Abstract
Purpose
The study aims to investigate the accuracy of different radiographic signs for predicting functional deficiency of anterior cruciate ligament (ACL) and test whether the prediction model constructed by integrating multiple radiographic signs can improve the predictive ability.
Methods
A total number of 122 patients from January 1, 2018, to September 1, 2021, were enrolled in this study. Among them, 96 patients were classified as the ACL-functional (ACLF) group, while 26 patients as the ACL-deficient (ACLD) group after the assessment of magnetic resonance imaging (MRI) and the Lachman’s test. Radiographic measurements, including the maximum wear point of the proximal tibia% (MWPPT%), tibial spine sign (TSS), coronal tibiofemoral subluxation (CTFS), hip–knee–ankle angle (HKA), mechanical proximal tibial angle (mPTA), mechanical lateral distal femoral angle (mLDFA) and posterior tibial slope (PTS) were measured using X-rays and compared between ACLF and ACLD group using univariate analysis. Significant variables (p < 0.05) in univariate analysis were further analyzed using multiple logistic regression analysis and a logistic regression model was also constructed by multivariable regression with generalized estimating models. Receiver-operating-characteristic (ROC) curve and area under the curve (AUC) were used to determine the cut-off value and the diagnostic accuracy of radiographic measurements and the logistic regression model.
Results
MWPPT% (odds ratio (OR) = 1.383, 95% confidence interval (CI) = 1.193–1.603, p < 0.001), HKA (OR = 1.326, 95%CI = 1.051–1.673, p = 0.017) and PTS (OR = 1.981, 95%CI = 1.207–3.253, p = 0.007) were shown as predictive indicators of ACLD, while age, sex, side, TSS, CTFS, mPTA and mLDFA were not. A predictive model (risk score = -27.147 + [0.342*MWPPT%] + [0.282*HKA] + [0.684*PTS]) of ACLD using the three significant imaging indicators was constructed through multiple logistic regression analysis. The cut-off values of MWPPT%, HKA, PTS and the predictive model were 52.4% (sensitivity:92.3%; specificity:83.3%), 8.5° (sensitivity: 61.5%; specificity: 77.1%), 9.6° (sensitivity: 69.2%; specificity: 78.2%) and 0.1 (sensitivity: 96.2%; specificity: 79.2%) with the AUC (95%CI) values of 0.906 (0.829–0.983), 0.703 (0.574–0.832), 0.740 (0.621–0.860) and 0.949 (0.912–0.986) in the ROC curve.
Conclusion
MWPPT% (> 52.4%), PTS (> 9.6°), and HKA (> 8.5°) were found to be predictive factors for ACLD, and MWPPT% had the highest sensitivity of the three factors. Therefore, MWPPT% can be used as a screening tool, while the model can be used as a diagnostic tool.
Similar content being viewed by others
Introduction
Knee osteoarthritis (OA), one of the most common orthopedic diseases, often leads to pain, limited range of motion, and joint deformation [1, 2]. The incidence of the disease is increasing, thus bringing a huge burden to the medical health system with the aging of the population [2,3,4].
Uni-compartment knee arthroplasty (UKA) is a successful and reliable option for minimally invasive treatment of anteromedial osteoarthritis (AMOA), which can significantly improve functional recovery, kinematic alignment, and quality of life for patients [5,6,7]. However, strict compliance with surgical indications is a key factor in the success of UKA, especially the need to evaluate the functional integrity of the anterior cruciate ligament (ACL) before surgery [8, 9]. Functionally insufficient ACL often leads to failure of UKA surgery, and an ACL with functional integrity is a prerequisite for a successful medial UKA surgery [10,11,12,13]. In addition, bicruciate-retaining total knee arthroplasty (TKA) needs an ACL with functional integrity as well [14].
According to previous literature, there have been several radiographic signs related to the status of ACL, including the tibial wear pattern on lateral radiographs [15, 16], coronal tibiofemoral subluxation (CTFS) on anterior–posterior (AP) radiographs [17, 18], posterior tibial slope (PTS) on lateral radiographs [19, 20], and so on. However, the diagnostic accuracy of those radiographic signs varied in different pieces of literature, and related literature lacked the calculation of the cut-off value of those radiographic signs. In addition, there was no report on the prediction model of functional ACL deficiency that integrated multiple radiographic signs.
The purposes of this study were to investigate (1) the relationship between different radiographic signs and the functional status of ACL; (2) the accuracy of different radiographic signs for predicting functional deficiency of ACL; (3) whether the predictive model constructed by integrating multiple radiographic signs can improve the predictive ability. We hypothesized that these radiographic signs (the maximum wear point of the proximal tibia% (MWPPT%), PTS, and HKA) were predictive factors for the functional deficiency of ACL and a predictive model constructed by integrating those radiographic signs can improve the predictive ability.
Methods
This retrospective study was conducted using patients from January 1, 2018, to September 1, 2021, in China-Japan Friendship Hospital. The inclusion criteria were as follows: (1) patients undergoing uni-compartmental knee arthroplasty or total knee arthroplasty for varus knee with osteoarthritis; (2) patients with knee magnetic resonance imaging (MRI); (3) patients with standardized AP standing knee X-rays, lateral X-rays, and hip-to-ankle AP standing X-rays before knee surgery; (4) patients with the Lachman’s test records before surgery; (5) patients with consistent knee MRI evaluation and the Lachman’s test. The exclusion criteria were as follows:(1) patients with poor MRI or X-rays which can’t be used for research (n = 13); (2) patients with inflammatory arthropathy (n = 5); (3) patients with secondary OA (n = 2); (4) patients with neutral or valgus knees (n = 2); (5) patients with fractures around the knee (n = 1). A total number of 122 patients were enrolled in this study. The flow chart was shown in Fig. 1. All patients were evaluated preoperatively to assess ACL integrity with the Lachman’s test (an anterior force was applied to the tibia while the knee was flexed at 20° to 30°). The Lachman’s test was graded as 0–5 mm displacement and > 5 mm displacement, and we considered > 5 mm displacement as indicating ACL instability [21]. The study was approved by the institutional review board of the China-Japan Friendship Hospital (approval number 2020–50-k28).
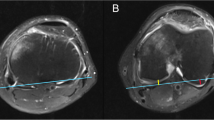
MRI assessment
All subjects underwent high-quality preoperative MRI using a GE Signa 1.5 T magnetic resonance imaging system (GE Company, USA). Patients were positioned in supine with the knee extended. The special coil for the knee joint was selected to perform routine serial scanning on the cross-section, sagittal plane, and coronal plane. The scanning parameters were SE-T1WI (TR = 540 ms, TE = 13 ms, 5 mm, FOV17 × 17) and FSE-T2WI (TR = 4500 ms, TE = 39.8 ms, 5 mm, FOV 17 × 17). The MRI was used to assess the status of ACL, graded as intact, with degenerative changes (including scarring, thinning, mucoid degeneration, ganglion formation, or partial tears) and completely torn [22, 23]. Based on the methods proposed by Boettner et.al. [15], the degenerative status can be further divided into functionally insufficient (< 14% posterior intact cartilage of the medial compartment) and functionally intact (> 14% posterior intact cartilage of the medial compartment) status. In this study, intact and degenerative (functionally intact) status (0–5 mm of displacement in the Lachman’s test at the same time) were classified as the ACL-functional (ACLF) group (functional integrity of ACL), while completely torn and degenerative (functionally insufficient) status (> 5 mm of displacement in the Lachman’s test at the same time) were regarded as the ACL-deficient (ACLD) group (functional deficiency of ACL). Of all patients, 96 patients were classified as the ACL-functional (ACLF) group, while 26 patients as the ACL-deficient (ACLD) group after the assessment of MRI and the Lachman’s test (Fig. 1). The status of ACL based on MRI was evaluated by two orthopedic surgeons using the hospital's imaging system (picture archiving and communication system, PACS), and the kappa’s coefficient was 0.915 (95%CI = 0.848 to 0.982), showing good interobserver reliability.
Radiographic assessment
Before surgery, all patients had standardized AP standing knee X-rays, lateral X-rays, and hip-to-ankle AP standing X-rays. These radiographic signs were measured using X-rays: MWPPT%, tibial spine sign (TSS), coronal tibiofemoral subluxation (CTFS), hip–knee–ankle angle (HKA), mechanical proximal tibial angle (mPTA), mechanical lateral distal femoral angle (mLDFA) and posterior tibial slope (PTS).
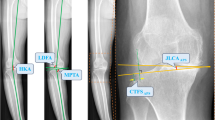
The AP standing knee X-rays were used to measure CTFS and TSS. CTFS was defined as the distance between the tangent line to the outermost joint edge of the lateral condyle of the femur and the tangent line of the lateral tibial plateau [18, 24] (Fig. 2). TSS included three types on the standardized AP standing knee X-rays: type0—no contact between the lateral condyle of the femur and the lateral intercondylar spine of the tibia, type1—contact between lateral condyle of the femur and lateral intercondylar spine of the tibia, type2 – the overlap of lateral condyle of the femur and lateral intercondylar spine of the tibia [25].
Measurement of Coronal tibiofemoral subluxation (CTFS) and the maximum wear point of the proximal tibia (MWPPT) a-c The anterior–posterior (AP) standing knee X-ray and lateral X-ray of an anterior cruciate ligament-deficient (ACLD) patient (a-c). CTFS is defined as the distance between the tangent line to the outermost joint edge of the lateral condyle of the femur and the tangent line of the lateral tibial plateau (a). The red arrow indicates the maximum wear point of the proximal tibia. MWPPT% is recorded as the ratio between the distance from the maximum wear point to the anterior edge of the tibia (yellow dotted line) and the length of the medial tibial plateau (green dotted line) (c)
The lateral X-rays were used to measure MWPPT% and PTS. MWPPT% was recorded as the ratio between the distance from the maximum wear point to the anterior edge of the tibia and the length of the medial tibial plateau [26, 27] (Fig. 2). PTS was the angle between the tibial anatomical axis (a straight line connecting the midpoint of the line at 5 cm and 15 cm from the knee joint line) and the tibial plateau (a line connecting the anterior and posterior points of the most proximal part of the tibial plateau) [28] (Fig. 3).
Measurement of different alignment parameters on hip-to-ankle anterior–posterior (AP) standing (a) and lateral (b) X-rays. Hip–knee–ankle angle (HKA) is the angle between the tibial mechanical axis and femoral mechanical axis, mechanical proximal tibial angle (mPTA) is the angle between the tangent of the medial and lateral tibial plateau and the mechanical axis of the tibia, and mechanical lateral distal femoral angle (mLDFA) is the angle between the tangent of the medial and lateral femoral condyle and the mechanical axis of the femur. Posterior tibial slope (PTS) is the angle between the tibial anatomical axis (a straight line connecting the midpoint of the line at 5 cm and 15 cm from the knee joint line) and tibial plateau (a line connecting the anterior and posterior points of the most proximal part of the tibial plateau)
On hip-to-ankle AP standing X-rays, HKA, mPTA, and mLDFA were measured (Fig. 3). HKA (recorded as a varus angle in our study) was the angle between the tibial mechanical axis and femoral mechanical axis, mPTA was the angle between the tangent of the medial and lateral tibial plateau and the mechanical axis of the tibia, and mLDFA was the angle between the tangent of the medial and lateral femoral condyle and the mechanical axis of the femur [29, 30].
All measurements were made by two orthopedic surgeons using the hospital's imaging system (PACS). Intra-class correlation coefficient (ICC) was used for continuous variables (MWPPT%, CTFS, PTS), while kappa’s coefficient was used for nominal variables (TSS) to test the interobserver reliability.
Statistical analysis
The continuous variables (age, MWPPT%, CTFS, HKA, mPTA, mLDFA, PTS) were presented as means and standard deviations (SD), while the categorical variables (sex, side, TSS) were given as frequencies and percentages (%).
The Shapiro–Wilk test was used to examine the normality of continuous variables. In univariate analysis between ACLF and ACLD groups, the independent-samples t-test or the Mann–Whitney U-test was used for continuous variables, while the Chi-square test or the Fisher’s exact test was used for categorical variables. Significant variables (p < 0.05) in univariate analysis were further analyzed using multiple logistic regression analysis to assess the predictive variables of ACLD and a predictive model of ACLD was constructed by multiple logistic regression analysis with generalized estimating models. Stepwise logistic regression analysis with backward elimination was performed according to the Akaike information criterion. Receiver operating characteristic (ROC) curves and area under the curve (AUC) were used to determine the cut-off value and the diagnostic accuracy of radiographic measurements and the logistic regression model.
Power analysis was performed in G-power (G*Power Version3.1.9, Germany) for the Mann–Whitney U test using an alpha of 0.05, a power of 80%, and an effect size of 0.5 resulting in a sample size of 106. We included a total of 122 patients in the study.
All statistical analyses were performed using SPSS24.0 (IBM, New York, USA), and a p < 0.05 (two-sides) was considered statistically significant.
Results
Subject characteristics
A total of 122 patients were enrolled in the study. The mean ± SD of age was 66.82 ± 8.40. The mean ± SD of MWPPT%, CTFS, HKA, mLDFA, mPTA, and PTS were 49.96 ± 6.41, 5.17 ± 1.47, 7.66 ± 3.81, 89.32 ± 2.16, 85.68 ± 2.08 and 8.98 ± 1.97. Of all patients, 21 patients were male and 101 patients were female; 61 patients had surgery on the left knee, while the others (61 patients) on the right knee; 76 patients were classified as type 0 of tibial spine sign, 20 patients as type 1 and 26 patients as type 2 (Table 1). All patients were divided into two groups, ACLF (n = 96) and ACLD (n = 26), and the demographic characteristics of each group were presented in Table 1. The ICCs (95%CI) of imaging indicators (MWPPT%, CTFS, and PTS) were 0.853 (0.796–0.895), 0.846 (0.787–0.890) and 0.807 (0.734–0.861), and the κ (95%CI) of imaging indicator (TSS) was 0.910 (0.841–0.979), all showing good interobserver reliability (Table 2).
Univariate analysis
In univariate analysis, there was no significant difference in these variables (age, sex, side, TSS, mLDFA, mPTA) between the ACLF group and ACLD group, but significant differences were found in MWPPT% (ACLF: 47.83 ± 4.69 < ACLD: 57.83 ± 5.93, p < 0.001), CTFS (ACLF: 4.91 ± 1.24 < ACLD: 6.13 ± 1.89, p = 0.003), HKA (ACLF: 6.94 ± 3.07 < ACLD: 10.34 ± 5.03, p = 0.003) and PTS (ACLF: 8.62 ± 1.90 < ACLD: 10.28 ± 1.73, p < 0.001) (Table 1).
Multiple logistic regression analysis and the predictive model construction
The significant variables (MWPPT%, CTFS, HKA and PTS) in univariate analysis were further analyzed by multiple logistic regression analysis. The three variables, including MWPPT% (OR = 1.383, 95%CI = 1.193–1.603, and p < 0.001), HKA (OR = 1.326, 95%CI = 1.051–1.673, and p = 0.017) and PTS (OR = 1.981, 95%CI = 1.207–3.253, and p = 0.007), were expressed as the predictive variables of ACLD in the multiple logistic regression analysis. Through multiple logistic regression analysis, a predictive model (with percentage accuracy in classification of 89.3%) was also constructed using the three significant imaging indicators: risk score = -27.147 + [0.342*MWPPT%] + [0.282*HKA] + [0.684*PTS] (Table 3).
Comparison of the ROC curves for radiographic measurements and logistic regression model
In the ROC curves of significant variables (MWPPT%, HKA and PTS) in logistic regression analysis, the cut-off values were 52.4%, 8.5° and 9.6° with the AUC (95% CI) values of 0.906 (0.829–0.983), 0.703 (0.574–0.832) and 0.740 (0.621–0.860). The sensitivity of MWPPT%, HKA, and PTS were 92.3%, 61.5% and 69.2%, while the specificity of these indicators were 83.3%,77.1% and 78.2% (Table 4 and Fig. 4).
The receiver operating characteristic (ROC) curve for MWPPT%, HKA, PTS, and predictive model. The area under the curve (AUC) was 0.906(0.829–0.983) for MWPPT%, 0.703(0.574–0.832) for HKA, 0.740(0.621–0.860) for PTS and 0.949(0.912–0.986) for predictive model (95%CI). MWPPT%, the maximum wear point of the proximal tibia%; HKA, Hip–knee–ankle angle; PTS, posterior tibial slope; CI, confidence interval
For the predictive model (risk score = -27.147 + [0.342*MWPPT%] + [0.282*HKA] + [0.684*PTS]), the cut-off value of the risk score was 0.1 and the AUC (95% CI) was 0.949 (0.912–0.986) in the ROC curve. In addition, the sensitivity and specificity of the model were 96.2% and 79.2% when predicting ACLD (Table 4 and Fig. 4).
Discussion
Our research found that the three imaging indicators, including MWPPT%, HKA, and PTS, were predictors of ACLD, and the cut-off values of the three indicators were calculated with the accuracy (AUC value), sensitivity, and specificity values. We further built a prediction model that combined the above three indicators to further improve the accuracy of the prediction of ACLD. It was worth mentioning that MWPPT% had the highest sensitivity of the three indicators. Therefore, MWPPT% can be used to screen for ACLD, and the model constructed in the study can be further used as a diagnostic tool to determine the status of ACL.
As we all know, the surgical indications for medial UKA include the following two points:(1) anteromedial osteoarthritis (AMOA) confirmed using the radiological examination. (2) knee joint stability, which means medial and lateral collateral ligaments, and anterior and posterior cruciate ligament are intact [8, 9]. For patients who are preparing for UKA surgery, it is extremely important to assess the status of the patient's ACL before surgery. The insufficient function of ACL often leads to failure of UKA surgery, and an ACL with functional integrity is a prerequisite for a successful medial UKA surgery [10,11,12]. In addition, bicruciate-retaining TKA also needs ACL with functional integrity [14]. However, the intact ACL through preoperative physical examination can sometimes be found to be damaged or even broken during the operation, and not all patients preparing for UKA or bicruciate-retaining TKA have preoperative MRI [21, 31]. Therefore, it is meaningful to find a preoperative radiographic method with high accuracy for ACL functional status assessment.
Our study revealed that the three imaging indicators, including MWPPT%, PTS, and HKA, were predictors of ACLD. MWPPT%-The known Keyes classification used the lateral radiograph to assess the status of ACL and graded the ACL based on the tibia wear pattern on the lateral radiograph [16]. Many studies have shown that there was a correlation between the tibia wear pattern on the lateral radiograph and the status of the ACL [15, 27, 32]. When the status of ACL changed from intact ACL to functionally deficient ACL, the location of tibia wear on the lateral radiograph moved from anterior to posterior tibial plateau. However, those studies only described the phenomenon qualitatively, not quantitatively. In our study, we quantified the tibia wear pattern on the lateral radiograph using MWPPT% and we found that MWPPT% of 52.4% was the cut-off value to predict the ACLD with a sensitivity of 92.3% and a specificity of 83.3% (AUC value: 0.906) (Table 4). It was worth mentioning that this study is the first to quantify the wear of the tibia pattern on the lateral radiograph to predict ACLD using the Asian population. PTS-It has been reported in the literature that there was a correlation between PTS and ACL damage [19, 20, 33]. The larger the PTS, the more easily the ACL was damaged. However, related research was limited to the relationship between non-contact ACL deficiency and PTS in young people, not contact ACL deficiency in the elderly. Recently, in a study of elderly people undergoing UKA surgery, Plancher et.al. [20] found that patients with ACL deficiency had greater preoperative PTS than patients with intact ACL (7.6 ± 2.8° > 5.4 ± 5.9°, p = 0.001). In our study, we found a similar result that patients with functional ACL deficiency have larger preoperative PTS (ACLD: 10.28 ± 1.73° > ACLF 8.62 ± 1.90°, p < 0.001) (Table 1). The different values in the two studies might due to the variety of race and measurement methods. Further, we calculated the cut-off value (9.6°) of PTS with the corresponding sensitivity (69.2%), specificity (78.2%), and AUC (0.740), which showed that PTS was a good predictor of contact ACLD in the elderly (Table 4). HKA-Mullaji et.al. [32] and Springer et.al [18]. reported that patients with functionally deficient ACL had a greater varus angle than patients with functionally integral ACL. We had a similar result. In our research, we found that HKA in the ACLD group was larger than that in the ACLF group (ACLF: 6.94 ± 3.07 < ACLD: 10.34 ± 5.03, p = 0.003) (Table 1). These results might be explained by the following theory: functionally deficient ACL could lead to the relaxation of the anterior part of the knee joint, which further led to knee osteoarthritis and varus deformities [34]. Moreover, we calculated the cut-off value of HKA (8.5°) with the sensitivity and specificity of 61.5% and 77.1% when predicting ACLD (Table 4). As the varus angle was only required to be less than 15° in a surgical indication of medial UKA, more attention needed to be paid to the functional integrity of ACL for patients with varus angles greater than 8.5° preoperatively [8].
Previous studies have reported the relationship between intraoperative findings of ACL and preoperative evaluations with physical examination, radiographs, or MRI [15, 21, 35]. Waldstein et.al. [15] reported that patients with > 14% posterior intact cartilage of the medial compartment (assessed by MRI) were more likely to have a functionally intact ACL. Tao et.al. [35] found that an axial global passive anterior tibial subluxation (PATS) (> 1.2 mm) on MRI could be used as a predictive factor for a functionally deficient ACL, with the AUC, sensitivity, and specificity values of 0.897, 55% and 100%. Johnson et.al. [21] found that the preoperative Lachman test together with MRI could provide a sensitivity of 93.3% and a specificity of 99% for assessing the ACL status intraoperatively. In our study, the preoperative Lachman test together with MRI was used to determine the status of the ACL, and a predictive model of ACLD was constructed by using three radiographic indicators (MWPPT%, PTS, and HKA). It was worth mentioning that the predictive model in our study had a higher accuracy (AUC = 0.949) than the predictive index (AUC = 0.897) of Tao et.al. [35], and higher sensitivity (96.2%) than the predictive index (55.0% and 93.3%) of Tao et.al. [35] and Johnson et.al. [21]. In clinical practice, the use of a single radiographic indicator to assess the status of ACL had great uncertainty, while a model constructed using multiple indicators could greatly improve the accuracy. At present, there have been many models with multiple indicators showing high predictive accuracy in other fields [36,37,38]. As far as we knew, this was the first study combining multiple imaging indicators to construct an ACLD prediction model. The prediction model in our study had high accuracy (AUC = 0.949) in predicting ACLD than that of the single radiographic indicators, MWPPT% (AUC = 0.906), PTS (AUC = 0.740), and HKA (AUC = 0.703), and could be used as a diagnostic tool of ACLD. As the predictive model in our study could determine the functional status of ACL through X-rays with high accuracy (AUC = 0.949), it had certain applicable value in clinical practice, for example, determining whether further evaluation (such as MRI) was needed and whether the surgical plan should be changed.
Our study had its limitations. First, the study was a single-center, retrospective clinical study. A multi-center and prospective clinical study is needed in the future. Second, the prediction model in this study had not been verified. Therefore, the model needs to be verified later, and the result of external verification is more reliable. Third, this retrospective study lacked the intraoperative data to judge the ACL status. However, all the subjects included in the study had MRI and the Lachman’s test record, and the ACL state was judged using MRI and the Lachman’s test. Fourth, considering the rotation of patients' lower limbs and the difference in alignments, it was difficult to obtain accurate X-rays of all patients, which might affect the accuracy and repeatability of the radiographic measurements. However, the interobserver reliability of imaging indicators in this study showed good consistency in radiographic measurements.
Conclusion
In this study, MWPPT% (> 52.4%), PTS (> 9.6°), and HKA (> 8.5°) were found to be predictive factors for ACLD and MWPPT% had the highest sensitivity of the three factors. Therefore, MWPPT% can be used as a screening tool and the model can be used as a diagnostic tool to help clinicians better judge the functional status of ACL through X-rays.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ACLF:
-
Anterior cruciate ligament-functional
- ACLD:
-
Anterior cruciate ligament-deficient
- MRI:
-
Magnetic resonance imaging
- MWPPT:
-
Maximum wear point of the proximal tibia
- TSS:
-
Tibial spine sign
- CTFS:
-
Coronal tibiofemoral subluxation
- HKA:
-
Hip–knee–ankle angle
- mPTA:
-
Mechanical proximal tibial angle
- mLDFA:
-
Mechanical lateral distal femoral angle
- PTS:
-
Posterior tibial slope
- ROC:
-
Receiver-operating-characteristic
- AUC:
-
Area under the curve
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- OA:
-
Osteoarthritis
- UKA:
-
Uni-compartment knee arthroplasty
- AMOA:
-
Anteromedial osteoarthritis
- TKA:
-
Total knee arthroplasty
- AP:
-
Anterior–posterior
- PACS:
-
Picture archiving and communication system
- ICC:
-
Intra-class correlation coefficient
- SD:
-
Standard deviations
References
Glyn-Jones S, Palmer AJ, Agricola R, Price AJ, Vincent TL, Weinans H, et al. Osteoarthritis Lancet. 2015;386:376–87.
Mandl LA. Osteoarthritis year in review 2018: clinical. Osteoarthritis Cartilage. 2019;27:359–64.
Di Matteo B, Murrell WD, Görtz S, Kon E. Osteoarthritis: an ancient disease, an unsolved conundrum. Int Orthop. 2021;45:313–7.
Bortoluzzi A, Furini F, Scirè CA. Osteoarthritis and its management - epidemiology, nutritional aspects and environmental factors. Autoimmun Rev. 2018;17:1097–104.
Walker T, Hetto P, Bruckner T, Gotterbarm T, Merle C, Panzram B, et al. Minimally invasive Oxford unicompartmental knee arthroplasty ensures excellent functional outcome and high survivorship in the long term. Knee Surg Sports Traumatol Arthrosc. 2019;27:1658–64.
Price AJ, Dodd CA, Svard UG, Murray DW. Oxford medial unicompartmental knee arthroplasty in patients younger and older than 60 years of age. J Bone Joint Surg Br. 2005;87:1488–92.
Li Z, Chen Z, Wei J, Zeng X, Sun H, Li Z, et al. Excellent outcomes with Oxford Uni-compartmental knee arthroplasty in anteromedial osteoarthritis patients (≤60 years) at mid-term follow-up. BMC Musculoskelet Disord. 2021;22:859.
Crawford DA, Berend KR, Thienpont E. Unicompartmental knee arthroplasty: US and global perspectives. Orthop Clin North Am. 2020;51:147–59.
Antoniadis A, Dimitriou D, Canciani JP, Helmy N. A novel preoperative scoring system for the indication of unicompartmental knee arthroplasty, as predictor of clinical outcome and satisfaction. Arch Orthop Trauma Surg. 2019;139:113–20.
Goodfellow J, O’Connor J. The anterior cruciate ligament in knee arthroplasty. A risk-factor with unconstrained meniscal prostheses. Clin Orthop Relat Res. 1992;276:245–52.
Hamilton TW, Pistritto C, Jenkins C, Mellon SJ, Dodd CA, Pandit HG, et al. Unicompartmental knee replacement: does the macroscopic status of the anterior cruciate ligament affect outcome? Knee. 2016;23:506–10.
Engh GA, Ammeen DJ. Unicondylar arthroplasty in knees with deficient anterior cruciate ligaments. Clin Orthop Relat Res. 2014;472:73–7.
Goodfellow JW, Kershaw CJ, Benson MK, O’Connor JJ. The Oxford Knee for unicompartmental osteoarthritis. The first 103 cases. J Bone Joint Surg Br. 1988;70:692–701.
Singh V, Yeroushalmi D, Christensen TH, Bieganowski T, Tang A, Schwarzkopf R. Early outcomes of a novel bicruciate-retaining knee system: a 2-year minimum retrospective cohort study. Arch Orthop Trauma Surg. 2022. Online ahead of print.
Waldstein W, Merle C, Monsef JB, Boettner F. Varus knee osteoarthritis: how can we identify ACL insufficiency? Knee Surg Sports Traumatol Arthrosc. 2015;23:2178–84.
Keyes GW, Carr AJ, Miller RK, Goodfellow JW. The radiographic classification of medial gonarthrosis. Correlation with operation methods in 200 knees. Acta Orthop Scand. 1992;63:497–501.
Khamaisy S, Zuiderbaan HA, Thein R, Gladnick BP, Pearle AD. Coronal tibiofemoral subluxation in knee osteoarthritis. Skeletal Radiol. 2016;45:57–61.
Springer B, Waldstein W, Bechler U, Jungwirth-Weinberger A, Windhager R, Boettner F. The functional status of the ACL in Varus OA of the knee: the association with varus deformity and coronal tibiofemoral subluxation. J Arthroplasty. 2021;36:501–6.
Ni QK, Song GY, Zhang ZJ, Zheng T, Feng Z, Cao YW, et al. Steep posterior tibial slope and excessive anterior tibial translation are predictive risk factors of primary anterior cruciate ligament reconstruction failure: a case-control study with prospectively collected data. Am J Sports Med. 2020;48:2954–61.
Plancher KD, Shanmugam JP, Brite JE, Briggs KK, Petterson SC. Relevance of the tibial slope on functional outcomes in ACL-deficient and ACL intact fixed-bearing medial unicompartmental knee arthroplasty. J Arthroplasty. 2021;36:3123–30.
Johnson AJ, Howell SM, Costa CR, Mont MA. The ACL in the arthritic knee: how often is it present and can preoperative tests predict its presence? Clin Orthop Relat Res. 2013;471:181–8.
Hovis KK, Alizai H, Tham SC, Souza RB, Nevitt MC, McCulloch CE, et al. Non-traumatic anterior cruciate ligament abnormalities and their relationship to osteoarthritis using morphological grading and cartilage T2 relaxation times: data from the Osteoarthritis Initiative (OAI). Skeletal Radiol. 2012;41:1435–43.
Van Dyck P, De Smet E, Veryser J, Lambrecht V, Gielen JL, Vanhoenacker FM, et al. Partial tear of the anterior cruciate ligament of the knee: injury patterns on MR imaging. Knee Surg Sports Traumatol Arthrosc. 2012;20:256–61.
Greif DN, Epstein AL, Hodgens BH, Jose J, Baraga MG. Current measurement strategies of coronal tibiofemoral subluxation: a systematic review of literature. AJR Am J Roentgenol. 2021;216:1183–92.
Boettner F, Springer B, Windhager R, Waldstein W. The tibial spine sign does not indicate cartilage damage in the central area of the distal lateral femoral condyle. Knee Surg Sports Traumatol Arthrosc. 2020;28:2592–7.
Ahlbäck S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh). 1968;277:7–72.
Scott CEH, Holland G, Krahelski O, Murray IR, Keating JF, Keenan OJF. Patterns of cartilage loss and anterior cruciate ligament status in end-stage osteoarthritis of the knee. Bone Joint J. 2020;102-b:716–26.
Utzschneider S, Goettinger M, Weber P, Horng A, Glaser C, Jansson V, et al. Development and validation of a new method for the radiologic measurement of the tibial slope. Knee Surg Sports Traumatol Arthrosc. 2011;19:1643–8.
Hazratwala K, O’Callaghan WB, Dhariwal S, Wilkinson MPR. Wide variation in tibial slopes and trochlear angles in the arthritic knee: a CT evaluation of 4116 pre-operative knees. Knee Surg Sports Traumatol Arthrosc. 2021. Online ahead of print.
Gielis WP, Rayegan H, Arbabi V, Ahmadi Brooghani SY, Lindner C, Cootes TF, et al. Predicting the mechanical hip-knee-ankle angle accurately from standard knee radiographs: a cross-validation experiment in 100 patients. Acta Orthop. 2020;91:732–7.
Leblanc MC, Kowalczuk M, Andruszkiewicz N, Simunovic N, Farrokhyar F, Turnbull TL, et al. Diagnostic accuracy of physical examination for anterior knee instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:2805–13.
Mullaji AB, Marawar SV, Luthra M. Tibial articular cartilage wear in varus osteoarthritic knees: correlation with anterior cruciate ligament integrity and severity of deformity. J Arthroplasty. 2008;23:128–35.
Li R, Yuan X, Fang Z, Liu Y, Chen X, Zhang J. A decreased ratio of height of lateral femoral condyle to anteroposterior diameter is a risk factor for anterior cruciate ligament rupture. BMC Musculoskelet Disord. 2020;21:402.
Cantin O, Magnussen RA, Corbi F, Servien E, Neyret P, Lustig S. The role of high tibial osteotomy in the treatment of knee laxity: a comprehensive review. Knee Surg Sports Traumatol Arthrosc. 2015;23:3026–37.
Tao Y, Tang S, Zhao P, Yan W, Zhou A, Zhang J. Value of passive anterior tibial subluxation on axial MRI in identifying anterior cruciate ligament functional deficiency in patients with advanced anteromedial osteoarthritis of the knee: a case-control study. BMC Musculoskelet Disord. 2021;22:434.
Park YB, Kim SH, Ha CW, Han JW, Noh JW. A predictive model with radiographic signs can be a useful supplementary diagnostic tool for complete discoid lateral meniscus in adults. Knee Surg Sports Traumatol Arthrosc. 2021;29:474–82.
Ha CW, Kim SH, Lee DH, Kim H, Park YB. Predictive validity of radiographic signs of complete discoid lateral meniscus in children using machine learning techniques. J Orthop Res. 2020;38:1279–88.
Dong S, Li W, Tang ZR, Wang H, Pei H, Yuan B. Development and validation of a novel predictive model and web calculator for evaluating transfusion risk after spinal fusion for spinal tuberculosis: a retrospective cohort study. BMC Musculoskelet Disord. 2021;22:825.
Acknowledgements
Not applicable.
Funding
This study was funded by the Capital Health Research and Development of Special (grant number 2020–2-4067), National Natural Science Foundation of China (grant number 82072494,81972130), Elite Medical Professionals project of China-Japan Friendship Hospital (grant number ZRJY2021-GG08), and Natural Science Foundation of Beijing Municipal (grant number 7202183). The funding was used for data collection, analysis, and publication of articles.
Author information
Authors and Affiliations
Contributions
CQL, QDZ, and WSG designed the study. CQL, JCG, and CH did the data collection. CQL and JCG did the data analysis. CQL wrote the article. WGW, QDZ, and WSG revised the article. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the institutional review board of China-Japan Friendship Hospital (approval number 2020–50-k28). Informed written consent was provided by every participant.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, C., Ge, J., Huang, C. et al. A radiographic model predicting the status of the anterior cruciate ligament in varus knee with osteoarthritis. BMC Musculoskelet Disord 23, 603 (2022). https://doi.org/10.1186/s12891-022-05568-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05568-3