Abstract
Background
Corona virus infectious pandemic makes outdoors rehabilitation a potential hazard. Patient education to perform simple home-based exercises seems to be an interesting and sometimes a mandatory option. This study provides a comparison between the conventional and home-based virtual rehabilitation after surgical repair of medial meniscus root tears.
Methods
In this prospective study, all patients who underwent medial meniscus posterior root repair with a modified trans-tibial pull-out technique from March 2019 to March 2021 were evaluated. Those who underwent surgery after December 2019 were trained to perform self-rehabilitation. The rest had undergone outdoors specialized rehabilitation according to a unified protocol and these were used as a historical control group. All patients were followed up for a minimum of 2 year after surgery. Final Lysholm scores were utilized to compare functional outcomes after considering the effect of age, body mass index and time from surgery by multivariate linear regression analysis.
Results
Forty-three consecutive patients with medial meniscal root tears were studied. Thirty-nine (90.7%) were women and 4 (9.3%) were men. The mean age of participants was 53.2 ± 8.1 years. The total Lysholm knee score, and all its items were significantly improved in both groups at a two-year follow-up (p < 0.05), except the “Using cane or crutches” item (p = 0.065). Nevertheless, the final Lysholm knee score improvement was higher in patients who performed outdoors specialized rehabilitation and in patients with shorter time-to-surgery.
Conclusion
Regardless of age and gender, home-based rehabilitation after meniscal root repair with the modified trans-tibial pull-out technique improved the patients’ function at a two-year follow-up. Nonetheless, this effect was still significantly lower than that of the outdoors specialized rehabilitation. Future work is required to clarify basic protocols for home-based tele-rehabilitation programs and determine clinical, radiological and functional results.
Level of evidence
Level IV, therapeutic, historically controlled study.
Similar content being viewed by others
Introduction
Meniscal roots convert the axial load into hoop stress and distribute the pressure symmetrically in the articular surface [1]. Root injuries are defined as either avulsion of posterior tibial attachment or radial tear of the posterior horn within 1 cm of its attachment [2, 3]. The meniscal root injury results in meniscal extrusion and if left untreated, root injury can lead to early osteoarthritis [4,5,6,7,8]. Several methods have been introduced for diagnosis and repair of a medial meniscal posterior root tear [9,10,11]. The trans-tibial pull-out repair technique involves passing a suture through the meniscal root and retrieving it through a tibial tunnel. Screw or button fixation can then be used. Biomechanical and clinical outcomes of different suturing techniques have been previously scrutinized [12,13,14]. Despite recent advances in meniscal root repair, this remains a challenging procedure with several potential complications including loosening and re-tear [15, 16].
The effects of corona virus infectious disease (COVID-19) pandemic on orthopedics cannot be overlooked [17,18,19]. It has profoundly affected postoperative rehabilitation. COVID-19 pandemic has created further obstacles on the way of achieving the best possible functional outcomes. Most patients are afraid to participate in outdoors rehabilitation and cannot afford home-based private physical therapy.
In the current study, patients with medial meniscal posterior root tear (MPRT) underwent surgical repair of the tear with a modified trans-tibial pull-out technique. We sought out to determine (1) if these patients can experience significant improvement in function with home-based self-rehabilitation, and (2) if there is a significant difference in functional outcomes between the patients who are forced to perform home-based self-rehabilitation and those who have access to specialized physical therapy.
Patients and methods
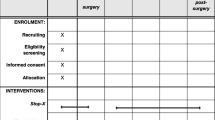
This retrospective cohort studies all patients who underwent surgical repair of the MPRT from March 2019 till March 2020 in a tertiary knee center. The study protocol was reviewed and approved by the local ethics committee. The procedure was described for all patients and informed written consents were obtained. Two separate fellowship trained knee surgeons were involved who used the same surgical technique for root repair. Baseline patient characteristics and the time interval from the acute onset/exacerbation of knee pain to the surgery (time-to-surgery intervals) were recorded. The severity of knee osteoarthritis prior to and after surgery was assessed based on Kellgren- Lawrence (K-L) classification [20]. Surgical repair was considered for patients with symptomatic MPRT with a stable knee joint and no major malalignment or severe osteoarthritis (KL II or less). Diagnosis of an MPRT was confirmed with magnetic resonance (MR) imaging, after identifying relevant clinical findings [2]. Those patients younger than 18 years of age, those with less than two-year follow-up or with concomitant anterior cruciate ligament (ACL) injury were excluded from the study. Those patients who underwent surgery after December 2019 (COVID-19 era patients) were trained to perform self-rehabilitation. Those who underwent surgery and completed their rehabilitation before December 2019 (non-COVID era patients) had undergone outdoors specialized rehabilitation according to a unified protocol and these were used as a historical control group. This methodology is sound and has been used before [21]. Patients were examined for a follow-up period of at least two years after surgery by their surgeon, and Lysholm knee score was recorded [22].
Surgical technique
The loop-post construct technique, which was introduced in 2020, as a modification of the standard trans-tibial pull-out method of repairing meniscal root tears was used [23]. After performing a diagnostic arthroscopy via the anterolateral (AL) portal, the near anteromedial (AM) portal was created by a vertical incision just adjacent to the medial border of the patellar tendon. Notchplasty of the medial wall helped to provide better access to the MPRT in cases of a narrow notch. Percutaneous release of the superficial medial collateral ligament was performed in all cases to increase the working space. A far AM portal was then created by a horizontal incision after identifying the appropriate location using a spinal needle. The MPRT footprint was identified and freshened using a curette. The meniscal root was reduced by an arthroscopic grasper. If scar tissue or fibrosis was limiting the mobility of the meniscus, it was debrided to release the meniscal root and help its reduction into the footprint. The fibrotic end of the torn or avulsed meniscal root was freshened with a shaver. Through the far AM portal, the EZPass™ 70˚ Suture Passer (Zimmer-Biomet) was introduced. A nylon 1/0 thread was passed from the superior to the inferior surface of the meniscus one centimeter from the torn end as a shuttle, to help passing the Fiber Wire 2–0 suture (Arthrex, Naples, FL) or Express-Braid™ no.2 suture (Zimmer Biomet, Warsaw, IN) as the first loop. The second loop was created in a similar manner at 5 mm from the torn end of the meniscal root (in the traditional trans-tibial pull-out technique, both sutures were passed 5 mm from the edge). Before tightening the second loop, both free ends of the first loop were passed and locked under the second loop and then they were retrieved through the portal (Fig. 1). In order to create the tibial tunnel, a tibial target guide for ACL (Karl Storz, Tuttlingen, Germany or Conmed Linvatec, USA) was used. The guide was inserted through the near AM portal, and its tip was placed at the footprint. Reaming was performed with a 4.3 mm ACL reamer. A Flip Cutter® II, 8 mm Drill (Arthrex) was inserted through the reamed canal, to (1) confirm the tunnel’s position in the anatomical footprint with arthroscopy and (2) perform minimally invasive inside-out reaming of the tibial tunnel. Both ends of the loop and post constructs were retrieved through the tunnel. Tension was applied to the thread ends in 30˚ of knee flexion, and then they were fixed on the tibial cortex around a screw-washer construct. We tend to over-reduce the meniscus by tensioning the root to the point that at least 5 mm of the root enters the tunnel before final fixation.
The arthroscopic view of the Loop-Post Construct technique. The first and second loop constructs are identified by green and red lines, respectively [23]. (Reproduced with permission from: Tahami M, Vaziri AS, Tahmasebi MN. Loop-Post Construct, A Novel Technique for Medial Meniscal Root Repair. Archives of Bone and Joint Surgery. 2020;8(4):545.)
Postoperative rehabilitation
Rehabilitation protocols were adjusted from Mueller et al. meniscus root rehabilitation concepts [24]. The knee was immobilized and locked in extension for two weeks. Range of motion exercises started 2 weeks postop, with the goal of reaching 90 degrees of flexion by the end of the 6th week. Passive range of motion exercises to reach 90 degrees of flexion during the first six weeks after the operation included supine wall slides and hanging the leg from the bed. Patellar mobilization exercises were started and performed by the therapist or the patient himself. Open chain quadriceps exercises were performed immediately after surgery during hospitalization period under supervision. Furthermore, partial weight-bearing exercises (i.e., toe touching using crutches) started during the first two weeks, with the brace locked in extension. Full weight-bearing was permitted after six weeks.
Postoperative rehabilitation was performed either as an outdoors specialized rehabilitation or by the patients themselves as a home-based self-rehabilitation due to the force of isolation after the COVID-19 outbreak. Self- rehabilitation at home included training of the patients to perform straight leg raising, range of motion and patellar mobilization exercises. Patient education was performed by the surgeon and the physical therapist before discharge from the hospital. After being discharged, virtual education and virtual follow-up with the physical therapist using social media, mostly Whatsapp (Facebook, Inc) helped to ensure proper adherence to the instructions and patient progressions during this process were supervised by both the surgeon and the physical therapist. The virtual postoperative follow ups were scheduled weekly until 6 weeks or until achievement of 90’ flexion and full weight bearing; whichever happened sooner. After which the patient was followed virtually at 3 months postoperative.
Meanwhile, outdoors specialized rehabilitation was performed by a trained physical therapist with a uniform protocol including range of motion exercises, vastus medialis strengthening, patellar mobilization, open-chain quadriceps isometric exercises, hamstring stretching and pain reduction modalities.
Statistical analysis
Statistical analysis was applied by R programming language (version 3.3.1 for Mac OS) with deducer graphical user interface (GUI) package, and the results were visualized by GraphPad Prism (version 8.2.1 for Mac OS). Quantitative and qualitative variables were described using mean ± standard deviation (SD) or median and frequency (percentage), respectively. The primary objective was to compare the baseline and the two-year post-surgical total Lysholm knee score and its domains. The effect of demographic, clinical variables and type of rehabilitation on Lysholm Knee Score change (Δ LKS) was analyzed using the Wilcoxon rank-sum test. Comparing means for normally distributed variables was performed by paired t test. Correlations were test by the Mann–Whitney test. A p-value < 0.05 was considered as statistically significant. Multivariate linear regression analysis was performed to detect the effect of age, BMI, time from surgery and type of rehabilitation on final LKS.
Results
Forty-nine consecutive patients who underwent root repair with the modified trans-tibial pull-out technique during the specified time period were eligible for inclusion in the study. Six patients were excluded (lost to follow-up), leaving 43 patients who participated in this study. Patient characteristics and clinical outcomes are provided separately (Tables 1 and 2). Approximately, two-thirds of the patients completed outdoors specialized rehabilitation before the COVID-19 outbreak (29 [67.4%]). The remaining 14 patients [32.5%] were trained to perform home-based self-rehabilitation. The median Kellgren- Lawrence grades of knee osteoarthritis were 1 both prior to and two years after surgery. No patient experienced a change in the grade of osteoarthritis during the study time frame. Furthermore, according to the total Lysholm knee scores, two-year functional outcome was excellent in 16 (37.2%), good in 18 (41.8%), fair in 7 (16.2%) and poor in 2 (4.6%) patients. Figure 2 illustrates pre-operative and two-year post-operative functional scores of patients using the Lysholm knee score (the entire cohort). The total final Lysholm knee score (LKS), along with all its subscales showed significant improvement in both groups, except the “Using cane or crutches” subscale which showed no significant difference (p = 0.065) (Fig. 2).
The increase in the final Lysholm knee score (which means functional improvement) was higher in patients in the non-COVID era (Δ LKS +rehabilitation = 20 ± 9.13 vs, Δ LKS -rehabilitation = 12.55 ± 5.01; p = 0.012) (Fig. 3). Furthermore, in both groups, improvement was significantly higher among the patients with shorter time-to-surgery interval (r coefficient = -0.51, 95%, confidence interval (CI) = -0.7264, -0.2026; p = 0.002). Patient’s age (r coefficient = 0.045, 95% CI = -0.3027, 0.3827; P = 0.849) and sex (Δ LKS female = 18.16 ± 9.65 vs. Δ LKS male = 15.5 ± 4.34; P = 0.802), on the other hand, did not show any significant correlation with final Lysholm knee scores.
Multivariate analysis (Table 3) showed that, after considering the confounding effect of age, BMI and time from surgery, still the type of rehabilitation was an independent factor associated with higher final Lysholm scores (β = 7.6, P = 0.008).
Discussion
During the last 15 years, techniques for surgical repair of MPRT have been developed to restore joint biomechanics and joint contact pressures, to prevent the joint from early osteoarthritis. Trans-tibial pull-out repair is one of the most common procedures for meniscal root repair [25]. The transtibial tunnel drilling releases growth factors and progenitor cells from bone marrow and may improve the healing process [26]. Moreover, previous studies [15, 27] reported significant improvement in clinical and radiographic outcomes. A slight modification of the trans-tibial pull-out technique has recently been introduced, called the loop-post construct technique, for meniscal root repair [23]. In the present study, the two-year functional outcomes of this technique showed significant improvement in Lysholm knee scoring items. Admittedly, without a control group utilizing a standard trans-tibial pull-out technique, it seems inappropriate to conclude anything on the clinical advantage of this modified technique.
Included patients were mostly females at their mid-fifties. Patients with a stable knee and no sign of severe osteoarthritis or major malalignment were scheduled for surgical repair of the MPRT. This demographic pattern and surgical indications are in consistency with previous reports [28, 29]. Conversion to total knee arthroplasty and the progression of Kellgren-Lawrence grade are two noticeable concerns in choosing the treatment modality for meniscal root tear. Hence, root repair is a wise choice for active patients with acute root tears or those with root tears who have minimal or absent osteoarthritis [14, 26, 30, 31]. Noticeably, our results show no progression of osteoarthritis during the study time frame; nevertheless, long-term follow up periods might yield different results.
No correlation was seen between demographic characteristics such as age or gender and functional outcomes after root repair. This finding is interesting since we expected to see variable results of self-rehabilitation between different age/sex groups, due to different levels of compliance. Frankly this study involved a limited age range, which might have masked this effect. Besides, previous studies such as Laprade et al. [32] reported no significant differences in clinical and radiological changes between patients older than 50 and younger than 50 years of age. The effects of age and gender on the functional outcomes of home-based rehabilitation have yet to be proven.
Time interval from the onset/ exacerbation of knee pain to surgery was significantly correlated with clinical outcomes. As a result, assigning meniscal root repair methods as soon as possible amongst eligible patients might improve the outcomes of the surgery, a notion which has been stated in the previous reports [2].
All patient undergoing root repair in our centers were started on a specialized rehabilitation program with a unified protocol in the non-COVID era. Outbreak of the SARS-COV-2 infection in December 2019 and isolation protocols prevented the patients from participating in such programs. Most patients were afraid to perform outdoors rehabilitation and were unable to afford home-based private physical therapy either. Therefore, we were forced to train the patients to perform simple rehabilitation tasks at home.
Our results show significant improvement in patient reported outcomes in both non-COVID and COVID era patients. Fortunately, no case of limited knee range of motion was encountered in neither group. Still and all, those who had access to specialized physical therapy (the non-COVID era group) experienced significantly better outcomes. While no study was found in the literature after the COVID-19 outbreak to take this matter into consideration, some previous reports have considered a comparison between restricted and accelerated rehabilitation [33,34,35]. VanderHave et al. [33], for instance, found a comparable successful clinical outcome regarding restricted and accelerated rehabilitation (70–94 vs. 64–96%). On the other hand, Vascellari et al. [34] did not report a difference in repair failure (10% vs. 13%). Noticeably, significant heterogeneity existed among previous reports.
Before jumping into any conclusions, one must consider some serious limitations of this study. We did not use visual analogue scale for pain, however we reported Lysholm scores which show the level of pain patients encounter during everyday activities. Lack of MRI evaluation and a follow-up of two years are two important limitations of this study. The COVID-19 outbreak has only begun since two to three years ago; therefore, follow-up period could not be any longer and our sample size is relatively small. Even so, we felt compelled to share our concerns and results. Indeed, this seems to be a global on-going problem which might deeply affect not only our routine clinical practice, but also our rehabilitation protocols and postoperative care. Due to a lack of control subjects, we compared the results with historical controls who had completed their postoperative rehabilitation before the start of the pandemic. Another limitation, is the modification of the standard trans-tibial pull-out technique that we used to repair root tears [23]. No biomechanical testing has been performed for this technique, still, its basics have been proven both biomechanically and clinically in the literature [13, 14, 32].
Conclusion
In summary, the results reveal that regardless of age and gender, patients can reach significant functional improvements even with home-based simple rehabilitation tasks after arthroscopic repair of MPRT. Nonetheless, better outcomes were associated with postoperative specialized rehabilitation programs and earlier surgery. Future work is required to clarify basic protocols for home-based tele-rehabilitation programs and determine clinical, radiological and functional results.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
Keyhani S, Vaziri AS, Vosoughi F, Verdonk R, Movahedinia M. Overview of posterior knee arthroscopy in the medial meniscal repair: Technical note. J ISAKOS. 2022;7(3):33–8.
Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Ziegler C, LaPrade RF. Meniscal root tears: current concepts review. Archives of Bone and Joint Surgery. 2018;6(4):250.
Hashemi SA, Ranjbar MR, Tahami M, Shahriarirad R, Erfani A. Comparison of accuracy in expert clinical examination versus magnetic resonance imaging and arthroscopic exam in diagnosis of meniscal tear. Adv Orthop. 2020;2020:1895852.
Foreman SC, Liu Y, Nevitt MC, Neumann J, Joseph GB, Lane NE, McCulloch CE, Link TM. Meniscal Root Tears and Extrusion Are Significantly Associated with the Development of Accelerated Knee Osteoarthritis: Data from the Osteoarthritis Initiative. Cartilage. 2021;13(1_suppl):239S–48S.
Krych AJ, Hevesi M, Leland DP, Stuart MJ. Meniscal root injuries. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2020;28(12):491–9.
Englund M, Roemer FW, Hayashi D, Crema MD, Guermazi A. Meniscus pathology, osteoarthritis and the treatment controversy. Nat Rev Rheumatol. 2012;8(7):412–9.
Tahami SM, Rad SMD. Outcome of ACL reconstruction and concomitant articular injury treatment. Arch Bone Jt Surg. 2015;3(4):260.
Aghaghazvini L, Tahmasebi MN, Gerami R, Vaziri AS, Rasuli B, Tahami M, Vosoughi F. Sonography: a sensitive and specific method for detecting trochlear cartilage pathologies. J Ultrasound. 2020;23(3):259–63.
Kennedy MI, Strauss M, LaPrade RF. Injury of the meniscus root. Clin Sports Med. 2020;39(1):57–68.
Bernard CD, Kennedy NI, Tagliero AJ, Camp CL, Saris DB, Levy BA, Stuart MJ, Krych AJ. Medial meniscus posterior root tear treatment: a matched cohort comparison of nonoperative management, partial meniscectomy, and repair. Am J Sports Med. 2020;48(1):128–32.
Sharafat Vaziri A, Aghaghazvini L, Jahangiri S, Tahami M, Borazjani R, Tahmasebi MN, Rabie H, Mamaghani HJ, Vosoughi F, Salimi M: Determination of Normal Reference Values for Meniscal Extrusion Using Ultrasonography During the Different Range of Motion. J Ultrasound Med. 2022. https://doi.org/10.1002/jum.15955. Epub ahead of print. PMID: 35137975.
Forkel P, Foehr P, Meyer JC, Herbst E, Petersen W, Brucker PU, Burgkart R, Imhoff AB. Biomechanical and viscoelastic properties of different posterior meniscal root fixation techniques. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):403–10.
LaPrade CM, LaPrade MD, Turnbull TL, Wijdicks CA, LaPrade RF. Biomechanical evaluation of the transtibial pull-out technique for posterior medial meniscal root repairs using 1 and 2 transtibial bone tunnels. Am J Sports Med. 2015;43(4):899–904.
LaPrade RF, LaPrade CM, James EW. Recent advances in posterior meniscal root repair techniques. JAAOS - Journal of the American Academy of Orthopaedic Surgeons. 2015;23(2):71–6.
Chung KS, Ha JK, Ra HJ, Nam GW, Kim JG. Pullout fixation of posterior medial meniscus root tears: correlation between meniscus extrusion and midterm clinical results. Am J Sports Med. 2017;45(1):42–9.
Steineman BD, LaPrade RF, Donahue TLH. Loosening of transtibial pullout meniscal root repairs due to simulated rehabilitation is unrecoverable: a biomechanical study. Arthroscopy. 2019;35(4):1232–9.
Nabian MH, Vosoughi F, Najafi F, Khabiri SS, Nafisi M, Veisi J, Rastgou V, Ghamari S, Aakhashi A, Bahrami N, et al. Epidemiological pattern of pediatric trauma in COVID-19 outbreak: data from a tertiary trauma center in Iran. Injury. 2020;51(12):2811–5.
Masiero S, Maccarone MC, Agostini F. Health resort medicine can be a suitable setting to recover disabilities in patients tested negative for COVID-19 discharged from hospital? a challenge for the future. Int J Biometeorol. 2020;64(10):1807–9.
Agostini F, Mangone M, Ruiu P, Paolucci T, Santilli V, Bernetti A. Rehabilitation setting during and after Covid-19: an overview on recommendations. J Rehabil Med. 2021;53(1):16501977–2776.
Kohn MD, Sassoon AA, Fernando ND. Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop Relat Res. 2016;474(8):1886–93.
Tahmasebi MN, Vaziri AS, Vosoughi F, Tahami M, Khalilizad M, Rabie H. Low post-arthroplasty infection rate is possible in developing countries: long-term experience of local vancomycin use in Iran. J Orthop Surg Res. 2021;16(1):199.
Briggs KK, Kocher MS, Rodkey WG, Steadman JR. Reliability, validity, and responsiveness of the Lysholm knee score and Tegner activity scale for patients with meniscal injury of the knee. JBJS. 2006;88(4):698–705.
Tahami M, Vaziri AS, Tahmasebi MN. Loop-post construct, a novel technique for medial meniscus root repair. Archives of Bone and Joint Surgery. 2020;8(4):545.
Mueller BT, Moulton SG, O’Brien L, LaPrade RF. Rehabilitation Following Meniscal Root Repair: A Clinical Commentary. J Orthop Sports Phys Ther. 2016;46(2):104–13.
Jiang EX, Everhart JS, Abouljoud M, Kirven JC, Magnussen RA, Kaeding CC, Flanigan DC. Biomechanical properties of posterior meniscal root repairs: a systematic review. Arthroscopy. 2019;35(7):2189-2206. e2182.
Woodmass JM, LaPrade RF, Sgaglione NA, Nakamura N, Krych AJ. Meniscal repair: reconsidering indications, techniques, and biologic augmentation. JBJS. 2017;99(14):1222–31.
Feucht MJ, Kühle J, Bode G, Mehl J, Schmal H, Südkamp NP, Niemeyer P. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: a systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31(9):1808–16.
Bin S-I, Kim J-M, Shin S-J. Radial tears of the posterior horn of the medial meniscus. Arthroscopy. 2004;20(4):373–8.
Furumatsu T, Okazaki Y, Okazaki Y, Hino T, Kamatsuki Y, Masuda S, Miyazawa S, Nakata E, Hasei J, Kunisada T. Injury patterns of medial meniscus posterior root tears. Orthop Traumatol Surg Res. 2019;105(1):107–11.
Kopf S, Beaufils P, Hirschmann MT, Rotigliano N, Ollivier M, Pereira H, Verdonk R, Darabos N, Ntagiopoulos P, Dejour D: Management of traumatic meniscus tears: the,. ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc. 2019;2020:1–18.
Stein JM, Yayac M, Conte EJ, Hornstein J. Treatment outcomes of meniscal root tears: a systematic review. Arthrosc Sports Med Rehabil. 2020;2(3):e251–61.
LaPrade RF, Matheny LM, Moulton SG, James EW, Dean CS. Posterior meniscal root repairs: outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45(4):884–91.
VanderHave KL, Perkins C, Le M. Weightbearing versus nonweightbearing after meniscus repair. Sports Health. 2015;7(5):399–402.
Vascellari A, Rebuzzi E, Schiavetti S, Coletti N. All-inside meniscal repair using the FasT-Fix meniscal repair system: is still needed to avoid weight bearing? A systematic review Musculoskeletal surgery. 2012;96(3):149–54.
Derakhshanrad N, Vosoughi F, Yekaninejad MS, Moshayedi P, Saberi H. Functional impact of multidisciplinary outpatient program on patients with chronic complete spinal cord injury. Spinal Cord. 2015;53(12):860–5.
Acknowledgements
None.
Funding
No funding was received for the current study.
Author information
Authors and Affiliations
Contributions
MT helped with study conception and design and critical revision of the manuscript. ASV helped with interpreting data, critical revision of the manuscript. MNT helped with data interpretation and critical revision of the manuscript. AA helped with study design and drafting the manuscript study design. MAA helped with data gathering and drafting the manuscript. FV helped with interpreting data and critical revision and submitting the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was reviewed and approved by the Institutional Review Board of Shiraz University of Medical Sciences (IR.sums.med.rec.1399.459). All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all participants.
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors are on file with the publication and can be viewed on request.
The current study was approved by the institutional review board of Shiraz University of Medical sciences (IR.sums.med.rec.1399.459).
This work was performed as a multi-center study in the Shiraz and Tehran Universities of medical sciences in Iran.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tahami, M., Vaziri, A.S., Tahmasebi, M.N. et al. The functional impact of home-based self-rehabilitation following arthroscopic meniscus root repair. BMC Musculoskelet Disord 23, 753 (2022). https://doi.org/10.1186/s12891-022-05662-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05662-6