Abstract
Background
Meniscal allograft transplantation (MAT) may improve symptoms and function, and may limit premature knee degeneration in patients with symptomatic meniscal loss. The aim of this retrospective study was to examine patient outcomes after MAT and to explore the different potential definitions of ‘success’ and ‘failure’.
Methods
Sixty patients who underwent MAT between 2008 and 2014, aged 18–50 were identified. Six validated outcome measures for knee pathologies, patient satisfaction and return to sport were incorporated into a questionnaire. Surgical failure (removal of most/all the graft, revision MAT or conversion to arthroplasty), clinical failure (Lysholm < 65), complication rates (surgical failure plus repeat arthroscopy for secondary allograft tears) and whether patients would have the procedure again were recorded. Statistics analysis included descriptive statistics, with patient-reported outcome measures reported as median and range. A binomial logistic regression was performed to assess factors contributing to failure.
Results
Forty-three patients (72%) responded, mean age 35.6 (±7.5). 72% required concomitant procedures, and 44% had Outerbridge III or IV chondral damage. The complication rate was 21% (9). At mean follow-up of 3.4 (±1.6) years, 9% (4) were surgical failures and 21% (9) were clinical failures. Half of those patients considered a failure stated they would undergo MAT again. In the 74% (32) reporting they would undergo MAT again, median KOOS, IKDC and Lysholm scores were 82.1, 62.1 and 88, compared to 62.2, 48.5 and 64 in patients who said they would not. None of the risk factors significantly contributed to surgical or clinical failure, although female gender and number of concomitant procedures were nearly significant. Following MAT, 40% were dissatisfied with type/level of sport achieved, but only 14% would not consider MAT again.
Conclusions
None of the risk factors examined were linked to surgical or clinical failure. Whilst less favourable outcomes are seen with Outerbridge Grade IV, these patients should not be excluded from potential MAT. Inability to return to sport is not associated with failure since 73% of these patients would undergo MAT again. The disparity between ‘clinical failure’ and ‘surgical failure’ outcomes means these terms may need re-defining using a specific/bespoke MAT scoring system.
Similar content being viewed by others
Background
The menisci act primarily as load bearers and secondary stabilisers within the knee joint, and are chondroprotective. Loss of meniscal tissue through trauma or degeneration increases the joint contact forces by up to 350%, exacerbating articular cartilage degeneration [1]. Meniscal tears are particularly common in sportspersons [2, 3] with the typical mechanism of injury involving twisting on a flexed knee or loaded hyperflexion [4]. Symptomatic meniscal tears may require repair, or, if irreparable, a partial meniscectomy [5], significantly increasing the risk of future chondral failure and, ultimately, secondary osteoarthritis [6].
Meniscal Allograft Transplantation (MAT) was first reported in 1989, and is a useful potential option for symptomatic patients where there is loss or discontinuity of the peripheral meniscus and where the degenerative damage is not yet severe enough or the patient is too young for artificial joint replacement surgery to be a suitable option [7,8,9]. However, MAT is a technically demanding procedure, performed by only a small number of surgeons, and graft availability and cost can be problematic [10]. Patients eligible for MAT are typically young and high-demand, and they are a highly-complex population who have often already endured multiple previous surgical procedures, and many have expectations to return to high activity levels [1]. Although a challenge, restoring function in this patient population is a priority within orthopaedics today [11].
Whilst outcome data is limited by low volumes and short follow-up, there is evidence that MAT can relieve pain, optimising knee function and comfort in selected patients [7]. A pilot randomised-controlled trial in 2018 confirmed MAT had better outcomes at 1 year compared to physiotherapy [12]. Authors have reported positive patient outcome measures following MAT using the KOOS, IKDC, Lysholm, Tegner, and SF-12 scores [13,14,15,16]. It remains unclear what proportion of any improvement might be due to MAT alone or from potential concomitant procedures [17], and it is also unclear whether MAT has any long-term chondroprotective effect [18]. Whilst many studies have found that the addition of concomitant procedures at the same time as MAT do not affect outcomes, a recent study showed that compared to isolated MAT, PROMs were improved by the addition of a high tibial osteotomy to offload the affected compartment [19]. Certainly, MAT has been shown to have a higher-failure rate in ACL-deficient knees [20].
Surgical failure is defined variably in studies, but is most often defined as the patient either requiring removal of the allograft, allograft revision or conversion to joint replacement (arthroplasty) [13]. Clinical failure is often defined as a Lysholm Score of < 65 and has been shown not to correlate well with surgical failure or poor patient-reported outcomes [13].
There are differing definitions of failure within the existing literature, with surgical failure not necessarily correlating to clinical failure. The aim of this study was to examine the outcomes of MAT in one surgeon’s patient cohort (using the same graft preparation and fixation techniques), using a variety of surgical and patient-reported outcome measures, with a view to exploring the question of what ‘success’ might actually mean. As with most studies of MAT, many patients required additional concomitant procedures alongside MAT, complicating the assessment of outcomes. It was hypothesized that patients classified as ‘surgical failures’ or ‘clinical failures’ would have significantly lower outcome measures compared to those who were not.
Methods
Ethical and Risk Assessment Approval was obtained from the University of Edinburgh’s Moray House School of Education, and use of the surgeon’s data was approved by The London Bridge Hospital Clinical Governance Committee, and information governance was maintained throughout the study.
Following informed consent, a retrospective analysis of patients aged 18 to 50 years who had undergone MAT by a single surgeon between 2008 and 2014 was undertaken. The indications for MAT were symptomatic patients with complete or subtotal loss of a meniscus causing pain and reduced function, with evidence of post-meniscectomy degenerative damage where artificial joint replacement surgery was not yet indicated. Each patient had previously been assessed for suitability for MAT by history, clinical examination, imaging and arthroscopic findings, with the principles of treatment fully explained. Alignment and stability were assessed before MAT, to check whether concomitant procedures were also required. Table 1 shows the list of the 31 concomitant procedures performed, with anterior cruciate ligament (ACL) reconstruction being the most common.
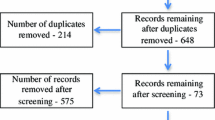
Sixty patients were identified and sent questionnaires, with zero excluded.
Surgical procedure
All grafts were fresh-frozen, non-irradiated BioCleansed® menisici obtained from RTI Surgical, Inc., Florida. The grafts were size-matched using the Pollard technique [21, 22] and fixed arthroscopically using transosseuous tibial bone tunnel suture fixation for the anterior and posterior insertional ligaments, plus peripheral capsular sutures, using the method described by Matava et al. [23]. This is considered by many to be the most practical way to secure fixation of the graft [24].
Rehabilitation
Following surgery, patients were advised to use crutches and a hinged knee brace locked at 0° to 90° for the first 6 weeks. Rehabilitation was then commenced to regain full range-of-motion, with proprioceptive reflex re-training, with slow and cautious muscle strengthening exercises, progressing to light non-impact cardiovascular fitness exercises. Patients were specifically advised to avoid loaded deep knee flexion, heavy weights, loaded twisting or impact through the knee. Patients were specifically advised against returning to any impact type exercise/sport [11].
Clinical assessment and questionnaire
A request to complete an online self-administered questionnaire was sent via email in December 2016 using QuestionPro software. The date of follow-up was the date the patient completed the online questionnaire. Validated patient-reported outcome measures (PROMs) for knee pathologies (IKDC, KOOS, Tegner and Lysholm) were incorporated into the questionnaire [25]. A Visual Analogue Score (VAS) pain score (0 to 10) and SF-12 Short-Form Health Survey were also used. The SF-12 was also split in the ‘mental’ and ‘physical’ subscales, which were analysed separately. Where questions from the IKDC and KOOS asked about specific joint-loading activities that the patients had specifically been advised not to perform, a ‘Not Applicable’ option was added. Questions on sport were included in the questionnaire, despite the surgeon having specifically advised all patients against ever returning to impact or twisting type activities. Patients were also asked whether they would have the procedure again.
Surgical failure was gathered from clinical documentation, and was defined as removal of most or all of the allograft, allograft revision or conversion to joint arthroplasty. ‘Clinical failure’ was defined as a Lysholm score of < 65. Time from MAT surgery to surgical failure was noted. Time to clinical failure was defined as being from the date of MAT surgery to the date of the patient completing the questionnaire. As there was no continual follow-up, it is acknowledged that clinical failure may have occurred prior to the study’s follow-up. The complication rate for MAT surgery was defined as including those patients who underwent repeat arthroscopy for secondary allograft tears as well as those patients who were surgical failures.
Statistical analysis
The results were analysed, with descriptive statistics and with PROMs reported as median and range.
Comparisons between PROMs from patients with versus without surgical failure, and with versus without clinical failure were carried out. Data were checked for normality using Shapiro-Wilk tests (Field [26]) with α-level set at 0.05, and if data were normally distributed then independent t-tests (α =0.05) were carried out. If data were non-normal, Mann-Whitney U non-parametric tests were performed. Effect sizes were also calculated and classified according to Cohen [27] [30]; small (0.2), medium (0.5), large (0.8). PROMS were also compared between patient groups on whether or not they would have the procedure again (Yes / No / Not sure) using One-Way ANOVA (α =0.05) or Kruskal-Wallis tests, depending on whether data were normal or not. Effect sizes were assessed with Partial Eta Squared with small, medium and large being 0.01, 0.06, 0.14 respectively [26]. The difference between pre- and post-operative Tegner scores was analysed using a repeated measures t-test if the data were normally distributed, and a Wilcoxon matched Pairs Signed Ranks test if they were not.
Relationships between five previously studied risk factors (age, gender, number of concomitant procedures, Outerbridge grade, lateral vs medial side of MAT) and surgical and clinical failures were examined with binary multiple logistic regression forced entry method (BMLR) with α =0.05 [26].
Results
Of the total of 60 MAT procedures performed on 60 patients by this surgeon during the period 2008–2014, 43 (72%) patients responded, with a mean follow-up of 3.4 (±1.6) years. Seventeen patients (28%) did not respond. Table 2 outlines the baseline demographics of the patients.
Data were not normally distributed for all the PROMs except the IKDC and VAS scores. Therefore Table 3 shows the median and interquartile PROM scores for the whole cohort and for the surgical failure and clinical failure groups. For 3 patients, their responses to the IKDC were < 90% complete, rendering them invalid, and these were therefore excluded. All KOOS scores were valid.
The complication rate was 21%. Four patients were classified as surgical failures and nine were classed as clinical failures, with three patients having both surgical and clinical failure. The mean times to surgical and clinical failures were 1.8 and 2.6 years respectively. Statistical comparison tests did not show any significant differences for any of the PROMs between the two groups. However, Effect Sizes for KOOS and Lysholm scores were large. The Effect Sizes for IKDC, post-operative Tegner scores and SF-12 mental subscale were medium-large and SF-12 (whole test) was small-medium. There was no effect between the two surgical failure groups for pre-operative Tegner Activity Scale. For clinical failure, there were significant differences (p < 0.001) between groups for KOOS and Lysholm scores, for the IKDC, the VAS and the post-operative Tegner values (all p = 0.002), for the SF-12 (p = 0.041) and SF-12 physical subscale (p = 0.024) but not for pre-operative Tegner. Effect Sizes for all PROMs were large, except for pre-operative Tegner score, which was small-medium. The Wilcoxon test showed that there was a significant difference (p < 0.001) between pre- and post-operative Tegner scores for the whole sample, and this also had a large effect size.
Six patients stated that they would not have the procedure again, with two of these being clinical failures, one being a surgical failure and clinical failure, but three of these did not come under either of the definite failure categories. Five patients were unsure whether they would repeat the procedure again, with the remaining 32 stating they would undergo it again. Table 4 shows the PROM scores grouped by patients’ statements about whether or not they would undergo the procedure again (Yes / No / Not Sure). There were no statistical differences between the groups, although the KOOS (p = 0.091), SF-12 physical subscale (p = 0.085) and Lysholm scores (p = 0.056) approached significance. Effect sizes between the groups were large for KOOS and Lysholm values, medium-large for the SF-12 physical subscale and small-medium for all other PROMs.
Full results for the BMLRs are shown in Tables 5 and 6. The regression found none of the five risk factors was significantly related to the chance of surgical failure, although gender (being female) was nearly significant (p = 0.064). In the regression for clinical failure, again, none of the risk factors was significant, although gender (p = 0.077) and number of concomitant procedures (p = 0.067) were nearly significantly linked to the chance of clinical failure.
Pre-operative and post-operative patient sporting activity, using a combination of findings from experimental studies and clinical investigations to define intensity of impact [28], is shown in Table 7. Thirty two (74%) patients returned to fewer, lower intensity sporting activities following MAT, with 34 patients (79%) expecting this change. Of those who did not return to the same level of sport, 73% stated that they would undergo the procedure again. At review, 39.2% were satisfied, 20.9% were neither satisfied nor dissatisfied, and 40% were dissatisfied with their level of sporting activity achieved following surgery.
Discussion
This study sought to record the PROMs of patients who had undergone MAT, and to investigate whether there were differences reported in those patients with ‘surgical failure’ or ‘clinical failure’ versus those categorised as being ‘successful’.
For the whole sample, PROM scores showed generally good outcomes, with median KOOS, IKDC and Lysholm scores being 80, 55.8 and 81. Further investigation showed that there was a trend towards PROMs being lower in those patients with surgical failure, although this was not statistically significant. This was possibly due to the small sample of surgical failures (n = 4). Patients classified as clinical failures did have significantly lower KOOS and IKDC scores, and lower post-operative Tegner values. In the present study, 74% of patients said that they would undergo MAT again. The median post-operative Lysholm, KOOS and IKDC scores in this sub-group were 88, 82, and 62.1 - scores consistent with good outcomes following MAT. However, there were no significant differences in PROMs between those who stated that they would undergo the procedure again compared to those who stated that they would not and those who were not sure.
The results for Lysholm, KOOS and Tegner scores compared favourably or similarly to other reported series in the published literature [14,15,16], although our IKDC scores were lower [15]. Naimark et al. reported similar outcomes in patients who underwent arthroscopic partial meniscectomy [29]. The Tegner scores were significantly reduced following surgery, probably due to the specific post-operative restrictions that were recommended by the operating surgeon.
It should be noted that there are other techniques to replace menisci, such as the Actifit and the Collagen Meniscal Implant. Interestingly, the studies evaluating the effect of these treatments also do not have a consensus on accepted definitions of failures [30]. However, these implants are only suitable specifically for the treatment of partial meniscal loss where the is still continuity of the peripheral meniscal rim, as they require a meniscal rim for attachment [31]. This therefore makes comparison to MAT difficult. De Coninck et al. reported more favourable outcomes in IKDC with the Actifit compared to our study, but our study showed higher results in KOOS and Lysholm scores [32]. The two studies had comparable mean ages, but De Coninck excluded patients who had severe cartilage damage, whilst in our study 44% had an Outerbridge Grade III or IV, and this may explain the higher IKDC scores in their study. Furthermore, the KOOS and IKDC scores both contain questions regarding activities such as jumping, twisting and pivoting; activities which our participants were advised not to undertake, and so may bias results, as other studies also report higher scores in these questionnaires [33, 34].
While the number of patients undergoing MAT remains small, finding the right tool to evaluate patients is problematic. New scoring systems may provide improved evaluation of MAT.
The Western Ontario Meniscal Evaluation Tool (WOMET) may be appropriate. It is a specific questionnaire aimed to detect the impact of meniscal tears on health-related quality of life [35]. When first designing this present study, it was decided not to include WOMET as there were doubts at that time with regard to WOMET’s reliability, construct validity and responsiveness [36]. It would also have caused questionnaire fatigue by adding a raft of further questions which may have reduced questionnaire completion rates. Whilst Sgroi et al. reported superior measurement of knee function and quality-of-life impairment using WOMET compared to the KOOS in patients treated for meniscal tears [37], to the authors’ knowledge, it had not been used in studies purely investigating MAT. Whether WOMET is indeed a more useful tool for the evaluation of patients who have undergone MAT, however, is a topic in itself for further research. Until the most appropriate and validated scoring system is established for the evaluation of patients who have undergone MAT, this present study suggests that success cannot be adequately defined.
The surgical failure rate of 9% was similar to that reported in other comparable studies, which have reported a failure rate of 10.4% [13]. The clinical failure rate of 21% was greater than that reported by Lee et al. [16] (8.5%) and Zaffagnini et al. [14], (11%). The complication rate was 21%; similar to the 21.3% rate reported in the meta-analysis by El Attar et al. [7]. A consensus regarding the current definition of clinical and surgical failure is required, since two (50%) patients with surgical failures and six (66.7%) with clinical failures said that they would undergo the MAT procedure again or were unsure. It is concerning that previous authors have solely used these endpoints to report the efficacy of MAT.
This study, therefore, suggests that the term ‘patient satisfaction’ may define success better than ‘surgical failure’ or ‘clinical failure’. Patient satisfaction, in terms of activity levels and current symptoms, do not in this study correlate with surgical outcomes. Patient satisfaction may be best incorporated into a questionnaire using the WOMET score, but again, this requires further research and discussion with specific patient focus groups.
The BMLR analysis did not find any risk factors that were significantly associated with failure, although gender (surgical and clinical failure) and number of concomitant procedures (clinical failure) were nearly significant. However, given the heterogeneity of concomitant procedures, future studies could investigate the effect of these different procedures on the success of MAT. The odds ratios showed that except for lateral (vs medial) MAT in surgical failure, all risk factors increased the odds of surgical or clinical failure. However, many of these odds ratios were close to unity, reinforcing their lack of statistical significance.
This study’s analyses support the findings of Parkinson et al. [13] and Ahn et al. [38] that potential risk factors of age, gender and number of concomitant procedures were not related to surgical failure. However, our study disagrees with those studies, in that Outerbridge classification and lateral vs medial were not found to be significant factors in our analysis. Whilst some studies have found that articular cartilage damage at the time of surgery and medial (vs. lateral) allografts are associated with a higher risk of surgical failure [13], this study supports the findings of other papers that conclude that cartilage damage does not make a difference [38,39,40] and that medial allografts are not at a higher risk of surgical failure [40]. Importantly, however, it should be noted that where articular cartilage damage was found in the relevant compartment of a patient’s knee at the time of MAT surgery, the articular cartilage pathology was also treated at the same time; with radiofrequency coblation chondroplasty for unstable or rough partial thickness chondral damage, with microfracture for small (<2cm2) full-thickness defects or with articular cartilage grafting (using Chondrotissue grafting) for larger (>2cm2) defects. Therefore, it could be surmised that appropriate concomitant treatment of articular cartilage lesions possibly lessens or even eliminates the otherwise increased risk of failure after MAT that might otherwise be associated with increasing severity of articular cartilage damage.
One reason for the lack of significance found in some of our analyses might be the small sample size in the present study, combined with the number of risk factors examined, which could have led to a lack of statistical power. The methods in the present study were better controlled compared to some previous research: only fresh-frozen meniscal allografts (which are biologically and mechanically superior to other forms of preservation [41]) were used, and these were all sourced from a single provider, and a single one-surgeon technique was used. Previous authors have either not reported their allograft sources [38, 42] or have used multiple providers with different preservation techniques [13]. Additionally, the generally good outcomes following MAT in the present study may be attributable to the surgical technique; suture fixation of the allograft to the capsule combined with trans-tibial bone tunnel suture fixation is the current preferred technique [14, 43, 44]. Techniques using bone plug fixation risk articular cartilage damage and have been associated with a higher failure rate [45, 46].
There was no difference in the SF-12 mental sub-scores in patients who said that they would undergo surgery again versus those who would not, although the physical sub-score was approaching significance. Saltzman et al. [47] and Rue et al. [48] also previously reported that the physical component improved significantly following MAT but that the mental score did not.
It was observed that following MAT, patients returned to fewer and lower levels of sport. Seventeen patients were satisfied with the level of sport achieved following MAT, but 17 others were dissatisfied. Nearly 80% of patients did expect there to be a difference in the level of physical activity that they could achieve after MAT, although there were no differences between the satisfaction levels between those who expected there to be a difference and those who did not. It is unclear whether the protective post-operative regime or the MAT procedure itself explains the dissatisfaction about not being able to return to sport.
Limitations
The present study had a number of limitations. First, the sample size was smaller than some comparable studies [13, 38] and so statistical power will have been weakened. However, this was offset by the tight control over materials and methods, and by the use of one surgeon, reducing variability in the procedures. Whilst this ensures homogeneity, longer-term studies are required to ensure a sample size is large enough for an adequately powered analysis for each failure sub-group analysis. MAT is a relatively new procedure in the UK and sample sizes are currently small.
Second, there were no pre-operative PROMs available, apart from the Tegner values. As this was a retrospective study, the collection of pre-operative scores was not feasible. However, this is not unusual, and other authors [13, 38] have also used retrospective methods. As with all retrospective studies, there will be significant recall bias. It is still possible to draw useful conclusions from retrospective studies, but in future more prospective PROMs should be taken prior to MAT surgery.
As there was no continual follow-up, clinical failure may have occurred prior to the time at which the study was performed. It was also not possible in this study to review the potential risk factors of mechanical axis, instability or BMI, as not enough information was available for this within the patient records, and therefore a confounding effect in our results cannot be ruled out. However, in the senior author’s practice it is standard practice to correct any varus or valgus malignment greater than 5o with an appropriate realignment osteotomy either in advance of or at the same time as MAT.
Conclusions
This retrospective study, with 3-year follow-up of 43 patients undergoing MAT, reported outcome scores that are consistent with success, with scores of 82.1, 62.1 and 88 for KOOS, IKDC and Lysholm, respectively. Those patients classified as clinical failures had significantly lower outcome scores, although the four patients with surgical failure did not, possibly due to the small sample. It was not possible to identify significant pre-operative risk factors associated with surgical or clinical failure, although gender (being female) and the number of concomitant procedures were nearly significant and had high odds ratios. The use of the terms ‘surgical failure’, ‘clinical failure’ and ‘patient satisfaction’ may need further consideration, since up to 60% of patients defined as clinical / surgical failures said that they would undergo the procedure again. Either newer outcome measures, such as the WOMET, or a bespoke MAT-specific measure could help to re-define success / failure and establish a more sensitive marker of graft survival and the anticipated chondroprotective effects of MAT.
Availability of data and materials
The full datasets generated and/or analysed during the current study are not publicly available due to patient data confidentiality and data protection laws, but an anonymised dataset may be available from the corresponding author upon reasonable request.
Abbreviations
- IKDC:
-
International Knee Documentation Committee
- KOOS:
-
Knee Injury and Osteoarthritis Outcome Score
- MAT:
-
Meniscal allograft transplantation
- SF-12:
-
The 12-Item Short-Form Health Survey
- VAS:
-
Visual Analogue Scale
- WOMET:
-
Western Ontario Meniscal Evaluation Tool
References
Frank RM, Cole BJ. Meniscus transplantation. Curr Rev Musculoskelet Med. 2015;8:443–50.
Englund M. Osteoarthritis: replacing the meniscus to prevent knee OA—fact or fiction? Nat Rev Rheumatol. 2015;11(8):1–2.
Waterman BR, Rensing N, Cameron KL, Owens BD, Pallis M. Survivorship of meniscal allograft transplantation in an athletic patient population. Am J Physiol - Integr Comp Physiol. 2016;44(5):1237–42.
Greis PE, Bardana DD, Holmstrom MC, Burks RT. Meniscal injury: I. basic science and evaluation. J Am Acad Orthop Surg. 2002;10(3):168–76.
Smith N, MacKay N, Costa ML, Spalding T. Meniscal allograft transplantation in a symptomatic meniscal deficient knee: a systematic review. Knee Surgery, Sport Traumatol Arthrosc. 2014;23(1):270–9.
Benedetto K, Rangger C. Arthroscopic partial meniscectomy: 5-year follow up. Knee Surg Sport Traumatoloy Arthrosc. 1993;1(3–4):235–8.
ElAttar M, Dhollander A, Verdonk R, Almqvist KF, Verdonk P. Twenty-six years of meniscal allograft transplantation: is it still experimental? A meta-analysis of 44 trials. Knee Surgery, Sport Traumatol Arthrosc. 2011;19(2):147–57.
Milachowski KA, Weismeier K, Wirth CJ. Homologous meniscus transplantation - experimental and clinical results. Int Orthop. 1989;13(1):1–11.
Harris JD, Hussey KE, Wilson H, Pilz K, Gupta AK, Gomoll A, et al. Biological knee reconstruction for combined malalignment, meniscal deficiency, and articular cartilage disease. Arthrosc J Arthrosc Relat Surg. 2015;31(2):275–82.
Getgood A, Robertson A. Meniscal tears, repairs and replacement - a current concepts review. Orthop Trauma. 2010;24(2):121–8.
Spalding T, Getgood A. Defining outcome after meniscal allograft transplantation: is buying time a valid measure of success? Knee surgery. Sport Traumatol Arthrosc. 2016;24(5):1424–6.
Smith NA, Parsons N, Wright D, Hutchinson C, Metcalfe A, Thompson P, et al. A pilot randomized trial of meniscal allograft transplantation versus personalized physiotherapy for patients with a symptomatic meniscal deficient knee compartment. Bone Jt J. 2018;100B(1):56–63.
Parkinson B, Smith N, Asplin L, Thompson P, Spalding T. Factors predicting meniscal allograft transplantation failure. Orthop J Sport Med. 2016;4(8):1–6.
Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, Benzi A, Serra M, Rotini M, et al. Survivorship and clinical outcomes of 147 consecutive isolated or combined arthroscopic bone plug free meniscal allograft transplantation. Knee Surgery, Sport Traumatol Arthrosc. 2016;24(5):1432–9.
Chalmers PN, Karas V, Sherman SL, Cole BJ. Return to high-level sport after meniscal allograft transplantation. Arthrosc J Arthrosc Relat Surg. 2013;29(3):539–44.
Lee B-S, Bin S-I, Kim J-M, Kim W-K, Choi JW. Survivorship after meniscal allograft transplantation according to articular cartilage status. Am J Sports Med. 2017;45(5):1095–101.
Noyes FR, Barber-Westin SD. Meniscal transplantation in symptomatic patients under fifty years of age: survivorship analysis. J Bone Joint Surg Am. 2015;97(15):1209–19.
Crook TB, Ardolino A, Williams LAP, Barlow IW. Meniscal allograft transplantation: a review of the current literature. Ann R Coll Surg Engl. 2009;91(5):361–5.
Bloch B, Asplin L, Smith N, Thompson P, Spalding T. Higher survivorship following meniscal allograft transplantation in less worn knees justifies earlier referral for symptomatic patients: experience from 240 patients. Knee Surg Sports Traumatol Arthrosc. 2019;27(6):1891–9.
van Arkel E, de Boer H. Human meniscal transplantation. Preliminary results at 2 to 5-year follow-up. J Bone Jt Surg [Br]. 1995;77(4):589–95.
McDermott ID, Sharifi F, Bull AMJ, Gupte CM, Thomas RW, Amis AA. An anatomical study of meniscal allograft sizing. Knee Surgery, Sport Traumatol Arthrosc. 2004;12(2):130–5.
Pollard ME, Kang Q, Berg EE. Radiographic sizing for meniscal transplantation. Arthrosc J Arthrosc Relat Surg. 1995;11(6):684–7.
Matava MJ. Meniscal allograft transplantation. Clin Orthop Relat Res. 2007;455(455):142–57.
Myers P, Tudor F. Meniscal allograft transplantation: how should we be doing it? A systematic review. Arthrosc J Arthrosc Relat Surg. 2015;31(5):911–25.
Tilley S, Thomas N. Focus On. What knee scoring system? J Bone Joint Surg. 2010. https://pdfs.semanticscholar.org/d0ed/1706e373ccb3b723873963cd96c40b508c2d.pdf.
Field A. Discovering statistics using IBM SPSS Statistics. 4th edition. Sage Publications. Los Angeles: SAGE; 2013. 1–952 p.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New York, NY: Psychology Press; 1998.
Buckwalter JA, Martin JA. Sports and osteoarthritis. Curr Opin Rheumatol. 2004;16(5):634–9.
Naimark MB, Kegel G, O’Donnell T, Lavigne S, Heveran C, Crawford DC. Knee function assessment in patients with meniscus injury: a preliminary study of reproducibility, response to treatment, and correlation with patient-reported questionnaire outcomes. Orthop J Sport Med. 2014;2(9):1–8.
Filardo G, Andriolo L, Kon E, de Caro F, Marcacci M. Meniscal scaffolds: results and indications. A systematic literature review. Int Orthop. 2015;39(1):35–46.
Gomoll AH, Filardo G, Almqvist FK, Bugbee WD, Jelic M, Monllau JC, et al. Surgical treatment for early osteoarthritis. Part II: allografts and concurrent procedures. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):468–86.
De Coninck T, Huysse W, Willemot L, Verdonk R, Verstraete K, Verdonk P. Two-year follow-up study on clinical and radiological outcomes of polyurethane meniscal scaffolds. Am J Sports Med. 2013;41(1):67–72.
Kon E, Filardo G, Zaffagnini S, Di Martino A, Di Matteo B, Marcheggiani Muccioli GM, et al. Biodegradable polyurethane meniscal scaffold for isolated partial lesions or as combined procedure for knees with multiple comorbidities: clinical results at 2 years. Knee Surg Sports Traumatol Arthrosc. 2014;22(1):128–34.
Zaffagnini S, Marcheggiani Muccioli GM, Bulgheroni P, Bulgheroni E, Grassi A, Bonanzinga T, et al. Arthroscopic collagen meniscus implantation for partial lateral meniscal defects: a 2-year minimum follow-up study. Am J Sports Med. 2012;40(10):2281–8.
Kirkley A, Griffin S, Whelan D. The development and validation of a quality of life-measurement tool for patients with meniscal pathology: the Western Ontario meniscal evaluation tool (WOMET). Clin J Sport Med. 2007;17(5):349–56.
Abram SG, Middleton R, Beard DJ, Price AJ, Hopewell S. Patient-reported outcome measures for patients with meniscal tears: a systematic review of measurement properties and evaluation with the COSMIN checklist. BMJ Open. 2017;7(10):1–15.
Sgroi M, Kocak S, Reichel H, Kappe T. Comparison of 3 knee-specific quality-of-life instruments for patients with meniscal tears. Orthop J Sport Med. 2018;6(1):1–6.
Ahn JH, Kang HW, Yang TY, Lee JY. Multivariate analysis of risk factors of graft extrusion after lateral meniscus allograft transplantation. Arthrosc J Arthrosc Relat Surg. 2016;32(7):1337–45.
Rosso F, Bisicchia S, Bonasia DE, Amendola A. Meniscal allograft transplantation. Am J Sports Med. 2015;43(4):998–1007.
Verdonk P, Verstraete KL, Almqvist KF, De Cuyper K, Veys EM, Verbruggen G, et al. Meniscal allograft transplantation: long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surgery, Sport Traumatol Arthrosc. 2006;14(8):694–706.
McDermott ID. What tissue bankers should know about the use of allograft meniscus in orthopaedics. Cell and Tissue Bank. 2009;11(1):75–85.
Stone KR, Pelsis JR, Surrette ST, Walgenbach AW, Turek TJ. Meniscus transplantation in an active population with moderate to severe cartilage damage. Knee Surg Sports Traumatol Arthrosc. 2014;23(1):251–7.
Marcacci M, Marcheggiani Muccioli GM, Grassi A, Ricci M, Tsapralis K, Nanni G, et al. Arthroscopic meniscus allograft transplantation in male professional soccer players: a 36-month follow-up study. Am J Sports Med. 2014;42(2):382–8.
Spalding T, Parkinson B, Smith N, Verdonk P. Arthroscopic meniscal allograft transplantation with soft-tissue fixation through bone tunnels. Arthrosc Tech. 2015;4(5):e559–63.
Rodeo S. A, Seneviratne a, Suzuki K, Felker K, Wickiewicz TL, Warren RF. Histological analysis of human meniscal allografts. A preliminary report. J bone Jt Surg - Am Vol. 2000;82-A(8):1071–82.
von Lewinski G, Kohn D, Wirth CJ, Lazovic D. The influence of nonanatomical insertion and incongruence of meniscal transplants on the articular cartilage in an ovine model. Am J Sports Med. 2008;36(5):841–50.
Saltzman BM, Bajaj S, Salata M, Daley EL, Strauss E, Verma N, et al. Prospective long-term evaluation of meniscal allograft transplantation procedure: a minimum of 7-year follow-up. J Knee Surg. 2012;25(2):165–75.
Rue JPH, Yanke AB, Busam ML, McNickle AG, Cole BJ. Prospective evaluation of concurrent meniscus transplantation and articular cartilage repair: minimum 2-year follow-up. Am J Sports Med. 2008;36(9):1770–8.
Acknowledgements
Thanks to the patients of IM who agreed to participate in this study.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
IM was the Consultant Surgeon undertaking the meniscal allograft transplantations and assisted in preparation of the manuscript. HS was responsible for the design, acquisition of data, statistical analysis, interpretation of data and writing the manuscript. SC supervised HS, and assisted with the statistical analysis and preparation of the manuscript. VA assisted in the preparation of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Formal written Ethical and Risk Assessment Approval was obtained from the University of Edinburgh’s Moray House School of Education. Use of the surgeon’s data was approved (by e-mail) by The London Bridge Hospital Clinical Governance Committee, and information governance was maintained throughout the study. All patients who responded to the questionnaire gave consent for their data to be used in this research as part of the questionnaire itself.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Searle, H., Asopa, V., Coleman, S. et al. The results of meniscal allograft transplantation surgery: what is success?. BMC Musculoskelet Disord 21, 159 (2020). https://doi.org/10.1186/s12891-020-3165-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-020-3165-0