Abstract
Background and study aims
Multiple surgical approaches have been studied and accepted for the removal of highly downward migrated lumbar disc herniation (LDH). Here, we investigated the efficacy and safety of full-endoscopic foraminoplasty for highly downward migrated LDH.
Patients and methods
Thirty-seven patients with highly down-migrated LDH treated by the full-endoscopic foraminoplasty between January 2018 and January 2020 were retrospectively investigated. Clinical parameters were evaluated preoperatively and 1, 6, and 12 months postoperatively, using pre- and post-operative Oswestry Disability Index (ODI) scores for functional improvement, visual analog scale (VAS) for leg and back pain, and modified MacNab criteria for patients satisfactory.
Results
Thirty-seven patients with highly downward migrated LDH were successfully removed via the transforaminal full-endoscopic discectomy. The average VAS back and leg pain scores were significantly reduced from 7.41 ± 1.17 and 8.68 ± 1.06 before operation to 3.14 ± 0.89 and 2.70 ± 0.46 at postoperative 1 month, and 1.76 ± 0.59 and 0.92 ± 0.28 at postoperative 12 months, respectively (P < 0.05). The average ODI scores were reduced from 92.86 ± 6.41 to 15.30 ± 4.43 at postoperative 1 month, and 9.81 ± 3.24 at postoperative 12 months (P < 0.05). Based on the modifed MacNab criteria, 36 out of 37 patients (97.30%) were rated as excellent or good outcomes.
Conclusion
The full-endoscopic foraminoplasty can be used successfully for surgical removal of high grade down-migrated LDH, and it could serve as an efficient alternative technique for patients with highly downward migrated LDH.
Similar content being viewed by others
Introduction
Lumbar disc herniation (LDH), extending beyond the inferior or superior margin of the intervertebral disc in downward or upward direction, was generally described as disc migration [1, 2]. According to the Lee’s classification depending on the distance from the disc space, the extent of down-migrated disc was classified into two zones: near-downward and far-downward [1]. Typically, patients with the compression of the dural sac or nerve roots will progress to the potential neurological symptoms, which adversely affect the quality of patients’ daily life [3, 4].
Several endoscopic discectomy techniques that achieve satisfying clinical results with less trauma have been extensively researched and used for LDH [4,5,6,7]. Despite the popularity of endoscopic discectomy techniques, the value of the full-endoscopic foraminoplasty for surgical removal of highly downward migrated LDH has yet to be well-demonstrated.
As the concept of endoscopic technique has been shifted from intra-discal decompression to adjustable alternative decompression, full-endoscopic discectomy for LDH has been developed and extensively used [6, 8, 9]. We therefore investigated the efficacy and safety of full-endoscopic foraminoplasty for highly downward migrated LDH.
Patients and methods
Ethics committee approval and informed consent for each patient were obtained in this series.
Patient population
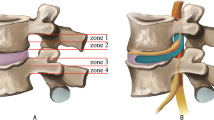
Between January 2018 and January 2020, 37 consecutive cases with highly downward migrated LDH were retrospectively investigated and included in the present study. Of them, herniations extending beyond the height of the posterior margin of the disc are defined as high-grade downward migrations [1, 10]. Herniations extending beyond the inferior margin of the pedicle are defined as very high-grade downward migrations [5]. The full-endoscopic foraminoplasty under local anesthesia was conducted for surgical removal of highly down-migrated LDH by the experienced spine surgeon. The schematic representation of the levels of herniation and 3 zones was presented in the Fig. 1.
The extent of down-migrated disc: Zone 1, low-grade downward: herniations within the height of the posterior margin of the disc in downward direction; Zone 2, high-grade downward: herniations extending beyond the height of the posterior margin of the disc in downward direction; Zone 3, very high-grade downward: herniations extending beyond the inferior margin of lower pedicle
The eligibility criteria were as follows: radiating pain and numbness in the unilateral lower extremity; single-level highly down-migrated LDH verified by imageology examination; patients’ clinical symptoms in accordance with imageology detection; ineffectual conservative treatment for at least 12 weeks, except for the patient was in severe pain that affected their daily life; and no surgical history at the same level. The exclusion criteria included non-downward migrated LDH, lumbar spinal stenosis, multiple level LDH, lumbar instability, and lumbar spinal infection or tumor.
Surgical technique
The patients were adjusted to prone position with a soft cushion under their abdomen. Based on the C-arm fluoroscopy, the body surface projection line of the target segment and the spinous process midline, as well as the puncture route were marked on the patient’s back. The surgical procedure under local anesthesia was performed for all patients. The puncture route on the lateral fluoroscopic view was set from the apex of the upper articular process to the posterior upper margin of the inferior vertebral body. Then, an 18-gauge needle was slowly advanced to the superolateral region of the superior articular process (Fig. 2a-b). The skin entry point was slightly located at upper margin of the disc level, making an angle of approximately 10–30° with the superior articular process. During the puncture pathway, the skin entry point, subcutaneous tissue, and peripheral facet joint were infiltrated for anesthesia with the mixture of lidocaine and ropivacaine. After the precise location of the needle was confirmed by C-arm fluoroscopy, the needle core was pulled out and the guide wire was inserted.
a Anteroposterior (AP) fluoroscopic view showing the needle tip located at the exterior margin of the superior articular process. b Lateral fluoroscopic view showing the needle tip located at the tip of the superior articular process. c AP view showing the working cannula located at the exterior margin of the superior articular process. d Lateral fluoroscopic view showing the working cannula located at the tip of the superior articular process
Subsequently, an about 7 mm incision, approximately 8–12 cm off the midline on the line of the puncture route, was made. Following a staged dilation along the guide wire, the working cannula (8.4 mm) (Fig. 2c-d) and endoscopic trephine (7.5 mm) (Fig. 3a) (Guanlong, Shandong, China) was placed, which were located at the exterior margin of the superior articular process from anteroposterior view and at the tip of the superior articular process from lateral fluoroscopic view. Then, the 30-degree endoscope (6.3 mm) (Joimax, Karlsruhe, Germany) was introduced and inserted into the working cannula. Under endoscopic direct vision, the soft tissue around the peripheral facet joint was ablated by the bipolar radiofrequency electrode (Guanlong, Shandong, China), and the ventral superior articular process was partially resected to enlarge the intervertebral foramen, using the endoscopic trephine (Fig. 3b). The working cannula and endoscope were further pushed toward the lumbar canal, and the ligamentum flavum was directly identified and then removed with the use of the endoscopic forceps. At this point, the traversing nerve root, squeezed by the annulus fibrosus, was observed. The dense adhesions between fibrous anchoring tissues and nerve root were released with bipolar radiofrequency electrode.
Surgical procedures of highly downward-migrated disc removal. a Placement of the endoscopic trephine; b The ventral superior articular process was partially resected using the endoscopic trephine; c The working cannula was directed downward to create an angle of a cranial-to-caudal approach; d The endoscopic forceps were scrupulously used to remove high grade down-migrated mass
In order to provide a sufficient decompression of the traversing nerve root, full-endoscopic discectomy under continuous visualization was preliminarily performed. Once the release of intra-discal and epidural space is sufficient, the highly down-migrated fragments can be detected clearly, and the epidural operating space can be achieved for endoscopic instruments. Subsequently, the working cannula was directed downward to create an angle of a cranial-to-caudal approach (Fig. 3c). Thereafter, endoscopic forceps were scrupulously used to remove high grade down-migrated mass (Fig. 3d). Following a careful endoscopic exploration, thorough decompression was confirmed when the traversing nerve root was repeatedly seen moving freely via the Valsalva maneuver. After active bleeding was controlled with the use of bipolar radiofrequency electrode, the endoscope with the working cannula was dislodged, and a piece of sterile dressing was placed on the stitched incision.
Clinical evaluation
Data for baseline characteristics and perioperative variables were recorded. Leg and back pain were evaluated using visual analog scale (VAS) [11] (range, 0–10) and neurologic function were evaluated using Oswestry disability index score (ODI) [12] (range, 0–100). Patient’s satisfaction was concurrently assessed on the basis of the modified MacNab criteria [7, 13]. Clinical parameters were scheduled preoperatively and 1, 6, and 12 months postoperatively.
Statistical analysis
Enumeration and quantitative data, respectively, were descriptively presented as percentage and mean (standard deviation). The clinical outcomes, based on the modified MacNab criteria, were categorized as excellent, good, fair, and poor. The difference in terms of pre- and post-operative VAS or ODI scores at different time points was calculated statistically by repeated measures analysis of variance. Statistical analyses for collected data were calculated with the assistance of IBM SPSS Statistics 20. P value less than 0.05 indicates a statistical difference.
Results
Base demographic and clinical characteristics
21 cases with highly down-migrated and 16 cases with very highly down-migrated were included. This series included three cases located at L2/3, three cases at L3/4, fifteen cases at L4/5, and sixteen cases at L5/S1. There were 12 females and 25 males. The age ranged from 30 to 63 years, with a mean of 46.43 ± 9.15 years. During surgery, the blood loss was not measured in these patients. The average fluoroscopy time and operation time were 6.03 ± 1.91 times and 92.70 ± 24.07 min, respectively. The mean hospitalization time was 6.27 ± 2.07 days. The patient-related information was recorded and summarized in Table 1.
Clinical outcomes
Pain measurement
Detailed results of clinical outcomes were present in Table 2. Thirty-seven patients with highly downward migrated LDH were successfully removed. All patients’ back and leg pain was relieved after operation. The average VAS back pain scores had reduced significantly, from 7.41 ± 1.17 before operation to 3.14 ± 0.89 at postoperative 1 month, 2.59 ± 0.69 at postoperative 6 months, and 1.76 ± 0.59 at postoperative 12 months (P < 0.05), as shown in supplementary Fig. 1. Similarly, the average VAS leg pain scores had also reduced significantly, from 8.68 ± 1.06 before operation to 2.70 ± 0.46 at postoperative 1 month, 1.81 ± 0.46 at postoperative 6 months, and 0.92 ± 0.28 at postoperative 12 months (P < 0.05), as shown in Supplementary Fig. 2.
Assessment of disability
As for neurological function, the average ODI scores had reduced significantly, from 92.86 ± 6.41 before operation to 15.30 ± 4.43 at postoperative 1 month, 12.03 ± 3.75 at postoperative 6 months, and 9.81 ± 3.24 at postoperative 12 months (P < 0.05), as shown in supplementary Fig. 3. Based on the modifed MacNab criteria, 36 out of 37 patients (97.30%) were rated as excellent or good outcomes, as shown in Table 3.
Complications
Lumbar radicular pain at the same segment was observed in one patient at 3 days postoperatively, which was successfully relieved via a second transforaminal full-endoscopic discectomy. Additionally, four patients had early postoperative dysesthesia of the traversing root that was satisfactorily resolved with neurotrophic drugs for 2 weeks. No occurrence of nerve root injury or dura tear was observed.
Illustrative case
Figure 4 presented the preoperative, postoperative images and intraoperative fluoroscopic views of a thirty-four-year-old man who was treated with full-endoscopic foraminoplasty. An illustrative case of the highly down-migrated disc was presented in Fig. 5a-d, and the very highly down-migrated disc in Figs. 6a-d and 7a-f.
Thirty-four-year-old man with highly downward-migrated LDH, whose complaint was low back and left lower limb pain. The full-endoscopic foraminoplasty was performed. a Preoperative sagittal and axial T2 MRI showing a highly down-migrated disc from L5 to S1. b The needle tip located at the exterior margin and tip of the superior articular process. c The working cannula located at the exterior margin and tip of the superior articular process. d The ventral superior articular process was partially resected using the endoscopic trephine. e Thorough decompression was obtained. f Postoperative sagittal and axial T2 MRI showing successful surgical removal of the downward migrated fragments
Discussion
Downward migrated LDH is sometimes discontinuous and sequestrated from the origin intervertebral disc, and it is generally fragmented into small pieces [2, 5, 14]. The posterior longitudinal ligament can be breached by the disc migrated sequestrations, which can drift cranially or caudally into the anterior epidural space, with an estimated prevalence of 35 to 70% [15, 16]. Conventionally, the removal of these highly down-migrated sequestrations via the traditional surgical approaches requires extensive soft tissue dissection, even at the cost of sacrificing part of the lamina and facet joints, which may result in potential lumbar instability and associated complications [17, 18]. Thus, in order to minimize the possibility of iatrogenic lumbar instability, an experienced surgeon may create a bony opening through the lamina [18, 19]. Nevertheless, it is difficult to reach and remove thoroughly these migrated fragments, since some sequestrations around the corner cannot completely be examined.
Specifically, several surgical approaches have been developed to easily get through the sequestrated LDH. In 2008, Choi et al. [20] conducted a retrospective analysis of 59 patients with highly migrated intracanal disc herniations who underwent percutaneous endoscopic approach using foraminoplastic technique, and found that the outcomes of foraminoplastic-PELD were comparable to those of conventional open procedures. Also, the author described patients with highly downward migrated LDH had superior outcomes compared with cases with highly downward migrated LDH. Kim et al. [5] in 2012 investigated surgical outcomes of interlaminar PELD for highly migrated LDH in 18 patients. The disc sequestrations were migrated inferiorly in 11 cases and superiorly in 7 cases. Of them, 12 patients had excellent outcomes in 66.67% of cases, good in 3 patients. But in one case, dural tear without cerebrospinal fluid leakage was suspected. Lin et al. [21] described their experience with accessing a highly migrated LDH using full endoscopic technique via a translaminar keyhole approach in 13 patients. Although these patients presented with highly upward disc migration and only two cases located at L5/S1, the satisfactory outcomes were observed in 92.3% of cases, which was consistent with our results. The difference was that the patients in our series were with a younger average age.
Nonetheless, the full-endoscopic foraminoplasty has not yet been well clarified as an effective removal for high-grade downward migrated LDH. Our experience in the present series demonstrates an effective and safe procedure for achieving majority removal of a highly downward migrated LDH in our patients. The clinical findings reveal that the effectiveness with respect to pain subsides, perioperative parameters, and neurological functional recovery was similar to those achieved with aforementioned approaches, which efficiently avoid an open limited incision, significant soft tissue dissection, and irreversible bony destruction. In terms of safety, the entire surgical procedure was performed under direct vision, which has the advantages of smaller wounds and less bleeding, and has the potential to decrease the likelihood of nerve damage and maximize rehabilitation potential with faster resumption of activities while minimizing hospitalization time. Ruetten et al. analyzed a series of cases who underwent interlaminar PELD, and found that 2% of the patients had nerve damage [22]. Fortunately, the retraction injury that can happen in posterior surgery was not observed in our series.
Technically, the full-endoscopic foraminoplasty can directly access initial site of a herniated disc and reach highly down-migrated fragments through adjusting the working cannula, possibly indicating it can be used as an alternative to traditional open discectomy since it is not restricted by the high iliac crest. Moreover, the area of operative exploration is very bright illumination and fully visualized, since the endoscope provides clearly high-resolution image under direct vision. It creates favorable conditions to avoid nerve damage and remove the migrated disc as completely as possible. Importantly, the radiation exposure and fluoroscopy time were significantly reduced because the establishment of working cannula was completed under continuous visualization, as well as foraminoplasty.
Importantly, several negative aspects of the full-endoscopic foraminoplasty should also be emphasized. First, complete removal of the migrated sequestrations that were separated into multiple pieces may not be attainable [2, 5]. However, the existence of the hidden fragment can be acceptable if there were no clinical symptoms after operation. With the time extension, some residual disc material can even be resorbed [5, 20]. Secondly, despite the skillful full-endoscopic transforaminal technique, traction or exfoliation between the nerve root and the migrated disc may cause additional dural sac or nerve root damage, especially in case with tight adhesion. Therefore, careful attentions should be taken to protect the dural sac or nerve root during the operation. Thirdly, partial surgical resection of the ventral superior articular process is a time-consuming procedure when foraminoplasty using the endoscopic trephine, and it could result in bleeding on the bone surface, which is hardly controlled with an aid of bipolar radiofrequency coagulators [23, 24]. Additionally, a large proportion of lumbar spine diseases may not be suitable for this technique, such as vertebral endplate (Modic) change, metastatic vertebral lesions, and central lumbar spinal stenosis.
Several shortcomings of the present study should be mentioned. First, as this is non randomized and not matched to control/cohort study, solid conclusion may not be drawn about the efficacy and advantages of the technique. Secondly, although all included patients’ radiating pain were relieved immediately after operation, a minority of patients were not reviewed by MRI during the follow up. There may be the existence of the hidden fragment. Thirdly, a limited number of cases with short-term follow-up may decrease the credibility of the findings that drawn from this series. Therefore, we believe that a larger number of cases is necessary to investigate the long-term efficacy of transforaminal full-endoscopic discectomy for highly down-migrated LDH.
Conclusion
Although surgical removal of highly downward migrated LDH is challenging, our favorable clinical results favor the full-endoscopic foraminoplasty performed in this series. We thus conclude that transforaminal full-endoscopic discectomy is an efficient alternative technique for surgical removal of highly downward migrated LDH. Nonetheless, further large sample size, multicenter comparative studies with long-term follow-up period need to validate our encouraging outcomes.
Availability of data and materials
The datasets presented in the current study are not publicly available since limitations of ethical approval involving patients’ data but are available from the corresponding author or co-author on reasonable request.
Abbreviations
- LDH:
-
Lumbar disc herniation
- ODI:
-
Oswestry Disability Index
- VAS:
-
Visual analogue scale
- MRI:
-
Magnetic resonance imaging
- AP:
-
Anteroposterior
- SD:
-
Standard deviation
References
Lee S, Kim S-K, Lee S-H, Kim WJ, Choi W-C, Choi G, et al. Percutaneous endoscopic lumbar discectomy for migrated disc herniation: classification of disc migration and surgical approaches. Eur Spine J. 2007;16(3):431–7.
Chen C-M, Lin G-X, Sharma S, Kim H-S, Sun L-W, Wu H-H, et al. Suprapedicular retrocorporeal technique of transforaminal full-endoscopic lumbar discectomy for highly downward-migrated disc herniation. World Neurosurg. 2020;143:e631–9.
Jeon CH, Chung NS, Son KH, Lee HS. Massive lumbar disc herniation with complete dural sac stenosis. Indian J Orthop. 2013;47(3):244–9.
Chen C, Fan P, Huang L, Zhen H, Liu L, Wang Y. Percutaneous endoscopic lumbar discectomy as an emergent surgery for cauda Equina syndrome caused by lumbar disc herniation. Pain Physician. 2020;23(3):E259–64.
Kim CH, Chung CK, Woo JW. Surgical outcome of percutaneous endoscopic interlaminar lumbar discectomy for highly migrated disk herniation. Clin Spine Surg. 2016;29(5):E259–66.
Sivakanthan S, Hasan S, Hofstetter C. Full-endoscopic lumbar discectomy. Neurosurg Clin N Am. 2020;31(1):1–7.
Zou HJ, Hu Y, Liu JB, Wu J. Percutaneous endoscopic transforaminal lumbar discectomy via eccentric trepan foraminoplasty technology for unilateral stenosed serve root canals. Orthop Surg. 2020;12(4):1205–11.
Hua W, Zhang Y, Wu X, Gao Y, Li S, Wang K, et al. Outcomes of discectomy by using full-endoscopic visualization technique via the interlaminar and transforaminal approaches in the treatment of L5-S1 disc herniation: an observational study. Medicine (Baltimore). 2018;97(48):e13456.
Hua W, Zhang Y, Wu X, Gao Y, Li S, Wang K, et al. Full-endoscopic visualized Foraminoplasty and discectomy under general anesthesia in the treatment of L4-L5 and L5-S1 disc herniation. Spine (Phila Pa 1976). 2019;44(16):E984–91.
Choi G, Prada N, Modi HN, Vasavada NB, Kim JS, Lee SH. Percutaneous endoscopic lumbar herniectomy for high-grade down-migrated L4-L5 disc through an L5-S1 interlaminar approach: a technical note. Minim Invasive Neurosurg. 2010;53(3):147–52.
Zanoli G, Strömqvist B, Jönsson B. Visual analog scales for interpretation of back and leg pain intensity in patients operated for degenerative lumbar spine disorders. Spine. 2001;26(21):2375–80.
Fairbank JC, Pynsent PB. The Oswestry disability index. Spine. 2000;25(22):2940–53.
Macnab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am. 1971;53(5):891–903.
Choi KC, Shim HK, Park CJ, Lee DC, Park CK. Usefulness of percutaneous endoscopic lumbar Foraminoplasty for lumbar disc herniation. World Neurosurg. 2017;106:484–92.
Schellinger D, Manz HJ, Vidic B, Patronas NJ, Deveikis JP, Muraki AS, et al. Disk fragment migration. Radiology. 1990;175(3):831–6.
Pan L, Zhang P, Yin Q. Comparison of tissue damages caused by endoscopic lumbar discectomy and traditional lumbar discectomy: a randomised controlled trial. Int J Surg. 2014;12(5):534–7.
Osman SG, Nibu K, Panjabi MM, Marsolais EB, Chaudhary R. Transforaminal and posterior decompressions of the lumbar spine. A comparative study of stability and intervertebral foramen area. Spine (Phila Pa 1976). 1997;22(15):1690–5.
Bernucci C, Giovanelli M. Translaminar microsurgical approach for lumbar herniated nucleus pulposus (HNP) in the “hidden zone”: clinical and radiologic results in a series of 24 patients. Spine. 2007;32(2):281–4.
Reinshagen C, Ruess D, Molcanyi M, Redjal N, Walcott BP, Goldbrunner R, et al. A novel translaminar crossover approach for pathologies in the lumbar hidden zone. J Clin Neurosci. 2015;22(6):1030–5.
Choi G, Lee S-H, Lokhande P, Kong BJ, Shim CS, Jung B, et al. Percutaneous endoscopic approach for highly migrated intracanal disc herniations by foraminoplastic technique using rigid working channel endoscope. Spine. 2008;33(15):E508–15.
Lin G-X, Park C-W, Suen T-K, Kotheeranurak V, Jun S-G, Kim J-S. Full endoscopic technique for high-grade up-migrated lumbar disk herniation via a translaminar keyhole approach: preliminary series and technical note. J Neurol Surg A Cent Eur Neurosurg. 2020;81(05):379–86.
Marković M, Živković N, Milan S, Gavrilović A, Stojanović D, Aleksić V, et al. Full-endoscopic interlaminar operations in lumbar compressive lesions surgery: prospective study of 350 patients-“ ENDOS” study. J Neurosurg Sci. 2016;64(1):16–24.
Li ZZ, Ma SY, Cao Z, Zhao HL. Percutaneous isthmus Foraminoplasty and full-endoscopic lumbar discectomy for very highly Upmigrated lumbar disc herniation: technique notes and 2 years follow-up. World Neurosurg. 2020;141:e9–e17.
Zhao Y, Yuan S, Tian Y, Liu X. Necessity of routinely performing foraminoplasty during percutaneous endoscopic transforaminal discectomy (PETD) for lumbar disc herniation. Br J Neurosurg. 2020:1–7. https://doi.org/10.1080/02688697.2020.1817853.
Acknowledgments
Ch Liu, and Hh Cai contributed equally to this case series and therefore are considered co-first authors. Also, we acknowledge that all authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors, and that all authors are in agreement with the manuscript.
We thank Professor Poonam Hiranandani, Roshani pawade, Editor-in-Chief, and all the reviewers for their valuable comments on the quality improvement of our manuscript.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
Hh Cai, Ch Liu, Hb Lin, Zq Wu, Xh Chen, Hz Zhang was responsible for study design, conceptualization, and manuscript drafting; Hh Cai, Ch Liu, Hb Lin, Zq Wu, Xh Chen, Hz Zhang conducted data collection, data entry, and manuscript writing; Hh Cai and Ch Liu made the data analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was conducted in line with the Declaration of Helsinki and approved by the Ethics Committee of Quanzhou Orthopedic-Traumatological Hospital and the Affiliated Hospital of Putian University. Also, informed consent for study participation were obtained from all subjects in this series.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cai, H., Liu, C., Lin, H. et al. Full-endoscopic foraminoplasty for highly down-migrated lumbar disc herniation. BMC Musculoskelet Disord 23, 303 (2022). https://doi.org/10.1186/s12891-022-05254-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05254-4