Abstract
Background
Elderly patients with type 2 diabetes mellitus (T2DM) experience fractures more frequently than elderly individuals without diabetes. Fractures requiring hospitalization greatly affect quality of life, and although elderly patients with T2DM have several risk factors associated with fractures, only a few studies have evaluated these in detail in the Asian population. We conducted a retrospective study of elderly patients with T2DM for evaluating factors associated with fracture risk.
Methods
We conducted a retrospective study using electronic medical records (EMR) of patients aged ≥65 years with T2DM who were admitted to a public general medical institute in central Tokyo, Japan. We evaluated factors associated with fractures necessitating hospitalization in elderly patients with T2DM characteristics and hypoglycemic agent use. Factors associated with fracture risk were identified using multivariable logistic regression analysis.
Results
A total of 2,112 elderly patients (age ≥ 65 years) with T2DM were analyzed. Among them, 69 (3.3%) patients had been hospitalized for fractures. Factors associated with fractures were female sex (OR, 3.46), eGFR < 60 ml / min / 1.73 m2 (OR, 0.55), and thiazolidine use (OR, 4.28). Further, a separate analysis based on sex revealed that the use of thiazolidines was significantly associated with fracture risk in both sexes.
Conclusions
In elderly patients with T2DM, the key factor associated with fractures was the use of thiazolidines in both males and females. In this study, the use of thiazolidines was newly identified as a factor which increased the risk of fractures requiring hospitalization in elderly males. The study findings should be considered when hypoglycemic agents are selected for treating elderly patients with T2DM. Information bias, selection bias, and the effect of concomitant drugs may be the underlying reasons for why eGFR < 60 mL / min / 1.73 m2 reduced the fracture risk. However, details are unknown, and additional investigations are needed.
Similar content being viewed by others
Background
The worldwide prevalence of diabetes has been on the rise, and Japan ranks among the top 10 countries in terms of the number of elderly patients with diabetes. Moreover, the increasing proportion of the elderly in Japan includes the diabetic population. Decreased bone mass and pathological aging put elderly patients at risk for bone fractures, which reportedly negatively affect activities of daily living (ADLs); in challenging and serious cases, such fractures increase the risk of mortality [1,2,3]. A study on patients aged ≥55 years who were hospitalized for fractures demonstrated that 7.4% of the patients were discharged with medical care services and 53.2% were transferred to another medical facility [4]. Thus, fractures requiring hospitalization for elderly patients have a significant effect on their quality of life (QOL). Patients with type 2 diabetes mellitus (T2DM) are at a higher risk of bone fractures than individuals without diabetes, regardless of bone density [5, 6].
In Japan, the frequently used hypoglycemic agents comprise seven oral drugs and two injectable drugs, acting via nine different mechanisms. Among these agents, the only family of agents that has a clear correlation with risk of fractures is the thiazolidine (TZD) family, which has been found to increase the risk of bone fractures in females [7,8,9,10]. Although reports have also implicated other types of drugs in the occurrence of bone fractures [10], no consensus has been reached. Elderly patients with T2DM have various risk factors associated with fractures, but few studies have evaluated these in detail in the Asian population. The aim of the present study was to investigate the relationship between patient background, hypoglycemic agents, and risk factors in elderly patients with T2DM in Japan.
Methods
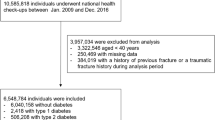
Subjects
We conducted a retrospective study using electronic medical records (EMR) of patients aged ≥65 years with T2DM mellitus who were admitted to Tokyo Saiseikai Central Hospital, which is a public general medical institute in central Tokyo, Japan. Data from January 2014 to January 2016 were used for analyses.
The inclusion criteria were (1) age ≥ 65 years, (2) a diagnosis of T2DM (ICD-10 code E11) or diabetes (ICD-10 code E14), and (3) inpatient status. The exclusion criteria were (1) a diagnosis of type 1 diabetes or no diagnosis of diabetes, (2) age < 65 years, (3) outpatient status, or (4) hospitalized ≥2 times within the study period. Data regarding patient characteristics and medicines used were recorded on the first day of hospitalization.
On the basis of the blood glucose target levels recommended by the Japanese Diabetes guidelines for patients with diabetes, the cutoff value for HbA1c was < 7.0 and that for BMI was < 25 kg/m2.
Survey items
We recorded patient characteristics and the number and type of regular oral medications used by each patient at the time of admission, and the use of hypoglycemic agents including sulfonylureas (SU), glinides, biguanides (BG), TZD, α-glucosidase inhibitors (αGI), sodium glucose cotransporter 2 (SGLT2) inhibitors, dipeptidyl peptidase-4 (DPP-4) inhibitors, glucagon-like peptide-1 (GLP-1) receptor agonist, and insulin.
Statistical analysis
Patient characteristics were tabulated as mean values plus or minus the standard deviation. Continuous variables were analyzed using unpaired t-test. Nominal variables were compared using χ2 test. Logistic regression was used for identifying which factors affect the incidence of fractures, using fractures necessitating hospitalization as the target variable. Univariate analysis was performed using explanatory variables including patient characteristics, hypoglycemic agent usage, and dosing of SU, glinides, BG, TZD, αGI, SGLT2 inhibitors, DPP-4 inhibitors, GLP-1 receptor agonist, and insulin. Explanatory variables with a significance of p < 0.2 were extracted using univariate analysis, and odds ratios (ORs) [at 95% confidence interval (CI)] were calculated using multivariate analysis. Because bone fracture incidence differs between males and females [11], the patients were separately analyzed on the basis of sex using the same method as described above for each subgroup. All statistical analyses were performed using the software Stata version 10 (stata corp, TX USA), and the statistical significance threshold was set at < 5%.
Ethics approval: This study was conducted in accordance with ethical guidelines for medical and health research involving human subjects. The ethics board of the Tokyo Saiseikai Central Hospital approved the study (control number, 27–51).
Results
Subjects
Patient background characteristics are shown in Table 1. There were a total of 2,112 subjects with a mean age of 76.5 ± 7.1 years, among which 55.3% were aged ≥75 years. Of them, 69 patients (3.3%) experienced fractures that necessitated hospitalization (hip fracture, n = 22; humeral fracture, n = 9; femoral neck fracture, n = 19; and spine fracture, n = 19). The mean HbA1c level was 7.1% ± 1.2%. Hypoglycemic agents were not administered to 33.1% (n = 700) of the patients. The most widely used hypoglycemic agents were DPP-4 inhibitors, used in 42.8% (n = 904) of patients, followed by SU (25.7%, n = 542), insulin (20.8%, n = 440), BG (19.3%, n = 407), αGI (9.5%, n = 200), TZD (7.0%, n = 148), GLP-1 receptor agonist (1.8%, n = 39), and SGLT2 inhibitors (0.4%, n = 8). None of the patients used glinides. We compared their background characteristics by dividing them into the following two groups: fracture group and no fracture group. Significant differences were noted in the following factors: percentage of males (fracture vs. non fracture, 36.8% vs. 65.5%, p < 0.001), age (fracture vs. non fracture, 79.7 ± 7.6 years vs. 76.4 ± 7.1 years, p = 0.002), the eGFR (fracture vs. non fracture, 62.1 ± 23.9 mL/min/1.73 m2 vs. 54.3 ± 22.1 mL/min/1.73 m2, p = 0.02), and TZD use (fracture vs. non fracture, 15.9% vs. 6.7%, p = 0.03).
Table 2 shows patient characteristics stratified by sex. Females had a higher age (78.1 ± 7.6 years vs. 76.4 ± 6.7 years, p < 0.001) and higher number of fractures (7.0% vs. 1.2%, p < 0.001), and a greater proportion of them were not using hypoglycemic agents (38.4% vs. 30.3%, p < 0.001) compared with males. On the contrary, a significantly larger proportion of females were using SU (females, 38.4% vs. males, 30.3%, p = 0.001) and a significantly smaller proportion were using TZD (females, 5.3% vs. males, 8.0%, p = 0.04) compared with males.
Factors affecting fracture risk
Results of logistic regression analysis using patient characteristics and hypoglycemic agent use as the explanatory variables and fracture occurrence as the response variable are shown in Table 3. Multivariate analysis with fracture as the objective variable revealed statistically significant differences for female sex (OR, 3.46; 95% CI, 1.88–6.37; p < 0.001), eGFR < 60 mL / min / 1.73 m2 (OR, 0.55; 95% CI, 0.31–0.99; p = 0.04), and TZD use (OR, 4.28; 95% CI, 1.71–10.7; p = 0.002).
Factors affecting the incidence of fractures in both sexes
Multivariate analysis with fracture as the objective variable (Table 3) revealed a statistically significant difference associated with TZD use (males: OR, 4.70; 95% CI, 1.14–19.3; p = 0.03, females: OR, 4.71; 95% CI, 1.43–15.5; p = 0.01).
Discussion
The present study found that female sex and TZD use are significant risk factors for bone fractures requiring hospitalization, and that an eGFR of < 60 mL / min / 1.73 m2 is associated with reduced fracture risk. Separate analysis of male and female patient characteristics revealed that TZD use is a risk factor for both sexes.
When estrogen levels decrease at menopause (at approximately 50 years of age), there is a significant accompanying decrease in bone mass, which progresses toward bone loss and osteoporosis [12]. Because the mean age of the females in the present study was 78.1 ± 7.6 years, and because 64.4% of the patients were aged ≥75 years, it was assumed that many of the females had gone through menopause approximately 20 years ago, and that their risk of bone fractures (relative to males) had increased via the same mechanism as in non-diabetic patients.
In the present study, an eGFR < 60 mL / min / 1.73 m2 was associated with a decreased risk of fractures and an OR of 0.55. Although chronic kidney disease (CKD) can cause bone fragility independent of other factors, the risk of bone fractures reportedly further increased with disease progression as a result of renal osteodystrophy caused by secondary hyperparathyroidism [13]. However, whether decreased kidney function increases the risk of bone fractures remains to be clarified; some researchers have reported that it does [14, 15], while others have reported that it does not [16, 17]. Administering activated vitamin D3 and calcium carbonate to patients with secondary hyperparathyroidism induced by decreased renal function may reduce the risk of fractures, and further investigation of the effects is warranted.
In terms of the relationship between glycemic control state and bone fracture risk, the risk of bone fractures reportedly increase with higher HbA1c levels [18]. Although HbA1c level was stratified and analyzed in this study, a significant reduction in fracture risk was not observed. Because bone turnover markers improve in the short term by controlling blood sugar [19], fracture risk may be correlated with the state of glycemic control. However, the ACCORD BONE ancillary study found that the risk of fractures was not improved in an intensive glycemic control group [20]. Therefore, good glycemic control in the short term may not be sufficient for reducing the risk of fractures. However, there was insufficient data in the present study to show the effect of glycemic control on fracture risk over a fixed duration, because only the HbA1c value targeted for investigation were used and no subsequent observations were made.
Odds ratios obtained in the present study suggest that TZD use significantly increases the odds of fractures in males (OR, 4.70), females (OR, 4.71), and overall (OR, 4.28). The relationship between T2DM use and the risk of fractures is complex, because the risk of fractures is not only affected by complications and patient characteristics, but also by treatments used in glucose level management. Several studies have reported that TZD use increases the risk of fractures in females, especially in postmenopausal females [21, 22]. This provides an explanation for why the rate of TZD use was significantly lower in females than in males. The use of TZD reportedly increases the risk of fracture in males aged ≥50 years with type 2 diabetes [23]. Because the study population involved patients aged ≥65 years, it can be concluded that use of TZD increased the risk of fracture. After 2011, when administration of the TZD pioglitazone was reportedly associated with bladder cancer [24], treatments with TZD were initiated with proper care. Therefore, many of the subjects in the present study were administered TZDs before 2011, and the increased OR in males may have resulted from the long-term TZD administration and because TZDs tend to be administered to patients with a prolonged history of morbidity.
Our study had several important limitations. First, it was a retrospective study conducted at a single institution and using electronic medical records (EHR); therefore, information and selection biases that may have affected results could not be eliminated. Second, patients with bone fractures who did not require hospitalization were excluded; thus, the study population may have been biased toward more severe cases being selected. Third, because TZDs promote weight gain, they were more likely to be administered (in light of their obesogenic properties) to non-overweight, low-BMI patients already at risk of fractures, which may have influenced the increased fracture risk associated with TZD use. Fourth, as this was a cross-sectional study, it was not possible to examine the effect of the length of administration period of diabetes drugs on fracture risk. Finally, because this study did not use data collected for research purposes, it lacks data regarding renal function, such as albuminuria, and information regarding Vitamin D3 and calcium preparations used for advanced renal dysfunction. Therefore, a detailed study stratifying kidney function could not be conducted.
Conclusions
In elderly patients with T2DM, the key factor associated with fractures was TZD use in both males and females. The present study also showed that TZD use increases risk of bone fractures necessitating hospitalization in males. These results may need to be considered while selecting hypoglycemic agents for treating elderly patients with T2DM. Information bias, selection bias, and the effect of concomitant drugs may be the underlying reasons for why eGFR < 60 mL / min / 1.73 m2 reduced the fracture risk. However, details are unknown, and additional investigations are needed.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADLs:
-
activities of daily living
- BG:
-
biguanides
- BMI:
-
body mass index
- CI:
-
confidence interval
- CKD:
-
chronic kidney disease
- DPP-4:
-
dipeptidyl peptidase-4
- eGFR:
-
estimated glomerular filtration rate
- GLP-1:
-
glucagon-like peptide-1
- HbA1c:
-
hemoglobin A1c
- ORs:
-
Odds ratios
- QOL:
-
quality of life
- SGLT2:
-
sodium glucose cotransporter 2
- SU:
-
sulfonylureas
- TZD:
-
thiazolidines
- αGI:
-
α-glucosidase inhibitors
References
Ensrud KE, Thompson DE, Cauley JA, Nevitt MC, Kado DM, Hochberg MC, et al. Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture Intervention Trial Research Group J Am Geriatr. 2000;48:41–9.
Nguyen ND, Center JR, Eisman JA, Nguyen TV. Bone loss, weight loss, and weight fluctuation predict mortality risk in elderly men and women. J Bone Miner Res. 2007;22:1147–54.
Suzuki T, Yoshida H. Low bone mineral density at femoral neck is a predictor of increased mortality in elderly Japanese women. Osteoporos Int. 2010;21:71–9.
Chippendale T, Gentile PA, James MK, Melnic G. Indoor and outdoor falls among older adult trauma patients: a comparison of patient characteristics, associated factors and outcomes. Geriatr Gerontol Int. 2017;17:905–12.
Sellmeyer DE, Civitelli R, Hofbauer LC, Khosla S, Lecka-Czernik B, Schwartz AV. Skeletal metabolism, fracture risk, and fracture outcomes in type 1 and type 2 diabetes. Diabetes. 2016;65:1757–66.
Melton LJ 3rd, Leibson CL, Achenbach SJ, Therneau TM, Khosla S. Fracture risk in type 2 diabetes: update of a population-based study. J Bone Miner Res. 2008;23:1334–42.
Janghorbani M, Van Dam RM, Willett WC, Hu FB. Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol. 2007;166:495–505.
Chen HF, Ho CA, Li CY. Increased risks of hip fracture in diabetic patients of Taiwan: a population-based study. Diabetes Care. 2008;31:75–80.
Yamamoto M, Yamaguchi T, Yamauchi M, Kaiji H, Sugimoto T. Diabetic patients have an increased risk of vertebral fractures independent of BMD or diabetic complications. J Bone Miner Res. 2008;24:702–9.
Losada E, Soldevila B, Ali MS, Martínez-Laguna D, Nogués X, Puig-Domingo M, et al. Real-world antidiabetic drug use and fracture risk in 12,277 patients with type 2 diabetes mellitus: a nested case–control study. Osteoporos Int. 2018;29:2079–86.
Li CI, Liu CS, Lin WY, Meng NH, Chen CC, Yang SY, et al. Glycated hemoglobin level and risk of hip fracture in older people with type 2 diabetes: a competing risk analysis of Taiwan diabetes cohort study. J Bone Miner Res. 2015;30:1338–46.
Soen S, Fukunaga M, Sugimoto T, Sone T, Fujiwara S, Endo N, et al. Diagnostic criteria for primary osteoporosis: year 2012 revision. J Bone Miner Metab. 2013;31:247–57.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–305.
Nickolas TL, McMahon DJ, Shane E. Relationship between moderate to severe kidney disease and hip fracture in the United States. J Am Soc Nephrol. 2006;17:3223–32.
Tseng CH, Huang WS, Li TC, Chen HJ, Muo CH, Kao CH. Increased risk of end-stage renal disease among hip fracture patients. Eur J Intern Med. 2014;25:956–61.
Pan HH, Li CY, Chen TJ, Su TP, Wang KY. Association of polypharmacy with fall-related fractures in older Taiwanese people: age- and gender-specific analyses. BMJ Open. 2014;28, 4.
Mitama Y, Fujiwara S, Yoneda M, Kira S, Kohno N. Association of type 2 diabetes and an inflammatory marker with incident bone fracture among a Japanese cohort. J Diabetes Investig. 2017;8:709–15.
Oei L, Zillikens MC, Dehghan A, Buitendijk GH, Castaño-Betancourt MC, Estrada K, et al. Bone mineral density and fracture risk in type 2 diabetes as skeletal complications of inadequate glucose control: the Rotterdam study. Diabetes Care. 2013;36:1619–28.
Kanazawa I, Yamaguchi T, Yamauchi M, Yamamoto M, Kurioka S, Yano S, et al. Adiponectin is associated with changes in bone markers during glycemic control in type 2 diabetes mellitus. J Clin Endocrinol Metab. 2009;94:3031–7.
Schwartz AV, Margolis KL, Sellmeyer DE, Vittinghoff E, Ambrosius WT, Bonds DE, et al. Intensive glycemic control is not associated with fractures or falls in the ACCORD randomized trial. Diabetes Care. 2012;35:1525–31.
Loke YK, Singh S, Furberg CD. Long-term use of thiazolidinediones and fractures in type 2 diabetes: a meta-analysis. CMAJ. 2009;180:32–9.
Schwartz AV, Chen H, Ambrosius WT, Sood A, Josse RG, Bonds DE, et al. Effects of TZD use and discontinuation on fracture rates in ACCORD bone study. J Clin Endocrinol Metab. 2015;100:4059–66.
Aubert RE, Herrera V, Chen W, Haffner SM, Pendergrass M. Rosiglitazone and pioglitazone increase fracture risk in women and men with type 2 diabetes. Diabetes Obes Metab. 2010;12:716–21.
Azoulay L, Yin H, Filion KB, Assayag J, Majdan A, Pollak MN, et al. The use of pioglitazone and the risk of bladder cancer in people with type 2 diabetes: nested case-control study. BMJ. 2012;344:e3645.
Acknowledgements
NA
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
TH designed the study and wrote the initial draft of the manuscript. YK contributed to analysis and interpretation of data and assisted in the preparation of the manuscript. All other authors have contributed to data collection and interpretation and have critically reviewed the manuscript. All authors approved the final version of the manuscript, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the ethical guidelines for medical and health research involving human subjects. The ethics board of the Tokyo Saiseikai Central Hospital approved the study (March 1, 2016; control number: 27–51).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Horii, T., Iwasawa, M., Kabeya, Y. et al. Investigating the risk of bone fractures in elderly patients with type 2 diabetes mellitus: a retrospective study. BMC Endocr Disord 19, 81 (2019). https://doi.org/10.1186/s12902-019-0413-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-019-0413-0