Abstract
Background
Tension band wiring (TBW) is a common surgical intervention for olecranon fractures. However, high rate of complications such as loss of reduction, skin irritation, and migration of the K-wires were reported up to 80%. Ding’s screw tension band wiring (DSTBW) is a new TBW technique that has shown positive results in the treatment of other fracture types. The objective of this study was to evaluate the stability of DSTBW in the treatment of olecranon fractures by finite element analysis.
Method
We used Ding’s screw tension band fixation (DSTBW) and K-wire tension band fixation (TBW) to establish a finite element model to simulate and fix olecranon fractures. The stress distribution, opening angle, twisting angle, and pullout strength of K-wires or screws were analyzed and compared.
Results
The maximum von Mises stress was observed on the internal fixation for 90° elbow motion in both groups. The von Mises value of the screw in DSTBW was 241.2 MPa, and the von Mises value of k-wire in TBW was 405.0 MPa. Opening angle: TBW was 0.730° and DSTBW was 0.741° at 45° flexion; TBW was 0.679° and DSTBW was 0.693° at 90° flexion. Twisting angle: TBW was 0.146° and DSTBW was 0.180° at 45° flexion; TBW was 0.111° and DSTBW was 0.134° at 90° flexion. The pullout strength of DSTBW was significantly higher than that of TBW. Maximum pullout strength of Ding’s screw was 2179.1 N, maximum pullout strength of K-wire was 263.6 N.
Conclusion
DSTBW technology provides stable fixation for olecranon fractures, reducing the risk of internal fixation migration and failure.
Similar content being viewed by others
Background
Olecranon fractures are relatively common fractures, accounting for about 10% of adult upper limb fractures, and are more frequent in young patients after high-energy trauma or the elderly after low-energy fall [1]. Olecranon fractures are usually associated with the articular surface and require surgical treatment [2]. The goals of surgical treatment are to reduce the fracture and restore joint stability, allowing for early functional exercise. There are a series of surgical interventions for olecranon fractures, including tension band wiring (TBW) [3], plate fixation [4], and intramedullary screws (IM) [5]. TBW is a simple, low-cost technique that relies on the principle of converting posterior tension into joint compression force and is the most widely used technique for displaced, non-comminuted olecranon fractures [6,7,8].
However, the incidence of complications associated with TBW is high (up to 80%), such as loss of reduction, olecranon bursitis, Kirschner wire (K-wire) migration, and skin irritation are often reported [9,10,11]. The subcutaneous nature and potential displacement of K-wires may be the cause of local pain and discomfort in patients. However, removing metalware does not always solve these symptoms. More than 65% of patients still experienced mild pain or discomfort after the metalware was removed after TBW [6]. In long term, whether the metalware is removed or not, the low level of pain is noticeable and degenerative changes have been developed [6].
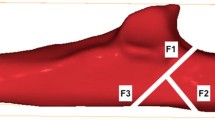
DSTBW is a new TBW technique that has shown positive results in the treatment of inferior pole patellar fractures [12]. The using of DSTBW technology(Fig. 1)in olecranon fractures may overcome these problems caused by K-wires in conventional TBW. In theory, the steel wires pass through the holes at the end of the Ding’ s screw, creating a solid " integrated structure” that makes the screws difficult to migrate. At the same time, the end of the screw is much smaller than the end of the curved K-wire, which can effectively reduce skin irritation symptoms. The objective of this study was to evaluate the effect of DSTBW on olecranon fracture by finite element analysis.
Methods
Finite element Biomechanical Study
Collection of imaging data
Radiologic images of a normal olecranon from a 28-year-old male were obtained from 0.5-mm width cuts of 64-slice computed tomography scans to observe bone tissue. The scanning conditions were as follows: 155 mA at 120 kV. The scanned CT data was saved in 512 × 512 pixels DICOM format.
Finite element model of proximal ulna construction
Radiological images in DICOM format were imported into Mimics 17 (Materialise, Belgium) to develop a 3D(three-dimensional) model of proximal ulna. Threshold segmentation, region growth, and calculation of the 3D model were performed in Mimics 17 software, and physicochemical processing was performed in software Imageware 13.0 (Siemens, Plano, TX) and Geomagic 2012 (Cary, NC) to build the olecranon model.
The Mayo type IIA type olecranon fracture line [10] was created and two different surgical procedures were performed for the fixation of the fracture by ProE 5.0 software (PTC Inc., Boston, MA). In the TBW group, the fracture was fixed by 2 bicortically placed K-wires. A 2.0-mm hole was made perpendicular to the ulnar shaft, an 18-gauge metal wire was then used to make a figure-of-eight wiring between the hole and the K-wires (Fig. 2a). In the DSTBW group, the fracture was fixed by two Ding’s screws (Double Medical Technology Inc, Xiamen, Fujian, China) which inserted from the tip of the olecranon through the proximal ulna, passing as close as possible to the subchondral bone. A 2.0-mm hole was made perpendicular to the ulnar shaft. Two 18-gauge metal wire were passed through the holes on the tail end of Ding’s screws separately and used to make the figure-of-eight wiring between the hole and Ding’s screws (Fig. 2b).
Volume mesh generation
The model of the established combined with the internal fixation system was output using step format and imported into the ANSYS Workbench 2020R2 software (ANSYS, Inc., Pittsburgh, PA, USA). The FE meshes were generated as a tetrahedral 1.6 mm for olecranon and 0.3 mm for K-wire, screw and tension band. The average mesh quality was 0.82. The Ding’s screw was modeled as 4 mm thick and 50 mm long. The K-wire was modeled as 2 mm thick, and the steel wire was 1.25 mm thick. In this study, there were 127,808 elements with 285,000 nodes in TBW model after meshing, and 135,642 elements with 302,470 nodes in DSTBW model.
Assignment of material properties
According to previous literatures [13,14,15], the material parameters were set (Table 1). The Poisson’s ratio was set to 0.3 for cortical bone and cancellous bone, and the elastic modulus were set to 18 GPa and 5 GPa respectively. The Ding’s screw and K-wires were modeled as titanium alloy Ti6Al4V. The material constants were as follows: the elastic modulus 106 Gpa and Poisson’s ratio 0.33. In the case of the steel wire, the elastic modulus and Poisson ratio were set to 210 GPa and 0.3, respectively.We change the “Tolerance Type” under the connections option in the software to “Value” and set the “Tolerance Value” to 0.05. The connection was automatically created by the software. According to previous literatures [16, 17], the contact definition was set: The relationship between cortical bone and cancellous bone was set as Bonded, the bone pieces at both ends of the fracture line were set as Rough, and the other relationships were set as No Separation.
Loading and boundary conditions
A mesh was generated with an element size from 4 mm to 0.3 mm (supplementary material 1) and a convergence analysis with 5% tolerance [18] was selected. The distal ulna point B (Fig. 3) was determined by ANSYS program, and the pulling direction of the triceps muscle to the proximal olecranon projection was simulated. A tensile force of 120 N for 90° and 200 N for 45° was applied according to previous literatures [13, 19].
After the mechanical loads were defined, the distribution of von Mises stress on fixation and the changes of opening and twisting angles in the fracture line were evaluated. Applying an axial displacement loading, record and draw the loading and displacement curves of K-wires or screws. The peak is considered as the maximum pullout strength.
Results
Finite element analysis: von mises stress distribution
There was no fixation failure in either fixation system. Compared with TBW, DSTBW has smaller von Mises stress distribution at different elbow movements (45° and 90°) (Table 2). The maximum von Mises stress in DSTBW was 212.0 MPa and 241.2 MPa at 45° and 90° elbow movements, respectively. The maximum von Mises stress at k-wire was 366.5 MPa and 405.0 MPa at 45° and 90° elbow movements, respectively (Figs. 4 and 5). The stress distribution of the internal fixation during 45° elbow movement in the TBW and DSTBW groups is shown in the supplementary materials 2.
Finite element analysis: opening and twisting angle
For TBW method; the opening angle was recorded 0.730°,0.679° at 45° and 90° elbow flexion position respectively (Fig. 5). For DSTBW method; the opening angle was recorded 0.741°, 0.693° at 45° and 90° elbow flexion position respectively.
For TBW group, the twisting angle was recorded 0.146°, 0.111° at 45° and 90° elbow flexion position respectively. For DSTBW group, the twisting angle was recorded 0.180°, 0.134° at 45° and 90° elbow flexion position respectively. The opening angle and twisting angle of TBW and DSTBW were similar in 45° and 90° elbow flexion position.
Finite element analysis: pullout strength
The pullout strength of DSTBW was significantly higher than that of TBW(P < 0.001). The average maximum pullout strength for the Ding’s screws was 2179.1 N. The average maximum pullout strength for the K-wires was 263.6 N (Fig. 6). The results indicated that the Ding’s screws increased stability and reduced the risk of migration of medical apparatus and instruments.
Discussion
TBW has been generally accepted as the standard treatment for Mayo type IIA olecranon fractures [3, 13]. Although this technique has shown excellent outcomes in both biomechanical and clinical studies [20,21,22,23], it has been reported that the incidence of complications and reoperation is very high [9,10,11]. Patient’s local pain and discomfort may be caused by the excessive tail of the curved K-wire and its potential migration. Therefore, improved techniques are used to improve the strength of fixation and reduce complications, such as cannulated screws. Cannulated screws have been reported for the treatment of olecranon fractures, including IM and IM-TBW [24]. However, previous studies have shown that fixation using IM screws is technically challenging and unreliable [25,26,27]. The IM-TBW technique provides better structural stability than fixation with the IM screw alone [28, 29]. Nevertheless, this technique requires the use of a large washer combined with steel wire to form tension bands, and the use of washers has a higher complication rate than using screws alone [30]. This may be the reason why this technique is rarely used by orthopedic surgeons. Edwards et al. [31] observed that IM-TBW technique was used in about 6% of cases in their multicenter study.
Therefore, in view of the shortcomings of the above fixations, the Ding’s screws have the following advantages: First, DSTBW is connected by steel wires through holes at the end of the Ding’s screw to form a strong “integral structure”, which effectively increases mechanical stability. At the same time, the end of the Ding’s screws is much smaller than the end of the curved k-wire and large washers, which can effectively avoid the k-wire migration and skin irritation symptoms. Second, compared with IM-TBW, there is no need to use large washers, which reduces complications caused by washers. Third, Ding’s screw has four holes at the end, which is designed to facilitate operation and simplify the procedure of steel wire passing through the holes at the end. When the steel wire is crossed, the remaining holes allow additional ultrabraid sutures to pass through, which is helpful to fix small fragments of fracture. If necessary, the ultrabraid sutures can also be sutured to the triceps tendon to further enhance the stability of internal fixation.
In this study, a finite element study was conducted on the stability of DSTBW in the treatment of olecranon fracture to provide a basis for its clinical application. The stress distribution of cortical bone, cancellous bone, K-wire, steel wire and Ding’s screws was tested after the model was constrained and loaded. The results of the finite element model show that the von Mises stress on DSTBW is smaller than that on TBW when the elbow joint is moving, indicating that DSTBW is less likely to be failed. Compared with TBW, the pullout strength of DSTBW is much higher after applying an axial load. When these findings are applied to clinical practice, it may be postulated that DSTBW will provide sufficient stability to reduce the risk of internal fixation migration and failure.
This study has some limitations. It is difficult to analysis the soft tissue structures in a finite element model, especially elbow is a complex joint with synovial fluid, multiple muscles and ligaments. The elbow joint is a hinge joint formed by the meeting of the humerus, radius and ulna. The biomechanical effects of humerus and radius were also ignored in this study. Further biomechanical experiments include all soft tissues, bony structures and the natural elbow movements are needed to verify the results.
Conclusion
In conclusion, the finite element analysis suggests that the DSTBW technique can provide stable fixation for olecranon fractures, reducing the risk of internal fixation migration and failure.
Data Availability
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Abbreviations
- 3D:
-
Three-dimensional
- K-wire:
-
Kirschner wire
- IM:
-
Intramedullary screw
- TBW:
-
Tension band wiring
- DSTBW:
-
Ding’s screw and tension band wiring
References
Wilkerson JA, Rosenwasser MP. Surgical techniques of olecranon fractures. J Hand Surg. 2014;39(8):1606–14.
Wiegand L, Bernstein J, Ahn J. Fractures in brief: Olecranon fractures. Clin Orthop Relat Res. 2012;470(12):3637–41.
Mu È ller, ME, Allgo È wer, Willengger W H, editors. Manual of Internal Fixation. Techniques Recommended by the AO-Group. New York: Springer, 1970.
Duckworth AD, Clement ND, White TO, Court-Brown CM, McQueen MM. Plate Versus Tension-Band Wire fixation for Olecranon Fractures: a prospective Randomized Trial. J Bone Joint Surg Am. 2017;99(15):1261–73.
Bosman WPF, Emmink BL, Bhashyam AR, Houwert RM, Keizer J. Intramedullary screw fixation for simple displaced olecranon fractures. Eur J Trauma Emerg Surg. 2020;46(1):83–9.
Chalidis BE, Sachinis NC, Samoladas EP, Dimitriou CG, Pournaras JD. Is tension band wiring technique the “gold standard” for the treatment of olecranon fractures? A long term functional outcome study. J Orthop Surg Res. 2008;3:9.
Horne JG, Tanzer TL. Olecranon fractures: a review of 100 cases. J Trauma. 1981;21(6):469–72.
Villanueva P, Osorio F, Commessatti M, Sanchez-Sotelo J. Tension-band wiring for olecranon fractures: analysis of risk factors for failure. J Shoulder Elbow Surg. 2006;15(3):351–6.
Mullett JH, Shannon F, Noel J, Lawlor G, Lee TC, O’Rourke SK. K-wire position in tension band wiring of the olecranon - a comparison of two techniques. Injury. 2000;31(6):427–31.
van der Linden SC, van Kampen A, Jaarsma RL. K-wire position in tension-band wiring technique affects stability of wires and long-term outcome in surgical treatment of olecranon fractures. J Shoulder Elbow Surg. 2012;21(3):405–11.
Macko D, Szabo M. Complications of tension-band wiring of olecranon fractures. J Bone Joint Surg. 1985;67(9):1396–401.
Du L, Yin N, Pan M, Xue F, Shen Y, Ding L. The effect of Ding’s screws and tension band wiring for treatment of inferior pole patellar fractures. Injury. 2023;54(4):1198–202.
Civan O, Ugur L, Yildiz G. Comparison of two surgical techniques for the treatment of transverse olecranon fractures: a finite element study. Int J Med Robot. 2021;17(4):e2265.
Kim Y, Kwon M, Ryu JY, Moon SW. Biomechanical analysis of the Kirschner-Wire depth of the modified tension Band Wiring technique in transverse patellar fractures: an experimental study using the finite-element Method. Clin Orthop Surg. 2021;13(3):315–9.
Zhang Y, Shao Q, Yang C, Ai C, Zhou D, Yu Y, Sun G. Finite element analysis of different locking plate fixation methods for the treatment of ulnar head fracture. J Orthop Surg Res. 2021;16(1):191.
Aziz MSR, Dessouki O, Samiezadeh S, Bougherara H, Schemitsch EH, Zdero R. Biomechanical analysis using FEA and experiments of a standard plate method versus three cable methods for fixing acetabular fractures with simultaneous. THA Med Eng Phys. 2017;46:71–8.
Meng D, Ouyang Y, Hou C. [A finite element analysis of petal-shaped poly-axial locking plate fixation in treatment of Y-shaped patellar fracture]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2017;31(12):1456–61.
Amaral CF, Gomes RS, Rodrigues Garcia RCM, Del Bel Cury AA. Stress distribution of single-implant-retained overdenture reinforced with a framework: a finite element analysis study. J Prosthet Dent. 2018;119(5):791–6.
Greenfield JRF, Lestriez P, Arand C, Gruszka D, Nowak T, Rommens PM, Taiar R. A numerical model of the tension band wiring technique for olecranon fracture reduction. Appl Math Comput. 2017;297:31–8.
Kim W, Choi S, Yoon JO, Park HY, Kim SH, Kim JS. Double tension band wiring for treatment of olecranon fractures. J Hand Surg Am. 2014;39(12):2438–43.
Midtgaard KS, Søreide E, Brattgjerd JE, Moatshe G, Madsen JE, Flugsrud GB. Biomechanical comparison of tension band wiring and plate fixation with locking screws in transverse olecranon fractures. J Shoulder Elbow Surg. 2020;29(6):1242–8.
Tan BYJ, Pereira MJ, Ng J, Kwek EBK. The ideal implant for Mayo 2A olecranon fractures? An economic evaluation. J Shoulder Elbow Surg. 2020;29(11):2347–52.
Ren YM, Qiao HY, Wei ZJ, Lin W, Fan BY, Liu J, Li A, Kang Y, Liu S, Hao Y, Zhou XH, Feng SQ. Efficacy and safety of tension band wiring versus plate fixation in olecranon fractures: a systematic review and meta-analysis. J Orthop Surg Res. 2016;11(1):137.
Labrum JT 4th, Foster BD, Weikert DR. Augmented intramedullary screw tension band construct for olecranon fracture reduction and fixation: a review of literature and surgical technique. JSES Int. 2020;4(3):470–7.
Wadsworth TG. Screw fixation of the olecranon. Lancet. 1976;2:1118–9.
Helm RH, Hornby R, Miller SW. The complications of surgical treatment of displaced fractures of the olecranon. Injury. 1987;18:48–50.
Ahmed AR, Sweed T, Wanas A. The role of cancellous screw with tension band fixation in the treatment of displaced olecranon fractures, a comparative study. Eur J Orthop Surg Traumatol. 2008;18:571–6.
Brink PR, Windolf M, de Boer P, Brianza S, Braunstein V, Schwieger K. Tension band wiring of the olecranon: is it really a dynamic principle of osteosynthesis? Injury. 2013;44(4):518–22.
Hutchinson DT, Horwitz DS, Ha G, Thomas CW. Bachus K.N. Cyclic loading of olecranon fracture fixation constructs. J Bone Joint Surg Am. 2003;85:831–7.
Pace GI, Hennrikus WL. Fixation of displaced medial epicondyle fractures in adolescents. J Pediatr Orthop. 2017;37(2):e80–2.
Edwards SG, Cohen MS, Lattanza LL, Iorio ML, Daniels C, Lodha S, Smucny M. Surgeon perceptions and patient outcomes regarding proximal ulna fixation: a multicenter experience. J Shoulder Elbow Surg. 2012;21(12):1637–43.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Liang Ding and Nuo Yin conceived and designed the study. Nuo Yin collected and analyzed the images. Mingmang Pan and Chenglei Li conducted the finite element models and simulation. Liang Ding and Li Du drafted the manuscript and critically revised the manuscript for intellectual content. Liang Ding inspected and approved the final version of the manuscript. All of the authors were involved in the manuscript preparation.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital South Campus.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yin, N., Pan, M., Li, C. et al. The effect of ding’s screw and tension band wiring for treatment of olecranon fractures: a finite element study. BMC Musculoskelet Disord 24, 603 (2023). https://doi.org/10.1186/s12891-023-06684-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06684-4