Abstract
Background
Recent studies have demonstrated that the distal forearm dual-energy X-ray absorptiometry (DEXA) scan might be a better method for screening bone mineral density (BMD) and the risk of a distal forearm fracture, compared with a central DEXA scan. Therefore, the purpose of this study was to determine the effectiveness of a distal forearm DEXA scan for predicting the occurrence of a distal radius fracture (DRF) in elderly females who were not initially diagnosed with osteoporosis after a central DEXA scan.
Methods
Among the female patients who visited our institutes and who were over 50 years old and underwent DEXA scans at 3 sites (lumbar spine, proximal femur, and distal forearm), 228 patients with DRF (group 1) and 228 propensity score-matched patients without fractures (group 2) were included in this study. The patients’ general characteristics, BMD, and T-scores were compared. The odds ratios (OR) of each measurement and correlation ratio among BMD values of the different sites were evaluated.
Results
The distal forearm T-score of the elderly females with DRF (group 1) was significantly lower than that of the control group (group 2) (p < 0.001 for the one-third radius and ultradistal radius measurements). BMD measured during the distal forearm DEXA scan was a better predictor of DRF risk than BMD measured during the central DEXA (OR = 2.33; p = 0.031 for the one-third radius, and OR = 3.98; p < 0.001 for the ultradistal radius). The distal one-third radius BMD was correlated with hip BMD, rather than lumbar BMD (p < 0.05 in each group).
Conclusion
Performing a distal forearm DEXA scan in addition to a central DEXA scan appears to be clinically significant for detecting the low BMD in the distal radius, which is associated with osteoporotic DRF in elderly females.
Level of evidence
III; case-control study.
Similar content being viewed by others
Introduction
As the global population ages, health systems are becoming strained with fragility fractures related to osteoporosis in older adults [1, 2]. Several studies have demonstrated the importance of an early diagnosis of osteoporosis to help prevent these fractures [1, 2]. Osteoporotic fragility fractures usually occur in the distal radius, proximal femur, spine, and proximal humerus, and are associated with socioeconomic costs exceeding $19 billion annually in the United States [1, 3]. Among these, the distal radius fracture (DRF) is the second most common accounting for 37% of overall osteoporotic fractures [4]. DRFs are known to occur approximately 15 years prior to the incidence of a hip fracture, so they have been considered to be a predictor of subsequent osteoporotic fractures [5,6,7,8]. A history of DRF in women increased the risk of hip fracture 1.4-fold and the risk of vertebral fracture 5.2-fold compared to women without prior DRF [9]. Therefore, earlier detection of a patient’s DRF risk may prevent further osteoporotic fractures.
Recent studies have demonstrated the necessity of measuring peripheral bone mineral density (BMD) of the distal forearm [10,11,12]. For this purpose, the distal forearm DEXA scan seems to be a better method for screening BMD and the risk of a distal forearm fracture, compared with a central DEXA scan [3, 10, 12]. The significant association between lower distal forearm BMD and the occurrence of a forearm fracture in the pediatric population has been previously reported [12]. In older adults, lower BMD of the distal forearm was related to an increased risk of osteoporotic fracture in the upper limbs, including the distal radius and proximal humerus. This risk was underestimated when a central DEXA scan was used alone [3, 10]. Additionally, several studies conducted on older adults with DRF showed that BMD measured using a central DEXA scan had no significant correlation with the occurrence of the fracture [13,14,15,16,17,18,19,20]. Moreover, for patients with DRF, there has been a lack of proper evaluation and management for osteoporosis compared with those of vertebral fractures or hip fractures [9, 21,22,23,24,25,26].
The use of a distal forearm DEXA scan is limited to specific circumstances according to the standard guidelines for the diagnosis of osteoporosis [11, 27]. While the current recommendations are to use the one-third radius of the non-dominant arm to diagnose osteoporosis, there have been some disagreements about the proper sites and methods for measuring distal forearm BMD [10, 11, 28].
Therefore, the purpose of this study was to evaluate the clinical necessity of a distal forearm DEXA scan for predicting DRF in elderly females who were not diagnosed with osteoporosis based on a central DEXA scan.
Materials and methods
Study design
We performed a retrospective case-control study using data collected from medical records and radiographic reports between May 2012 and May 2019. The study protocol was reviewed and approved by the institutional review board. All participants provided informed consent before data collection.
Female patients over 50 years of age who underwent DEXA scans (Lunar Prodigy Advance, GE Healthcare, Madison, WI) at 3 different sites (lumbar spine, proximal femur, and distal forearm) in our hospital were initially classified into two groups. The experimental group consisted of patients with low energy-induced DRF (group 1), and the control group consisted of patients with other injuries excluding fragility fractures (group 2). A detailed list of inclusion and exclusion criteria is described in Fig. 1.
Bone mineral density measurements
In this study, we focused on the areal BMD measured using a DEXA scan. For all patients, the central DEXA scan, including the lumbar spine, total hip, and femoral neck, was performed according to the standard guidelines outlined by the International Society for Clinical Densitometry [11, 29]. For spine BMD, the mean values of L2–L4 were used in this study after the exclusion of degenerative and sclerotic lesions and other bone abnormalities. Additionally, we performed a distal forearm DEXA scan at two different sites (ultradistal radius and one-third distal radius) for all patients (Fig. 2). Written informed consent for the additional peripheral DEXA scans were obtained from all study participants. Peripheral BMD was measured using the non-dominant wrist [11] unless the non-dominant wrist was a fracture site, then BMD was measured on the dominant side. This was based on a previous report demonstrating the similarity in BMD between the dominant and non-dominant forearms of healthy patients [30]. The T-score is defined as the number of standard deviations (SD) of a measured BMD value from the average BMD of the reference population (young adult females) [27]. For group 1, the DEXA scan was performed when the fractures were initially diagnosed and the BMD measurements were investigated for this study. For group 2, the BMD values measured when the patients first visited our hospital were used.
Dual-energy X-ray absorptiometry image of the left forearm. Two regions of interest (ultradistal radius and one-third radius) were included in this study. Radius UD = ultradistal radius, radius 33% = distal one-third radius. The image should include 2 cm of diaphysis over one-third of the forearm and a part of the carpal bones [29]
Patient characteristics and clinical evaluations
Patients’ characteristics include age, height, weight, body mass index (BMI), types of fracture according to the AO/OTA classification of a distal radius fracture, Charlson Comorbidity Index (CCI), and history of previous fractures. The Fracture Risk Assessment Tool (FRAX®) was used for assessing the FRAX score indicating the 10-year osteoporosis-related fracture risk [31].
Statistical analysis
SPSS version 23 (IBM Corporation, Armonk, NY, USA) was used for statistical analyses. Baseline data are reported as mean ± SD, frequencies, or percentages. Independent t-test and chi-squared test were used to compare patient characteristics and measurements between groups. Before the comparison, propensity score matching was performed to reduce bias and was calculated for each group based on a logistic regression model using age, height, weight, BMI, CCI, and the side on which they received the distal forearm DEXA scan [32].
We assessed the odds ratio (OR) of each BMD measurement and T-score for all the different sites, and the FRAX score associated with an occurrence of a distal radius fracture using the multivariate logistic regression analysis. In both groups, correlations between BMD measurements for different sites were evaluated using Pearson’s correlation test. The correlation coefficient was interpreted using the following scale: 0.00–0.19, very weak; 0.20–0.39, weak; 0.40–0.59, moderate; 0.60–0.79, strong; and 0.80–1.00, very strong. The paired t-test was also used to compare the mean T-score for different sites within each group.
To determine the appropriate number of patients required, we performed a power analysis during the initial study design. We observed that the mean difference in T-score was 0.12 ± 0.35 in our pilot study. The sample size for each group was calculated with 0.05 (two-sided) for α and 0.1 (power = 90%) for β. The analysis identified 186 as the minimum number of subjects required for each group.
Results
To form group 1, the medical records of 384 female patients with distal radius fractures were initially assessed, and 228 patients were selected to be part of the DRF group (group 1) (Fig. 1). To form group 2, among the 1062 patients initially assessed 726 patients were selected for the control group (group 2). A propensity score was calculated from age, height, weight, BMI, CCI, history of fractures, and the side on which the peripheral DEXA scan was performed (dominant or non-dominant arm). After propensity score matching, 228 patients from group 1 and 228 patients from group 2 were included in the study (Table 1).
A detailed comparison of each measurement between the two groups is described in Table 2.
T-scores for the one-third radius and ultradistal radius in group 1 were significantly lower than those in the control group (p < 0.001 and p < 0.001, respectively). BMD measurements for the one-third radius and ultradistal radius in group 1 were significantly lower (p = 0.043 and p = 0.041, respectively). Among the patients not initially diagnosed with osteoporosis by a central DEXA scan, the number of patients with a T-score measured at the distal forearm under − 2.5 was remarkably identified in both groups (16.7% of group 1 and 7.5% of group 2), which was also significantly higher in group 1 (p = 0.004).
We also assessed the risk factors of the distal radius fracture using a multivariate logistic regression analysis (Table 3). The T-scores calculated for the central DEXA scans did not suggest any correlation with the occurrence of DRF. FRAX score, which was calculated using proximal femur BMD, was not a significant predictor of the occurrence of DRF either. On the contrary, T-scores measured for the one-third distal radius and the ultradistal radius indicated significant risk for DRF (OR = 2.33; p = 0.031 and OR = 3.98; p < 0.001, respectively).
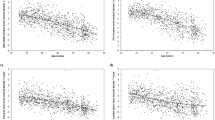
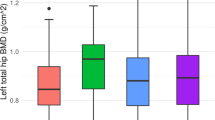
The comparisons of mean T-scores measured at each site are shown in Figs. 3 and 4. In group 1, the ultradistal radius T-score was significantly lower than the central and one-third radius DEXA scan T-scores (p < 0.05). The one-third radius T-score was also significantly lower than the central DEXA scan T-scores (p < 0.05 at each comparison). In group 2, the ultradistal radius T-scores were significantly lower than the central scan T-scores (p < 0.05 at each comparison), but were similar to those of the one-third radius. The one-third radius T-score was significantly lower than the lumbar T-score (p < 0.05), but was similar to that of the hip.
Correlation coefficients among the BMDs measured at each site are described in Table 4. In group 1, the BMD measured at the femoral neck and the total hip were statistically similar to each other (p < 0.001). Lumbar BMD was significantly correlated with BMD of the femoral neck, total hip, and one-third radius (p < 0.05 for each analysis). Ultradistal radius BMD measurements showed a significant correlation with the one-third radius BMD (p < 0.001). However, it showed no correlation with the other central BMD measurements. On the contrary, one-third radius BMD was significantly correlated with central BMD, which was more strongly correlated with the proximal femur BMD (p < 0.05 for lumbar spine BMD and p < 0.001 for both proximal femur BMDs). In group 2, proximal femur BMD showed a stronger correlation with the lumbar spine BMD (p < 0.001 for both correlations) than with those from group 1. And the one-third radius BMD showed moderate correlation with the proximal femur BMD and the ultradistal radius BMD, similar to that of the group 1(p < 0.001 for each correlation).
Discussion
There were three main findings in this study. The first is that the T-score of the distal forearm DEXA scan measurements for elderly females with a DRF was significantly lower than the control group. The second is that according to the T-scores, the distal forearm DEXA scan measurements were better predictors of the occurrence of DRF. Finally, the ultradistal radius T-score was the strongest and independent predictor of the DRF. And the distal one-third radius BMD was correlated more closely with the hip BMD than the lumbar BMD. These results suggest that a distal forearm DEXA scan is useful for measuring BMD and better assessing the risk of DRF in patients who were not initially diagnosed with osteoporosis by a central DEXA scan.
The distal forearm T-scores were significantly lower for the fracture group compared with the control group. This indicates that the lower distal forearm DEXA scan measurements may be more closely correlated with the occurrence of a distal radius fracture, especially in patients that might not necessarily be candidates for conventional osteoporosis treatment plans. Our findings that the distal radius BMD measurements were overall lower than the central BMD measurements and that the ultradistal radius BMD measurement was lower than the one-third radius BMD measurement align with what has been reported in existing literature [3, 10, 33]. Moreover, a remarkable number of patients with a T-score under − 2.5 for distal forearm BMD in both groups indicates that measuring distal forearm BMD in addition to central BMD might be helpful for the early detection of osteoporosis and the prevention of further osteoporotic fractures. Recent studies similar to ours also describe the significance of identifying microstructural deficits and low BMD of the distal radius for predicting DRFs or fragility fractures at other sites [3, 10, 12, 34, 35].
We also identified the clinical significance of a distal forearm DEXA scan for earlier diagnosis and prevention of DRFs in both sites (ultradistal radius and distal one-third radius). First, the T-scores for the ultradistal radius were the strongest predictor of a DRF. This is one of the most important findings of this study because the conventional approach to measuring peripheral BMD has focused on the distal one-third radius. Although there is no consensus on which site is better for predicting osteoporosis, the distal one-third radius is the current standard of care [11, 27, 28]. Our findings present a new option that may provide more accurate diagnoses for patients and ultimately better prevent fragility fractures. Second, a previous study described that a lower value for both cortical volumetric and areal BMD for the one-third radius was significantly correlated with DRFs in the pediatric population [12]. However, DRFs in older adults predominantly occur in the distal metaphysis, comprised of both rich cortical and trabecular bone, rather than the diaphysis which is predominantly comprised of cortical bone [36]. Age-related bone loss first occurs in the cancellous bone, then secondary bone, followed by a loss in cortical bone and endocortical surface. Distal radial metaphysis seems to be more affected by age-related changes [3, 37], and this might be reflected by the earlier loss of BMD at the ultradistal radius compared with other sites. Likewise, a previous study described premenopausal women with forearm fractures showing deficits only in trabecular bone volume with the normal cortical area, while older postmenopausal women with forearm fractures showed deficits in the trabecular bone volume and cortical porosity [36]. Second, the distal one-third radius BMD is closely related to the hip BMD. This could be explained by a larger portion of cortical bone affecting the hip BMD, similar to the distal one-third of radial diaphysis. However, the lumbar spine BMD seems to contain a relatively large proportion of cancellous bone and this could sometimes be overestimated due to degeneration of vertebra in elderly patients3. Based on all these findings, we anticipate that measuring the distal forearm BMD at both sites would be important. However, as the ultradistal radius BMD measurements showed significant differences and independence from the other sites, distal forearm DEXA scans would be valuable only when performed along with a central DEXA. Moreover, as the conventional methods for predicting osteoporotic fractures including the FRAX score were not adjustable for the population that was not diagnosed with osteoporosis, the distal forearm BMD could be a useful tool for specific circumstances like those in our study design (when osteoporosis was not diagnosed at the central DEXA but identification of bone deficits within the distal radius is required).
The present study had some limitations. First, this was a retrospective, single-center case-control study design, which may have a selection bias. Due to the strict inclusion and exclusion criteria, it only represented a specific subset of older female patients, not the average older adults. Second, some variables that could affect the outcomes such as smoking history, nutritional status, and some serum biochemical markers for bone turnover were not investigated. Third, as the outcomes could be affected by patient position or difference in the region of interest by each measurement, some information biases could exist, especially for the lumbar spine BMD as we only used the average value of L2–L4. Finally, although current research trends have focused on more detailed measurements using quantitative computed tomography (QCT), including volumetric BMD, bone geometry, and distinguishment between the cortical and trabecular area, our study was performed mainly on the DEXA. However, the superiority of the QCT over the DEXA for improving the prediction of fragility fractures has not been established [34]. Further, when using the QCT, more specific circumstances and more detailed measurements are required, and its results may have limited reproducibility in a less-equipped healthcare facility. Moreover, the current standard of care for the diagnosis of osteoporosis is still areal BMD measured by DEXA [11, 27].
Conclusion
A distal forearm DEXA scan performed in addition to a central DEXA may be an effective tool for detecting the osteoporotic conditions of the distal radius, which is associated with an increased risk of osteoporotic DRF. The ultradistal radius T-score was the strongest value for predicting the DRF and the distal one-third radius DEXA measurements were correlated with the hip DEXA measurements.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- DEXA:
-
Dual-energy X-ray absorptiometry
- BMD:
-
Bone mineral density
- DRF:
-
Distal radius fracture
- SD:
-
Standard deviations
- BMI:
-
Body mass index
- CCI:
-
Charlson comorbidity index
- FRAX®:
-
The fracture risk assessment tool
- OR:
-
Odds ratio
- QCT:
-
Quantitative computed tomography
References
Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465–75.
Samelson EJ, Broe KE, Xu H, et al. Cortical and trabecular bone microarchitecture predicts incident fracture independently of DXA bone mineral density and FRAX in older women and men: the bone microarchitecture international consortium (BoMIC). Lancet Diabetes Endocrinol. 2019;7:34–43.
Wilson J, Bonner TJ, Head M, et al. Variation in bone mineral density by anatomical site in patients with proximal humeral fractures. J Bone Joint Surg (Br). 2009;91:772–5.
Jung HS, Jang S, Chung HY, et al. Incidence of subsequent osteoporotic fractures after distal radius fractures and mortality of the subsequent distal radius fractures: a retrospective analysis of claims data of the Korea National Health Insurance Service. Osteoporos Int. 2021;32:293–9.
Barrett-Connor E, Sajjan SG, Siris ES, et al. Wrist fracture as a predictor of future fractures in younger versus older postmenopausal women: results from the National Osteoporosis Risk Assessment (NORA). Osteoporos Int. 2008;19:607–13.
Melton LJ III. Epidemiology of fractures. In: Riggs BL, Melton III LJ, editors. Osteoporosis: etiology, diagnosis and management. Philadelphia: Lippincott-Raven; 1995. p. 225–47.
Schousboe JT, Fink HA, Taylor BC, et al. Association between self-reported prior wrist fractures and risk of subsequent hip and radiographic vertebral fractures in older women: a prospective study. J Bone Miner Res. 2005;20:100–6.
Oyen J, Brudvik C, Gjesdal CG, et al. Osteoporosis as a risk factor for distal radial fractures: a case-control study. J Bone Joint Surg Am. 2011;93:348–56.
Cuddihy MT, Gabriel SE, Crowson CS, et al. Forearm fractures as predictors of subsequent osteoporotic fractures. Osteoporos Int. 1999;9:469–75.
Miyamura S, Kuriyama K, Ebina K, et al. Utility of distal forearm DXA as a screening tool for primary osteoporotic fragility fractures of the distal radius: a case-control study. JBJS Open Access. 2020;5:e0036.
The International Society for Clinical Densitometry. 2019 ISCD official positions—adult 2019. https://iscd.org/learn/official-positions/adult-positions. Accessed 21 October 2021.
Kalkwarf HJ, Laor T, Bean JA. Fracture risk in children with a forearm injury is associated with volumetric bone density and cortical area (by peripheral QCT) and areal bone density (by DXA). Osteoporos Int. 2011;22:607–16.
Earnshaw SA, Cawte SA, Worley A, et al. Colles' fracture of the wrist as an indicator of underlying osteoporosis in postmenopausal women: a prospective study of bone mineral density and bone turnover rate. Osteoporos Int. 1998;8:53–60.
Hegeman JH, Oskam J, van der Palen J, et al. The distal radial fracture in elderly women and the bone mineral density of the lumbar spine and hip. J Hand Surg (Br). 2004;29:473–6.
Löfman O, Hallberg I, Berglund K, et al. Women with low-energy fracture should be investigated for osteoporosis. Acta Orthop. 2007;78:813–21.
Lashin H, Davie MW. DXA scanning in women over 50 years with distal forearm fracture shows osteoporosis is infrequent until age 65 years. Int J Clin Pract. 2008;62:388–93.
Lee JO, Chung MS, Baek GH, et al. Age-and site-related bone mineral densities in Korean women with a distal radius fracture compared with the reference Korean female population. J Hand Surg [Am]. 2010;35:1435–41.
Jung HJ, Park HY, Kim JS, et al. Bone mineral density and prevalence of osteoporosis in postmenopausal Korean women with low-energy distal radius fractures. J Korean Med Sci. 2016;31:972–5.
Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996;312:1254–9.
Siris ES, Miller PD, Barrett-Connor E, et al. Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. JAMA. 2001. https://doi.org/10.1001/jama.286.22.2815.
Freedman KB, Kaplan FS, Bilker WB, et al. Treatment of osteoporosis: are physicians missing an opportunity? J Bone Joint Surg Am. 2000;82:1063–70.
Andrade SE, Majumdar SR, Chan KA, et al. Low frequency of treatment of osteoporosis among postmenopausal women following a fracture. Arch Intern Med. 2003;163:2052–7.
Rozental TD, Makhni EC, Day CS, et al. Improving evaluation and treatment for osteoporosis following distal radial fractures: a prospective randomized intervention. J Bone Joint Surg Am. 2008;90:953–61.
Sarfani S, Scrabeck T, Kearns AE, et al. Clinical efficacy of a fragility care program in distal radius fracture patients. J Hand Surg [Am]. 2014;39:664–9.
Gong HS, Oh WS, Chung MS, et al. Patients with wrist fractures are less likely to be evaluated and managed for osteoporosis. J Bone Joint Surg Am. 2009;91:2376–80.
Shah GM, Gong HS, Chae YJ, et al. Evaluation and management of osteoporosis and sarcopenia in patients with distal radius fractures. Clin Orthop Surg. 2020;12:9–21.
World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: report of a WHO study group [meeting held in Rome from 22 to 25 June 1992]. 1992 https://apps.who.int/iris/handle/10665/39142. Accessed 23 October 2021.
Yu W, Ying Q, Guan W, et al. Impact of reference point selection on DXA-based measurement of forearm bone mineral density. Arch Osteoporos. 2019;14:1–7.
Lorente-Ramos R, Azpeitia-Armán J, Muñoz-Hernández A, et al. Dual-energy x-ray absorptiometry in the diagnosis of osteoporosis: a practical guide. AJR Am J Roentgenol. 2011;196:897–904.
Min DG, Lee JH, Choe HS, et al. Comparison of bone density on the dominant and nondominant sides between healthy elderly individuals and stroke patients. J Phys Ther Sci. 2016;28:2533–6.
World Health Organization Collaborating Centre for Metabolic Bone Diseases. FRAX® WHO Fracture Risk Assessment Tool. 2011. http://www.shef.ac.uk/FRAX. Accessed 1 October 2021.
D'Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–81.
Arlot ME, Sornay-Rendu E, Garnero P, et al. Apparent pre-and postmenopausal bone loss evaluated by DXA at different skeletal sites in women: the OFELY cohort. J Bone Miner Res. 1997;12:683–90.
Biver E, Durosier-Izart C, Chevalley T, et al. Evaluation of radius microstructure and areal bone mineral density improves fracture prediction in postmenopausal women. J Bone Miner Res. 2018;33:328–37.
Link TM, Vieth V, Matheis J, et al. Bone structure of the distal radius and the calcaneus vs BMD of the spine and proximal femur in the prediction of osteoporotic spine fractures. Eur Radiol. 2002;12:401–8.
Bala Y, Bui QM, Wang XF, et al. Trabecular and cortical microstructure and fragility of the distal radius in women. J Bone Miner Res. 2015;30:621–9.
Chen H, Zhou X, Fujita H, et al. Age-related changes in trabecular and cortical bone microstructure. Int J Endocrinol. 2013;2013:213234.
Acknowledgements
None.
Funding
This paper was supported by Eulji University in 2022 (EJRG-22-23), Daejeon, Republic of Korea.
Author information
Authors and Affiliations
Contributions
S.B.M: conception and design of the study; acquisition of data; drafting the article. S.K.L: conception of the study; drafting the article and revising it critically for important intellectual content; final approval of the version for submission. Y.S.A: acquisition of data; statistics. W.S.K: acquisition of data. W.S.C: acquisition of data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was reviewed and approved by the University of Eulji Institutional Review Board. Written informed consent was obtained from all study participants. In this study, all methods were performed following the Declaration of Helsinki relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ma, S.B., Lee, S.K., An, Y.S. et al. The clinical necessity of a distal forearm DEXA scan for predicting distal radius fracture in elderly females: a retrospective case-control study. BMC Musculoskelet Disord 24, 177 (2023). https://doi.org/10.1186/s12891-023-06265-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06265-5