Abstract
Background
Identification of poor prognostic factors for OVF is important but has not yet been clearly established. Despite paraspinal muscles could play an important role in the etiology of OVF, what influence time-dependent changes in paraspinal muscles have after OVF, and the impact on conservative treatments for patients who have an OVF remain largely unknown. The purposes of this study were to (1) evaluate time-dependent changes of the paraspinal musculature using MRI after injury in patients with osteoporotic vertebral fractures (OVFs), and (2) compare paraspinal muscles between conservatively treated patients with OVF who have successful union and those failed to conservative treatment.
Methods
A total of 115 consecutive patients who had sustained a recent OVF injury in the thoracolumbar region were assessed for eligibility using medical records and all required data were available from 90 patients who had been followed up for at least 6 months. Patients who needed to undergo surgery and patients who were diagnosed as having insufficient union after 6 months of follow-up were assigned to a group with insufficient union. Lumbar trunk parameters, relative cross-sectional area (rCSA) and proportion of fat infiltration (FI%) were calculated from MRI. To evaluate the time-dependent changes in the paraspinal muscle in patients after OVF injury, correlations between the timing of MRI and rCSA, FI% were determined. To clarify the impact of paraspinal muscles on the outcome of conservative treatments of patients with OVF, we compared rCSA between the groups.
Results
Sixty-five patients were assigned to a group with insufficient union and 25 patients were assigned to a group with successful union. FI% of the multifidus and erector spinae in the group with insufficient union were significantly greater than in the group with union. The timing of MRI in relation to initial injury was significantly correlated with FI% of the multifidus and erector spinae. rCSA of the erector spinae was significantly larger in the group with successful union than in the group with insufficient union.
Conclusions
These findings indicated a time-dependent increase of fatty degeneration of the multifidus and erector muscles, but no change in the rCSA and larger rCSAs of spinal erectors may play a role in successful union in patients with OVF.
Similar content being viewed by others
Background
Osteoporotic vertebral fractures (OVFs) increase overall mortality [1, 2], and are becoming increasingly common as the proportion of the population that is older continues to increase [3]. Described as stable spinal injuries, OVF are treated with conservative methods such as rest, immobilization, drug treatment and brace therapy [4]. However, these vertebral fractures sometimes fail to union, resulting in progressive collapse or pseudarthrosis and these patients often suffered from persistent back pain or neurological deficits [5]. The prevalence of insufficient union in elderly patients with OVFs ranges from 10 to 13.5% after conventional conservative treatments, resulting in marked reductions in the quality of life and activities of daily living of these patients [6,7,8]. Therefore, identification of risk factors associated with a poor prognosis for OVF is important but has not yet been clearly established.
Magnetic resonance imaging (MRI) plays crucial role in evaluation of spinal pathologies [9]. Recent studies have indicated the clinical importance of measuring the cross-sectional area (CSA) and proportion of fat infiltration (FI%) of paraspinal muscles using MRI to evaluate OVF or lumbar degenerative disease [10,11,12,13,14,15]. The CSA and FI% of paraspinal muscles correlate with spinal stability and alignment [11]. Additionally, trunk muscles could play an important role in the etiology of OVF based on how they affect spinal stability and vertebral strength via muscle–bone interactions [16]. However, what influence time-dependent changes in paraspinal muscles have after OVF, and the outcomes of conservative treatments for patients who have an OVF remain largely unknown.
The purpose of the present study was to (1) evaluate time-dependent changes of the paraspinal musculature after injury in patients with OVFs using MRI, and (2) compare paraspinal muscles between conservatively treated patients with OVF with successful union and insufficient union after conservative treatment.
Methods
Patient population
A total of 115 consecutive patients older than 65 years who had sustained a recent OVF injury in the thoracolumbar region were assessed for eligibility using their medical records between 2010 and 2016 in this retrospective single-center cohort study. During their initial visit to our institute, a new vertebral fracture was diagnosed if the following were present: onset of back pain within 3 weeks before presentation, a deformed vertebral body visible on radiographs, and an abnormal intensity within the vertebral bodies visible with MRI had on the initial visit. Patients with multiple fracture, pathological fractures associated with a tumor, high-energy injury, or those with neurological deficits, or who had not undergone MRI of thoracolumbar spine were not eligible to participate in the present study. Initially, patients underwent conservative treatment determined by three board-certified spinal surgeons at a single institution and were followed-up for a minimum of 6 months. Treatment options, including the use of a brace or drug therapy, or both, were selected by the individual physicians based on their experience. All of the required data were available from 90 patients who had been followed up for at least 6 months (Fig. 1).
Insufficient union was diagnosed when patients underwent surgery within 6 months or were diagnosed based on intravertebral vacuum clefts on plain radiography or CT, or had apparent segmental motion on plain X-ray dynamic images (≥5° between supine and weight-bearing positions) after 6 months of follow-up, as assessed by two spine surgeons independently [17]. Surgical treatment was indicated for patients with progressive neurological deficits or continuous severe lower back pain (visual analog scale > 80/100 points) caused by insufficient vertebral bone union, or both. Sixty-three patients required surgical treatment because of insufficient bone union of their OVF for the present study.
Patient groups
Patients who needed to undergo surgery and patients who were diagnosed as having insufficient union after 6 months of follow-up were assigned to a group with insufficient union (Fig. 1). Average time from original injury to surgery was 4.2 ± 1.5 months. After 6 months of follow-up, based on radiographs of satisfactory bony union without associated severe pain, we assigned 25 patients to a group with successful union (Fig. 1).
MRI protocol
The patients were placed in a supine position with the spine in a neutral position and a pillow was placed under their knees. Imaging was performed using a 3.0 T dual gradient superconducting MRI system (Discovery 750; GE Medical Systems, Milwaukee, WI, USA) with an 8-channel NeuroVascular-full neck coil, at a gradient strength of 40 mT/m, and a slew rate of 150 mT/m/ms. Sagittal and axial T1-weighted and T2-weighted MRI was performed routinely.
Measurement of the CSA and FI% of paraspinal muscles as visualized by MRI
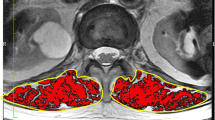
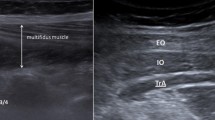
All MRI measurements were made by an experienced orthopedic surgeon blinded to the clinical information and study hypothesis. Following a previously used method [18], the regions of interest (ROI) were defined by manual tracing of the fascial boundary of the following muscles on both sides of the spinal column to the superior endplate of the L3 vertebral body on T1 axial images: psoas major, multifidus (including rotatores lumborum spinae), spinal erectors (encompassing both the longissimus and iliocostalis), and quadratus lumborum muscles (Fig. 2A). The ROIs were analyzed, and histograms showing the signal intensity were generated using digitalized image processing software (Image J, National Institutes of Health, Bethesda, MD, USA). The FI% in the total CSA of both muscles was evaluated using a threshold technique. Briefly, the number of pixels representing intramuscular fatty tissue were distinguished using a threshold grayscale value of 120 [15]. Relative CSA (rCSA) was defined as the CSA of each of the muscles divided by the CSA of the L3 vertebral body [12, 18]. The investigator evaluated and re-evaluated MRI, 2 weeks apart, blinded to MRI identifiers, to assess the intraobserver reliability of the rCSA and FI% of paraspinal muscle measurement. The intraobserver error of FI% of all patients is shown in a Additional file 1.
Data collection
For each patient who was treated for OVF, we searched the clinical records and laboratory database to record their basic characteristics, such as age, sex, body mass index (BMI), vertebral levels of injury, and which type of brace was used initially. Standardized bone mass density (BMD) measurements at the femoral neck were conducted using DXA (Lunar Prodigy; GE Medical Systems) within 4 weeks from the first visit. OVF were classified according to Genant’s semiquantitative criteria using plain X-ray images at the initial visit [19]. The severity of lumbar spinal stenosis seen on MRI was graded qualitatively according to the classification reported previously [20].
Statistical analysis
All data are reported as mean ± SD. Data were analyzed using an unpaired t test and a Fisher exact test to determine significant differences. Pearson correlation coefficients between rCSA, FI%, BMD (YAM%), and timing of MRI after the initial injury were determined. All statistical calculations were conducted using Prism, version 6.0 (Graph Pad Software, La Jolla, CA). For all tests, P < 0.05 was considered significant (*P < 0.05, **P < 0.005, ***P < 0.0005, ****P < 0.0001).
Results
We included 90 patients (58 women and 22 men) with an average age of 75.4 (65–88) years in the present study. Table 1 summarizes the characteristics of the patients, type of brace that was used initially and drug treatment for osteoporosis at their initial visit to our institute. There was no significant difference in the mean age, sex, BMD, and grading of LSS severity between the groups. The patients in the group with insufficient bony union had a more severe Genant grade of OVF than patients in the group with successful union. Overall, there were no significant differences in conservative management with hard braces or elastic braces between the groups. The rCSAs of total paraspinal muscles were positively correlated with BMD (YAM%) of all patients (Fig. 2c).
Despite that only patients who had undergone MRI were enrolled in this study, the timing of MRI after injury was indefinite and was assessed by three board certified spinal surgeons independently. The average time to obtain MRI in all cases was 64.1 ± 13.71 days after the initial injury. To evaluate the time-dependent changes in the paraspinal muscle in patients after OVF injury, correlations between the timing of MRI and rCSA, FI% were determined (Figs. 3 and 4). Timing of MRI after the initial injury was correlated with the FI% seen in the multifidus and erector spinae (Fig. 3a and b). By contrast, there was no correlation between the timing of MRI after the initial injury and the FI% of the psoas and quadratus, or rCSA of any paraspinal muscles (Fig. 3c and d, Fig. 4a–d). These findings indicated a time-dependent increase in FI% of the multifidus and erector muscles after injury, but no change in the rCSA of any paraspinal muscles (the paraspinal muscles of representative cases are shown in Fig. 4e).
To clarify the impact of paraspinal muscles on the outcome of conservative treatments of patients with OVF, we compared rCSA between the groups. rCSA of the erector spinae of patients in the group with sufficient union was significantly larger than the rCSA in patients in the group with insufficient union (Fig. 5b). No significant difference between the groups was found in the rCSA of multifidus, psoas, or quadratus muscles (Fig. 5a, c, and d). These results indicate that the rCSA of the erector spinae in patients with OVF who were treated successfully with conservative treatment is larger than in patients with OVF who had insufficient union (the paraspinal muscles of representative cases of both groups are shown in Fig. 5e).
Discussion
The present study showed that rCSAs of total paraspinal muscles were positively correlated with BMD (YAM%) of patients with OVF (Fig. 2c). The timing of MRI after injury was not controlled because of the retrospective nature of the present study, but the average timing of MRI was 64.1 ± 13.71 days after the initial injury. We found a correlation between rCSA and FI% of paraspinal muscles and the timing of MRI after injury, and found FI% of the multifidus and erector muscles was positively correlated with the timing of MRI after initial injury. Interestingly, the rCSA of paraspinal muscles was not correlated with the timing of MRI after the initial injury. Based on this finding, we compared rCSA, but not FI, of paraspinal muscles in patients with insufficient union to the rCSA of patients with successful union. We found that the rCSA of the erector spinae of patients in the group with successful union was significantly larger than that in patients in the group with insufficient union.
MRI plays crucial role in evaluation of spinal pathologies [9]. Numerous studies have found an association linking morphological changes in paraspinal muscles with low back pain (LBP), lumbar spinal stenosis and spinal pathology using MRI [10, 12, 21]. Advancing age is associated with profound changes in the spine and its surrounding musculature, such as atrophied lumbar paraspinal muscles, with a reduction in their CSA and increased intramuscular FI [22]. Despite current study showed there was no significant difference LSS severity between groups, influence of morphometric change of paraspinal muscle by reduced innervation in LSS patients has been focused [12]. However, whether muscle control problems contribute to cause LBP, or whether LBP is a trigger for morphological changes in musculature, such as disuse muscle atrophy, remains largely unknown [21]. A recent report stated that profound changes in lumbar paraspinal muscles, a reduction in the CSA, and increased intramuscular FI occur in patients with osteoporotic spinal compression fractures [23]. However, this report lacked detailed information on the timing of the MRI assessments that were performed after injury. Therefore, we first examined the time-dependent changes of the paraspinal muscles of patients with OVFs to determine the influence of persistent back pain on paraspinal muscle morphology. We found a time-dependent increase in FI% of the multifidus and spinal erectors, but found no change in the rCSA of the paraspinal muscles of patients with OVF. These findings might suggest the mechanism underlying changes in muscle morphology in which fatty degeneration of the paraspinal muscles has occurred ahead of muscle atrophy (Fig. 4e). Further study using muscle biopsy during surgery is needed to elucidate the mechanism, which is likely related to the relationship between fatty degeneration and pathological muscle atrophy.
Despite the numerous studies in which efforts have been made to screen patients with an OVF who are at high risk of a poor prognosis [8, 24, 20], images of fresh vertebral fractures remain difficult to interpret. Recent studies have indicated the roles paraspinal muscles can play in OVFs, fracture prevention, interventions for management, rehabilitation after fracture, and modification of kyphotic changes after fracture [16, 25, 26]. We believe the present study has clinical importance because it shows that rCSAs correlate significantly with bone union; that is, larger rCSAs of spinal erectors can play a crucial role in reducing the risk of an insufficient union in patients with an OVF by contributing to spinal column stability in a protective way (Fig. 5e). Future mechanical study is needed to elucidate the reason for the significant contribution of the spinal erectors among all paraspinal muscles as found in the present study.
The present study has some limitations. First, because of the comparatively small sample size, data from men and women were analyzed together. Differences in the quality and size of paraspinal muscles by sex should be considered in future studies. Second, the retrospective study design was not conducive to obtaining control patients (no fracture) and MRI data from patients according to a structured routine. Third, measuring BMD at the femoral neck using DXA may not be representative of the mineralization of the axial skeleton, because osteoporosis in the peripheral and axial skeleton often develops disparately; thus, quantitative computed tomography of the lumbar spine should be used for further study. Last, conservative treatment was not fully standardized according to drug treatment including calcium/vitaminD, physiotherapy, brace type or the time the brace was worn as these items were selected by 3 physicians independently. The mechanism of fatty degeneration in the paraspinal muscles is presumed to be influenced by brace immobilization, the influence of persistent back pain, or degeneration as a result of muscle disuse, so these possibilities limit identification of the specific mechanism. In current study, 63% of the patients in insufficient group had severe fracture in Genant’s classification as compared to 20% in successful union group. This might be one factors the difference of fatty degeneration between groups. Further prospective studies, in which the timing of MRI after injury is controlled and conservative treatment is standardized, are needed to clarify the mechanism of fatty degeneration in the paraspinal muscles. Nevertheless, to our knowledge, this is the first report to determine that (1) fatty degeneration of the paraspinal muscles has occurred ahead of muscle atrophy in patients after OVF injury, and (2) larger rCSAs of spinal erectors can play a crucial role in in successful union in patients with OVF.
Conclusions
These findings indicated a time-dependent increase of fatty degeneration of the multifidus and erector muscles, but no change in the rCSA and larger rCSAs of spinal erectors may play a role in successful union in patients with OVF.
References
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353(9156):878–82.
Lau E, Ong K, Kurtz S, Schmier J, Edidin A. Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J Bone Joint Surg Am. 2008;90(7):1479–86.
Lee YL, Yip KM. The osteoporotic spine. Clin Orthop Relat Res. 1996;323:91–7.
Francis RM, Aspray TJ, Hide G, Sutcliffe AM, Wilkinson P. Back pain in osteoporotic vertebral fractures. Osteoporos Int. 2008;19(7):895–903.
Hasegawa K, Homma T, Uchiyama S, Takahashi H. Vertebral pseudarthrosis in the osteoporotic spine. Spine (Phila Pa 1976). 1998;23(20):2201–6.
Cook DJ, Guyatt GH, Adachi JD, Clifton J, Griffith LE, Epstein RS, Juniper EF. Quality of life issues in women with vertebral fractures due to osteoporosis. Arthritis Rheum. 1993;36(6):750–6.
Kim DY, Lee SH, Jang JS, Chung SK, Lee HY. Intravertebral vacuum phenomenon in osteoporotic compression fracture: report of 67 cases with quantitative evaluation of intravertebral instability. J Neurosurg. 2004;100(1 Suppl Spine):24–31.
Tsujio T, Nakamura H, Terai H, Hoshino M, Namikawa T, Matsumura A, Kato M, Suzuki A, Takayama K, Fukushima W, et al. Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: a prospective multicenter study. Spine (Phila Pa 1976). 2011;36(15):1229–35.
Kumar Y, Gupta N, Chhabra A, Fukuda T, Soni N, Hayashi D. Magnetic resonance imaging of bacterial and tuberculous spondylodiscitis with associated complications and non-infectious spinal pathology mimicking infections: a pictorial review. BMC Musculoskelet Disord. 2017;18(1):244.
Singh R, Yadav SK, Sood S, Yadav RK, Rohilla R. Magnetic resonance imaging of lumbar trunk parameters in chronic low backache patients and healthy population: a comparative study. Eur Spine J. 2016;25(9):2864–72.
Choi MK, Kim SB, Park CK, Malla HP, Kim SM. Cross-sectional area of the lumbar spine trunk muscle and posterior lumbar interbody fusion rate: a retrospective study. Clin Spine Surg. 2017;30(6):E798–E803.
Chen YY, Pao JL, Liaw CK, Hsu WL, Yang RS. Image changes of paraspinal muscles and clinical correlations in patients with unilateral lumbar spinal stenosis. Eur Spine J. 2014;23(5):999–1006.
Kim H, Lee CK, Yeom JS, Lee JH, Cho JH, Shin SI, Lee HJ, Chang BS. Asymmetry of the cross-sectional area of paravertebral and psoas muscle in patients with degenerative scoliosis. Eur Spine J. 2013;22(6):1332–8.
Arbanas J, Pavlovic I, Marijancic V, Vlahovic H, Starcevic-Klasan G, Peharec S, Bajek S, Miletic D, Malnar D. MRI features of the psoas major muscle in patients with low back pain. Eur Spine J. 2013;22(9):1965–71.
Ranson CA, Burnett AF, Kerslake R, Batt ME, O'Sullivan PB. An investigation into the use of MR imaging to determine the functional cross sectional area of lumbar paraspinal muscles. Eur Spine J. 2006;15(6):764–73.
Mokhtarzadeh H, Anderson DE. The role of trunk musculature in osteoporotic vertebral fractures: implications for prediction, prevention, and management. Curr Osteoporos Rep. 2016;14(3):67–76.
Takahashi S, Hoshino M, Takayama K, Iseki K, Sasaoka R, Tsujio T, Yasuda H, Sasaki T, Kanematsu F, Kono H, et al. Predicting delayed union in osteoporotic vertebral fractures with consecutive magnetic resonance imaging in the acute phase: a multicenter cohort study. Osteoporos Int. 2016;27:3567–75.
Sions JM, Smith AC, Hicks GE, Elliott JM. Trunk muscle size and composition assessment in older adults with chronic low back pain: an intra-examiner and inter-examiner reliability study. Pain Med. 2016;17(8):1436–46.
Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 1993;8(9):1137–48.
Schizas C, Theumann N, Burn A, Tansey R, Wardlaw D, Smith FW, Kulik G. Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine (Phila Pa 1976). 2010;35(21):1919–24.
Barker KL, Shamley DR, Jackson D. Changes in the cross-sectional area of multifidus and psoas in patients with unilateral back pain: the relationship to pain and disability. Spine (Phila Pa 1976). 2004;29(22):E515–9.
Mengiardi B, Schmid MR, Boos N, Pfirrmann CW, Brunner F, Elfering A, Hodler J. Fat content of lumbar paraspinal muscles in patients with chronic low back pain and in asymptomatic volunteers: quantification with MR spectroscopy. Radiology. 2006;240(3):786–92.
Kim JY, Chae SU, Kim GD, Cha MS. Changes of paraspinal muscles in postmenopausal osteoporotic spinal compression fractures: magnetic resonance imaging study. J Bone Metab. 2013;20(2):75–81.
Hoshino M, Nakamura H, Terai H, Tsujio T, Nabeta M, Namikawa T, Matsumura A, Suzuki A, Takayama K, Takaoka K. Factors affecting neurological deficits and intractable back pain in patients with insufficient bone union following osteoporotic vertebral fracture. Eur Spine J. 2009;18(9):1279–86.
Greig AM, Briggs AM, Bennell KL, Hodges PW. Trunk muscle activity is modified in osteoporotic vertebral fracture and thoracic kyphosis with potential consequences for vertebral health. PLoS One. 2014;9(10):e109515.
Katzman WB, Miller-Martinez D, Marshall LM, Lane NE, Kado DM. Kyphosis and paraspinal muscle composition in older men: a cross-sectional study for the osteoporotic fractures in men (MrOS) research group. BMC Musculoskelet Disord. 2014;15:19.
Availability of data and materials
According to study protocol, the raw data have to be stored in hard disk which is not connected with outside. We can’t share raw data, because our institutional review board by ethical committee does not allow us to share raw data, which is included patient information.
Author information
Authors and Affiliations
Contributions
MK substantially contributed to the study design and analyzed the patient data. TO substantially analyzed and interpreted the patient data and was a major contributor in drafting the manuscript. SE substantially contributed to the conception and design of the study and contributed to drafting the manuscript. HH substantially contributed to the study design and critically revised the manuscript. All authors read, approved, and take responsibility for the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by our institutional review board by ethical committee of University of Yamanashi School of Medicine, Chairperson Zentarou Yamagata (Application number 1183). We received informed consent from all eligible patients and patient consent was written.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
The intraobserver error of FI% of all patients. The reader evaluated and re-evaluated MRI, 2 weeks apart, blinded to MRI identifiers, to assess the intraobserver reliability of the rCSA and FI rate of paraspinal muscle measurement. (TIF 947 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Katsu, M., Ohba, T., Ebata, S. et al. Comparative study of the paraspinal muscles after OVF between the insufficient union and sufficient union using MRI. BMC Musculoskelet Disord 19, 143 (2018). https://doi.org/10.1186/s12891-018-2064-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-018-2064-0