Abstract
Background
Primary hyperparathyroidism is a common endocrine disorder. Hypercalcemia with normal PTH levels is very unusual and can lead to diagnostic difficulties. There are very few very few studies in the literature and all with limited numerical samples. The goal of the present study was to determine the real incidence and characteristics of primary hyperparathyroidism with normal PTH and to evaluate if intraoperative PTH testing is useful in these patients.
Methods
We performed a retrospective review of 314 patients who had undergone parathyroidectomy to treat primary hyperparathyroidism between January 2002 and December 2016. Patients were divided in two groups according to biochemical preoperative findings: in Group A were included patients with normal serum PTH, in Group B those with increased serum PTH.
Results
Nine patients (3.7%) were included in group A and 235 in group B. Patients in group A were younger (51.5 ± 12.9 years vs 59.6 ± 12.5); preoperative serum calcium and the incidence of coexisting thyroid disease were similar between the two groups. Symptomatic patients were more frequent in Group A (77.8% vs 39.1%; p = 0.048). There were no significant differences regarding preoperative localization studies and surgical procedure. Intraoperative PTH determination demonstrated sensitivity of 86% in group A and 97% in group B, specificity and positive predictive value of 100% in both the groups, negative predictive value of 67% in group A and 79% in group B. Histopathological examination demonstrated a single gland disease in 8 (88.9%) patients in group A and a multi gland disease in 1 (11.1%), in group B single gland disease was found in 218 (92.8%) patients and multi gland disease in 17 (7.2%). Unsuccessful surgery with persistent or recurrent hyperparathyroidism occurred in 1 (11.1%) patient in group A and 4 (1.7%) in group B.
Conclusions
Primary hyperparathyroidism with normal PTH is rare but physicians should be aware of this possibility in patients with hypercalcaemia. Patients with normal PTH levels are younger and more frequently symptomatic. Intraoperative PTH testing plays an important role in the operative management even in such patients.
Similar content being viewed by others
Background
Primary hyperparathyroidism (PHP) is the third most common endocrine disorder in the United States and the second most common cause of hypercalcemia [1,2,3,4,5,6,7].
The diagnosis of PHP is classically based on the finding of hypercalcemia in the presence of high (or non suppressed) PTH levels [6, 8,9,10,11]; additional laboratory hallmark features are hypophosphatemia and elevated urinary cyclic adenosine monophospate [10]. Unfortunately, the diagnosis is not always so simple and a number of other factors must be considered [6]. Preoperative serum calcium and intact-parathyroid hormone (iPTH) levels are the most useful diagnostic parameters that allow differentiating PHP from non-parathyroid-dependent hypercalcemia [10]. Parathyroid adenomas, predominantly composed of chief cells, are the most common cause of PHP [10].
While normocalcemic hyperparathyroidism is well recognized in PHP, less is known about patients with high calcium but normal iPTH possibly leading to diagnostic difficulties [1, 3, 9, 10, 12,13,14]. The literature on this condition is poor and consists mainly of clinical cases [3, 4, 12,13,14,15,16]. An incidence of 5 to 33% has been documented in the literature [2, 10, 12, 13, 17] but no etiologic explanation has been given [10]. In 1987, parathyroid-hormone-related peptide (PTHrp) has been isolated as a causative factor of malignant hypercalcemia [10]. Previous studies have suggested that this condition is a less symptomatic, lighter and weaker form of PHP [18].
Intraoperative PTH (IoPTH) testing has revolutionized the way we treat patients with PHP by allowing focused and minimally invasive procedures [1, 19, 20]. The successful removal of hyperfunctioning parathyroid glands is indicated by a decrease in PTH levels > 50% within 10–20 min [1, 21, 22].
The goal of the present study was to determine the real incidence and characteristics of PHP with normal PTH and to evaluate if IoPTH testing is useful in these patients.
Methods
After approval from our Institutional Board Committee we performed a retrospective review of 314 patients who had undergone parathyroidectomy to treat PHP between January 2002 and December 2016 within the Unit of General and Endocrine Surgery at the University of Cagliari, Italy. Only patients with preoperative PHP diagnosis were included in this study: 61 patients in which diagnosis was made during neck surgery for other diseases as well as 10 patients with persistent or recurrent PHP were excluded from the study.
We analysed the following data: age, sex, comorbidities, coexisting thyroid diseases, serum calcium and PTH levels, preoperative localization studies, surgical procedure, histopathological features and follow up.
Serum PTH level was defined normal for values ranging from 15 pg/ml to 65 pg/ml. Patients were considered symptomatic if presenting with typical symptoms of hyperparathyroidism (urolithiasis, osteoporosis with bone or joint pain, mood or neurological disorders, cardiovascular disease). Preoperative localization studies (neck ultrasound (US) and MIBI scans) were performed preoperatively in all patients.
All the patients were submitted to parathyroidectomy. IoPTH determination was routinely used during surgery to confirm removal of all pathological glands; we defined a positive test when PTH value 10′ after excision of suspected pathological gland was 50% or lesser than preoperative value and when it was within range values (10–65 pg/ml). In case of negative test another measurement was made 20′ after excision and, if negative result was confirmed, a bilateral exploration was performed.
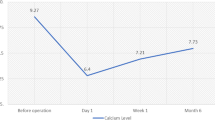
Patient follow-up was performed by serum calcium and PTH dosing once daily during hospitalization, then once a week for the first month and every 6 months thereafter. Definition of persistent or recurrent hyperparathyroidism was used in the case of high serum and calcium PTH levels detected within or after 6 months postoperatively, respectively.
Patients were divided in two groups according to biochemical preoperative findings: in Group A were included patients with PHP and normal serum PTH, in Group B those with PHP and increased serum PTH.
Statistical analysis
Chi-squared test was used for categorical data and t-test for continuous variables. Results were considered statistically significant if p value was ≤0.05. Continuous data are reported as the mean value ± standard error of the mean. Calculations were performed with MedCalc ® 12.7.0.0.
Results
Two-hundred and forty-four patients with preoperative diagnosis of PHP were included in the study. Nine patients (3.7%) were included in group A (PHP with normal serum PTH), with a mean preoperative serum PTH of 55 ± 12.2 pg/ml, and 235 in group B (PHP with increased serum PTH), with a mean preoperative serum PTH of 305 ± 301.1 pg/ml.
Full demographic and clinical data are reported in Table 1. Patients in group A were younger (51.5 ± 12.9 years vs 59.6 ± 12.5), even if this difference was not statistically significant (p = 0.06). Preoperative serum calcium was similar between the two groups (11.2 ± 0.6 mg/dl vs 11.4 ± 1.2 mg/dl; p = 0.64); also the incidence of coexisting thyroid disease was similar (33.3% vs 30.6%; p = 0.84). Symptomatic patients were more frequent in Group A (77.8% vs 39.1%; p = 0.048).
Surgical procedure, histopathological diagnosis and surgical outcome are reported in Table 2. Surgical procedure consisted in mini-invasive parathyroidectomy in 4 (44.4%) patients in group A and in 143 (60.8%) patients in group B. Histopathological examination demonstrated a single gland disease in 8 (88.9%) patients in group A and a multi gland disease in 1 (11.1%); in group B, single gland disease was found in 218 (92.8%) patients and multi gland disease in 17 (7.2%) (p = 0.83). Unsuccessful surgery with persistent or recurrent PHP occurred in 1 (11.1%) patient in group A and 4 (1.7%) in group B (p = 0.44).
IoPTH determination demonstrated sensitivity of 86% in group A and 97% in group B, specificity and positive predictive value of 100% in both the groups, negative predictive value of 67% in group A and 79% in group B (Table 3).
Odds ratio of patients of patients with PHP with normal serum PTH are reported in Table 4.
Discussion
Normohormonal PHP is a distinct PHP entity that exhibits normal PTH levels [14]. Since 1976, approximately 140 cases of hypercalcemia and normal PTH levels due to parathyroid adenoma have been reported in the literature [4, 10, 15, 16]. The true incidence of normohormonal PHP is very difficult to ascertain [14]. The reported incidence in the literature is 3–10.5% [6, 13, 14, 18, 23, 24]. To our knowledge, the cohort of Amin [18] of 58 sporadic PHP patients with normal PTH levels is the largest reported in the literature to date. However, because of the difficulty in recognizing this entity, the number of patients with normohormonal PHP could be much higher [14]. We report 9 cases of PHP with normal PTH with a rate of 3.7%, in line with other reports in the literature.
The first authors to propose potential etiopathogenetic mechanisms were Hollenberg and Arnold [15] in 1991. Theories have included the pulsatile secretion of PTH, the secretion of abnormal PTH altering its measurement but not its function, the presence of unmeasured active PTH fragments, the presence of a circulating antibodies interfering with the assay, the presence of another mediator of hypercalcemia (PTH-related peptide), and the increased peripheral tissue sensitivity to normal PTH [2, 8, 10, 14, 16, 17, 25]. Potential mechanisms to consider are also discrepancies between different types of equipment, methods of dosing and sampling as well as early diagnosis [14]. Wallace [14] also hypothesize lower PTH setpoints in some patients and anatomic barriers in local circulation around a parathyroid neoplasm.
Patients with normal PTH were a decade younger with an increased frequency of premenopausal females compared to the patients with overt PHP [12]. Our experience confirms that patients with normal PTH tend to be younger (51.5 ± 12.9 vs 59.6 ± 12.5 years) even if the data does not reach full statistical significance (p = 0.06).
The patients in the normal PTH group did not differ in symptoms and signs from the patients in the overt PHP group, supporting the concept that the PTH level does not correlate with patient symptoms [12, 13, 18, 23]. The normal serum PTH values delayed diagnosis in a significant proportion of patients (40%) in the study of Mischis-Troussard [13]. In our experience patients with normal PTH were more frequently symptomatic (77.7% vs 39.1%, p = 0.048) probably in relation to the fact that the diagnosis was taken into consideration later and that, in these cases, we tend to operate only patients with relevant symptomatology.
Patients with normal levels of PTH had smaller adenomas with low bone turn-over and preserved bone density and glomerular filtration rate compared with the patients with overt PHP [12, 13, 18]. In the experience of Amin [18], imaging modalities were less sensitive perhaps for the small gland weight, although the results were not statistically significant. In our experience the sensitivities of US and 99mTc sestamibi parathyroid scintigraphy were comparable to those observed in the entire PHP group; these results were similar to other reports in the literature [13].
Alhefdhi [1] reports higher rates of multi gland diseases; on the contrary, Amin [18] did not find differences. Our results are in line with those of Amin [18]: we detected only one case of multi gland disease among patients with normal PTH and the difference with group B was not statistically significant.
In the experience of Mischis-Troussard [13], the frequency of parathyroid hyperplasia was high (20%), but not enough to conclude that the proportion of hyperplasia is higher in PHP with normal serum PTH levels. Our results are in line with this report.
The use of IoPTH associated with MIP has allowed to reduce the operative time, the length of hospital stay and the costs, as well as to eliminate the risk of bilateral recurrent laryngeal nerve palsies and hypocalcemia [1, 26,27,28]. In the experience of Amin [18] a MIP or unilateral exploration was feasible in 43% of patients, while most were submitted to a bilateral neck exploration, probably for the smaller gland weight and the problems in preoperative localization [18]. In our experience, we have carried out the same surgical strategy in both groups and the incidence of MIP and bilateral exploration have been similar.
IoPTH is useful to confirm the removal of pathological parathyroids in this group of patients [1]. In our experience, sensitivity and negative predictive value were slightly lower in group A (86% vs 97 and 67% vs 79% respectively), while specificity and positive predictive value were 100% in both the groups, confirming the high reliability of the technique.
Our study is limited by the small number of patients and the retrospective nature of the study. Further multicenter studies with a large number of patients could give more precise indications regarding this pathology for the future.
Conclusions
PHP with normal PTH is rare but physicians should be aware of this possibility in patients with hypercalcemia. Patients with normal PTH levels are younger and more frequently symptomatic. IoPTH testing plays an important role in the operative management even in such patients.
Abbreviations
- IoPTH:
-
Intraoperative PTH
- iPTH:
-
Intact-parathyroid hormone
- PHP:
-
Primary hyperparathyroidism
- PTH:
-
Parathyroid hormone
- PTHrp:
-
Parathyroid-hormone-related peptide
- US:
-
Neck ultrasound
References
Alhefdhi A, Pinchot SN, Dacis R, Sippel RS, Chen H. The necessity and reliability of intraoperative parathyroid hormone (PTH) testing in patients with mild hyperparathyroidism and PTH levels in the normal range. World J Surg. 2011;35:2006–9.
Bhadada SK, Cardenas M, Bhansali A, Mittal BR, Behera A, Chanukya GV, et al. Very low or undetectable intact parathyroid hormone levels in patients with surgically verified parathyroid adenomas. Clin Endocrinol. 2008;69:382–5.
Glendenning P, Gutteridge DH, Retallack RW, Stuckey BG, Kermode DG, Kent GN. High prevalence of normal total calcium and intact PTH in 60 patients with proven primary hyperparathyroidism: a challenge to current diagnostic criteria. Aust NZ J Med. 1998;28:173–8.
Lafferty FW, Hamlin CR, Corrado KR, Arnold A, Shuck JM. Primary hyperparathyroidism with a low-Normal, atypical serum parathyroid hormone as shown by discordant immunoassay curves. J Clin Endocrinol Metab. 2006;91:3826–9.
Medas F, Erdas E, Longheu A, Gordini L, Pisano G, Nicolosi A, et al. Retrospective evaluation of the pre- and postoperative factors influencing the sensitivity of localization studies in primary hyperparathyroidism. Int J Surg. 2016;25:82–7.
Norman J, Goodman A, Politz D. Calcium, parathyroid hormone, and vitamin D in patients with primary hyperparathyroidism: normograms developed from 10,000 cases. Endocr Pract. 2011;17:384–94.
Panarese A, D'Andrea V, Pontone S, Favoriti P, Pironi D, Arcieri S, et al. Management of concomitant hyperparathyroidism and thyroid diseases in the elderly patients: a retrospective cohort study. Aging Clin Exp Res. 2017;29(Suppl 1):29–33.
Glendenning P, Pullan PT, Gulland D, Edis AJ. Surgically proven primary hyperparathyroidism with a suppressed intact parathyroid hormone. Med J Aust. 1996;165:197–8.
Gulcelik NE, Bozkurt F, Tezel GG, Kaynaroglu V, Erbas T. Normal parathyroid hormone levels in a diabetic patient with parathyroid adenoma. Endocr. 2009;35:147–50.
Gurrado A, Marzullo A, Lissidini G, Lippolis A, Rubini D, Lastilla G, et al. Susternal oxyphil parathyroid adenoma producing PTHrP with hypercalcemia and normal PTH level. World J Surg Oncol. 2008;6:24.
Minisola S, Cipriani C, Diacinti D, Tartaglia F, Scillitani A, Pepe J, et al. Imaging of the parathyroid glands in primary hyperparathyroidism. Eur J Endocrinol. 2016;174:D1–8.
Bergenfelz A, Lindblom P, Lindergård B, Valdemarsson S, Westerdahl J. Preoperative Normal level of parathyroid hormone signifies an early and mild form of primary hyperparathyroidism. World J Surg. 2003;27:481–5.
Mischis-Troussard C, Goudet P, Verges B, Cougard P, Tavernier C, Maillefert JF. Primary hyperparathyroidism with normal serum intact parathyroid hormone levels. Q J Med. 2000;93:365–7.
Wallace LB, Parikh RT, Ross LV, Mazzaglia PJ, Foley C, Shin JJ, et al. The phenotype of primary hyperparathyroidism with normal parathyroid hormone levels: how low can parathyroid hormone go? Surgery. 2011;150:1102–12.
Hollenberg AN, Arnold A. Hypercalcemia with low-Normal serum intact PTH: a novel presentation of primary hyperparathyroidism. Am J Med. 1991;91:547–8.
Perez JB, Pazianos AG. Unusual presentation of primary hyperparathyroidism with osteoporosis, hypercalcemia, and normal parathyroid hormone level. South Med J. 2001;94:339–41.
Benaderet AD, Burton AM, Clifton-Bligh R, Ashraf AP. Primary hyperparathyroidism with low intact PTH levels in a 14-year-old girl. J Clin Endocrinol Metab. 2011;96:2325–9.
Amin AL, Wang TS, Wade TJ, Yen TW. Normal PTH levels in primary hyperparathyroidism: still the same disease? Ann Surg Oncol. 2011;18:3437–42.
Calò PG, Medas F, Loi G, Erdas E, Pisano G, Nicolosi A. Feasibility of unilateral parathyroidectomy in patients with primary hyperparathyroidism and negative or discordant localization studies. Updat Surg. 2016;68:155–61.
Calò PG, Pisano G, Loi G, Medas F, Tatti A, Piras S, et al. Surgery for primary hyperparathyroidism in patients with preoperatively negative sestamibi scan and discordant imaging studies: the usefulness of intraoperative parathyroid hormone monitoring. Clin Med Insights Endocrinol Diabetes. 2013;6:63–7.
Calò PG, Pisano G, Loi G, Medas F, Barca L, Atzeni M, et al. Intraoperative parathyroid hormone assay during focused parathyroidectomy: the importance of 20 minutes measurement. BMC Surg. 2013;13:36.
Calò PG, Pisano G, Tatti A, Medas F, Boi F, Mariotti S, et al. Intraoperative parathyroid hormone assay during focused parathyroidectomy for primary hyperparathyroidism: is it really mandatory? Minerva Chir. 2012;67:337–42.
Ljunghall S, Larsson K, Lindh E, Lindqvist U, Rastad J, Akerström G, et al. Disturbance of basal and stimulated serum levels of intact parathyroid hormone in primary hyperparathyroidism. Surgery. 1991;110:47–53.
Rosario PW. Primary hyperparathyroidism with Normal calcium and PTH. World J Surg. 2017;41:1649–50.
Au AY, McDonald K, Gill A, Sywak M, Diamond T, Conigrave AD, et al. PTH mutation with primary hyperparathyroidism and undetectable intact PTH. N Engl J Med. 2008;359:1184–6.
Boi F, Lombardo C, Cocco MC, Piga M, Serra A, Lai ML, et al. Thyroid diseases cause mismatch between MIBI scan and neck ultrasound in the diagnosis of hyperfunctioning parathyroids: usefulness of FNA-PTH assay. Eur J Endocrinol. 2012;168:49–58.
Calò PG, Tatti A, Medas F, Piga G, Farris S, Pisano G, et al. New techniques in parathyroid surgery. G Chir. 2010;31:322–4.
Gioviale MC, Gambino G, Maione C, et al. Use of monitoring intraoperative parathyroid hormone during parathyroidectomy in patients on waiting list for renal transplantation. Transplant Proc. 2007;39:1775–8.
Acknowledgements
Not Applicable.
Funding
The publication costs will be funded by the research funds of the University of Cagliari.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. The datasets used and/or analysed during the current study are available from the Unit of General and Endocrine Surgery AOU Cagliari, Policlinico D. Casula, Monserrato Cagliari, on reasonable request.
About this supplement
This article has been published as part of BMC Surgery Volume 18 Supplement 1, 2018: Updates and New Technology in Endocrine Surgery. The full contents of the supplement are available online at https://bmcsurg.biomedcentral.com/articles/supplements/volume-18-supplement-1.
Author information
Authors and Affiliations
Contributions
All authors contributed significantly to the present research and reviewed the entire manuscript. FM: Participated substantially in conception, design and execution of the study and in the analysis and interpretation of the data; also participated substantially in the drafting and editing of the manuscript. EE: Participated substantially in conception, design and execution of the study and in the analysis and interpretation of the data. GL: Participated substantially in conception, design and execution of the study and in the analysis and interpretation of the data. FP: Participated substantially in conception, design and execution of the study and in the analysis and interpretation of the data. LB: Participated substantially in conception, design and execution of the study and in the analysis and interpretation of the data. GP: Participated substantially in conception, design and execution of the study and in the analysis and interpretation of the data. PGC: Participated substantially in conception, design and execution of the study and in the analysis and interpretation of the data; also participated substantially in the drafting and editing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the AOU Cagliari ethics committee. All patients gave informed consent.
Consent for publication
All patients gave a written consent to publish their data.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Medas, F., Erdas, E., Loi, G. et al. Intraoperative parathyroid hormone (PTH) testing in patients with primary hyperparathyroidism and PTH levels in the normal range. BMC Surg 18 (Suppl 1), 124 (2019). https://doi.org/10.1186/s12893-018-0459-3
Published:
DOI: https://doi.org/10.1186/s12893-018-0459-3