Abstract
Background
One of the major concerns of patients with upper tract urothelial carcinoma (UTUC) treated with nephroureterectomy is intravesical recurrence (IVR). The purpose of the present study was to investigate the predictive risk factors for IVR after retroperitoneoscopic nephroureterectomy (RNU) for UTUC.
Methods
Clinicopathological and surgical information were collected from the medical records of 73 patients treated with RNU for non-metastatic UTUC, without a history of or concomitant bladder cancer. The association between IVR after RNU and clinicopathological and surgery-related factors, including preoperative urine cytology and pneumoretroperitoneum time, was analyzed using the Fisher exact test.
Results
During the median follow-up time of 39.1 months, 18 (24.7%) patients had subsequent IVR after RNU. The 1- and 3-year IVR-free survival rates were 85.9% and 76.5%, respectively. The Fisher exact test revealed that prolonged pneumoretroperitoneum time of ≥ 210 min was a risk factor for IVR in 1 year after RNU (p = 0.0358) and positive urine cytology was a risk factor for IVR in 3 years after RNU (p = 0.0352).
Conclusions
In UTUC, the occurrences of IVR in 1 and 3 years after RNU are highly probable when the pneumoretroperitoneum time is prolonged (≥ 210 min) and in patients with positive urine cytology, respectively. Strict follow-up after RNU is more probable recommended for these patients.
Similar content being viewed by others
Background
Upper tract urothelial carcinoma (UTUC) is a relatively uncommon condition and accounts for 5–10% of all urothelial malignancies [1]. Nephroureterectomy (NU) with excision of the bladder cuff is the gold standard treatment for non-metastatic UTUC. However, intravesical recurrence (IVR) after NU for UTUC frequently occurs, with an incidence rate of approximately 22–47% [1,2,3,4]. Several studies have investigated the risk factors of IVR after NU for UTUC. Reportedly, the risk factors for IVR after NU for UTUC include positive preoperative urine cytology, preoperative diagnostic ureteroscopic biopsy for UTUC, surgery-related factors, such as laparoscopic surgery or endoscopic approach of the bladder cuff excision, lymphovascular invasion (LVI), and concomitant carcinoma in situ (CIS) [4,5,6,7,8].
Recently, laparoscopic NU (LNU) and retroperitoneoscopic NU (RNU) are being performed globally for UTUC. However, there have been discussions about whether LNU and RNU increase the risk of postoperative IVR compared to open NU, and a consensus is yet to be reached [9,10,11,12,13]. On the other hand, few studies have investigated the risk factors of IVR after LNU and RNU, including surgery-related factors.
The purpose of the present study was to investigate the association between IVR after RNU for UTUC and clinicopathological and surgical factors, including preoperative urine cytology, urinary bladder tumor antigen (BTA), urinary nuclear mitotic apparatus protein (NMP22), and pneumoretroperitoneum time.
Methods
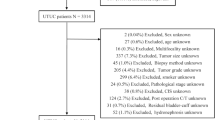
Patient selection
We retrospectively identified 102 patients treated with RNU for non-metastatic UTUC at Nippon Medical School Hospital between 2012 and 2020. UTUC was diagnosed using computed tomography (CT), magnetic resonance imaging (MRI), and urine cytology. A diagnostic ureteroscopic biopsy was performed when required. All patients underwent preoperative cystoscopy. Of the 102 patients, 29 patients with a history of bladder cancer or concomitant bladder cancer were excluded from our study. Finally, 73 patients were included in the study.
Clinicopathological data
From the medical records, we collected clinicopathological and surgical information of the patients, including age, sex, laterality and location of the main tumor, presence or absence of hydronephrosis, preoperative urine cytology, preoperative urinary BTA level, preoperative urinary NMP22 level, necessity of diagnostic ureteroscopic biopsy, pneumoretroperitoneum time, total operating time, multifocality of the tumor, tumor size, pathological characteristics, necessity of adjuvant systemic chemotherapy (ASC), and oncological outcomes. Tumors were staged according to the 2002 American Joint Committee of Cancer tumor-node-metastasis classification and were graded according to the 2004 World Health Organization classification [14].
Surgical procedure
While performing RNU, retroperitoneoscopic procedures were performed in the kidney position, with 8 mmHg CO2 gas pressure in all cases. The CO2 gas pressure was increased temporally when necessary. The maximum pressure of the CO2 gas was 12 mmHg. In the retroperitoneoscopic procedure, we clamped the ureter after ligation of the renal arteries. In all patients, a small iliac incision (Gibson incision) or lower abdominal midline incision was made to retrieve the kidney and ureter and to perform bladder cuff resection with sufficient surgical margin using the extravesical approach. In our institution, we have performed RNU in patients with non-metastatic localized or locally advanced UTUC (cTa-3N0M0). Lymphadenectomy was not performed in this study.
Adjuvant therapy and follow-up
Adjuvant intravesical therapy is not administered at our institution. Four courses of ASC, such as the gemcitabine/cisplatin regimen or gemcitabine/carboplatin regimen, were administered to select pT2–4 patients. Of these patients, those with an estimated glomerular filtration rate (eGFR) of < 30 ml/min/1.73 m2 received ASC with the gemcitabine/carboplatin regimen, and the other patients received ASC with the gemcitabine/cisplatin regimen. After RNU, all patients were generally followed-up using blood tests, urine analysis, urine cytology, cystoscopy, and CT scan every three months for two years, and every six months thereafter. We defined IVR as a pathologically diagnosed bladder cancer after RNU. We also defined progression disease as radiologically diagnosed local or distance recurrence.
Endpoint of the present study
The primary endpoint of the present study was to investigate the association between IVR after RNU for UTUC and clinicopathological and surgical factors, including preoperative factors of urine cytology, urinary BTA, urinary NMP22, and pneumoretroperitoneum time.
Statistical analysis
Statistical analyses were performed using JMP® 13 (SAS Institute Inc., Cary, NC, USA). The value of statistical significance was set at p < 0.05. The categorical variables were compared using the Fisher exact test and continuous variables using the t-test or the Mann–Whitney U test, depending on the results of the one-sample Kolmogorov–Smirnov test. Survival curves were constructed using the Kaplan–Meier method. To determine the risk factors for IVR in 1 and 3 years after RNU, the Fisher exact test was performed. In the analyses of IVR and progression 1 year after RNU, no IVR and progression cases without 1 year or > 1 year of follow-up were excluded. In the analyses of IVR and progression 3 years after RNU, no IVR and progression cases without 3 years or > 3 years of follow-up were excluded. The cut-off value of the pneumoretroperitoneum time of RNU was 210 min, which was defined as the maximum pneumoretroperitoneum time in the technical certification test of RNU by the Japanese Society of Endourology [15].
Results
Table 1 demonstrates the characteristics of 73 patients treated with RNU for UTUC. Surgical margins of the bladder cuff were negative in all patients.
During the median follow-up of 39.1 months after RNU, 18 (24.7%) patients had IVR. The 1-year and 3-year IVR-free survival rates were 85.9% and 76.5%, respectively (Fig. 1A). The histological type of bladder cancer in 18 patients was urothelial carcinoma. Table 2 demonstrates the multifocality and location of IVR tumors. In 50% of these bladder cancers, the grade was lower than that of the initial UTUC diagnosis. In the other 50% of bladder cancer cases, the grade was the same grade as that of the initial UTUC. None of the bladder cancers had a higher grade than the initial UTUC diagnosis.
The Fisher exact test revealed that prolonged pneumoretroperitoneum time of ≥ 210 min was a risk factor for IVR in 1 year after RNU (p = 0.0358) (Table 3) and positive urine cytology was a risk factor for IVR in 3 years after RNU (p = 0.0352) (Table 4).
Table 5 demonstrates two group analyses based on the pneumoretroperitoneum time of 210 min to investigate the presence of bias. No significant difference between these two groups was noted.
Of the 73 cases, 15 (20.5%) were positive for urine cytology, NMP22, and BTA, and 18 (24.7%) were positive for two of these three.
During the median follow-up of 41.9 months after LNU, 12 (16.4%) patients had a metastatic recurrence. The 1-year and 3-year progression-free survival (PFS) rates were 92.9% and 84.5%, respectively (Fig. 1B). The Fisher exact test revealed that pathological T ≥ 3 was a risk factor for progression in 1 year after RNU (p = 0.0439) (Table 6), and pathological T ≥ 3 (p = 0.0007), Grade 3 (p = 0.0145), LNI (p = 0.0073), and ASC (p = 0.0088) were the risk factors for progression in 3 years after RNU (Table 7).
Discussion
LNU is the mainstream surgery for UTUC and RNU is not popularly performed [8, 16, 17]. Therefore, most studies are focused on LNU. Here, we focused on RNU. This is the first report investigating the risk factors, including the pneumoretroperitoneum time, for IVR after RNU.
In this study, prolonged pneumoretroperitoneum time of ≥ 210 min was a risk factor for IVR in 1 year after RNU, with 8 mmHg CO2 gas pressure (Table 3). In a previous study, Shigeta et al. reported that prolonged pneumoperitoneum time of LNU for UTUC was an independent risk factor for IVR [8]. They performed LNU (62.8%) and RNU (37.2%) for their cohort. The results of the present and the previous studies suggested that CO2 gas pressure time impact on IVR. Shigeta et al. analyzed a cohort similar to this study that excluded patients with a history of bladder cancer or concomitant bladder cancer; the IVR rate was 47.3% during the median follow-up of 31.1 months postoperatively. They performed LNU or RNU with 10 mmHg CO2 gas pressure and the median pneumoperitoneum or pneumoretroperitoneum time was 150 min; meanwhile, the median pneumoretroperitoneum time of the present study was 202 min, which was significantly longer than that of their study. However, in the present study, the IVR rate after RNU was 24.7% during the median follow-up of 39.1 months postoperatively, which was significantly lower than that of the study by Shigeta et al. When the two studies were compared, the differences were observed in CO2 gas pressure and surgical procedure. It was suggested that a low CO2 gas pressure of 8 mmHg and/or RNU in the present study might have influenced the low IVR rates. Further studies with large cohorts comparing different CO2 gas pressures are needed to investigate the impact of CO2 gas pressure on IVR postoperatively. Moreover, we only analyzed RNU in this study; therefore, it remains unclear whether the results of this study apply to LNU, because the pressure on the ureter during surgery might be different between RNU and LNU. Further studies comparing RNU and LNU are required.
This study was a retrospective study without a pilot study. The study began in February 2021, and the results were disclosed to all urologists at our institution in April 2021. Therefore, there was no bias of knowledge in the study results. We also analyzed the factors related to prolonged pneumoretroperitoneum time. However, any factors related to prolonged pneumoretroperitoneum time were not present (Table 5).
Recent molecular genetic studies have suggested that intraluminal seeding is one of the main mechanisms of IVR after NU [18,19,20]. It was also reported that continuous intravesical irrigation with distilled water or physiological saline solution during LNU decreased the rate of IVR incidence [16]. They concluded that continuous intravesical irrigation might eliminate cancer cells floating in the bladder during surgery before they become engrafted on the mucous membrane of the bladder. This result suggests that IVR after NU occurs due to intraluminal seeding. Recent studies demonstrated that prolonged CO2 gas pressure time and diagnostic ureteroscopic biopsy are independent factors of IVR after NU [5, 8]. Based on these results of past studies, long-term CO2 gas pressure to the tumor and direct destruction of the tumor by diagnostic ureteroscopic biopsy might contribute to intraluminal seeding. In the present study, the grade of bladder cancer with IVR was not higher than that of initial UTUC. It has also been suggested that IVR tumors are caused by intraluminal seeding from UTUC.
The BTA test detects the human complement factor H-related protein secreted in the urine. While the NMP22 test detects the protein level of the nuclear mitotic apparatus. Positive urinary BTA and NMP22 have been reported as predictors of the presence of bladder cancer and UTUC, along with positive urine cytology [21,22,23,24]. In the present study, the risk factor for IVR 3 years after RNU was not positive urinary BTA or urinary NMP22, but positive urine cytology (Table 4). Additionally, only 20.5% of patients had all three positive urine cytology, urinary BTA, and urinary NMP22. There is not much overlap between urine cytology, urinary BTA, and urinary NMP22. Urinary BTA and NMP22 are considered unsuitable for predicting IVR after RNU because the values of urinary BTA and NMP22 generally have a positive correlation with tumor volume; however, urinary BTA and NMP22 do not directly detect cancer cells.
Physical injury to the bladder is associated with increased adherence of tumor cells to the urothelium [25]. In NU, the bladder cuff and ureteral orifice are resected, while a urethral catheter is maintained in the bladder during and several days after NU. Physical injury to the urothelium, such as bladder cuff resection and stimulation of the bladder mucosa with a ureteral catheter, might support the growth of tumor cells in the urothelium [26]. In the present study, 11 (61.1%) and 5 (27.8%) patients had IVR tumors located at scar site and bladder neck, which could have been stimulated by the urethral catheter (Table 2). Hence, this result is consistent with the that of the previous study [26].
Recently, two prospective randomized trials have demonstrated that a single early intravesical chemotherapy cycle using mitomycin C or pirarubicin after NU decreased the risk of IVR [27, 28]. However, the type of patients that will benefit from this treatment remains unclear. In this study, prolonged pneumoretroperitoneum time of ≥ 210 min was a risk factor for IVR in 1 year after RNU and positive urine cytology was a risk factor for IVR in 3 years after RNU. From our results, we strongly recommend that patients with pneumoperitoneum time of ≥ 210 min and/or with positive urine cytology should receive a single early intravesical chemotherapy after RNU with 8 mmHg CO2 gas pressure.
In this study, pathological findings of UTUC were the risk factors for progression after RNU, not pneumoretroperitoneum time (Tables 6, 7). Therefore, when the pneumoretroperitoneum time of RNU is prolonged, an attending physician can perform a follow-up imaging after RNU at normal intervals.
The present study has several limitations. UTUC is a relatively uncommon condition. We excluded patients with a history of bladder cancer or concomitant bladder cancer, because the purpose of the present study was to investigate the risk factors for IVR after RUN for UTUC. In addition, this study was conducted in a single institution; therefore, the cohort in this study was small. Since the study was a retrospective analysis, there might be a selection bias for the surgeons. In this study, 13 surgeons performed the RUN procedure. However, three experienced surgeons who had performed more than 100 laparoscopic surgeries performed or supervised all of the RUN procedures. In addition, the rate of IVR incidence in our study was lower than that reported in previous studies. Based on these facts, we believe that the participation of inexperienced surgeons in RUN had little impact on the IVR rate in the present study. To reduce these limitations, prospective studies with larger cohorts from several institutions are required. Currently, lymphadenectomy is recommended for pathological T ≥ 2 UTUC. However, lymphadenectomy was not performed in this study. The reasons are that there are several discrepancies between the clinical T stage and the pathological T stage, and there are technical issues with retroperitoneoscopic lymphadenectomy. The lack of lymphadenectomy in this study might impact on PFS. In our institution, we performed open NU and lymphadenectomy only in cases suspected of visible lymph node metastasis on CT. There is an urgent need to improve the accuracy of diagnostic imaging for staging and lymphadenectomy for clinical T ≥ 2 UTUC. Finally, the risks of IVR logically related to the time from infusing CO2 gas pressure to the clipping of the ureter. However, we were only able to collect the data on clipping time of the ureter for some patients using their operation and intraoperative nursing records. Therefore, it was difficult to analyze association between IVR after RNU and the time from infusing CO2 gas pressure to the clipping of the ureter. Further studies analyzing the association between IVR after RNU and the time from infusing CO2 gas pressure to the clipping of the ureter are required.
Conclusions
In UTUC, the occurrence of IVR in 1 year after RNU is highly probable when the pneumoretroperitoneum time is prolonged (≥ 210 min) and the occurrence of IVR in 3 years after RNU is highly probable in patients with positive urine cytology. Strict follow-up after RNU is more probable recommended for these patients.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ASC:
-
Adjuvant systemic chemotherapy
- BTA:
-
Bladder tumor antigen
- CIS:
-
Carcinoma in situ
- CT:
-
Computed tomography
- eGFR:
-
Estimated glomerular filtration rate
- INF:
-
Infiltrative growth
- IVR:
-
Intravesical recurrence
- LNU:
-
Laparoscopic nephroureterectomy
- LVI:
-
Lymphovascular invasion
- NMP22:
-
Nuclear mitotic apparatus protein 22
- NU:
-
Nephroureterectomy
- PFS:
-
Progression-free survival
- RNU:
-
Retroperitoneoscopic nephroureterectomy
- UTUC:
-
Upper tract urothelial carcinoma
References
Rouprêt M, Babjuk M, Burger M, Capoun O, Cohen D, Compérat EM, et al. European association of urology guidelines on upper urinary tract urothelial carcinoma: 2020 update. Eur Urol. 2021;79:62–79.
Tanaka N, Kikuchi E, Kanao K, Matsumoto K, Shirotake S, Kobayashi H, et al. The predictive value of positive urine cytology for outcomes following radical nephroureterectomy in patients with primary upper tract urothelial carcinoma: a multi-institutional study. Urol Oncol. 2014;32(48):e19-26.
Hirano D, Okada Y, Nagane Y, Satoh K, Mochida J, Yamanaka Y, et al. Intravesical recurrence after surgical management of urothelial carcinoma of the upper urinary tract. Urol Int. 2012;89:71–7.
Liu W, Wang Z, Liu S, Yao Y, Liu Y, Zhang G. Preoperative positive voided urine cytology predicts poor clinical outcomes in patients with upper tract urothelial carcinoma undergoing nephroureterectomy. BMC Cancer. 2020;20:1113.
Sharma V, Miest TS, Juvet TS, Toussi A, Packiam V, Chamie K, et al. The impact of upper tract urothelial carcinoma diagnostic modality on intravesical recurrence after radical nephroureterectomy: a single institution series and updated meta-analysis. J Urol. 2021. https://doi.org/10.1097/JU.0000000000001834.
Xylinas E, Colin P, Audenet F, Phe V, Cormier L, Cussenot O, et al. Intravesical recurrence after radical nephroureterectomy for upper tract urothelial carcinomas: predictors and impact on subsequent oncological outcomes from a national multicenter study. World J Urol. 2013;31:61–8.
Xylinas E, Rink M, Cha EK, Clozel T, Lee RK, Fajkovic H, et al. Upper Tract Urothelial Carcinoma Collaboration. Impact of distal ureter management on oncologic outcomes following radical nephroureterectomy for upper tract urothelial carcinoma. Eur Urol. 2014;65:210–7.
Shigeta K, Kikuchi E, Hagiwara M, Ando T, Mizuno R, Miyajima A, et al. Prolonged pneumoperitoneum time is an independent risk factor for intravesical recurrence after laparoscopic radical nephroureterectomy in upper tract urothelial carcinoma. Surg Oncol. 2017;26:73–9.
Shigeta K, Kikuchi E, Abe T, Hagiwara M, Ogihara K, Anno T, et al. Long-term oncologic outcomes of laparoscopic versus open radical nephroureterectomy for patients with T3N0M0 upper tract urothelial carcinoma: a multicenter cohort study with adjustment by propensity score matching. Ann Surg Oncol. 2019;26:3774–81.
Kim SH, Song MK, Kim JK, Hong B, Kang SH, Ku JH, et al. Laparoscopy versus open nephroureterectomy in prognostic outcome of patients with advanced upper tract urothelial cancer: a retrospective, multicentre, propensity-score matching analysis. Cancer Res Treat. 2019;51:963–72.
Piszczek R, Nowak Ł, Krajewski W, Chorbińska J, Poletajew S, Moschini M, et al. Oncological outcomes of laparoscopic versus open nephroureterectomy for the treatment of upper tract urothelial carcinoma: an updated meta-analysis. World J Surg Oncol. 2021;19:129.
Ni S, Tao W, Chen Q, Liu L, Jiang H, Hu H, et al. Laparoscopic versus open nephroureterectomy for the treatment of upper urinary tract urothelial carcinoma: a systematic review and cumulative analysis of comparative studies. Eur Urol. 2012;61:1142–53.
Seisen T, Granger B, Colin P, Léon P, Utard G, Renard-Penna R, et al. A systematic review and meta-analysis of clinicopathologic factors linked to intravesical recurrence after radical nephroureterectomy to treat upper tract urothelial carcinoma. Eur Urol. 2015;67:1122–33.
Soukup V, Čapoun O, Cohen D, Hernández V, Babjuk M, Burger M, et al. Prognostic performance and reproducibility of the 1973 and 2004/2016 World Health Organization Grading Classification Systems in Non-muscle-invasive Bladder Cancer: a European Association of Urology non-muscle invasive bladder cancer guidelines panel systematic review. Eur Urol. 2017;72:801–13.
Yanagi M, Kimura G, Sekine T, Takeda H, Akatsuka J, Endo Y, et al. Factors associated with prolonged retroperitoneal laparoscopic radical nephrectomy performed by non-expert surgeons. J Nippon Med Sch. 2021;88:109–12.
Yamamoto S, Sakamoto S, Imamura Y, Sazuka T, Nakamura K, Inoue T, et al. Intravesical irrigation might prevent bladder recurrence in patients undergoing radical nephroureterectomy for upper urinary tract urothelial carcinoma. Int J Urol. 2019;26:791–6.
Zou L, Zhang L, Zhang H, Jiang H, Ding Q. Comparison of post-operative intravesical recurrence and oncological outcomes after open versus laparoscopic nephroureterectomy for upper urinary tract urothelial carcinoma. World J Urol. 2014;32:565–70.
Hafner C, Knuechel R, Stoehr R, Hartmann A. Clonality of multifocal urothelial carcinomas: 10 years of molecular genetic studies. Int J Cancer. 2002;101:1–6.
Hafner C, Knuechel R, Zanardo L, Dietmaier W, Blaszyk H, Cheville J, et al. Evidence for oligoclonality and tumor spread by intraluminal seeding in multifocal urothelial carcinomas of the upper and lower urinary tract. Oncogene. 2001;20:4910–5.
Miyake H, Hara I, Kamidono S, Eto H. Multifocal transitional cell carcinoma of the bladder and upper urinary tract: molecular screening of clonal origin by characterizing CD44 alternative splicing patterns. J Urol. 2004;172:1127–9.
Babjuk M, Soukup V, Pesl M, Kostírová M, Drncová E, Smolová H, et al. Urinary cytology and quantitative BTA and UBC tests in surveillance of patients with pTapT1 bladder urothelial carcinoma. Urology. 2008;71:718–22.
Walsh IK, Keane PF, Ishak LM, Flessland KA. The BTA stat test: a tumor marker for the detection of upper tract transitional cell carcinoma. Urology. 2001;58:532–5.
Kumar A, Kumar R, Gupta NP. Comparison of NMP22 BladderChek test and urine cytology for the detection of recurrent bladder cancer. Jpn J Clin Oncol. 2006;36:172–5.
Jovanovic M, Soldatovic I, Janjic A, Vuksanovic A, Dzamic Z, Acimovic M, et al. Diagnostic value of the nuclear matrix protein 22 test and urine cytology in upper tract urothelial tumors. Urol Int. 2011;87:134–7.
See WA, Chapman PH. Heparin prevention of tumor cell adherence and implantation on injured urothelial surfaces. J Urol. 1987;138:182–6.
Ito A, Shintaku I, Satoh M, Ioritani N, Tochigi T, Numata I, et al. Intravesical seeding of upper urinary tract urothelial carcinoma cells during nephroureterectomy: an exploratory analysis from the THPMG trial. Jpn J Clin Oncol. 2013;43:1139–44.
Ito A, Shintaku I, Satoh M, Ioritani N, Aizawa M, Tochigi T, et al. Prospective randomized phase II trial of a single early intravesical instillation of pirarubicin (THP) in the prevention of bladder recurrence after nephroureterectomy for upper urinary tract urothelial carcinoma: the THP Monotherapy Study Group Trial. J Clin Oncol. 2013;31:1422–7.
O'Brien T, Ray E, Singh R, Coker B, Beard R; British Association of Urological Surgeons Section of Oncology. Prevention of bladder tumours after nephroureterectomy for primary upper urinary tract urothelial carcinoma: a prospective, multicentre, randomised clinical trial of a single postoperative intravesical dose of mitomycin C (the ODMIT-C Trial). Eur Urol. 2011;60:703–10.
Acknowledgements
The authors thank Editage for editing English of our manuscript.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
Conception and Design: MY Collection of data: MY and YE Data analysis: MY. Manuscript writing: All authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. The Ethics Committee at Nippon Medical School Hospital approved this study (approval number: 30–03-1100). All study participants provided informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yanagi, M., Hamasaki, T., Akatsuka, J. et al. Risk factor analysis of intravesical recurrence after retroperitoneoscopic nephroureterectomy for upper tract urothelial carcinoma. BMC Urol 21, 167 (2021). https://doi.org/10.1186/s12894-021-00932-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-021-00932-2