Abstract
Background
Ectopic mediastinal parathyroid tumor (EMPT) is a rare cause of primary hyperparathyroidism (PHPT); it is difficult to resect using the cervical approach. We describe a case of using video-assisted thoracic surgery (VATS) for EMPT resection.
Case presentation
A 67-year-old woman with a history of postoperative thyroid cancer had no symptoms. She was diagnosed with PHPT and underwent thyroid cancer surgery. She had serum calcium and intact parathyroid hormone (PTH) levels of 11.1 mg/dL and 206 pg/mL, respectively. Chest computed tomography showed a 10-mm nodule in the anterior mediastinum. Technetium-99 m methoxyisobutyl isonitrile scintigraphy showed an abnormal uptake lesion in the anterior mediastinum. She was diagnosed with PHPT caused by EMPT and underwent VATS. The pathological examination confirmed parathyroid adenoma. Her serum calcium and intact PTH levels were normal from 15 min after tumor resection. She has had no recurrence of EMPT.
Conclusions
The VATS approach was effective for the resection of EMPT.
Similar content being viewed by others
Background
Primary hyperparathyroidism (PHPT) is a disease that excessively secretes parathyroid hormone (PTH) and causes osteoporosis, ureteral stone, and hypercalcemia. The incidence of asymptomatic PHPT that is discovered by chance during examination of other diseases has been increasing. Ectopic mediastinal parathyroid tumor (EMPT) is a rare cause of PHPT. Although most parathyroid adenomas are located in the neck, only 1–2% of them are located in the mediastinum [1]. As surgical resection of EMPT is often difficult to perform using the cervical approach, thoracoscopic surgical resection has been used for the resection. We describe a case of video-assisted thoracoscopic surgery (VATS) for excision of EMPT. In this case, detailed preoperative information and magnified visual fields through the thoracoscope led to the correct tumor location.
Case presentation
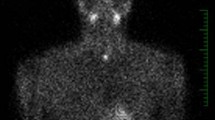
A 67-year-old woman with a history of thyroid cancer surgery had no symptoms. Her serum calcium and intact PTH levels were high according to the blood biochemical examination when she underwent thyroid cancer surgery. Chest computed tomography showed a 10-mm nodule in the anterior mediastinum (Fig. 1a). Technetium-99 m methoxyisobutyl isonitrile (99mTc-MIBI) scintigraphy showed an abnormal uptake lesion in the anterior mediastinum (Fig. 1b). She was diagnosed with PHPT caused by EMPT. Although she was followed up for 7 years, her serum calcium and PTH levels increased. Because the cervical approach was considered difficult for surgical resection, she was referred to our department. Preoperatively, she had a serum calcium level of 11.1 mg/dL (normal range, 8.5–9.9 mg/dL) and intact PTH level of 206 pg/mL (normal range, 16–65 pg/mL).
Under general anesthesia, she was intubated with a double-lumen endotracheal tube and positioned in a right lateral decubitus position. A 4-cm vertical skin incision along the left breast trailing edge at the fourth rib was made, mini-thoracotomy was performed at the fourth intercostal space, and an XXS size wound retractor (Alexis® Wound Retractor; Applied Medical, Rancho Santa Margarita, CA, USA) was placed. A 10.5-mm thoracoport was inserted at the sixth intercostal space of the anterior axillary line and a rigid 30° thoracoscope was inserted into the seventh intercostal space of the middle axillary line. By careful inspection of the anterior mediastinum using a thoracoscope, we found a small 15-mm-diameter dark red nodule, which differed in color from its surroundings, inside the thymus and in front of the ascending aorta (Fig. 2). Without fracturing its capsule, the tumor was removed with thymic tissue. Fifteen minutes after resecting the nodule, her serum PTH level decreased immediately and became 27 pg/mL.
The pathological examination confirmed the diagnosis of parathyroid adenoma (Fig. 3). She had a serum calcium level of 8.9 mg/dL on the first postoperative day, and her postoperative course was uncomplicated. She has had no increase of serum calcium and PTH levels and no recurrence of EMPT.
Discussion and conclusions
PHPT causes hypercalcemia, urolithiasis, and osteoporosis due to hypersecretion of PTH. In PHPT, the incidence of EMPT is rare at about 1–2% [1]. The superior parathyroid glands develop from the fourth pharyngeal sac and descend along the esophagus with the thyroid gland. Therefore, parathyroid glands may be present in the posterior mediastinum. As the inferior parathyroid glands develop from the third pharyngeal sac and descend with the thymus, the parathyroid gland may be present in the anterior mediastinum [2]. In this case, the parathyroid adenoma was found in the anterior mediastinum, so it was considered to be EMPT derived from the inferior parathyroid gland.
Recently, the incidence of asymptomatic PHPT has increased because of improvement of examinations, which has resulted in an increase in surgical cases. The National Institutes of Health criteria for surgery in asymptomatic PHPT are as follows: (i) serum calcium level > 1.0 mg/dl above the normal upper limit; (ii) creatinine clearance < 60 ml/min, the presence of nephrolithiasis or nephrocalcinosis, or marked hypercalciuria (> 400 mg/dl); (iii) bone density T-score < − 2.5 standard deviation or medical history of vulnerable fracture; and (iv) age < 50 years. When patients meet one of these criteria, surgery is recommend [3]. In the present case, the serum calcium level increased by more 1.0 mg/dl above the normal upper limit.
PHPT is diagnosed based on serological and imaging findings. Serologically, PHPT shows high serum calcium and PTH levels and low serum phosphorus levels. For the treatment of EMPT, localization diagnosis by imaging examinations, such as computed tomography, magnetic resonance imaging, and ultrasonography, is important. The diagnostic rate of responsible lesions increased for PHPT using 99mTc-MIBI scintigraphy. By using the intraoperative intact PTH rapid measurement in EMPT surgery, the failure rate of surgery decreased from 21.2 to 3% [4]. Further, when using the preoperative diagnosis and intraoperative intact PTH rapid measurement, a minimally invasive approach is mainly used to remove only the responsible lesion. Depending on the tumor location, various approaches have been used for EMPT surgery. If the tumor is on the head side of the brachiocephalic vein, the cervical approach is used, and if the tumor is on the foot side of the brachiocephalic vein, median sternotomy or thoracotomy is selected. Recently, minimally invasive thoracoscopic surgery has been performed for PHPT [5]. It is important to use examinations such as preoperative 99mTc-MIBI scintigraphy and the intraoperative intact PTH rapid measurement to ensure tumor removal by thoracoscopic surgery.
As it is often difficult to identify EMPT intraoperatively, a method for identifying the tumor by administering methylene blue at the time of intraoperative has been reported. Injury of the capsule of the tumor causes seeding, so an easy method, such as administering methylene blue, is needed to identify the tumor [6].
For surgical treatment of EMPT, it is important to combine examinations such as preoperative 99mTc-MIBI scintigraphy and the intraoperative intact PTH rapid measurement to ensure tumor removal by thoracoscopic surgery.
Availability of data and materials
All the data and materials supporting our findings are included within the article.
Abbreviations
- 99mTc-MIBI:
-
Technetium-99 m methoxyisobutyl isonitrile
- EMPT:
-
Ectopic mediastinal parathyroid tumor
- PHPT:
-
Primary hyperparathyroidism
- PTH:
-
Parathyroid hormone
- VATS:
-
Video-assisted thoracoscopic surgery
References
Noussios G, Anagnostis P, Natsis K. Ectopic parathyroid glands and their anatomical, clinical, and surgical implications. Exp Clin Endoclinol Diabetes. 2012;120:604–10.
Miya A. Diagnosis and surgical treatment of hyperparathyroidism arising from ectopic parathyroid glands. Official Journal of the Japan Association of Endocrine Surgeons and the Japanese Society of Thyroid Surgery. 2012;29:193–7.
Bilezikian JP, Brandi ML, Eastell R, Silverberg SJ, Udelaman R, Marcocci C, et al. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the fourth international workshop. J Clin Endocrinol Metab. 2014;99:3561–9.
Sagan D, Gozadziuk K. Surgical treatment of mediastinal parathyroid adenoma: rationale for intraoperative parathyroid hormone monitoring. Ann Thorac Surg. 2010;89:1750–5.
Ishikawa M, Sumitomo S, Imamura N, Nishida T, Mineura K. A rare case of mediastinal functioning parathyroid adenoma removed successfully with thoracoscopy. J Surg Case Rep. 2017;4:1–3.
Adachi Y, Nakamura H, Taniguchi Y, Miwa K, Fujioka S, Haruki T. Thoracoscopic resection with intraoperative use of methylene blue to localize mediastinal parathyroid adenoma. Gen Thorac Cardiovasc Surg. 2012;60:168–70.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SM drafted the manuscript. HM performed the surgery. HA, TI, and TM assisted in performing the surgery. HO examined the pathologic pictures of the tumor. MK critically revised the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The patient consented to publication of this case. A copy of written consent is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Mitsuboshi, S., Maeda, H., Aoshima, H. et al. Thoracoscopic surgical case of an ectopic mediastinal parathyroid adenoma detected by chance: a case report. BMC Surg 19, 171 (2019). https://doi.org/10.1186/s12893-019-0641-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-019-0641-2