Abstract
Background
Subacromial decompression, that consists of the release of the coracoid-acromial ligament, subacromial bursectomy and anterior-inferior acromioplasty, has traditionally been performed in the management of this pathology. However, the purpose of subacromial decompression procedure is not clearly explained. Our reaserch aimed to analyse the differences among the outcomes of arthroscopic rotator cuff repair (RCR) made with suture anchors, with or without the subacromial decompression procedure.
Methods
116 shoulders of 107 patients affected by rotator cuff (RC) tear were treated with Arthroscopic RCR. In 54 subjectes, the arthroscopic RCR and the subacromial decompression procedure (group A) were executed, whereas 53 took only arthroscopic RCR (group B). Clinical outcomes were evaluated through the use of the modified UCLA shoulder rating system, Wolfgang criteria shoulder score and Oxford shoulder score (OSS). Functional outcomes were assessed utilizing active and passive range of motion (ROM) of the shoulder, and muscle strength. The duration of the follow up and the configuration of the acromion were used to realize the comparison between the two groups.
Results
In patients with 2 to 5 year follow up, UCLA score resulted greater in group A patients. In subjectes with longer than five years of follow up, group B patients showed considerably greater UCLA score and OSS if related with group A patients. In subjectes that had the type II acromion, group B patients presented a significant greater strength in external rotation.
Conclusion
The long term clinical outcomes resulted significantly higher in patients treated only with RCR respect the ones in patients underwent to RCR with subacromial decompression.
Similar content being viewed by others
Background
The prevalence of rotator cuff (RC) lesions chenges between 5 to 39% among people, often occurring in patients younger than 40 years old, and may be bilateral in 16% of patients [1,2,3,4,5]. Outcomes of surgical repair are unpredictable, in part because surgical repair does not reproduce the natural enthesis, and in part because the physiological processes responsible for the ability of the tendon to reconnected to the bone have not been completely known [6,7,8,9,10,11,12,13].
Subacromial impingement syndrome was considered the most frequent cause of RC pathology, and Neer [1, 14, 15] was the first that described this condition as an irritation of the subacromial tissue under the coraco-acromial arch with consequent degeneration and rupture. The role, and even the presence, of subacromial impingement has recently been questioned [16]. Spurs on the acromion and the shape of the acromion are often associated with RC tears, even if their causality has not been proved [16, 17].
Subacromial decompression that comprehend the release of the coracoid-acromial ligament, subacromial bursectomy and anterior-inferior acromioplasty has traditionally been performed in the management of this pathology. Various researches have shown excellent results of arthroscopic RC repair (RCR) conducted together with subacromial decompression [18, 19]. However, only one randomized controlled trial has compared the arthroscopic RCR outcome realized with or without the subacromial decompression [20].
Our research aims to analyse the differences between clinical and functional outcomes of arthroscopic RCR with or without subacromial decompression in patients with full-thickness RC tears.
Methods
Ethics
The ethics committee of the university “Campus Bio Medico” of Rome authorized the research and all subjects signed consent to be enrolled.
Patient enrolment
Inclusion criteria were: RC tear, absence of shoulder instability, absence of fracture of the higher/lower tuberosity of the humerus or the glenoid, full-thickness RC tear confirmed by shoulder MRI, pain and/or functional impairment of the shoulder for at least six months, symptoms refractory to conservative protocol of treatment (anti-inflammatory, rehabilitation, repose, and local corticosteroid infiltration), treatable RC tears.
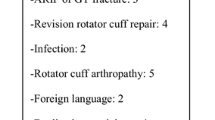
Exclusion criteria included: inflammatory joint disease, preceding operative treatment on the damaged shoulder, labral pathology agreeable to operative treatment, degenerative osteoarthritis of the glenohumeral joint, symptomatic osteoarthritis of the acromioclavicular joint, RC arthropathy, impossibility to write up questionnaires consequent to language disease or cognitive disturbs.
117 subjects (126 shoulders) presented the inclusion\exclusion criteria and were contacted telephonically. Of these, 107 (116 shoulders) accepted our invitation to participate to the study and were retrospectively examined and assigned into Group 1 (54 patients (59 shoulders) RCR associated with simultaneous subacromial decompression) or Group 2 (53 patients (57 shoulders) RCR without subacromial decompression). The two groups were evaluated in relation to the of clinical and functional outcomes according to the shape of acromion and length of the follow-up.
Clinical assessment
Clinical outcomes were assessed employing the modified UCLA score, Wolfgang criteria, and Oxford Shoulder Score (OSS) score, all administered by two blinded examiners at the last follow-up.
The modified UCLA [21] evaluates post-surgical shoulder discomfort (10 points), function (10 points), active forward flexion (5 points), strength (5 points) and patient well-being (5 points). The final result extends from 0 to 35, and it can be subdivided in excellent (34–35 points), good (28–33), fair (21–27), or poor (0–20).
The Wolfgang criteria estimate post-operative shoulder discomfort (4 points), active abduction (4 points), strength (4 points) and patient well-being (1 point or minus 1 point). The final score extends from 0 to 17, and it can be subdivided in excellent (14–17 points), good (11–13 points), fair (8–10 points) or poor (0–7 points).
The OSS [22, 23] is a simple questionnaire made of 12 self-administered items assessing shoulder function, pain and strength related to quotidian actions. The final result ranges from 12 to 60 points, where 60 indicates the worst function of the shoulder.
Functional assessment
Two blinded testers evaluated passive and active range of motion (ROM), and muscle strength at the last follow-up.
Standard measurement guidelines were used to assess supine passive and active forward elevation, intra and extra rotation ROM (90° abduction). A conventional goniometer was employed in order to calculate with scales scored in one-degree increments. A dynamometer (model 01163, Lafayette Instrument Company, Lafayette, Indiana) was utilized to estimate the strength of anterior elevation, intra and extra rotation of the shoulder.
Both testers made three estimations for each ROM and strength measurement examined. The average value for each variable was utilized for statistical determinations.
Imaging
Preoperative MRI scans and oblique coronal, oblique sagittal and axial T2-weighted spin-echo MRIs (repetition time (RT) were executed for each subject: 3200 milliseconds; echo time (ET): 85 milliseconds) and standard radiographs (antero-posterior view, lateral view of the scapula, and axillary one).
Arthroscopic technique
Patient were positioned in lateral decubitus: the brachial plexus block, together with the general anaesthesia, were performed. The arm was suspended at 45° of abduction and 20° of forward flexion with 4.5 to 6.5 kg of traction.
The RC back was mobilized to its bone site of attachment employing a lateral portal and the footprint of the greater tuberosity was weared. One row of suture anchors double loaded with N° 2 Fiberwire (Corkscrew or Biocorkscrew, Arthrex, Naples, FL) were positioned in the lateral aspect of the footprint to perform the RC repair. The subacromial decompression, that consist of the subacromial bursectomy, the release of coraco-acromial ligament and of the antero-inferior acromioplasty was performed in all patients of Group 1, often because of acromion type III or acromial spurs or reduced subacromial space or acromioclavicular joint arthritis. In acromion type III, the most anterior portion of the acromion has a hooked shape with a subacromial spur. However, subacromial decompression was also performed in patients with subacromial spurs and without acromion type III.
Postoperative management
Post-surgical protocol was identical for the two categories of patients. An abduction bolster was used for 6 weeks. Active elbow flexion and extension were permitted, but the last part of the extension and overhead stretching was limited. The day immediately after the surgery patients began passive external rotation of the arm. The sling was removed after 6 weeks. Isoinertial strengthening and physiotherapy of the rotator cuff, deltoid and scapular were started at 10–12 weeks then surgery. Rehabilitative Physiotherapy was prolonged for 6 months. Substantial manual task and overhead activities were permitted 6 to 10 months post surgical treatment.
Sample size and power analysis
It was made a post hoc power analysis on our results with a specific statistical software (G*Power, version 3.1.2, Heinrich Heine University, Dusseldoerf, Germany). According to the post hoc power analysis, our study power to detect a significant difference is of 0.80 with and an alfa error of 0.05.
Statistics
The Statistics was elaborated utilizing the clinical and functional outcome scores. Then we studied active and passive ROM and strength of shoulder range of movement. The independent variables analyzed were: age; gender; arm dominance; history of trauma; size of the rotator cuff tear; biceps tendon break or tendinopathy; type of treatment of biceps tendon; configuration of the acromion. A two-tailed Mann-Whitney U test for continuous variables and the X2 test for categorical variables were used to evaluate each independent variable for the two patients groups. The outcome variables examined were analyzed using a two-tailed Mann-Whitney U test. The level of significativity was fixed at P < 0.05.
Results
Demographics
Demographic data and surgical details of the enrolled subjects are reported in Table 1. we noticed no significative differences among the groups in terms of age, gender, arm dominance, history of trauma, size of lesion, and shape of the acromion.
Clinical assessment
All patients had a follow up of at least 5 years. The comparison among the two patient categories respect to the duration of follow up did not show any significative difference for each questionnaire administered at 2 years. Between 2 to 5 year of follow up, the UCLA score was greater in the patients who underwent subacromial decompression. On the other hand, at five years of follow up, the group without subacromial decompression shown UCLA score significantly greater and OSS significantly lesser when equated with the group which underwent subacromial decompression (Table 2).
Regarding the shape of the acromion, no statistically significative differences were found for each questionnaire administered. (Table 3).
Functional assessment
Inter-group comparison according to the length of follow up did not display any significative difference in both passive and active ROM, and strength at each follow up time (Table 4).
Inter-group comparison according to the shape of the acromion did exhibit any significative difference for both passive and active ROM, and strength in subjects with acromion type I and III according to Bigliani’s classification. In subjects with acromion type II, the group without subacromial decompression displayed a significantly greater strength in extrarotation (Table 5).
Complications
No patient developed complications or clinical symptoms of RC re-tears.
Discussion
The principal finding of our job is that no significative difference respect to clinical outcome scores and functional outcomes revealed among subjects treated by RCR with or without subacromial decompression in every types of acromion by Bigliani’s classification. Moreover, according to the length of follow up, subjects who took RCR without subacromial decompression exhibited significantly superior long term clinical outcomes when compared with patients took by RCR with subacromial decompression.
Subacromial conflict syndrome is characterized by reduction of the subacromial space and alteration of the coraco-acromial arch [24,25,26]. It determines an irritation of the subacromial tissue with a major risk to develop a RC tear.
Morrison and Bigliani described three acromial shapes on outlet view radiographs (type I: flat undersurface; type II: curved; and type III: hooked) that raised with age and were related with RC tears. Several authors subsequently analyzed the possible relation between acromion morphologies and outcome after subacromial decompression. Gartsman and O’Connor showed that, in subjects with complete rotator cuff tear and acromion type II, acromioplasty did not bring to superior functional outcome [19]. Milano et al. [27], MacDonald et al. [28] and Abrams et al. [29] showed that acromion type exerted no significant influence on post-surgical functional scores. However, Abrams et al. [29] stated that a type III acromion harmed the Constant score, SST score, and VAS confronted with a type I acromion. Some authors suggested different causes related to the theory of impingement responsible of RC disease [16, 30]. Subacromial decompression is frequently performed in association with RCR. This procedure was effective in improving subacromial space, reducing subacromial tissue irritation, relieving pain and improving shoulder function [18, 31, 32]. However, no clinical studies have compared surgical issues with turning the acromion shape to a type 1 [16]. Moreover, several aspects of subacromial decompression as well as its role in association with RCR are still confusing or not well established.
The role of coraco-acromial ligament release is still debated, because it determines the destruction of coraco-acromial arch and may lead to the loss of active gleno-humeral elevation [33]. Furthermore, the release of the coraco-acromial ligament made together with acromioplasty determines the loss of secondary stabilizer of the humeral head against antero-superior migration and the consequent risk to develop rotator cuff pathology.
Indeed, the coracoacromial ligament was demonstrated to be the primary obstacle to superior dislocation of the humeral head, mainly if a large to massive RC lesion is present [34]. Finally, the current arthroscopic subacromial decompression technique generally recommends, if possible, the preservation of the coraco-acromial ligament [18, 31].
Acromioplasty is associated with a relevant percentage of satisfactory results [35, 36], and also massive and irreparable tears. However, its role is not clearly understood. In a nine-year follow up study of 96 subjects who took anterolateral acromioplasty, the RC disease progressed in 20% of them. The authors suggested other etiologic factors as causative of the condition. Another 9 year follow up cohort study found that more than one third of the subjects had RC disease advancement after anterolateral acromioplasty [37]. Anterolateral acromioplasty did not inhibit the advancement of the RC disease. In a systematic review of level I and level II studies, the authors made a comparison between the results of subacromial bursectomy with or without acromioplasty, concluding that, even though few high level randomized trials are available in the literature, similar results are obtained with subacromial bursectomy with or without acromioplasty [31]. In a systematic review and meta-analysis performed on four level I randomized studies including 373 patients, no significative differences in personal outcome successively to the arthroscopic RCR with or without acromioplasty at intermediate follow up were found [18]. Another level I randomized clinical trial, conducted on 120 patient with small or medium size rotator cuff tears, demonstrated that there were no significant variations concerning pain, ability of action, function and strength when comparing two groups of subjects underwent to RCR with or without acromioplasty [38]. These findings, therefore, suggest that acromioplasty could be no needful in the operative management of subjects with small- to medium-sized rotator cuff tears in lack of acromial spurs. Nevertheless, RCR failures are more frequently associated with other circumstances such as age, size of the RC tear, fatty degeneration of the tendons and intrinsic overload.
According to our results, significative differences about clinical and functional outcomes comparing arthroscopic RCR with or without subacromial decompression regardless of the shape of the acromion weren’t found. Moreover, patients without subacromial decompression exhibited superior clinical long term outcomes. For this reason, we believe that subacromial decompression procedure should be performed only in selected patients. It is possible that the worse outcome after spur resection was caused by degenerative changes of the tendon from the spur.
The primary point of strength of our study is that the two groups were homogeneous for all variables considered. Other forces are that two adequately prepared shoulder specialists made all the operations; two blinded examiners performed the follow-up evaluations and estimation of ROM and strength according to conventional guidelines.
We are conscious of our study limitations. First of all, the allocation of patients was not randomized, and the data were collected in a retrospective fashion; moreover, most of the patients allocated in the group 1 had a reduction of subacromial space because of an acromion type III or acromial spurs or acromioclavicular joint arthritis, and for this reason they underwent a subacromial decompression; we did not conduct an a precedent power analysis and sample size estimation, and we enrolled all the suitable subjectes trained in our hospital throughout the index period. However, the post hoc power analysis showed that the enrolled sample provided adequate power to justify the clinical relevance of our results.
Conclusion
The long term clinical outcomes resulted significantly higher in patients treated only with RCR respect the ones in patients underwent to RCR with subacromial decompression.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- MRI:
-
Magnetic Resonance Imaging
- N:
-
Newton
- OSS:
-
Oxford shoulder score
- RC:
-
Rotator cuff
- RCR:
-
Rotator cuff repair
- ROM:
-
Range of motion
- UCLA:
-
University of California at Los Angeles
References
Longo UG, Berton A, Papapietro N, Maffulli N, Denaro V. Epidemiology, genetics and biological factors of rotator cuff tears. Med Sport Sci. 2012;57:1–9.
Longo UG, Salvatore G, Rizzello G, Berton A, Ciuffreda M, Candela V, Denaro V. The burden of rotator cuff surgery in Italy: a nationwide registry study. Arch Orthop Trauma Surg. 2017;137(2):217–24.
Salvatore G, Longo UG, Candela V, Berton A, Migliorini F, Petrillo S, Ambrogioni LR, Denaro V. Epidemiology of rotator cuff surgery in Italy: regional variation in access to health care. Results from a 14-year nationwide registry. Musculoskelet Surg. 2019;28. https://doi.org/10.1007/s12306-019-00625-y. [Epub ahead of print] PubMed PMID: 31659710.
Rees JL. The pathogenesis and surgical treatment of tears of the rotator cuff. J Bone Joint Surg Br. 2008;90(7):827–32.
Piper CC, Hughes AJ, Ma Y, Wang H, Neviaser AS. Operative versus nonoperative treatment for the management of full-thickness rotator cuff tears: a systematic review and meta-analysis. J Shoulder Elb Surg. 2018;27(3):572–6.
Longo UG, Franceschi F, Ruzzini L, Spiezia F, Maffulli N, Denaro V. Higher fasting plasma glucose levels within the normoglycaemic range and rotator cuff tears. Br J Sports Med. 2009;43(4):284–7.
Longo UG, Franceschi F, Spiezia F, Marinozzi A, Maffulli N, Denaro V. The low-profile Roman bridge technique for knotless double-row repair of the rotator cuff. Arch Orthop Trauma Surg. 2011;131(3):357–61.
Franceschi F, Longo UG, Ruzzini L, Rizzello G, Maffulli N, Denaro V. Soft tissue tenodesis of the long head of the biceps tendon associated to the Roman bridge repair. BMC Musculoskelet Disord. 2008;9:78.
Franceschi F, Longo UG, Ruzzini L, Rizzello G, Maffulli N, Denaro V. The Roman bridge: a “double pulley - suture bridges” technique for rotator cuff repair. BMC Musculoskelet Disord. 2007;8:123.
Longo UG, Lamberti A, Rizzello G, Maffulli N, Denaro V. Synthetic augmentation in massive rotator cuff tears. Med Sport Sci. 2012;57:168–77.
Baldino L, Cardea S, Maffulli N, Reverchon E. Regeneration techniques for bone-to-tendon and muscle-to-tendon interfaces reconstruction. Br Med Bull. 2016;117(1):25–37.
Longo UG, Petrillo S, Rizzello G, Candela V, Denaro V. Deltoid muscle tropism does not influence the outcome of arthroscopic rotator cuff repair. Musculoskelet Surg. 2016;100(3):193–8.
Del Buono A, Oliva F, Longo UG, Rodeo SA, Orchard J, Denaro V, Maffulli N. Metalloproteases and rotator cuff disease. J Shoulder Elb Surg. 2012;21(2):200–8.
Neer CS. Impingement lesions. Clin Orthop Relat Res. 1983;173:70–7.
Neer CS. Anterior acromioplasty for the chronic impingement syndrome in the shoulder. 1972. J Bone Joint Surg Am. 2005;87(6):1399.
McFarland EG, Maffulli N, Del Buono A, Murrell GA, Garzon-Muvdi J, Petersen SA. Impingement is not impingement: the case for calling it “rotator cuff disease”. Muscles Ligaments Tendons J. 2013;3(3):196–200.
Longo UG, Berton A, Khan WS, Maffulli N, Denaro V. Histopathology of rotator cuff tears. Sports Med Arthrosc Rev. 2011;19(3):227–36.
Chahal J, Mall N, Macdonald PB, Van Thiel G, Cole BJ, Romeo AA, Verma NN. The role of subacromial decompression in patients undergoing arthroscopic repair of full-thickness tears of the rotator cuff: a systematic review and meta-analysis. Arthroscopy. 2012.
Gartsman GM, O’connor DP. Arthroscopic rotator cuff repair with and without arthroscopic subacromial decompression: a prospective, randomized study of one-year outcomes. J Shoulder Elb Surg. 2004;13(4):424–6.
Milano G, Grasso A, Salvatore M, Saccomanno MF, Deriu L, Fabbriciani C. Arthroscopic rotator cuff repair with metal and biodegradable suture anchors: a prospective randomized study. Arthroscopy. 2010;26(9 Suppl):S112–9.
Marchese C, Cristalli G, Pichi B, Manciocco V, Mercante G, Pellini R, Marchesi P, Sperduti I, Ruscito P, Spriano G. Italian cross-cultural adaptation and validation of three different scales for the evaluation of shoulder pain and dysfunction after neck dissection: University of California - Los Angeles (UCLA) Shoulder Scale, Shoulder Pain and Disability Index (SPADI) and Simple Shoulder Test (SST). Acta Otorhinolaryngol Ital. 2012;32(1):12–7.
Murena L, Vulcano E, D'Angelo F, Monti M, Cherubino P. Italian cross-cultural adaptation and validation of the Oxford shoulder score. J Shoulder Elb Surg. 2010;19(3):335–41.
Younis F, Sultan J, Dix S, Hughes PJ. The range of the Oxford shoulder score in the asymptomatic population: a marker for post-operative improvement. Ann R Coll Surg Engl. 2011;93(8):629–33.
Aydin A, Yildiz V, Kalali F, Yildirim OS, Topal M, Dostbil A. The role of acromion morphology in chronic subacromial impingement syndrome. Acta Orthop Belg. 2011;77(6):733–6.
Garofalo R, Karlsson J, Nordenson U, Cesari E, Conti M, Castagna A. Anterior-superior internal impingement of the shoulder: an evidence-based review. Knee Surg Sports Traumatol Arthrosc. 2010;18(12):1688–93.
de Witte PB, Nagels J, van Arkel ER, Visser CP, Nelissen RG, de Groot JH. Study protocol subacromial impingement syndrome: the identification of pathophysiologic mechanisms (SISTIM). BMC Musculoskelet Disord. 2011;12:282.
Milano G, Grasso A, Salvatore M, Zarelli D, Deriu L, Fabbriciani C. Arthroscopic rotator cuff repair with and without subacromial decompression: a prospective randomized study. Arthroscopy. 2007;23(1):81–8.
MacDonald P, McRae S, Leiter J, Mascarenhas R, Lapner P. Arthroscopic rotator cuff repair with and without acromioplasty in the treatment of full-thickness rotator cuff tears: a multicenter, randomized controlled trial. J Bone Joint Surg Am. 2011;93(21):1953–60.
Abrams GD, Gupta AK, Hussey KE, Tetteh ES, Karas V, Bach BR Jr, Cole BJ, Romeo AA, Verma NN. Arthroscopic repair of full-thickness rotator cuff tears with and without Acromioplasty: randomized prospective trial with 2-year follow-up. Am J Sports Med. 2014;42(6):1296–303.
Mulligan EP, Huang M, Dickson T, Khazzam M. The effect of Axioscapular and rotator cuff exercise training sequence in patients with subacromial impingement syndrome: a randomized crossover trial. Int J Sports Phys Ther. 2016;11(1):94–107.
Donigan JA, Wolf BR. Arthroscopic subacromial decompression: acromioplasty versus bursectomy alone--does it really matter? A systematic review. Iowa Orthop J. 2011;31:121–6.
Järvelä S, Järvelä T, Aho H, Kiviranta I. Arthroscopic subacromial decompression: outcome comparison between outpatient and hospitalized patients with 2- to 5-year follow-up. Scand J Surg. 2010;99(1):50–4.
Payne LZ, Deng XH, Craig EV, Torzilli PA, Warren RF. The combined dynamic and static contributions to subacromial impingement. A biomechanical analysis. Am J Sports Med. 1997;25(6):801–8.
Holt EM, Allibone RO. Anatomic variants of the coracoacromial ligament. J Shoulder Elbow Surg. 1995;4(5):370–5.
De Baere T, Dubuc JE, Joris D, Delloye C. Results of arthroscopic acromioplasty for chronic rotator cuff lesion. Acta Orthop Belg. 2004;70(6):520–4.
Cordasco FA, Backer M, Craig EV, Klein D, Warren RF. The partial-thickness rotator cuff tear: is acromioplasty without repair sufficient? Am J Sports Med. 2002;30(2):257–60.
Kartus J, Kartus C, Rostgard-Christensen L, Sernert N, Read J, Perko M. Long-term clinical and ultrasound evaluation after arthroscopic acromioplasty in patients with partial rotator cuff tears. Arthroscopy. 2006;22(1):44–9.
Shin SJ, Oh JH, Chung SW, Song MH. The efficacy of Acromioplasty in the arthroscopic repair of small- to medium-sized rotator cuff tears without acromial spur: prospective comparative study. Arthroscopy. 2012.
Acknowledgements
Not applicable.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript. UGL: manuscript preparation, study design, database interpretation and manuscript revision. SP: manuscript preparation, database interpretation and statistical analysis. VC, GR: manuscript preparation, figures and tables preparation, study design. ML: Manuscript preparation and database interpretation. VD, NM: Study design, manuscript revision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
the ethics committee of the university “Campus Bio Medico” of Rome approved the study and all patients gave written consent to participate.
Consent for publication
Written informed consent to publish this information was obtained from study participants. All the data are available for the consultation.
Competing interests
UGL is a member of the Editorial Board of BMC Musculoskeletal Disorders. The remaining authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Longo, U.G., Petrillo, S., Candela, V. et al. Arthroscopic rotator cuff repair with and without subacromial decompression is safe and effective: a clinical study. BMC Musculoskelet Disord 21, 24 (2020). https://doi.org/10.1186/s12891-019-3032-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-019-3032-z