Abstract
Background
Big data research is important for studying uncommon diseases in real-world settings. Most big data studies in axial spondyloarthritis (axSpA) have been limited to populations identified with billing codes for ankylosing spondylitis (AS). axSpA is a more inclusive concept, and reliance on AS codes does not produce a comprehensive axSpA study population. The first objective was to describe our process for establishing an appropriate sample of patients with and without axSpA for developing accurate axSpA identification methods. The second objective was to determine the classification performance of AS billing codes against the chart-reviewed axSpA reference standard.
Methods
Veteran Health Affairs clinical and administrative data, between January 2005 and June 2015, were used to randomly select patients with clinical phenotypes that represented high, moderate, and low likelihoods of an axSpA diagnosis. With chart review, the sampled patients were classified as Yes axSpA, No axSpA or Uncertain axSpA, and these classification assignments were used as the reference standard for determining the positive predictive value (PPV) and sensitivity of AS ICD-9 codes for axSpA.
Results
Six hundred patients were classified as Yes axSpA (26.8%), No axSpA (68.3%), or Uncertain axSpA (4.8%). The PPV and sensitivity of an AS ICD-9 code for axSpA were 83.3% and 57.3%, respectively.
Conclusions
Standard methods of identifying axSpA patients in a large dataset lacked sensitivity. An appropriate sample of patients with and without axSpA was established and characterized for developing novel axSpA identification methods that are anticipated to enable previously impractical big data research.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Big data research is necessary for studying uncommon diseases and outcomes in real-world settings [1]. Big data research is particularly important for spondyloarthritis (SpA), since concepts of SpA have broadened in recent years [2]. The axial SpA (axSpA) concept was introduced in 2009 [3], when it became apparent from advances in imaging and treatment that nearly one-half of patients with an axial inflammatory arthritis phenotype were excluded from traditional axSpA definitions (i.e. ankylosing spondylitis [AS]) [4]. Despite the growing recognition of more inclusive axSpA concepts, big data axSpA studies continue to be limited to the AS subtype [5,6,7,8,9], since there are no billing codes for non-AS subtypes. In more broadly defined axSpA populations, little is known about real-life outcomes, such as comorbidities, mortality, diagnostic and treatment patterns, health care utilization , and costs [10]. New methods of identifying axSpA patients are needed for a wide range of big data research in axSpA.
In order to develop and evaluate new axSpA identification methods, an appropriate sample of patients with and without axSpA is needed [11]. The ideal approach is to screen patients from the general population and classify them as having or not having axSpA. This approach is impractical for uncommon diseases, like axSpA, since tens of thousands of patients would need to be screened to identify a sufficient number of axSpA patients for research.
For feasibility purposes, patient populations are frequently enriched with patients at high risk of having the outcome of interest [12, 13]. For example, in an axSpA radiographic progression study, the population may consist of patients at elevated risk for structural disease progression (elevated C-Reactive Protein or baseline syndesmophytes) [14]. A disadvantage of this high-risk sampling approach is that the generalizability of the study results is limited by excluding lower risk patients (i.e. the results of the radiographic progression studies cannot be applied to axSpA patients without an elevated CRP or baseline syndesmophytes).
An alternative approach is to include both patients with high and low risk of disease. The sampled population is enriched for the disease of interest by including a greater percentage of patients at high risk than occurs in the general population. To improve generalizability, people at low risk are also required to be included in the sampled population. Compared to the distribution of high and low risk people in the general population, people at high risk for the disease are over-sampled and people at low risk are under-sampled [15]. This risk stratification sampling approach balances the advantages of feasibility with enrichment of high risk patients vs. generalizability with inclusion of low risk patients.
The first objective of this study was to describe our sampling strategy and chart-review process for establishing an appropriate sample of patients with and without axSpA for the future development of accurate axSpA identification methods for big data research. The second objective was to determine the classification performance of the International Classification of Diseases- Ninth Revision (ICD-9) code for AS against the chart-reviewed axSpA reference standard.
Methods
Design, setting, and data sources
This retrospective study used data from Veterans enrolled in the Veterans Health Administration (VHA). The data source was the Corporate Data Warehouse, a national repository of data from the VHA medical record system (VistA) and other VHA clinical and administrative systems [16]. The patient Integration Control Number was used to link patients across VHA stations. Data were housed and analyzed within the Veterans Affairs Informatics and Computing Infrastructure (VINCI) [17].
Patient sampling strategy
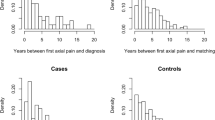
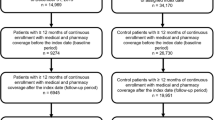
The sampled population consisted of 600 randomly selected Veterans with conditions representing high (n = 200), moderate (n = 200), and low (n = 200) risk for axSpA, between January 1, 2005 to June 30, 2015. Structured Query Language (SQL) server newid function was used for randomization [18]. Veterans were considered by clinical experts to be at high risk for having axSpA if they had ≥1 AS ICD-9 code or a clinically available positive HLA-B27 result. Veterans with ICD-9 codes for sacroiliitis or a non-AS SpA subtypes (psoriatic arthritis, undifferentiated spondyloarthritis, reactive arthritis, and enteropathic arthritis) were categorized as moderate axSpA risk. The low risk category included patients with chronic back pain or other diseases that may mimic SpA [rheumatoid arthritis, diffuse idiopathic skeletal hyperostosis (DISH), crystal arthritis (gout and pseudogout), and other types of inflammatory arthritis (connective tissue disease, vasculitis, polymyalgia rheumatic, sarcoidosis, Paget’s disease)].
AxSpA classification by chart review
Methods for classifying patients as having or not having axSpA occurred in multiple steps. First, clinical experts determined concepts that were expected to be useful for classification assignments. The concept categories included diagnostic language, disease features, laboratory results, and medications. Diagnostic language included statements affirming or negating the presence of SpA or an alternative diagnosis (i.e. “Mr. X has ank spond…”, “there is no evidence of spondyloarthritis”, or “her back pain is due to a herniated disk”. Disease features included language affirming or negating sacroiliitis, uveitis, enthesitis, inflammatory arthritis, dactylitis, psoriasis, inflammatory bowel disease, and syndesmophytes. Disease modifying anti-rheumatic drugs (DMARDs) included apremilast, leflunomide, methotrexate, sulfasalazine, adalimumab, certolizumab, etanercept, golimumab, infliximab, rituximab, and ustekinumab. Laboratory results included HLA-B27 positivity, elevated erythrocyte sedimentation rate, elevated C-reactive protein, rheumatoid factor, and anti-cyclic citrullinated protein.
Second, data were extracted for the 600 sampled patients. Four types of data were included: provider notes, imaging reports, laboratory results, and medications. For provider notes, all Text Integration Utility notes from primary care, rheumatology, orthopedics, gastroenterology, dermatology, ophthalmology, physical medicine and rehabilitation, pain clinics, geriatrics, emergency medicine, urgent care, and podiatry were extracted. Imaging reports were extracted with note titles indicating inclusion of a joint (neck, shoulder, elbow, wrist, hand, finger, pelvis, sacroiliac joint, hip, spine, knee, ankle, feet, and toe). The laboratory results were extracted by their Logical Observation Identifiers Names and Codes (LOINC) [19]. Quality review and revisions were used to ensure correct mapping and to standardize laboratory values. DMARD exposure data were extracted for all DMARDs dispensed during the study period.
Third, annotation software (eHOST [20]) was adapted and applied to the 600 sampled patients. A customized user interface was built for eHOST that enabled reviewers to efficiently view the extracted provider notes, imaging, laboratory results, and medications on a single screen, for the purpose of making patient-level classifications. Data were extracted and displayed in a manner that maintained the sequential nature and prioritization of the relevant documents. Annotation functions were designed for the reviewers to highlight and annotate the sections of text that were used to make classification decisions. Classification categories for axSpA status included Yes axSpA, No axSpA, and Uncertain axSpA. The uncertain category was assigned to patients with conflicting information or an axSpA diagnosis without additional information to support an axSpA diagnosis.
Two rheumatologists (JAW and GKP) independently annotated and classified the sampled patients. Classification guidelines were developed and revised. The protocol required reviewers, at a minimum, to assess specific types of documents (rheumatology consults and most recent rheumatology note, all articular imaging reports, dermatology notes, etc.). Additionally, the eHOST software was programmed to pre-annotate (highlight) every mention of terms relevant to axSpA (ankylosing spondylitis, spondyloarthr*, iritis, uveitis, dactylitis, enthesitis, erosion, *B27, etc.) in each document. After completing the initial annotation of the required documents (without pre-annotation), the reviewers annotated the pre-annotated terms that were not captured with the chart reviewers' previous annotation, to minimize the risk of overlooking data relevant to classification assignments. Both reviewers completed chart review classifications in batches of 20 until inter-rater agreement exceeded 85%. Discrepancies were adjudicated. After the 85% inter-rater agreement goal was achieved, the remainder of the sampled population was classified by a single reviewer.
Characterizing the chart-reviewed population and evaluating AS ICD-9 codes
The demographics and health care utilization of the sampled patients were described in three groups: Yes axSpA, No axSpA, and Uncertain axSpA. Health care utilization was measured with duration of active VA system use during the study period (time between initial and most recent encounter with a provider or medication dispensation) and mean number of provider visits per year. The PPV of an AS ICD-9 code for axSpA was calculated in all patients with ≥1 ICD-9 code for AS [21]. The sensitivity of an AS ICD-9 code for axSpA was calculated in the subset who were not specifically selected to the sampled population because of an AS ICD-9 code. For PPV and sensitivity calculations, patients with sufficient evidence of axSpA (Yes axSpA) were compared to patients with insufficient evidence of axSpA (No axSpA and Uncertain axSpA). For confidence intervals, exact binomial confidence intervals were used for categorical variables and normal approximation was used for continuous variables.
Results
Patient population
During the study period, 9,803,429 Veterans participated in the VHA system. Patients eligible for selection into the sampled population included Veterans with ICD-9 codes for specific diseases or a laboratory result that placed them at high, moderate and low risk for axSpA (Table 1). Six hundred Veterans were randomly selected, including 0.83% of Veterans from the high risk stratum (n = 200), 0.25% from the moderate risk stratum (n = 200), and 0.01% from the low risk stratum (n = 200). Among the 600 sampled Veterans, 162 (27.0%) were classified as Yes axSpA, 409 (68.2%) were classified as No axSpA, and 29 (4.8%) were classified as Uncertain axSpA (Table 2). Within the group selected from the high risk stratum, 87% with an AS ICD-9 code were classified as Yes axSpA, while 38% of patients with a clinically available positive HLA-B27 result were classified as Yes axSpA. In the moderate risk groups, 27% with an ICD-9 code for a non-AS SpA subtype were classified as Yes axSpA and 7% with a sacroiliitis ICD-9 code were classified as Yes axSpA. In the low risk category, 2% of patients with an ICD-9 code for a SpA mimic were classified as Yes axSpA, and 1% of patients with ICD-9 codes chronic back pain were classified as Yes axSpA. The demographics and health care utilization patterns of the sampled population were similar between the Yes axSpA group and the No axSpA group, with the exception of younger age (56.2 vs. 59.9) and higher percentage of males (95.7% vs. 88.8%) in the Yes axSpA group (Table 3).
Performance of AS diagnosis codes for classifying axSpA
Among the 156 axSpA patients with an AS ICD-9 code, the PPV of the AS ICD-9 code for axSpA was 83.3% (Fig. 1). Within the 75 axSpA patients who were not specifically selected to into the sampled population because of an AS ICD-9 code, the sensitivity of an AS ICD-9 code for axSpA was 57.3%.
Discussion
We established and characterized an appropriate sample of patients with and without axSpA for developing novel axSpA identification methods and for evaluating AS billing codes in axSpA patients. This population is enriched with axSpA patients and is representative of more generalizable disease states (i.e. chronic back pain). Additionally, patients were included with diseases that may mimic axSpA (DISH, peripheral psoriatic arthritis, crystal arthritis, etc.) to maximize the ability of axSpA identification methods to differentiate between axSpA and axSpA mimics. These sampled patients will be used to identify and prioritize data that differentiate between patients with and without axSpA, for the development of novel axSpA classification algorithms.
The evaluation of the AS ICD-9 code demonstrated a reasonably high PPV for axSpA (83.3%). This is similar to the PPV of ≥1 AS ICD-9 code for AS reported in a Veteran population attending rheumatology clinics (83%) [22]. However, the PPV estimates in both of these studies are likely overestimated compared to the PPV in the general population, since these population were enriched with AS patients, and PPV estimates increase when the prevalence of the underlying condition increases.
The sensitivity of the AS ICD-9 code for axSpA was low (57%). Not all patients with axSpA have AS, since axSpA also includes non-AS subtypes. However, it is likely that providers used the AS ICD-9 code as a proxy for non-AS axSpA subtypes, since there are no billing codes for non-AS axSpA subtypes. While precise usage patterns of AS billing codes remain unknown, the lack of an AS ICD-9 code in 43% of axSpA patients over the 10.5 year study period, demonstrated that nearly one-half of axSpA patients were not identifiable with the only ICD-9 billing code that indicates that presence of inflammatory axial arthritis.
Strengths of this study include the large sample size and access to a medical record system that enabled consistent data capture across VHA sites throughout the United States. Furthermore, the chart review process was feasible for comprehensive review of multiple types of data for several hundred patients over a period exceeding 10 years. Another strength was the clinical expertise of the chart reviewers. As rheumatologists specializing in SpA within the VA system, both reviewers are experienced with the intricacies of axSpA patient care and documentation within the VA system.
This study was limited by the inability of chart reviewers to directly interact with patients or access digital radiologic images (radiology reports were reviewed). Thus, classification decisions had to be made with incomplete and otherwise imperfect data. These data limitations inevitably led to classification errors, particularly in patients with sparse data. Since patients with early or mild axSpA are expected to have fewer encounters than established and severe axSpA patients, the classification process was likely more accurate with established and more severe axSpA than early and milder axSpA [23]. Another limitation is that ICD-10 codes for axSpA were not evaluated, since the study period preceded the implementation of ICD-10 codes. It is anticipated that ICD-10 codes will be similarly limited with axSpA cohort identification, since ICD-10 codes do not include non-AS axSpA subtypes.
Conclusion
There is an unmet need for accurate methods of identifying axSpA patients in large datasets. We established and characterized an appropriate sample of patients for developing axSpA identification methods that are anticipated to enable a wide array of previously impractical big data studies in axSpA.
Abbreviations
- AS:
-
Ankylosing spondylitis
- axSpA:
-
Axial spondyloarthritis
- DISH:
-
Diffuse idiopathic skeletal hyperostosis
- ICD:
-
International Classification of Diseases
- PPV:
-
Positive predictive value
- SpA:
-
Spondyloarthritis
- VHA:
-
Veterans Health Administration
References
Lee CH, Yoon H-J. Medical big data: promise and challenges. Kidney Res Clin Pract. 2017;36:3–11.
Garg N, van den Bosch F, Deodhar A. The concept of spondyloarthritis: where are we now? Best Pract Res Clin Rheumatol. 2014;28:663–72.
Rudwaleit M, van der Heijde D, Landewé R, Listing J, Akkoc N, Brandt J, et al. The development of assessment of SpondyloArthritis international society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009;68:777–83.
Poddubnyy D, Sieper J. Similarities and differences between nonradiographic and radiographic axial spondyloarthritis: a clinical, epidemiological and therapeutic assessment. Curr Opin Rheumatol. 2014;26:377–83.
Walsh JA, Adejoro O, Chastek B, Park Y. Treatment patterns of biologics in US patients with ankylosing spondylitis: descriptive analyses from a claims database. J Comp Eff Res. 2018;7:369–80.
Deodhar A, Mittal M, Reilly P, Bao Y, Manthena S, Anderson J, et al. Ankylosing spondylitis diagnosis in US patients with back pain: identifying providers involved and factors associated with rheumatology referral delay. Clin Rheumatol. 2016;35:1769–76.
Walsh JA, Song X, Kim G, Park Y. Evaluation of the comorbidity burden in patients with ankylosing spondylitis treated with tumor necrosis factor inhibitors using a large administrative claims data set. J Pharm Health Serv Res. 2018;9:115–21.
Lu MC, Koo M, Lai NS. Incident spine surgery in patients with ankylosing spondylitis: a secondary cohort analysis of a nationwide, population-based health claims database. Arthritis Care Res (Hoboken). 2017; https://doi.org/10.1002/acr.23478.
Wysham KD, Murray SG, Hills N, Yelin E, Gensler LS. Cervical Spinal Fracture and Other Diagnoses Associated With Mortality in Hospitalized Ankylosing Spondylitis Patients. Arthritis Care Res (Hoboken). 2017;69:271–7.
Wang R, Ward MM. Epidemiology of axial spondyloarthritis: an update. Curr Opin Rheumatol. 2018;30:137–43.
Sarmiento RF, Dernoncourt F. Improving patient cohort identification using natural language processing. In: Secondary analysis of electronic health records. Cham: Springer; 2016. p. 405–17.
Macklin EA, Blacker D, Hyman BT, Betensky RA. Improved design of prodromal Alzheimer's disease trials through cohort enrichment and surrogate endpoints. J Alzheimers Dis. 2013;36(3):475–86.
Cohen G, Hilario M, Sax H, Hugonnet S, Geissbuhler A. Learning from imbalanced data in surveillance of nosocomial infection. Artif Intell Med. 2006;37:7–18.
Baraliakos X, Listing J, Rudwaleit M, Haibel H, Brandt J, Sieper J, et al. Progression of radiographic damage in patients with ankylosing spondylitis: defining the central role of syndesmophytes. Ann Rheum Dis. 2007;66:910–5.
Wang X, Zhou J, Wang T, George SL. On Enrichment Strategies for Biomarker Stratified Clinical Trials. J Biopharm Stat. 2017;21:1–17.
Fihn S, Francis J, Clancy C, Neilson C, Nelson K, Rumsfeld J, et al. Insights from advanced analytics at the veteran health administration. Health Aff. 2014;33:1203–11.
US Department of Veterans Affairs “VINCI Central. VA Informatics and Computing Infrastructure (VINCI). 2017. http://www.hsrd.research.va.gov/for_researchers/vinci/. Accessed 6 Feb 2018.
Marcelo De Barros M, Gidewall K. Selecting Rows Randomly from a Large Table. 2008. https://msdn.microsoft.com/en-us/library/cc441928.aspx. Accessed 3 July 2018.
Loinc: The universal standard for identifying health measurements, observations, and documents. https://loinc.org/. Accessed 29 June 2018.
Chris Jianwei Leng CJ, South B, Shuying S. eHOST: The Extensible Human Oracle Suite of Tools. 2012. https://orbit.nlm.nih.gov/browse-repository/software/nlp-information-extraction/62-ehost-the-extensible-human-oracle-suite-of-tools. Accessed 6 Feb 2018.
Parikh R, Mathai A, Parikh S, Chandra Sekhar G, Thomas R. Understanding and using sensitivity, specificity and predictive values. Indian J Ophthalmol. 2008;56:45–50.
Singh JA, Holmgren AR, Krug H, Noorbaloochi S. Accuracy of the diagnoses of spondylarthritides in veterans affairs medical center databases. Arthritis Rheum. 2007;57:648–55.
Walsh JA, Pei S, Burningham Z, Penmetsa G, Cannon GW, Clegg DO, et al. Use of Disease-modifying Antirheumatic Drugs for Inflammatory Arthritis in US Veterans: Effect of Specialty Care and Geographic Distance. J Rheumatol. 2018;45:430–6.
Funding
Funding for this project was provided by the Marriott Daughters Foundation and the Rheumatology Research Foundation Scientist Development Award. The funding Foundations were uninvolved in study design, data collection, analyses, and manuscript preparation. Support for Dr. Cannon was provided in part by Specialty Care Center of Innovation, Veterans Health Administration and Department of Veterans Affairs, Health Services Research and Development.
Availability of data and materials
The data generated and analyzed during this study are not publically available due to protection of patient privacy.
All data for this project was housed and analyzed within the VA Informatics and Computing Infrastructure (VINCI) environment. Upon reasonable request, we can submit a Data Access Request Tracker (DART) application to seek approval to download specific de-identified data from VINCI. The DART application would need to be reviewed and approved by the VA Informatics Research Center (VIReC).
Author information
Authors and Affiliations
Contributions
JAW contributed to study design, chart review, data analyses, data interpretation, and manuscript preparation. SP analyzed and interpreted patient data. GKP classified and characterized patients with chart review. JL customized software for chart review and prepared data for chart review. GWC contributed to study design and data interpretation. DOC contributed to study design and data interpretation. BCS contributed to study design and data interpretation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was conducted in compliance with the Helsinki Declaration, with the approval of the University of Utah Institutional Review Board (IRB_00052363). A waiver of consent was obtained for record review.
Consent for publication
N/A
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Walsh, J.A., Pei, S., Penmetsa, G.K. et al. Cohort identification of axial spondyloarthritis in a large healthcare dataset: current and future methods. BMC Musculoskelet Disord 19, 317 (2018). https://doi.org/10.1186/s12891-018-2211-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-018-2211-7