Abstract
Background
Locomotive syndrome (LS) is associated with weakness and loss of function in the musculoskeletal organs. We aimed to determine the association between LS components and blood parameters in middle-aged and elderly individuals.
Methods
We included 223 middle-aged and elderly individuals in this study (104 men and 119 women; age: 40–85 years). All participants were asked to fast for at least 3 h before the venous blood samples were obtained and the hemoglobin, total protein, glycated hemoglobin (HbA1c), growth hormone, albumin and lipid profile were measured. Three functional tests, the stand-up test, the two-step test, and the 25-question geriatric locomotive function scale (GLFS) were used to assess the risk of LS. Walking speed was assessed by the 10-m walking test. Maximal isometric muscle strengths of the knee extensors were examined, and the weight bearing index (knee extension strength/body weight) was calculated. To assess an independent association between blood parameters and LS, the area under the receiver operating characteristic curve analysis (area under the curve, sensitivity, and specificity) and a binary logistic regression analysis were performed with adjustment for age.
Results
Of the 223 subjects, 119 (53.3%) fulfilled the diagnostic criteria for LS (including a two-step test score < 1.3, difficulty with one-leg standing from 40 cm in the stand-up test, and a 25-question GLFS score ≥ 7). Increased levels of HbA1c were significant risk factors for LS with an OR of 2.62 (OR95%CI = 1.43–4.80), as determined by a logistic regression analysis. Additionally, dehydroepiandrosterone-sulfate (DHEA-S) levels were significant only in the male subjects (OR = 0.992 [OR95%CI = 0.986–0.998]), at a threshold of 88 (AUC; 0.70, sensitivity; 79.6%, specificity; 49.1%). Moreover, 101 of 223 participants (41 men, 60 women) were analyzed for serum albumin levels, with a prevalence of LS at 55.4%, indicating that low levels of albumin were significant risk factors for LS (OR = 0.148 [OR95%CI = 0.023–0.954], p = 0.0445).
Conclusions
These results suggest that higher HbA1c and lower albumin are associated with the prevalence of LS in Japanese middle-aged and elderly individuals. Furthermore, low DHEA-S levels may be useful screening tools for LS in men.
Similar content being viewed by others
Background
Locomotive syndrome (LS) is the term proposed by the Japanese Orthopedic Association (JOA) to identify individuals with locomotive organ impairment [1]. LS leads to difficulties in the ability to stand, walk, run, climb stairs, and perform other physical functions essential to daily living and mobility [1]. This syndrome is caused by weakness and fragility of the function of musculoskeletal organs, such as bone, joint, and muscle. Any impairment in these organs results in pain, limited range of motion at the joints or spine, muscle weakness, and balance deficits, thereby resulting in limitations in the activities of daily living, reduction of quality of life, and necessity of nursing care [2]. Recently, LS evaluation methods have been established by the JOA, and include three functional tests: the stand-up test, two-step test, and 25-question geriatric locomotive function scale (GLFS) for assessing the risk of LS [3, 4].
Recent evidence has indicated that LS risk is ascertained by three risk indices that are based on age-dependent changes in healthy adults aged 23–95 years [1, 5]. Yoshimura et al. [1] examined the association between the LS risk test and a decline in mobility and demonstrated that three LS risk tests predict immobility and increased risk of LS. Moreover, Ogata et al. [5] determined whether these risk tests were beneficial as predictive screening programs for evaluating motor function and quality of life across a wide range of ages. Their findings suggest that this short battery of tests is a feasible tool for screening the adult population at risk of LS. Despite advances in screening methods of LS, the development of other predictive indicators of LS have not been established.
It is well known that blood parameters are effective screening tools for identifying the risk of metabolic syndrome and other multi-factorial diseases [6,7,8]. However, the association between blood parameters and LS has not been established in Japanese adults. Some investigators have demonstrated that dehydroepiandrosterone-sulfate (DHEA-S) has anti-aging effects [9], and circulating DHEA-S levels decline with age [10, 11]. Valenti et al. [12] revealed that low levels of DHEA-S are associated with muscle weakness in older men. Moreover, a decrease in the production of anabolic hormones, such as testosterone, growth hormone, and insulin-like growth factor-1 impairs the capacity of the skeletal muscles to incorporate amino acids and synthesize proteins [13]; therefore, these parameters were thought to be associated with the prevalence of LS. However, the association between these blood parameters and the components of LS remains unclear. Therefore, the purpose of this study was to determine the association between the components of LS and blood parameters in Japanese middle-aged and elderly people.
Methods
Subjects and measurements
We performed a cross-sectional analysis between May 2015 and November 2016. In total, 223 untrained community-dwelling middle-aged and elderly individuals (104 men and 119 women; ages: 40–85 years; mean height: 159.3 ± 8.2 cm; mean weight: 58.4 ± 9.5 kg) were included in this study. The participants had not performed any resistance training for at least 1 year prior to the start of the study. We excluded individuals who were unable to follow our instructions and those with chronic orthopedic conditions or any health or medical condition that limited the ability to undertake light-to-moderate walking. In addition, the participants completed a self-report questionnaire regarding medical history and comorbid conditions. All participants were informed about the contents of the study, and they provided a signed informed consent. This study was approved by the Ethics Committee of the Juntendo University (Approval Number: 27–10).
Body weight, skeletal muscle mass, fat mass, and percentage of body fat (% Fat) were measured via bioelectrical impedance analysis using a body composition analyzer (InBody730; Biospace). Venous blood samples of about 13 mL were obtained between 10:00 am and 5:00 pm after at least a 3-h fast, and the following parameters were analyzed: white blood cell (WBC) count, hematocrit (Hct) value, and levels of hemoglobin (Hb), total protein (TP), triglyceride (TG), low density lipoprotein (LDL)-cholesterol (C), high density lipoprotein (HDL)-C, HDL/LDL-C ratio, glycated hemoglobin (HbA1c) (National Glycohemoglobin Standardization Program [NGSP]), aspartate amino transferase (AST/GOT), alanine amino transferase (ALT/GPT), alkaline phosphatase (ALP), leucine aminopeptidase (LAP), γ-glutamyl transpeptidase (γ-GTP), growth hormone (GH), insulin-like growth factor-1 (IGF-1), testosterone, cortisol, dehydroepiandrosterone-sulfate (DHEA-S), and albumin. Of 223 participants, 101 (41 men, 60 women) were analyzed for albumin levels because we adopted it as an indicator after October 2015. All assays were performed by SRL Inc. (Tokyo, Japan).
After blood collection, all participants were measured for LS risk, walking speed, and maximal isometric muscle strength. LS risk tests (the stand-up test, two-step test, and 25-question GLFS) were performed as described previously [14]. Briefly, in the stand-up test, the participants were asked to stand from a sitting position on two legs or one leg, and from four different seat heights (40, 30, 20, and 10 cm). Participants were instructed to stand up without leaning back to gain momentum and to maintain the standing posture for at least 3 s. A score from “0” to “8” was allocated based on the difficulty, as described by Ogata et al. [5]. For the two-step test, participants stood with the toes of both feet behind the starting line and performed two maximal stride lengths, one with each foot, and the distance from the starting line was measured. The score was calculated as the length of the two steps (cm)/height (cm) [5]. The 25-question GLFS is a self-reported questionnaire, which is a comprehensive measure consisting of 25 items, including pain, activities of daily living, and mental health during the last month [3]. These 25 items were graded on a five-point scale, from 0 (no impairment) to 4 (severe impairment) points, with the scores summed to provide the total GLFS score; a higher GLFS score was associated with a higher risk of developing LS. Our previous study indicated that the measured variables from the stand-up test, two-step test, and GLFS have enough validity and reliability, with the intra-class correlation coefficients being 0.87, 0.93, and 0.76 and Cronbach’s α being 0.93, 0.95, and 0.88, respectively [14].
Walking speed was evaluated by timing each subject as they walked across a 10-m corridor on a hard-surfaced floor. They were asked to walk down the corridor as fast as possible without running. The maximum isometric strength of the knee extension was also measured (Takei, Tokyo, Japan) as described previously [14]. Each subject was seated on a chair with the hip joint angle at 90° flexion (0° = full hip extension), and they were instructed to perform maximum isometric knee extensions two or three times. The best recorded value was used as the representative one, and the weight bearing index (knee strength/body weight) was calculated.
Definition of locomotive syndrome
According to the results of the LS risk test, the participants were classified as having LS when a participant met one or more of the following criteria: (1) difficulty in standing from a seat at a height of 40 cm using one leg in the stand-up test (either leg), (2) two-step test score < 1.3, and (3) GLFS score ≥ 7 [15]. All other participants were placed in the non-LS group. In this study, we focused on the stage 1 of JOA definition of LS considered as LS group (including stage 1 and 2), and the independent values were compared between the LS and non-LS groups.
Statistical analysis
The data are presented as the mean ± standard deviation (SD). To compare the variables between the LS and non-LS groups, we used Student’s unpaired t-test. For variables that did not show normal distribution (for HbA1c levels and DHEA-S levels in males), the Mann-Whitney U test was used. The medians [interquartile ranges (IQRs)] are also presented for variables that did not show a normal distribution (i.e., for HbA1c and DHEA-S levels in males). The Benjamini-Hochberg procedure was performed to control the false discovery rate at 0.05 (used 14 tests for blood characteristics and biochemical examinations and 6 tests for hormone levels in males and females, respectively) [16]. To determine whether blood parameters were associated with LS risk, a binary logistic regression analysis (adjusted for age) was performed for HbA1c, DHEA-S levels in males, and albumin. We used the odds ratio (OR) and 95% confidence intervals (OR95%CI) to estimate the relative risk. A receiver operating characteristics (ROC) curve was used to select an appropriate cutoff and to determine the area under curve (AUC) and maximum sensitivity and specificity. Correlations between HbA1c and albumin levels and characteristics of participants [% Fat, body mass index (BMI), skeletal muscle mass, 10-m walking speed, and the weight bearing indices of knee extension] were analyzed using simple linear regression and Pearson’s correlation analysis. All of the statistical analyses were performed using the EZR package (Saitama Medical Center, Jichi Medical University) [17], which is a modified version of the R programming environment (The R Foundation for Statistical Computing, Vienna, Austria). The statistical significance level was set at p < 0.05.
Results
Characteristics of subjects
Table 1 shows the characteristics of the participants. In this study, 53.3% (119 of 223 participants: 55 men, 64 women) of participants fulfilled the diagnostic criteria for LS. Age, weight, and body fat percentage in the LS group were significantly higher than those in the non-LS (control) group (Table 1, p < 0.05). There was no significant difference between the non-LS and LS groups with respect to height, BMI, and total skeletal muscle mass (Table 1). The maximal isometric muscle strength of knee extension and the weight bearing indices of knee extension were significantly lower in the LS group than in the control group. Additionally, the 10-m walking speed was significantly lower in the LS group than in the control group. The stand-up and two-step test scores in the LS group were significantly lower than those in the non-LS group (3.95 ± 1.05 vs. 5.25 ± 0.57 and 1.34 ± 0.11 vs. 1.48 ± 0.10, respectively). In addition, the GLFS scores in the LS group were significantly higher than those in the non-LS group (6.03 ± 4.63 vs. 2.00 ± 1.70).
Blood characteristics and biochemical examinations
The blood parameters of the LS and non-LS groups are shown in Table 2 with adjusted p values. The LS group had higher HbA1c levels than the non-LS group (p < 0.05). However, no significant differences were observed in terms of WBC count, HDL/LDL-C ratio, and Hb, Hct, TP, TG, AST, ALT, ALP, LAP, and γ-GTP levels in both groups (p > 0.05).
An ROC analysis was conducted for each blood parameter, and the threshold for discriminating the non-LS and LS groups was identified, which was 5.7% for HbA1c (AUC; 0.64, sensitivity; 70.2%, specificity; 54.6%). A higher HbA1c level was a significant risk factor for LS, with an OR of 2.62 (OR95%CI = 1.43–4.80), as determined by the logistic regression analysis (p = 0.0018).
The linear regression analysis revealed significant positive or negative correlations between HbA1c level and BMI or 10-m walking speed (BMI, r = 0.1628; 10-walking speed, r = − 0.2206, p < 0.05) (Table 3). In addition, significant differences were present in HbA1c level between LS and non-LS when the two functional tests (stand-up test or two-step test) were used for classification (p = 0.0008 or p = 0.132) (Table 4).
Hormone levels
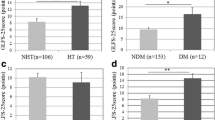
Figure 1(A-F) shows the comparison of blood hormone concentrations between the non-LS and LS groups in the male and female participants. The two-way ANOVA revealed that there was an association between the prevalence of LS and DHEA-S level, and the male participants had significantly higher DHEA-S levels than the female participants (Fig. 1F). In addition, DHEA-S levels in male participants were significantly lower in the LS group than in the non-LS group (men in non-LS: 148.1 ± 85.5; men in LS: 106.6 ± 61.0; women in non-LS group: 88.7 ± 51.8; women in LS group; 77.1 ± 37.5 μg/dL). The levels of other hormones did not present statistically significant difference regardless of LS risk in both sexes.
Comparison of blood hormone concentrations between non-locomotive syndrome and locomotive syndrome in male and female participants. a) GH, b) IGF-1, c) Testosterone, d) Cortisol, e) Testosterone/Cortisol ratio, and f) DHEA-S levels. Values are means ± standard division (SD). The medians [interquartile ranges (IQRs)] are presented for DHEA-S levels in males, which did not show normal distribution: 119.0 (94.0–174.5) for non-LS and 93.0 (61.0–150.8) for LS. GH: growth hormone, IGF-1: insulin-like growth factor-1, DHEA-S: dehydroepiandrosterone-sulfate. □:Non-LS participant, ■: LS participant. * p < 0.05 vs. each gender. The results of two-way ANOVA are displayed
In the male subjects, the ROC analysis indicated that the cutoff point was 88 μg/dL (AUC; 0.70, sensitivity; 80.2%, specificity; 59.8%), and low level of DHEA-S was a significant risk factor for LS (p = 0.0088) with an OR of 0.992 (OR95%CI = 0.986–0.998).
Albumin level
The level of serum albumin is shown in Fig. 2. In the current study, the blood samples of 101 of 223 participants (41 men, 60 women) were analyzed for serum albumin level, with an LS prevalence of 55.4% (56 of 101, 24 men, 32 women). This LS prevalence was approximately equivalent to the cohort of our study (119 of 223 [53.3%]; 55 men, 64 women) (Fig. 3). Serum albumin level was significantly lower in the LS group than in the non-LS group (non-LS vs LS: 4.40 ± 0.27 vs. 4.26 ± 0.22%, p = 0.0070). Moreover, 29 of 56 (51.8%) and 12 of 45 (26.7%) participants had low albumin levels in the LS and non-LS groups, respectively.
Moreover, the ROC analysis indicated that the cutoff point was 4.3 g/dL for albumin (AUC; 0.69, sensitivity; 58.8%, specificity; 79.9%), and high level of albumin significantly lowered the LS risk (p = 0.0445) with an OR of 0.148 (OR95%CI = 0.023–0.954).
Additionally, significant correlations were observed between albumin level and % Fat or albumin and total skeletal muscle mass (% Fat, r = 0.2149; skeletal muscle mass, r = − 0.2196, p < 0.05) (Table 3). Furthermore, there were significant differences in albumin level between LS and non-LS when the two-step test were used (p = 0.0178) (Table 4).
Discussion
This study aimed to determine the association between the components of LS and blood parameters in the Japanese middle-aged and elderly people. In our study, 119 of 223 subjects (53.3%) fulfilled the diagnostic criteria for LS. The participants with LS had lower relative knee extension strength (weight bearing index of knee extension) and slower walking speeds than the non-LS participants, suggesting that the onset of mobility decline is diagnosed in accordance with previous cross-sectional studies [1, 5, 18]. The present study demonstrated, for the first time to the best of our knowledge, that higher levels of HbA1c and lower serum albumin were associated with the prevalence of LS in the Japanese middle-aged and elderly people. Furthermore, DHEA-S levels may be a useful screening tool for LS in men.
The main findings of this study were that higher HbA1c levels were associated with a higher prevalence of LS, and that the OR for participants with levels above the threshold value was 2.62 in the LS group. Our data suggest that the participants with HbA1c level ≥ 5.7% had a higher risk of LS than those with HbA1c level < 5.7% among the Japanese middle-aged and elderly individuals. HbA1c, one of the diagnostic criteria for diabetes, is the most widely used indicator of glucose control, and can be used to assess overall metabolic control over the preceding 6–8 weeks [19]. The American Diabetes Association and the World Health Organization recently proposed the use of HbA1c to diagnose diabetes at threshold levels of 6.5% (48 mmoL/moL) and to identify individuals at high risk of developing type 2 diabetes based on a cutoff value of 5.7% (39 mmoL/moL) [20, 21]. In contrast, a meta-analysis by Boulé et al. [22] demonstrated that reductions in the HbA1c levels following an aerobic training program in diabetic patients were better predicted by exercise intensity than by exercise volume. Moreover, our data showed that the HbA1c level negatively correlated with the maximal 10-m walking speed and positively correlated with the BMI; therefore, HbA1c levels seem to be higher in individuals who do not regularly perform exercise or who maintain reduced physical activity. Although the relationship between LS and other diseases, such as diabetes, cardiovascular disease, and other age-related diseases, is unknown, we nonetheless consider that higher HbA1c levels may be one of the characteristics of increased risk of LS among Japanese middle-aged and elderly people.
In the present study, the prevalence of LS was higher in men with lower DHEA-S levels (cutoff: 88 μg/dL). Indeed, although we could not show a linear relationship between DHEA-S level and physical function (muscle strength and gait speed, data not shown), LS men subjects exhibited lower muscle strength in knee extension in accordance with the results of a previous study by Valenti et al. [12]. DHEA-S is an endogenously produced sex steroid that has been hypothesized to have anti-aging effects [9]. Circulating DHEA-S levels decline significantly with age, resulting in mean levels at the age of 65 years being less than one fifth of those at the age of 20 years, according to cross-sectional [11] and longitudinal [10] studies. Moreover, several studies have demonstrated that low levels of DHEA-S are associated with cardiovascular disease [23] and muscle weakness [12] in older men. In older women, either low or high levels of DHEA-S compared to reference levels, confer a greater risk of death (cardiovascular or cancer mortality) than do intermediate levels [24]. Considering that several longitudinal studies have confirmed that 30% of individuals older than 65 years do not experience a decline in DHEA-S levels [25,26,27]; therefore, the clinical significance of DHEA-S remains unclear. Moreover, there were no associations between DHEA-S levels and LS in women. This may be due to sex differences in the DHEA-S levels (women tend to have lower levels of DHEA-S), suggesting that the physiological significance of DHEA-S in women may be less. Therefore, more research is needed to determine whether targeted DHEA-S supplementation would provide clinical benefit for preventing LS in men. Nonetheless, our data suggest that low DHEA-S levels may be a useful tool for identifying increased risk of LS in middle-aged and older men.
Interestingly, we also found that lower levels of serum albumin (< 4.3 g/dL) were significant risk factors for LS. In general, serum albumin is a marker of nutritional condition [28], acts as an antioxidant [29], and is a plasma volume expander [30]. Although, we have no data to support the relationship between reduced albumin level and LS, lower levels of serum albumin may be associated with a decline in the muscle mass. LS is partly caused by weakness and loss of skeletal muscle with aging, so called sarcopenia, which results in drastically reduced qualities of life, and leads to an increased risk for the development of insulin resistance and various diseases [31, 32]. Our data indicated that the albumin level was negatively correlated with the total skeletal muscle mass measured via bioelectrical impedance analysis. Consequently, a lower level of albumin may be associated with decline in the skeletal muscle mass, thus appearing to be related to increased risk of LS. Although it was sufficient to detect statistically significant changes in the variables, the sample size for the serum albumin analysis was relatively small (n = 101 [41 men, 60 women]) compared to the other blood parameters (n = 223) in the present study. Therefore, additional studies are required to clarify the significance of serum albumin levels in predicting an increased risk for LS among Japanese middle-aged and elderly individuals.
Limitations
This study had several limitations. First, the sample size of 223 was small, particularly, the sample size that underwent albumin analysis (101 of 223). Second, we did not control the diet before the experiment. Although we had taken the blood samples after at least a 3-h fast, we did not analyze the influence of diet intake on the blood parameters. Third, we could not examine the causal relationship between HbA1c, DHEA-S (for men), and albumin levels and LS because of the cross-sectional study design. Therefore, a future follow-up study is necessary to clarify the causal relationships among these factors. Fourth, our participants were limited to relatively healthy individuals, especially elderly people; therefore, our findings may not be extrapolated to the entire Japanese population. Finally, as shown in Table 4, there were significant differences in HbA1c and Albumin levels between LS and non-LS for the two functional tests (stand-up test and/or two-step test), while not for GLFS-25. That is, given that the criteria of LS would differ by measurement tools (functional tests or GLFS-25), future studies should be focused on the optimized criteria of the LS to predict an increased risk for LS with higher accuracy. Despite these limitations, our data first demonstrated that higher levels of HbA1c and lower levels of serum albumin were associated with a higher prevalence of LS among the Japanese middle-aged and elderly individuals.
Conclusions
Our data suggested that higher HbA1c and lower albumin levels were associated with a higher prevalence of LS among the Japanese middle-aged and elderly people. Furthermore, low DHEA-S levels may be a useful screening tool for LS in men.
Abbreviations
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine amino transferase
- AST:
-
Aspartate amino transferase
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- DHEA-S:
-
Dehydroepiandrosterone-sulfate
- GH:
-
Growth hormone
- GLFS:
-
Geriatric locomotive function scale
- Hb:
-
Hemoglobin
- HbA1c:
-
Glycated hemoglobin
- Hct:
-
Hematocrit
- HDL-C:
-
High-density lipoprotein cholesterol.
- IGF-1:
-
Insulin-like growth factor-1
- IQR:
-
Interquartile range
- JOA:
-
Japanese Orthopedic Association
- LAP:
-
Leucine aminopeptidase
- LDL-C:
-
Low-density lipoprotein cholesterol
- LS:
-
Locomotive syndrome
- NGSP:
-
National Glycohemoglobin Standardization Program
- OR:
-
Odds ratio
- ROC:
-
Receiver operating characteristics
- SD:
-
Standard deviation
- TG:
-
Triglyceride
- TP:
-
Total protein.
- WBC:
-
White blood cell
- γ-GTP:
-
γ-glutamyl transpeptidase
References
Yoshimura N, Muraki S, Oka H, Tanaka S, Ogata T, Kawaguchi H, Akune T, Nakamura K. Association between new indices in the locomotive syndrome risk test and decline in mobility: third survey of the ROAD study. J Orthop Sci. 2015;20(5):896–905.
Hirano K, Imagama S, Hasegawa Y, Wakao N, Muramoto A, Ishiguro N. Impact of spinal imbalance and back muscle strength on locomotive syndrome in community-living elderly people. J Orthop Sci. 2012;17(5):532–7.
Seichi A, Hoshino Y, Doi T, Akai M, Tobimatsu Y, Iwaya T. Development of a screening tool for risk of locomotive syndrome in the elderly: the 25-question geriatric locomotive function scale. J Orthop Sci. 2012;17(2):163–72.
Matsumoto H, Hagino H, Wada T, Kobayashi E. Locomotive syndrome presents a risk for falls and fractures in the elderly Japanese population. Osteoporos Sarcopenia. 2016;2(3):156–63.
Ogata T, Muranaga S, Ishibashi H, Ohe T, Izumida R, Yoshimura N, Iwaya T, Nakamura K. Development of a screening program to assess motor function in the adult population: a cross-sectional observational study. J Orthop Sci. 2015;20(5):888–95.
Mukai N, Doi Y, Ninomiya T, Hata J, Hirakawa Y, Fukuhara M, Iwase M, Kiyohara Y. Cut-off values of fasting and post-load plasma glucose and HbA1c for predicting type 2 diabetes in community-dwelling Japanese subjects: the Hisayama study. Diabet Med. 2012;29(1):99–106.
Arai H, Yamamoto A, Matsuzawa Y, Saito Y, Yamada N, Oikawa S, Mabuchi H, Teramoto T, Sasaki J, Nakaya N, et al. Prevalence of metabolic syndrome in the general Japanese population in 2000. J Atheroscler Thromb. 2006;13(4):202–8.
Pellicano R, Oliaro E, Fagoonee S, Astegiano M, Berrutti M, Saracco G, Smedile A, Repici A, Leone N, Castelli A, et al. Clinical and biochemical parameters related to cardiovascular disease after helicobacter pylori eradication. Int Angiol. 2009;28(6):469–73.
Nawata H, Yanase T, Goto K, Okabe T, Ashida K. Mechanism of action of anti-aging DHEA-S and the replacement of DHEA-S. Mech Ageing Dev. 2002;123(8):1101–6.
Nafziger AN, Bowlin SJ, Jenkins PL, Pearson TA. Longitudinal changes in dehydroepiandrosterone concentrations in men and women. J Lab Clin Med. 1998;131(4):316–23.
Orentreich N, Brind JL, Rizer RL, Vogelman JH. Age changes and sex differences in serum dehydroepiandrosterone sulfate concentrations throughout adulthood. J Clin Endocrinol Metab. 1984;59(3):551–5.
Valenti G, Denti L, Maggio M, Ceda G, Volpato S, Bandinelli S, Ceresini G, Cappola A, Guralnik JM, Ferrucci L. Effect of DHEAS on skeletal muscle over the life span: the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2004;59(5):466–72.
Deschenes MR. Effects of aging on muscle fibre type and size. Sports Med. 2004;34(12):809–24.
Yoshihara T, Ozaki H, Nakagata T, Natsume T, Kitada T, Ishihara Y, Deng P, Osawa T, Ishibashi M, Ishijima M, et al. Effects of a progressive walking program on the risk of developing locomotive syndrome in elderly Japanese people: a single-arm trial. J Phys Ther Sci. 2018;30(9):1180–6.
Nakamura K, Ogata T. Locomotive syndrome: definition and management. Clin Rev Bone Miner Metab. 2016;14:56–67.
Benjamini Y, Drai D, Elmer G, Kafkafi N, Golani I. Controlling the false discovery rate in behavior genetics research. Behav Brain Res. 2001;125(1–2):279–84.
Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
Sasaki E, Ishibashi Y, Tsuda E, Ono A, Yamamoto Y, Inoue R, Takahashi I, Umeda T, Nakaji S. Evaluation of locomotive disability using loco-check: a cross-sectional study in the Japanese general population. J Orthop Sci. 2013;18(1):121–9.
Nathan DM, Turgeon H, Regan S. Relationship between glycated haemoglobin levels and mean glucose levels over time. Diabetologia. 2007;50(11):2239–44.
Association AD. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–9.
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation World Health Organ Tech Rep Ser. 2000;894(i-xii):1–253.
Boule NG, Kenny GP, Haddad E, Wells GA, Sigal RJ. Meta-analysis of the effect of structured exercise training on cardiorespiratory fitness in type 2 diabetes mellitus. Diabetologia. 2003;46(8):1071–81.
Tchernof A, Labrie F. Dehydroepiandrosterone, obesity and cardiovascular disease risk: a review of human studies. Eur J Endocrinol. 2004;151(1):1–14.
Cappola AR, Xue QL, Walston JD, Leng SX, Ferrucci L, Guralnik J, Fried LP. DHEAS levels and mortality in disabled older women: the Women's health and aging study I. J Gerontol A Biol Sci Med Sci. 2006;61(9):957–62.
Kahonen MH, Tilvis RS, Jolkkonen J, Pitkala K, Harkonen M. Predictors and clinical significance of declining plasma dehydroepiandrosterone sulfate in old age. Aging (Milano). 2000;12(4):308–14.
Mazat L, Lafont S, Berr C, Debuire B, Tessier JF, Dartigues JF, Baulieu EE. Prospective measurements of dehydroepiandrosterone sulfate in a cohort of elderly subjects: relationship to gender, subjective health, smoking habits, and 10-year mortality. Proc Natl Acad Sci U S A. 2001;98(14):8145–50.
Orentreich N, Brind JL, Vogelman JH, Andres R, Baldwin H. Long-term longitudinal measurements of plasma dehydroepiandrosterone sulfate in normal men. J Clin Endocrinol Metab. 1992;75(4):1002–4.
Harris D, Haboubi N. Malnutrition screening in the elderly population. J R Soc Med. 2005;98(9):411–4.
Roche M, Rondeau P, Singh NR, Tarnus E, Bourdon E. The antioxidant properties of serum albumin. FEBS Lett. 2008;582(13):1783–7.
Arroyo V. Human serum albumin: not just a plasma volume expander. Hepatology. 2009;50(2):355–7.
Keller K, Engelhardt M. Strength and muscle mass loss with aging process. Age and strength loss. Muscles Ligaments Tendons J. 2013;3(4):346–50.
Kalyani RR, Corriere M, Ferrucci L. Age-related and disease-related muscle loss: the effect of diabetes, obesity, and other diseases. Lancet Diabetes Endocrinol. 2014;2(10):819–29.
Acknowledgements
We would like to thank Editage (www.editage.jp) for English language editing.
Funding
This research was supported by the Center of Innovation (COI) Program from Japan Science and Technology Agency (JST). The program is one of the main funding programs under the Center of Innovation Science and Technology based Radical Innovation and Entrepreneurship Program (COI STREAM), which was launched in 2013 by the Ministry of Education, Culture, Sports, Science and Technology (MEXT). The funding source had no control over the interpretation, writing, or publication of this work. The corresponding author had full access to all the data in the study and had the final responsibility of the decision to submit for publication.
Availability of data and materials
All data generated or analyzed during this study are included in this article.
Author information
Authors and Affiliations
Contributions
T.Y. designed and performed experiments, analyzed and interpreted data, and prepared the manuscript. H.O., Ta.N, To.N., T.K., Y.I., and S.S. performed the LS risk, walking speed, and maximal isometric muscle strength measurements. M.I. contributed in the statistical analysis, preparation of the manuscript, and in the discussion. H.K. was responsible for medical examination of the participants. S.M. and H.N. contributed to the manuscript preparation and to the discussion, and they are the guarantors of this work. All the authors reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants were informed about the content of the study and provided a signed informed consent. This study was approved by the Ethics Committee of the Juntendo University (Approval Number: 27–10).
Consent for publication
Not Applicable.
Competing interests
None.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Yoshihara, T., Ozaki, H., Nakagata, T. et al. Association between locomotive syndrome and blood parameters in Japanese middle-aged and elderly individuals: a cross-sectional study. BMC Musculoskelet Disord 20, 104 (2019). https://doi.org/10.1186/s12891-019-2480-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-019-2480-9