic men. Aging Male. 2019. https://doi.org/10.1080/13685538.2019.1632283.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
DZ conceived the study, SZ, LW, TP and XZ participated in the study design. LW performed statistical analyses, DZ drafted the manuscript, TP and XZ edited and checked the manuscript. All of the authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All subjects have given their written informed consent and the study was approved by the ethics committee of the Second Affiliated Hospital of Anhui Medical University. It was conducted according to the standards of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, D., Zhang, S., Wang, L. et al. The relationship between red blood cell distribution and islet β-cell function indexes in patients with type 2 diabetes. BMC Endocr Disord 21, 7 (2021). https://doi.org/10.1186/s12902-020-00668-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-020-00668-4