Abstract
Background
Pancreatic fistula (PF) remains the most challenging complication after pancreaticoduodenectomy (PD). The purpose of this study was to identify the risk factors of PF and delineate its impact on patient outcomes.
Methods
We retrospectively reviewed clinical data of 532 patients who underwent PD and divided them into PF group and no PF group. Risk factors and outcomes of PF following PD were examined.
Results
PF was found in 65 (12.2%) cases, of whom 11 were classified into ISGPF grade A, 42 grade B, and 12 grade C. Clinically serious postoperative complications in the PF versus no PF group were mortality, abdominal bleeding, bile leak, intra-abdominal abscess and pneumonia. Univariate and multivariate analysis showed that blood loss ≥ 500 ml, pancreatic duct diameter ≤ 3 mm and pancreaticojejunostomy type were independent risk factors of PF after PD.
Conclusions
Blood loss ≥ 500 ml, pancreatic duct diameter ≤ 3 mm and pancreatico-jejunostomy type were independent risk factors of PF after PD. PF was related with higher mortality rate, longer hospital stay, and other complications.
Similar content being viewed by others
Background
Pancreaticoduodenectomy (PD) is the classic surgical approach for both malignant and benign disease of pancreatic head, duodenum and periampullary region. PD was associated with high mortality and morbidity since introduced as a treatment approach. Recently, both the mortality and morbidity following PD were significantly reduced for the improvement of surgical skills and perioperative care. The mortality rate after PD was kept even as low as 5% in many specialized centers [1-4]. Although the mortality following PD has decreased, the morbidity rate remains at a high level [1,4,5], with pancreatic fistula (PF) as the most challenging complication. Risk factors for PF after PD described in the literature included patient demographics, diameter of pancreatic duct, pancreatic texture and anastomotic technique [5-8]. Generally, PF is correlated with other major complications such as intraperitoneal bleeding, abdominal abscess, delayed gastric emptying and wound infection, all of which prolong the hospital stays and increase health-care costs [6-8].
To identify patients at high risk for PF and avoid the accompanying complications, it is important to predict its occurrence so that prompt treatment can be administered. The purpose of this study was to analyze the risk factors and outcomes of PF from a prospective database of 532 patients undergoing PD.
Methods
Five hundred thirty-two patients undergoing elective PD in the first Affiliated Hospital of Sun Yat-sen University between April 2000 and November 2011 were included in this study. Clinical data including demographics, intraoperative procedures and postoperative complications were reviewed. Prior approval from the committee for Ethical Review of research involving Human Subject of the first Affiliated Hospital of Sun Yat-sen University (Guangzhou, China) and informed consent from patients were obtained before study. One hundred and forty-one patients (26.5%, 141/532) accepted preoperative biliary drainage.
All patients were divided into 2 groups, according to the presence of PF or not: PF group and no PF group. PF, delayed gastric emptying (DGE), and post-pancreatectomy hemorrhage (PPH) were defined according to the International Study Group on Pancreatic Fistula (ISGF) [9-11]. Bile leak was diagnosed based on the following criteria: (1) bile fluid in the peritoneal drainage or oozing from the wound; or (2) radiographically proven fluid collection requiring percutaneous drainage and demonstrating elevated bilirubin levels [12,13]. The operative mortality was defined as death within 30 days after operation or before discharge from the hospital (irrespective of the duration of stay). Other morbidities were defined as any of the following: intraabdominal abscess (IAA) (drainage from an intraoperatively placed drain with positive cultures requiring the placement of a new percutaneous drain or operative intervention); pneumonia (fever, leukocytosis, culture-positive sputum with polymorphonuclear leukocytes on Gram stain, and chest radiograph demonstrating focal infiltrates); wound infection (purulent drainage from the postoperative wound, requiring opening and packing of the wound), deep venous thrombosis (characteristic venous obstruction, demonstrated on Doppler ultrasound), chyle leak (milky drainage from the peritoneal drain) [13]. Postoperative complications were graded according to Clavien-Dindo classification [5].
Surgical technique
Of the 532 patients, 7 cases had a pylorus-preserving pancreaticoduodenectomy (PPPD) and the others had a classical pancreaticoduodenectomy (PD). The pancreaticojejunostomy was performed using a traditional 2-layer anastomosis (n = 304), an invaginated anastomosis (n = 125), and a duct-mucous anastamosis (n = 103) based on surgeon’s preference. No pancreaticogastrostomy was used in our study. Four hundred and seventeen anastomoses (78.4%) were constructed using pancreatic duct stents. The biliary stent was not routinely placed. Drains were placed routinely in the Winslow’s foramen for draining peritoneal fluid in all patients. Prophylactic octreotide or somatostatin was not routinely used.
Statistical analysis
All statistical analyses were performed with SPSS version 21.0 software (IBM, USA). Quantitative data are expressed as mean ± SD. Independent sample Student’s t test was used to compare continuous variables. The Chi-square test or Fisher exact test was used to compare categorical variables. Of all the variables tested in univariate analysis, only those with P < .05 were put into multivariate analysis. Logistic regression (forward selection) was performed to determine the independent risk factors of PF. P < .05 was considered statistically significant.
Results
Incidence of pancreatic fistula
The indications for PD included duodenal neoplasm, pancreatic cancer, bile duct neoplasm, ampullary neoplasm, chronic pancreatitis, gastric antrum cancer, cystadenoma, pancreatic cyst, and so on. Three major indications for PD were duodenal neoplasm in 164 patients (30.8%), pancreatic cancer in 140 patients (26.3%) and ampullary neoplasm in 102 patients (19.2%). Sixty-five patients (12.2%) developed PF after PD, A grade 11 cases (16.9%, 11/65), B grade 42 cases (64.6%, 42/65) and C grade 12 cases (18.5%, 12/65).
Risk factors of pancreatic fistula
Fourteen clinical factors of PF were compared between the PF group and the no PF group by univariate analysis. We found that blood loss ≥ 500 ml, pancreatic duct diameter ≤ 3 mm and pancreaticojejunostomy type had statistical significance. Multivariate logistic regression analysis was used to identify the independent risk factors of PF. We identified that blood loss ≥ 500 ml (hazard ratio [HR] = 2.281; 95% confidence interval [CI] 1.334-3.901; P = .003), pancreatic duct diameter ≤ 3 mm (HR = 0.351; 95%CI, 0.192-0.641; P = .001) and pancreaticojejunostomy type (HR = 1.355; 95%CI, 1.007-1.823; P = .045) were independent risk factors for PF after PD (Table 1).
Postoperative outcomes
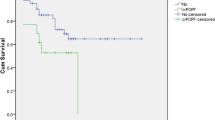
A total of 303 (57.0%, 303/532) patients didn’t develop any complication, while 229 (43.0%, 229/532) patients had at least one complication: 60 (11.3%, 60/532) patients had grade Icomplications, 50 (9.4%, 50/532) patients had grade II complications, 93 (17.5%, 93/532) patients had grade III complications, 3 (0.6%, 3/532)patients had grade IV complications. Grade V (death) occurred in 23 patients (4.3%, 23/532). Besides PF, other postoperative complications included PPH (60/532, 11.3%), bile leak (17/532, 3.2%), delayed gastric emptying (18/532, 3.4%), intraabdominal abscess (IAA) (97/532, 18.2%), pneumonia (27/532, 5.1%), wound infection (88/532, 16.5%), deep venous thrombosis (DVT) (1/532, 0.2%) and chyle leak (2/532, 0.4%). Mortality, IAB, bile leak, IAA and pneumonia were significantly higher in the PF group when compared with the no PF group. The length of hospital stay significantly increased in those patients who developed PF compared with those that did not (Table 2).
Discussion
PF is the most challenging complication after PD. Because it was associated with substantial mortality and morbidity, some authors even defined it as an “Achilles heel” of PD [6]. Our results demonstrate that the incidence of PF after PD was about 12.0%, which appears to be comparable to the PF rate of 9–14% reported in other specialized centers [14-17].
The formation of PF is associated with many variables involving demographic, preoperative, intraoperative and pathological factors. Previous studies had reported that pancreaticogastrostomy was associated with significantly lower pancreatic fistula rate than pancreaticojejunostomy. Pancreaticogastrostomy was more efficient than pancreatico-jejunostomy in reducing the incidence of postoperative pancreatic fistula [18-23]. In our institution, we have not performed pancreaticogastrostomy after PD so far. There is still a controversy in the relationship between preoperative biliary drainage and the incidence of PF. A study from Hopkins suggested that preoperative stent was associated with high incidence of postoperative pancreatic fistula [24]. Schmidt et al. also showed that those patients who had preoperative percutaneous transhepatic biliary (PTB) stent showed an increased risk of PF formation [6]. However, Aranha et al. found that no difference in the incidence of PF versus no-PF in those patients having ERCP or PTC and an increase in PF in those patients who did not have preoperative stents compared with those patients who did [8]. Lin et al. indicated that no difference in the incidence of PF versus no-PF in those patients having preoperative stent (either endoscopic or PBD) [14]. Our results also showed that there was no relationship between preoperative biliary drainage and postoperative PF.
As expected, increased intraoperative blood loss appeared to be an important risk factor of PF. Yeh et al. demonstrated increased intraoperative blood loss was an independent risk factor for PF after PD by univariate and multivariate analysis [25]. The factors which might increase blood loss during operation included a more advanced stage of the disease such as portal vein invasion or superior mesenteric vein, adhesions due to prior operations, jaundice-associated coagulopathy, obesity, and concurrent pancreatitis [25]. In our study, Intraoperative blood loss exceeding 500 ml occurred in 39.7% (211 of 532 patients) of patients, and of those, 17.5% patients (37/211) developed PF, which was significantly higher than patients with blood loss less than 500 ml (28/321, 8.7%). Again, our results showed blood loss ≥ 500 ml (hazard ratio [HR] = 2.281; 95% confidence interval [CI] 1.334-3.901; P = .003) was an independent risk factor for PF after PD. Kawai et al. showed that the preoperative CT image-assessed ligation of inferior pancreaticoduodenal artery (IPDA) method (CLIP) was a useful and reliable operative technique for reducing intraoperative bleeding in PD [26]. Ishizaki et al. reported early ligation of the inferior pancreatoduodenal artery (IPDA) not only reduced intraoperative blood loss during PD but also alleviated postoperative morbidity and mortality [27]. Therefore, IPDA method was suggested to decrease intraoperative bleeding.
Type of pancreaticojejunostomy anastomosis has also been cited as a predictor of PF after PD. Berger et al. reported considerably fewer fistulas with invagination compared with duct to mucosapancreaticojejunostomy after pancreaticoduodenectomy by a randomized, prospective, dual-institution trial [28]. However, Schmidt et al. and Bartoli et al. reported that lowest incidence of PF in patients who had a duct to mucous anastomosis than other anastomoses [6,29]. We also found that the lowest incidence of PF in patients who had a duct to mucous anastomosis (4.9%) versus a traditional 2-layers pancreaticojejunostomy (10.9%) or an invaginated pancreaticojejunostomy (21.6%) (P < .001). Since the diameter of major pancreatic duct played an important role in selection of PJ types, some studies have concluded that major pancreatic duct diameter was also an independent risk factor of PF after PD [4,23]. Generally, the narrowed pancreatic duct diameter is not only more challenging to reconstruct, but also more likely to either occlude or dehisce. In our study, we found that PF in patients who had pancreatic duct diameter > 3 mm (6.4%) was significantly lower than those who had pancreatic duct diameter ≤ 3 mm (17.3%) (P < .001). Soft pancreatic tissue has been regarded as a potent contributor for PF formation [4,7,14], while it had no effect on PF in our study. Based on our results and literatures, we think we should try to adopt duct to mucous anastomosis when the pancreatic duct diameter > 3 mm. If the pancreatic duct diameter measured 3 mm or less, we can expand the pancreatic duct by placing a fine stay suture in the middle of the anterior wall of the pancreatic duct as described by Hatori [30] and performed pancreaticojejunostomy with duct-to-mucosa anastomosis without a stent tube [31].
PF is associated with a greater many of other complications and prolonged hospital stay [6,8,14,28]. In our study, it was found to be associated with mortality, abdominal bleeding, bile leakage, intraabdominal abscess, pneumonia, reoperations and long hospital stay. Other complications including gastrointestinal bleeding, delayed gastric emptying, wound infection, deep venous thrombosis (DVT) and chyle leak were not significant when the PF group was compared with the no PF group.
Conclusions
In conclusion, blood loss and the pancreatic duct diameter and pancreaticojejunostomy type were independent risk factors for PF after PD. Outcomes in patients with PF were remarkable for a higher rate of mortality, abdominal bleeding and septic complications, an increased incidence of reoperations, and a longer hospital stay.
Abbreviations
- PF:
-
Pancreatic fistula
- PD:
-
Pancreaticoduodenectomy
- DEG:
-
Delayed gastric emptying
- PPH:
-
Post-pancreatectomy hemorrhage
- ISGF:
-
International study group on pancreatic fistula
- IAA:
-
Intraabdominal abscess
- PPPD:
-
Pylorus-preserving pancreaticoduodenectomy
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- DVT:
-
Deep venous thrombosis
- PTB:
-
Percutaneous transhepatic biliary
- IPDA:
-
Inferior pancreaticoduodenal artery
References
Winter JM, Cameron JL, Campbell KA, Arnold MA, Chang DC, Coleman J, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastro-intest Surg. 2006;10:1199–210.
Bottger TC, Junginger T. Factors influencing morbidity and mortality after pancreatico-duodenectomy: critical analysis of 221 resections. World J Surg. 1999;23:164–71.
Schmidt CM, Powell ES, Yiannoutsos CT, Howard TJ, Wiebke EA, Wiesenauer CA, et al. Pancreatico-duodenectomy; a 20-year experience in 516 patients. Arch Surg. 2004;139:718–25. discussion 725–727.
Braga M, Capretti G, Prcorelli N, Balzano G, Doglioni C, Ariotti R, et al. A prognostic score to predict major complications after pancreaticoduodenectomy. Ann Surg. 2011;254:702–7.
DeOliveira ML, Winter JM, Schafer M, Cunningham SC, Cameron JL, Yeo CJ, et al. Assessment of complications after pancreatic surgery: a novel grading system applied to 633 patients undergoing pancreatico-duodenectomy. Ann Surg. 2006;244:931–7.
Schmidt CM, Choi J, Powell ES, Yiannoutsos CT, Zyromski NJ, Nakeeb A, et al. Pancreatic fistula following pancreatico-duodenectomy: clinical predictors and patient outcomes. HPB Surg. 2009; doi: 10.1155 /2009/404520.
Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer Jr CM. A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg. 2013;216:1–14.
Aranha GV, Aaron JM, Shoup M, Pickleman J. Current management of pancreatic fistula after pancreaticoduodenectomy. Surgery. 2006;140:561–8.
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. International Study Group on Pancreatic Fistula Definition: Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8–13.
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DEG) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761–8.
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142:20–5.
Li SQ, Liang LJ, Peng BG, Lu MD, Lai JM, Li DM. Bile leakage after hepatectomy for hepatolithiasis: risk factors and management. Surgery. 2007;141:340–5.
Balcom IV JH, Rattner DW, Warshaw AL, Chang Y, Fernandez-del Castillo C. Ten year experience with 733 pancreatic resection: changing indications, older patients, and decreasing length of hospitalization. Arch Surg. 2001;136:391–8.
Lin JW, Cameron JL, Yeo SJ, Riall TS, Lillemoe KD. Risk factors and outcomes in postpancreatico-duodenectomy pancreaticocutaneous fistula. J Gastrointst Surg. 2004;8:951–9.
Kazanjian KK, Hines OJ, Eibl G, Reber HA. Management of pancreatic fistulas after pancreaticoduodenectomy: results in 437 consecutive patients. Arch Surg. 2005;140:849–55.
Kirihara Y, TakahaShi N, Hashimoto Y, Sclabas GM, Khan S, Moriya T, et al. Prediction of pancreatic anastomotic failure after pancreatoduodenectomy: the use of preoperative, quantitative computed tomography to measure remnant pancreatic volume and body composition. Ann Surg. 2013;257:512–9.
Relles DM, Richards NG, Bloom JP, Kennedy EP, Sauter PK, Leiby BE, et al. Serum blood urea nitrogen and serum albumin on the first postoperative day predict pancreatic fistula and major complications after pancreatico-duodenectomy. J Gastrointest Surg. 2013;17:326–31.
Arnaud JP, Tuech JJ, Cervi C, Bergamaschi R. Pancreaticogastrostomy compared with pancreaticojejunostomy after pancreaticoduodenectomy. Eur J Surg. 1999;165:357–62.
Ihse I, Axelson J, Hansson L. Pancreaticogastrostomy after subtotal pancreatectomy for cancer. Dig Surg. 1999;16:389–92.
Takano S, Ito Y, Watanabe Y, Yokoyama T, Kubota N, Iwai S. Pancreaticojejunostomy versus pancreatico-gastrostomy in reconstruction following pancreaticoduodenectomy. Br J Surg. 2000;87:423–7.
Peng SY, Wang JW, Hong De F, Liu YB, Wang YF. Binding pancreaticoenteric anastomosis: from binding pancreaticojejunostomy to binding pancreaticogastrostomy. Upstate Surg. 2011;63:69–74.
Shen YF, Jin WY. Reconstruction by Pancreaticogastrostomy versus Pancreatico-jejunostomy following Pancreaticoduodenectomy: a meta-analysis of randomized controlled trials. Gastroenterol Res and Pract. 2011. doi:10.1155/2012 /627095.
Topal B, Fieuws S, Aerts R, Weerts J, Feryn T, Roeyen G, et al. Belgian Section of Hepatobiliary and PancreaticSurgery: Pancreaticojejunostomy versus pancreaticogastrostomy reconstruction after pancreatico-duodenectomy for pancreatic or periampullary tumours: a multicentre randomised trial. Lancet Oncol. 2013;14:655–62.
Sohn TA, Yeo CJ, Cameron JL, Pitt HA, Lillemoe KD. Do preoperative biliary stents increase postpancreaticoduodenectomy complications? J Gastrointest Surg. 2000;4:258–68.
Yeh TS, Jan YY, Jeng LB, Hwang TL, Wang CS, Chao TC, et al. Pancreaticojejunal anatomotic leak after pancreatico-duodenectomy– multivariate analysis of perioperative risk factors. J Surg Res. 1997;67:119–25.
Kawai M, Tani M, Ina S, Hirono S, Nishioka R, Miyazawa M, et al. CLIP method (preoperative CT image-assessed ligation of inferior pancreaticoduodenal artery) reduces intraoperative bleeding during pancreaticoduodenectomy. World J Surg. 2008;32:82–7.
Ishizaki Y, Sugo H, Yoshimoto J, Imamura H, Kawasaki S. Pancreaticoduodenectomy with or without early ligation of the inferior pancreatoduodenal artery: comparison of intraoperative blood loss and short outcome. World J Surg. 2010;34:2939–44.
Berger AC, Howard TJ, Kennedy EP, Sauter PK, Bower-Cherry M, Dutkevitch S, et al. Does type of pancreaticojejunostomy after pancreaticoduodenectomy decrease rate of pancreatic fistula? A randomized, proepective, dudal-institution trial. J Am Coll Surg. 2009;208:738–47. discussion 747–749.
Bartoli FG, Arnone GB, Ravera G, Bachi V. Pancreatic fistula and relative mortality in malignant disease after pancreaticoduodenectomy. Review and statistical meta-analysis regarding 15 years of literature. Anticancer Res. 1991;11:1831–48.
Hatori T. Pancreaticojejunostomy without stent (with video). J Hepatobiliary Pancreat Sci. 2012;19:125–30.
Imaizumi T, Hatori T, Tobita K, Fukuda A, Takasaki K, Makuuchi H. Pancreatico-jejunostomy using duct-to-mucosa anastomosis without a stenting tube. J Hepatobiliary Pancreat Sci. 2006;13:194–201.
Acknowledgements
We thank Professor Stephen Tomlinson from the Department of Microbiology and Immunology, Medical University of South Carolina, for review and correction of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SJF, SLS and BGP were the main authors of the manuscript. They were involved in the conception, design and coordination of the study as well as in data analysis, interpretation of results and drafting the manuscript. BGP was in charge of all experimental procedures. SQL, WJH, YPH, MK and LJL participated in the experimental procedures and revised critically the content of the manuscript. All authors contributed to the interpretation of data and critically revised the manuscript. All authors read and approved the final manuscript.
Shun-Jun Fu and Shun-Li Shen contributed equally to this work.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Fu, SJ., Shen, SL., Li, SQ. et al. Risk factors and outcomes of postoperative pancreatic fistula after pancreatico-duodenectomy: an audit of 532 consecutive cases. BMC Surg 15, 34 (2015). https://doi.org/10.1186/s12893-015-0011-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-015-0011-7