Abstract
Background
We examined pain levels in 2 cohorts assembled from the British Society for Rheumatology Biologics Register (BSRBR), and investigated which factors predicted Bodily Pain scores and discontinuation of TNFα-inhibitors.
Method
Data were retrieved from BSRBR-RA databases for up to 1 year after commencing TNFα-inhibitors (n = 11995) or being treated with non-biologic therapies (n = 3632). Bodily Pain scores were derived from the Short Form-36 (SF36) questionnaire and norm-transformed to allow comparison with UK population averages. Discontinuation data were from physician reports. Other data, including 28-joint disease activity score (DAS28) measurements, were from clinical examination, interview, medical records and self-report questionnaires. DAS28-P was derived as the proportion of DAS28 attributed to patient-reported factors (tender joint count and visual analogue score). Missing baseline variables from both cohorts were imputed into 20 replicate datasets. Odds ratios (OR) and adjusted OR were calculated for higher than median pain within each cohort.
Results
Participants reported moderate to severe pain at baseline, and pain scores remained >1SD worse than normal population standards at 1 year, even when disease activity responded to treatment. Baseline pain was associated with DAS28-P, worse physical function, worse mental health, and DAS28. After logistic regression, independent predictors of higher than median pain at follow up were baseline Bodily Pain score, higher DAS28-P, worse physical function or mental health and co-morbidities. Higher age, male gender, and higher BMI were additional independent predictors of higher pain in participants who received TNFα-inhibitors. Baseline pain was also one of the predictors of discontinuation of the first TNFα-inhibitor within 1 year, as were female gender, current smoking, co-morbidities, extra-articular manifestations and worse function.
Conclusion
Pain persists in people with treated RA, even in those for whom inflammation responds to treatment. Worse pain outcomes are predicted by factors different to those typically found to predict inflammatory disease activity in other studies. Worse pain at baseline also predicts discontinuation of TNFα-inhibitors. Improved pain management should complement inflammatory disease suppression in RA.
Similar content being viewed by others
Background
Treatment of rheumatoid arthritis (RA) with biologic or non-biologic disease modifying anti-rheumatic drugs (DMARDs) aims to control inflammation in order to retain functional capacity into later life. People with RA often name pain as one of the most unpleasant characteristics of their condition [1, 2]. Although patient-centred measures related to quality of life (QoL) improve during treatments that suppress inflammation [3], pain remains a problem for people with treated RA.
Inflammation is a cause of pain in RA, but other factors might also be important. Pain can persist even in people who achieve remission of inflammatory disease [4]. Previous studies have highlighted risk factors for worse pain prognosis, such as low mood [5–7] and gender [8]. We previously reported that in early RA, pain was not readily predicted by classic RA risk factors and severity measures [9]. Instead it was predicted by the proportion of 28-joint disease activity score (DAS28) contributed by the patient-reported components tender joint count (TJC) and visual analogue score (VAS-GH)), and we have proposed that a derived index, termed DAS28-P, might be related to abnormal pain processing [9, 10]. These factors that predict worse pain contrast with those that predict inflammatory disease activity or radiographic damage (recent literature reviews include [11, 12]). Predictors of pain in RA resemble risk factors that predict outcomes of other painful, chronic musculoskeletal conditions, such as low back pain [13]. Disease activity assessment, using DAS28, may be importantly confounded by pain [14, 15]. If non-inflammatory pain mechanisms inflate DAS28, then pain management strategies might be indicated rather than or in addition to escalating anti-inflammatory treatment.
In this study, we aimed to measure relationships between pain and inflammatory disease activity, and to identify baseline predictors of pain 1 year after commencing either a new biologic or undergoing non-biologic treatment in established RA. Continuation of biologic therapy should, in part, be determined by satisfactory symptomatic response and so we also measured association between pain-related factors and discontinuation of TNFα-inhibitors. We examined factors associated with baseline pain, 1 year pain and 1 year discontinuation of TNFα-inhibitors using data from 2 British Society for Rheumatology Biologics Register (BSRBR) cohorts of people with RA.
Methods
Data retrieval
Two biologic-naïve groups were assembled for analysis from the British Society for Rheumatology-Biologics Registry (BSRBR) national registry databases (University of Manchester, UK. Cohorts ethical approval reference number: MREC 00/8/53). The first was a hospital-based UK cohort of people initiating treatment at baseline with their first ever biologic agent. Participants were eligible for this cohort if they commenced treatment at baseline with one of 3 TNFα-inhibitors (infliximab, etanercept or adalimumab). UK national guidelines recommend that TNFα-inhibitors should be commenced after inadequate response to 2 other non-biological DMARDs [16]. Data from a total of 11995 people were supplied, of whom 92 % (11013) had baseline pain data and 68 % (8113) had 1 year pain data available and (92 %) 10949 were eligible for analysis of TNF-inhibitor discontinuation after 1 year. A second (non-biologic) cohort was hospital-based and collected by the BSRBR-RA as a referent for the BSRBR biologic cohort. Each participant was eligible if they were biologic-naïve, and were starting or receiving only non-biologic therapies at baseline. We analysed the BSRBR non-biologic cohort in its own right. The BSRBR cohorts have provided high-quality longitudinal data regarding disease activity, clinical characteristics and QoL [17]. Analyses of the BSRBR-RA cohorts have already provided data showing responses to treatment [18–20], safety [21, 22] and prevalence of co-morbidities [23].
Data from a total of 3632 people were supplied, of whom 80 % (2916) had baseline pain data and 63 % (2284) had 1 year pain data available. All participants from both cohorts satisfied 1987 American College of Rheumatology (ACR) classification criteria for RA [24]. Demographic and lifestyle data available at baseline included age, gender, smoking history and body mass index. RA disease data were seropositivity (positive or negative for rheumatoid factor); the presence of erosions (present or absent); physician-reported extra-articular RA features, which we classified as present or absent; DAS28 (TJC, swollen joint count (SJC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), VAS-GH). The variables ESR, CRP and SJC were used as the best estimates of current inflammation. Use of each DMARD at the time of recruitment to the cohort was recorded as present, absent or data unavailable (methotrexate, sulphasalazine, hydroxychloroquine, leflunomide, azathioprine, gold salts, cyclophosphamide and ciclosporin, plus steroid use were recorded). Other related clinical data were for co-morbidities, which included physical and mental health conditions and we classified as present or absent [23]; and self-report questionnaires addressing disability Health Assessment Questionnaire (HAQ) [25, 26], or QoL (including bodily pain); Short Form-36 (SF36) (Bodily Pain, Mental Health, Vitality (fatigue) and Physical Function (disability)) [27]. Baseline DAS28 and DAS28-P (the proportion of DAS28 attributed to tender joint count and visual analogue scale) were calculated as previously reported [9, 28]. DAS28-P is a ratio of the TJC and VAS-GH, after weighting and transformation, divided by the DAS28-ESR score, and is only calculated for active RA cases due to loss of normality at low values of DAS28. The formula used was ((0.56 * √TJC) + (0.014 * VAS-GH)) / DAS28-ESR, for RA cases with DAS28-ESR ≥3.2 [9].
Study outcomes
Norm-based SF36-Bodily Pain subscale scores at 1 year were used as the primary measure of pain outcome. This used the semi-continuous SF36-Bodily Pain scores [27], has been validated in RA populations [29], and yields a score where the mean for the UK population is 50 with a sd of 10. Use of norm-based data facilitates comparison between this study and the UK population [30]. The pain items from the SF36 were “how much bodily pain have you had during the past week?” and “During the past week, how much did pain interfere with your normal work (including both work outside the home and housework)?” SF36 version 2 was used for the data collection.
Discontinuation of TNFα-inhibitors was used as a surrogate outcome for treatment failure, and this analysis was performed independently of the prediction of pain outcome. TNFα-inhibitor use or discontinuation (plus the reason for discontinuation) was reported by each study centre at each data collection. Discontinuation was defined as absence of the initial TNFα-inhibitor treatment after baseline in a participant in the TNFα-inhibitor cohort. Switching from the initial biologic drug was taken as discontinuation, even if it was replaced by another TNFα-inhibitor. Two important reasons for discontinuation, inefficacy (IE) and adverse event (AE), were also analysed. Almost all (>99 %) of the participants that discontinued TNFα-inhibitor were using either non-biologic DMARDs or glucocorticoids at 1 year follow up. Data on any new biologics were not available for this study.
Statistical analyses
Greater than median pain measures (at baseline or at 1 year) or 1 year discontinuation of TNF-inhibitors were the primary outcomes. Mean (standard deviation) and percentage prevalences of participant characteristics are presented. Simple univariate comparisons between groups used ANOVA (followed by pairwise testing with a Bonferroni correction), t-tests or χ2 tests. Cohen’s d statistic was calculated using the difference between means over the pooled standard deviation of both time points. Pain was stratified into bands delimited by the sd of the UK population norm (10 points) and presented graphically. ESR readings were divided into <23 for men and <30 for women for secondary analyses [31].
To attempt to address some of the biases potentially introduced by missing data, analyses using multiple imputations of 20 datasets were performed for baseline variables (age, gender, height, weight, TJC, SJC, ESR, VAS-GH, HAQ, seropositive, smoking, all SF36 variables at baseline). The follow up pain outcome variable was not imputed. Fully conditional specification methodology was used with continuous variables imputed using multiple linear regression and categorical variables using multiple logistic regression. Hosmer-Lemeshow χ2 and the Nagelkerke pseudo-R2 were used to assess model fit and model power respectively for complete case data. Comparisons were made between cases with complete data for all covariates and those where at least one variable would require imputation.
Imputed data were used for the primary analyses. The composite indices of DAS28 and DAS28-P were calculated from measured or imputed ESR, SJC, TJC and VAS-GH; whereas the BMI was imputed directly. Imputed continuous variables were converted into tertiles, or WHO BMI groups (<25, 25–30, ≥30 kg/m2). These are described in Additional file 1: Table S1. For associations with dichotomised outcome variables, the odds ratios (OR) and 95 % confidence intervals (CI) were calculated for the risk of above vs below median pain score (at baseline or at 1 year) or 1 year discontinuation. The univariate potential associations SF36-Bodily Pain score and discontinuation were not adjusted for multiple comparisons.
Multivariable-adjusted logistic regression models were generated, which yielded adjusted OR (aOR) and 95 % CI. The measures at baseline were used to investigate the baseline association with the pain outcome, and also to predict 1 year pain (1 year change in pain from baseline was also used so confirm findings). In order to minimise collinearity, inclusion of SF36 subscales was limited those with a priori hypothesised associations with pain; mental health, baseline pain, fatigue (SF36-vitality) and disability (SF36-physical function). DAS28 was not strongly associated with DAS28-P (TNFα-inhibitor cohort: r = 0.19; non-biologic cohort r = 0.34), and therefore this did not preclude inclusion of both within the same statistical models.
Subgroups of the cohorts at the 1 year time point were examined at the individual patient level to assess pain reported by people considered as having a good response to treatment or with low inflammation. These subgroups were either those that achieved good EULAR response [32], those satisfying remission criteria [33], those with both normal ESR levels and a swollen joint count of zero, or those who achieved CRP ≤5 g/L at 1 year.
Statistical significance was taken when p < 0.05 or the 95 % CI did not encompass unity.
Results
The demographics of each cohort are shown in Table 1. The non-biologic cohort had fewer females, was older, had a shorter RA duration, and lower DAS28-P. The non-biologic cohort also displayed milder disease, with lower DAS28 and less impact on QoL than did the TNFα-inhibitor cohort (p < 0.003 for each comparison).
Mean SF36-Bodily Pain scores at baseline were >2 s.d. higher than the UK general population average, indicating moderate to severe pain. The respective median self-report for TNF-inhibitor and non-biologic cohorts pain levels were ‘severe’ and ‘moderate’; and the respective interference that pain had on their normal work, including housework, was ‘quite a bit’ and ‘moderately’. Bodily Pain scores improved significantly after 6 months in both cohorts, and these improvements were maintained at 1 year (p < 0.001 for all comparisons) (Fig. 1a). The improvements and Cohens d statistic for pain improvement between baseline and year 1 was 0.91 for TNFα-inhibitor cohort and 0.04 for non-biologic cohort. After 6 months of treatment, reported pain was comparable between TNFα-inhibitor and non-biologic cohorts. Mean Bodily Pain scores in both cohorts remained >1 s.d. higher than the average for the UK population after 1 year (Fig. 1a). After 1 year, The median self-report for TNF-inhibitor and non-biologic cohorts pain levels were both ‘moderate’; and the interference that pain had on their normal work, including housework were both ‘moderately’).
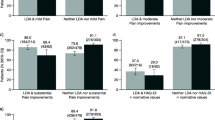
Pain up to 1 year of follow up. a, c, e, g show mean (sd) of norm-based SF36-Bodily Pain Scores using all data available at each time point. The UK population has an average norm-based score of 50 (grey, solid line), and lower scores indicate worse pain. b, d, f,) show the individual patient data from the TNF-inhibitor cohort demonstrating the proportion of participants with pain levels stratified by the norm-based standard deviation of 10. a shows mean (sd) of SF36-Bodily Pain scores from baseline to year 1. c, e and g show mean (sd) of norm based SF36-Bodily Pain scores at 1 year stratified by treatment response using c EULAR criteria; e DAS28 remission; and g normal swollen joint count (SJC = 0) with normal ESR range. Panels b, d, f and h show the stratification of individual patient data by SF36-Bodily Pain score in the TNF-inhibitor cohort at 1 year follow up. The cross-hatched, light shaded portion represents “better than UK average SF36-Bodily Pain” (≥50) and darker shaded plain portions represent increasingly worse pain at 1 year (increments of 10, which is ~1 sd for norm based SF36 scores). b Proportions individual patients with increasing severity of SF36-Bodily Pain scores at 1 year follow up; d stratified by EULAR response criteria, f stratified by DAS28 remission criteria, and h stratified into normal ESR and SJC ranges
Further analyses examined whether persistent pain was also evident in people in whom the inflammatory component of their disease was well controlled at the 1 year time point. In the TNFα-inhibitor cohort, 6517, 6581, 6210 and 4341 participants provided data for 1 year analysis of EULAR response; DAS28 < 2.6 remission; normal levels for both ESR and swollen joints (0/28); and measurements of CRP ≤5 g/L. Fifty four percent of participants achieved moderate, and 29 % achieved good EULAR responses. Seventeen percent achieved DAS28 < 2.6 remission. Twenty percent achieved normal levels for both ESR and swollen joints. Thirty three percent achieved CRP ≤5 g/L. Pain improved significantly after 1 year (Fig. 1a), in those with moderate and good EULAR responses (Fig. 1c), for those in DAS28 remission (Fig. 1e) and for those with normal ESR and SJC at 1 year (Fig. 1g) (p < 0.001 for all comparisons). Despite this improvement in pain, the SF36-Bodily Pain scores at 1 year indicated higher pain than UK population means in each of these ‘well controlled’ subgroups (Figs. 1c, e, g). Analysis of individual patient data at the 1 year time point revealed that more than half of the participants in each ‘well controlled’ subgroup had SF36-Bodily Pain scores >1 sd worse than the national average, that is a normed SF36-Bodily Pain score of less than 40 (Figs. 1d, f, h). Similar analysis was performed in the non-biologic cohort, where available data indicated that 29 % (265/905) achieved moderate, and 23 % (207/905) good EULAR response criteria, and 18 % (155/909) achieved DAS28 < 2.6 remission at 1 year. Of those with good EULAR response or those in DAS28 remission, 58 or 50 % (respectively) showed 1 year SF36-Bodily Pain scores >1 sd worse than national average (Figs. 1c and e).
After the characterisation and description of pain progression, further analysis focussed upon factors associated with pain. The variables at baseline with the greatest percentage of missing values in the TNF-inhibitor cohort were HAQ (7 %), ESR (8 %), DAS28-P (9 %), DAS28-ESR (9 %), BMI (12 %) and SF36 subscales (9 - 10 %). In the non-biologic cohort the greater percentages of missing values were found in HAQ (20 %), ESR (11 %), DAS28-ESR (12 %), DAS28-P (18 %) and SF36 subscales (19 - 20 %). In the TNFα-inhibitor and non-biologic cohorts, DAS28-ESR was higher in the complete cases than in cases with imputed 1 year values (6.6 vs 6.4 and 5.3 vs 4.4 respectively), and SF36-Bodily Pain scores indicated worse pain (25 vs 26 and 31 vs 33 respectively). Baseline SF36-Bodily Pain scores were analysed for all available data and were associated with many baseline factors in each cohort (Table 2). The baseline characteristics that predicted median SF36-Bodily Pain scores indicating worse pain at 1 year were similar between TNFα-inhibitor and non-biologic cohorts in univariate analyses (Table 3). Baseline characteristics of older age, higher BMI, current smoking, co-morbidities, DAS28, DAS28-P, and worse mental health, vitality, physical function and pain were positive predictors of SF36-Bodily Pain scores indicating worse pain at 1 year in both cohorts (Table 3). SF36-Bodily Pain scores indicating worse pain at 1 year were also predicted by male gender and extra-articular disease at baseline in the TNFα-inhibitor cohort, and by HAQ disability in the non-biologic cohort. In both cohorts, methotrexate use at baseline was associated with less pain at follow up, whereas glucocortiocosteroids or leflunomide was each associated with SF36-Bodily Pain scores indicating worse pain at 1 year. The overall models were weak (TNFα-inhibitor cohort) or moderate (non-biologic cohort) in explaining pain scores at 1 year (Nagelkerke pseudo-R2 = 0.16 and 0.32, respectively).
Logistic regression confirmed that higher DAS28-P, worse mental health, physical function or pain at baseline each independently predicted worse than median SF36-Bodily Pain score indicating worse pain at 1 year in each cohort (Table 4). For example, for DAS28-P at baseline the adjusted odds ratio (95 % CI) for worse pain at 1 year in the TNFα-inhibitor cohort was 1.14 (1.07–1.21), p < 0.001 and in the non-biologic control cohort it was 1.27 (1.11 – 1.46), p = 0.001. Pain was also predicted by co-morbidities, male gender, higher BMI and current smoking at baseline in the TNFα-inhibitor cohort; and less vitality and lower function in the non-biologic cohort. A sensitivity analysis showed that the presence of variables describing concurrent DMARD and steroid use did not alter the main findings of the models. Two secondary analyses, to further assess whether persistent inflammation would explain the predictors of pain, were performed in the participant subgroups in the TNF-inhibitor cohort who achieved ESR levels <23 for men and <30 for women, or CRP ≤5 g/L respectively after 1 year. A similar logistic regression analysis was performed for each subgroup, adjusting for baseline pain and potential confounding covariates. For the subgroup who achieved a lower ESR at 1 year, predictors of 1 year SF36-Bodily Pain scores indicating worse pain (aOR, (95 % CI)) were worse baseline pain (1.50, (1.29 – 1.76) p < 0.001), current smoking (1.45 (1.10 – 1.91, p = 0.008), comorbidity (1.37 (1.08 – 1.73), p = 0.008), higher DAS28-P (1.17 (1.01 – 1.34) p = 0.034), worse mental health (1.36 (1.17 – 1.58) p < 0.001), worse physical function (1.80 (1.54 – 2.10) p < 0.001), higher BMI (1.16 (1.00 – 1.34) p = 0.043) while methotrexate at baseline was negatively associated (0.63 (0.048 – 0.82) p = 0.001), each of which was similar to our primary findings. Similarly, for the subgroup who achieved CRP < 5 g/L at 1 year, SF36-Bodily Pain scores indicating worse pain were independently predicted (aOR, 95 % CI) by baseline current smoking (1.97, 1.26 – 3.07, p = 0.003) and higher DAS28-P (1.26, 1.02 – 1.56, p = 0.030).
Discontinuation of the initial TNFα-inhibitor was reported by 32 % (3475/10949) at 1 year. Of patients with median SF36-Bodily Pain scores indicating worse pain at 1 year, 39 % (1302/3376) had discontinued their original TNF inhibitor, as compared to 17 % (722/4140) of those with less than median pain. Mean (s.d.) SF36-Bodily Pain scores at 1 year were worse in those who stopped or changed their TNFα-inhibitors (29 (9)) than in those who continued (35 (10), p < 0.001). SF36-Bodily Pain scores at 1 year were worse both in those who discontinued TNFα-inhibitors due to inefficacy (28 (9)) and in those who discontinued due to adverse events (29 (9)), compared with those who continued (each p < 0.05). Univariate predictors of discontinuation included higher baseline DAS28, extra-articular disease, co-morbidities, worse physical function, mental health, vitality and Bodily Pain scores (Additional file 1: Table S2). Logistic regression showed independent prediction of discontinuation by baseline smoking, extra-articular disease, comorbidities, worse physical function and Bodily Pain score at baseline, and baseline non-biologic treatment (Table 5). People with a baseline treatment that did not include methotrexate or sulphasalazine were more likely to discontinue TNFα-inhibitors, whether due to inefficacy or to adverse events. Shorter disease duration and higher pain at baseline were stronger predictors of TNFα-inhibitor discontinuation due to inefficacy rather than to adverse events, whereas age, poorer physical function, longer disease duration and extra-articular disease were stronger predictors of discontinuation due to adverse events rather than inefficacy (Table 5). The main model showed a weak effect for predicting discontinuation for any cause (inefficacy or adverse events) (Hosmer-Lemeshow χ2 = 3.1, p = 0.925; and the Nagelkerke pseudo-R2 = 0.04).
Discussion
In this study we found that pain persists in many people with RA, despite the initial clinically significant [34] improvement upon commencing a TNFα-inhibitor. Several baseline factors, including a high contribution of patient reported factors to disease activity scores (high DAS28-P), poor mental health, poor physical function and the presence of co-morbidities, predicted pain outcomes after either TNFα-inhibitors or traditional DMARDs. Discontinuation of TNFα-inhibitors within 1 year from their initiation was associated with persistent pain, and predicted by baseline factors that overlapped with predictors of 1 year pain outcomes, including smoking, and higher baseline pain.
We identified a broad range of demographic and clinical factors that predicted 1 year pain outcomes in this study. However, teasing apart inflammatory and non-inflammatory pain mechanisms in the clinic can be extremely difficult. Although all 4 components of DAS28 are related to inflammation, the TJC and VAS-GH have also been associated with non-inflammatory pain mechanisms and concurrent fibromyalgia [10]. Derived indices such as DAS28-P might provide insight into the balance of different pain mechanisms. In a previous study of people with early RA commencing non-biologic DMARDs we found that higher DAS28-P scores predicted less improvement in pain at 12 months [9]. Early RA differs from established disease in several important aspects, such as the establishment of chronic inflammation and psychological adaptions to chronic pain, plus the effects of new DMARD treatments on DMARD-naïve patients. The current analysis of data from the BSRBR confirms and extends to established disease our findings in early RA, showing that high baseline DAS28-P was also associated with worse pain after commencing TNFα-inhibitors. High DAS28-P might be an indicator that pain is driven by non-inflammatory mechanisms such as central pain processing, resulting in disproportionately high tender joint counts and VAS-GH [10, 14, 15]. DAS28-P might be higher in people with fibromyalgia, either with [15] or without [14] RA, and was associated with widespread sensitivity to pressure induced pain, even at sites distant to inflamed joints in people with longstanding RA and DAS28 > 3.1 [10]. These observations are consistent with DAS28-P representing an index of augmented pain processing in RA, which might have utility for epidemiology studies where more detailed pain measurements cannot be obtained, and in retrospective studies or secondary data analysis. Targeting inflammatory pain mechanisms alone, either with TNFα-inhibitors or traditional DMARDs, may be insufficient to adequately manage pain in these patients.
Other baseline factors that consistently predicted 1 year pain outcomes were poor mental health, poor physical function and the presence of co-morbidities. Poor mental health predicts worse pain prognosis in a range of chronic conditions [35]. Fear and low mood represent emotional components of the pain experience, and might impair uptake or response to treatment [36]. Furthermore, psychological factors might specifically interact with central pain processing to augment or maintain chronic pain [5]. Physiotherapy and some exercise regimes can improve outcomes [37, 38], and our data raise the possibility that poor physical function may be a barrier to responding to treatments. Prediction of poor pain outcomes by baseline physical function was observed in both cohorts, but was particularly strong in the non-biologic DMARD cohort, and when physical function was measured by SF36 rather than HAQ. Differences between data from the 2 questionnaires might reflect their different emphases on mobility (SF36) or hand function (HAQ). We found that the presence of comorbidities predicted poorer pain prognosis. Osteoarthritis is a possible additional source of pain in those with RA and might be prevalent in the aged population. Further work could investigate whether comorbidities are a source of pain, or have been barriers to effective RA treatment. Poor mental health, physical function and comorbidities might each be amenable to treatment in their own right, but randomised clinical trials would be required to test whether targeting them can improve pain. Gender was found to predict future pain in our previous study of early RA using similar methodologies to this one [9]. This association may be due to reporting preferences, different pain sensitivities or different manifestations of RA across the genders. We found no association between baseline erosions and future pain but more detailed assessment would be required to determine whether pain in RA might be partly mediated by progressive joint damage.
We have found that factors that predicted early discontinuation of TNFα-inhibitors only partially overlapped with those that predicted poor pain outcomes. Pain levels were higher at baseline and at 1 year in those who discontinued TNFα-inhibitors, suggesting that inadequate pain control contributes to some of the decisions involved in discontinuation. We were not able to exclude in this study the possibility that worse pain outcomes might be caused by TNFα-inhibitor discontinuation, and pain might further improve if more effective biologic therapy were initiated. However, our secondary analysis on those with low CRP levels and those in remission suggests that persistent inflammation was not the sole reason for worse pain during follow up. The decision to discontinue medication is based upon the balance between efficacy and adverse events, and so discontinuation is often difficult to exclusively assign to one or other reason. However, in the current study, pain predicted discontinuation due to inefficacy, and not due to adverse events. We cannot be certain from our study of any causal relationship between pain and TNFα-inhibitor discontinuation, and further research would be required to determine whether more effective analgesic strategies would facilitate continuation of concurrently administered TNFα-inhibitors.
Several factors limit interpretation of our findings. We have identified baseline factors that predict 1 year pain outcomes in people with RA, but further research is required to determine what interventions can improve on these outcomes. Chanelling bias might have contributed to observed associations between baseline non-DMARD biologic medication use and 1 year pain, such that medications should not be interpreted as representing independent risk factors. Exploration of the effects of treatments upon RA pain is best addressed through randomised controlled trials, although it was important to include DMARD treatment in our models to ensure that they did not confound our results. Patient choice to use analgesics is moderated by a wide range of factors in addition to pain severity, including efficacy, adverse events and beliefs about medications and illness [39]. Further research would be required, therefore, to determine whether factors found in the current study to predict pain also predict healthcare utilisation due to that pain. Our models predicting 1 year pain were based upon an outcome variable (SF36 Bodily Pain score) with a moderate percentage of missingness due to attrition. The use of multiple imputation reduced the total level of missingness in this study, but might have selected from subsets of our data showing some degree of bias. Our models had only weak to moderate effects in explaining pain outcomes, and unmeasured factors might make important contributions to predicting Bodily Pain scores. In particular, measurements of centrally-augmented pain, or fibromyalgia classification criteria or a pain Manikin, would also have been useful to verify our findings. DAS28-P was associated with fibromyalgia classification in a study of 50 people with RA [10], but data were not available to determine fibromyalgia status in the BSRBR cohorts. Even though the BSRBR cohorts are large, un-measured factors, such as gene polymorphisms or additional treatment details, could have mediated or obscured associations between baseline characteristics and pain outcomes. The search for additional risk factors for worse pain or predictive markers requires further work. Similarities between our findings in the BSRBR and early RA [9] cohorts suggest that they might be generalisable to some other RA populations. Participants in the TNFα-inhibitor cohort are likely to be representative of patients commenced on their first biologic agent in the UK, but caution should be exercised before generalising our findings. Further work should determine whether the factors that we identified predict longer term outcomes. Our findings suggest possible mechanisms of pain but this study is not sufficient to justify stratification of treatment based on these factors alone.
Conclusions
In conclusion, pain persists in many people with treated RA, even when inflammation responds to treatment. Worse 1 year pain outcomes are predicted by factors different to those typically found to predict inflammatory disease activity, and include baseline Bodily Pain scores, the proportion of DAS28 attributable to patient-reported components, worse physical function or mental health, and co-morbidities. Worse pain at baseline also predicts TNFα-inhibitor discontinuation within 1 year. Improved pain management should complement inflammatory disease suppression in RA.
Abbreviations
Aza, azathioprine; BSRBR, British Society for Rheumatology Biologics Register; DAS28, 28 joint disease activity score; ESR, erythrocyte sedimentation rate; EULAR, European League Against Rheumatism; HCQ, hydroxychloroquine; Lef, leflunomide; MTX, methotrexate; QoL, quality of life; SF36, short form-36 questionnaire; SJC, swollen joint count; SSZ, sulphasalazine; TJC, tender joint count; VAS, visual analogue scale
References
Minnock P, FitzGerald O, Bresnihan B. Women with established rheumatoid arthritis perceive pain as the predominant impairment of health status. Rheumatology (Oxford). 2003;42(8):995–1000.
Taylor P, Manger B, Alvaro-Gracia J, Johnstone R, Gomez-Reino J, Eberhardt E, Wolfe F, Schwartzman S, Furfaro N, Kavanaugh A. Patient perceptions concerning pain management in the treatment of rheumatoid arthritis. J Int Med Res. 2010;38(4):1213–24.
Wassenberg S, Rau R, Steinfeld P, Zeidler H. Very low-dose prednisolone in early rheumatoid arthritis retards radiographic progression over two years: a multicenter, double-blind, placebo-controlled trial. Arthritis Rheum. 2005;52(11):3371–80.
Wolfe F, Boers M, Felson D, Michaud K, Wells GA. Remission in rheumatoid arthritis: physician and patient perspectives. J Rheumatol. 2009;36(5):930–3.
Zautra AJ, Parrish BP, Van Puymbroeck CM, Tennen H, Davis MC, Reich JW, Irwin M. Depression history, stress, and pain in rheumatoid arthritis patients. J Behav Med. 2007;30(3):187–97.
Hagglund KJ, Haley WE, Reveille JD, Alarcon GS. Predicting individual differences in pain and functional impairment among patients with rheumatoid arthritis. Arthritis Rheum. 1989;32(7):851–8.
Odegard S, Finset A, Mowinckel P, Kvien TK, Uhlig T. Pain and psychological health status over a 10-year period in patients with recent onset rheumatoid arthritis. Ann Rheum Dis. 2007;66(9):1195–201.
Hakkinen A, Kautiainen H, Hannonen P, Ylinen J, Makinen H, Sokka T. Muscle strength, pain, and disease activity explain individual subdimensions of the Health Assessment Questionnaire disability index, especially in women with rheumatoid arthritis. Ann Rheum Dis. 2006;65(1):30–4.
McWilliams DF, Zhang W, Mansell JS, Kiely PD, Young A, Walsh DA. Predictors of change in bodily pain in early rheumatoid arthritis: an inception cohort study. Arthritis Care Res (Hoboken). 2012;64(10):1505–13.
Joharatnam N, McWilliams DF, Wilson D, Wheeler M, Pande I, Walsh DA. A cross sectional study of pain sensitivity, disease activity assessment, mental health and fibromyalgia status in rheumatoid arthritis. Arthritis Res Ther. 2015;17(1):11.
Jilani AA, Mackworth-Young CG. The role of citrullinated protein antibodies in predicting erosive disease in rheumatoid arthritis: a systematic literature review and meta-analysis. Int J Rheum. 2015;2015:728610.
Bugatti S, Manzo A, Caporali R, Montecucco C. Assessment of synovitis to predict bone erosions in rheumatoid arthritis. Therap Adv Musculoskeletal Dis. 2012;4(4):235–44.
van der Windt DA, Kuijpers T, Jellema P, van der Heijden GJ, Bouter LM. Do psychological factors predict outcome in both low-back pain and shoulder pain? Ann Rheum Dis. 2007;66(3):313–9.
Leeb BF, Andel I, Sautner J, Nothnagl T, Rintelen B. The DAS28 in rheumatoid arthritis and fibromyalgia patients. Rheumatology (Oxford). 2004;43(12):1504–7.
Pollard LC, Kingsley GH, Choy EH, Scott DL. Fibromyalgic rheumatoid arthritis and disease assessment. Rheumatology (Oxford). 2010;49(5):924–8.
NICE. Rheumatoid arthritis - the management of rheumatoid arthritis in adults. London: HMSO; 2009.
Silman A, Symmons D, Scott DG, Griffiths I. British society for rheumatology biologics register. Ann Rheum Dis. 2003;62 Suppl 2:ii28–9.
Hyrich KL, Watson KD, Silman AJ, Symmons DP. Predictors of response to anti-TNF-alpha therapy among patients with rheumatoid arthritis: results from the British Society for Rheumatology Biologics Register. Rheumatology (Oxford). 2006;45(12):1558–65.
Soliman MM, Ashcroft DM, Watson KD, Lunt M, Symmons DP, Hyrich KL. Impact of concomitant use of DMARDs on the persistence with anti-TNF therapies in patients with rheumatoid arthritis: results from the British Society for Rheumatology Biologics Register. Ann Rheum Dis. 2011;70(4):583–9.
Hyrich KL, Watson KD, Lunt M, Symmons DP. Changes in disease characteristics and response rates among patients in the United Kingdom starting anti-tumour necrosis factor therapy for rheumatoid arthritis between 2001 and 2008. Rheumatology (Oxford). 2011;50(1):117–23.
Dixon WG, Hyrich KL, Watson KD, Lunt M, Symmons DP. Influence of anti-TNF therapy on mortality in patients with rheumatoid arthritis-associated interstitial lung disease: results from the British Society for Rheumatology Biologics Register. Ann Rheum Dis. 2010;69(6):1086–91.
Dixon WG, Watson KD, Lunt M, Hyrich KL, Silman AJ, Symmons DP. Reduction in the incidence of myocardial infarction in patients with rheumatoid arthritis who respond to anti-tumor necrosis factor alpha therapy: results from the British Society for Rheumatology Biologics Register. Arthritis Rheum. 2007;56(9):2905–12.
Hyrich K, Symmons D, Watson K, Silman A. Baseline comorbidity levels in biologic and standard DMARD treated patients with rheumatoid arthritis: results from a national patient register. Ann Rheum Dis. 2006;65(7):895–8.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31(3):315–24.
Bruce B, Fries JF. The Stanford health assessment questionnaire: dimensions and practical applications. Health Qual Life Outcomes. 2003;1:20.
Bruce B, Fries JF. The Stanford health assessment questionnaire: a review of its history, issues, progress, and documentation. J Rheumatol. 2003;30(1):167–78.
Ware JE, Snow KK, Kosinski M. SF-36 Health Survey: Manual and Interpretation Guide. 2nd ed. Lincoln: Quality Metric Inc; 2000.
Disease activity score in Rheumatoid arthritis [http://www.das-score.nl/das28/en/]. Accessed 8 Aug 2016.
Talamo J, Frater A, Gallivan S, Young A. Use of the short form 36 (SF36) for health status measurement in rheumatoid arthritis. Br J Rheumatol. 1997;36(4):463–9.
Jenkinson C, Stewart-Brown S, Petersen S, Paice C. Assessment of the SF-36 version 2 in the United Kingdom. J Epidemiol Community Health. 1999;53(1):46–50.
Tests and Procedures: Sed rate (erythrocyte sedimentation rate) [http://www.mayoclinic.org/tests-procedures/sed-rate/basics/results/prc-20013502]. Accessed 8 Aug 2016.
Fransen J, van Riel PL. The disease activity score and the EULAR response criteria. Rheum Dis Clin N Am. 2009;35(4):745–57. vii-viii.
Fransen J, Creemers MC, Van Riel PL. Remission in rheumatoid arthritis: agreement of the disease activity score (DAS28) with the ARA preliminary remission criteria. Rheumatology (Oxford, England). 2004;43(10):1252–5.
Kosinski M, Zhao SZ, Dedhiya S, Osterhaus JT, Ware Jr JE. Determining minimally important changes in generic and disease-specific health-related quality of life questionnaires in clinical trials of rheumatoid arthritis. Arthritis Rheum. 2000;43(7):1478–87.
Goldenberg DL. The interface of pain and mood disturbances in the rheumatic diseases. Semin Arthritis Rheum. 2010;40(1):15–31.
Fitzcharles MA, DaCosta D, Ware MA, Shir Y. Patient barriers to pain management may contribute to poor pain control in rheumatoid arthritis. J Pain. 2009;10(3):300–5.
Al-Qubaeissy KY, Fatoye FA, Goodwin PC, Yohannes AM. The effectiveness of hydrotherapy in the management of rheumatoid arthritis: a systematic review. Musculoskeletal care. 2013;11(1):3–18.
Hurkmans EJ, Jones A, Li LC, Vliet Vlieland TP. Quality appraisal of clinical practice guidelines on the use of physiotherapy in rheumatoid arthritis: a systematic review. Rheumatology (Oxford, England). 2011;50(10):1879–88.
Lai YH, Keefe FJ, Sun WZ, Tsai LY, Cheng PL, Chiou JF, Wei LL. Relationship between pain-specific beliefs and adherence to analgesic regimens in Taiwanese cancer patients: a preliminary study. J Pain Symptom Manag. 2002;24(4):415–23.
Acknowledgements
We would like to thank the BSR Biologics Register for collection, processing and provision of the data used in this study. We would also like to acknowledge specific contributions from Dr Kimme Hyrich, Dr Alan Roach, Dr Kath Watson and Dr Xuejuan Fan.
Funding
This study was funded by an I-CRP grant (#WI190792) from Pfizer UK.
Availability of data and materials
The data used in this study are owned by the BSRBR. Requests for the data should be directed to the BSRBR.
Authors’ contributions
Study design, conception, data analysis, writing/editing, approval of final manuscript (DAW & DFM).
Competing interests
DFM is supported by Pfizer UK and has received a speaking honorarium from Pfizer UK. DAW has received grants from Pfizer UK, and performed consultancy work for Novartis. No non-financial conflicts of interest exist for either author.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Data collection for the BSRBR was approved by NHS North West Multicentre Research Ethics Committee, reference number 00/8/53. Data were supplied to the authors in de-identified, anonymous formats with no indication of which TNFα-inhibitor was used or the date of treatment for each participant. No additional ethical approval or patient consent was sought for this study.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
Univariate associations with discontinuation of TNFα-inhibitor. (DOCX 54 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
McWilliams, D.F., Walsh, D.A. Factors predicting pain and early discontinuation of tumour necrosis factor-α-inhibitors in people with rheumatoid arthritis: results from the British society for rheumatology biologics register. BMC Musculoskelet Disord 17, 337 (2016). https://doi.org/10.1186/s12891-016-1192-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-016-1192-7