Abstract
Background
Neuromuscular electrical stimulation (NMES) is widely used as a rehabilitation methods to restore muscle mass and function in prolonged immobilization individuals. However, its effect in mechanically ventilated patients to improve clinical outcomes remains unclear.
Methods
A comprehensive search was conducted using PubMed, Embase, Web of Science, PEDro, and the Cochrane Library from their inception until December 24th, 2023. The search targeted randomized controlled trials (RCTs) comparing NMES with physical therapy (PT) or usual ICU care (CG), for improving clinical outcomes in mechanically ventilated patients. We performed a network meta-analysis utilizing Stata version 14.0 and R 4.3.1.
Results
We included 23 RCTs comprising 1312 mechanically ventilated adults. The treatments analyzed were NMES, PT, NMES combined with PT (NMES+PT), and CG. Network meta-analyses revealed that NMES or NMES+PT significantly improved extubation success rate compared to CG, with ORs of 1.85 (95% CI: 1.11, 3.08) and 5.89 (95% CI: 1.77, 19.65), respectively. Additionally, NMES exhibited a slight decrease in extubation success rate compared with NMES+PT, with OR of 0.31 (95% CI: 0.11, 0.93). Nevertheless, neither NMES nor NMES+PT showed any significant improvement in ICU length of stay (LOS), ventilation duration, or mortality when compared with PT or CG. NMES+PT emerged as the most effective strategy for all considered clinical outcomes according to the ranking probabilities. The evidence quality ranged from “low” to “very low” in this network meta-analysis.
Conclusions
NMES appears to be a straightforward and safe modality for critically ill, mechanically ventilated patients. When combined with PT, it significantly improved the extubation success rate against standard ICU care and NMES alone, and showed a better ranking over PT or NMES alone for clinical outcomes. Therefore, NMES combined with PT may be a superior rehabilitation strategy for this patient group.
Similar content being viewed by others
Background
Critically ill patients often experience prolonged periods of bed rest and inactivity resulting from their stay in the intensive care unit (ICU), and this is particularly true for those requiring mechanical ventilation (MV) [1]. Such patients are at a heightened risk of rapid muscle mass deterioration, with approximately 37% exhibiting signs of muscle atrophy as early as the fourth day of their ICU admittance [2]. This loss of skeletal muscle is correlated with diminished physical capabilities, extended duration of mechanical ventilation, prolonged ICU stays, and an increase in mortality [3]. Therefore, it is essential to implement immediate strategies to mitigate muscle degradation as promptly as possible for these individuals.
Early physical rehabilitation, including early mobility and exercise during the initial days of ICU admission for ventilated patients, stands as a crucial method to influence or even prevent skeletal muscle debilitation and atrophy [4,5,6,7]. Studies have shown that early physiotherapy protocol can enhance muscle quality and functionality in critically ill patients, as well as decrease length of ICU stay and mechanical ventilation duration [8, 9]. Nonetheless, early and intensive mobilization in ventilated patients presents challenges due to their severe conditions, high levels of ventilatory support, or impaired consciousness [10, 11]. In the early stages, feasible exercises for these patients typically involve low-intensity or passive activities, such as passive cycling at the bedside [12]. Another obstacle to early active rehabilitation is the potential insufficient duration of available physiotherapy time, often due to the lack of physiotherapists. Consequently, there is a need for alternative or supplemental rehabilitation methodologies that do not rely on patient cooperation or that utilize automated devices.
Neuromuscular electrical stimulation (NMES) is a technique that utilizes an automated device to apply surface electrodes on the skin, which activates intramuscular nerve branches and induces visible muscle contractions [13]. It has been demonstrated to be effective in mitigating muscle loss and enhancing muscle strength in patients requiring MV [14, 15]. Nakanishi N. et al. investigated the use of NMES in mechanically ventilated patients and found that it could prevent both upper and lower limb muscle atrophy and reduce the duration of hospitalization [16]. Furthermore, NMES is well-tolerated and does not necessitate patient cooperation.
To date, several systematic reviews have been conducted to assess the effects of NMES on critically ill or ventilated patients [17,18,19,20,21,22,23], however, these studies report conflicting results. Certain meta-analyses have shown that NMES application can not only effectively shorten the duration of ventilation but also ameliorate the functional status of mechanically ventilated patientss [17, 18, 23], while others have not found such effects, noting that NMES combined with standard care did not yield significant benefits in terms of muscle strength, ventilation duration, ICU mortality, or ICU length of stay (LOS) when compared to standard care alone [21].
These discrepancies could be attributed to varying inclusion criteria and publication dates of the reviews. Another possible contribution to the inconsistency is the heterogeneity of the interventions of the interventions among the included trails. In some trials within the experimental group, NMES was used alone, while in others it was combined with physical therapy. Conversely, some trials employed physical therapy as a control method, while others applied standard ICU care without exercise. Such variability makes it difficult to determine the true effect of NMES.
Therefore, we conducted this systematic review and network meta-analysis, focusing on different rehabilitation strategies, to determine whether NMES application can improve clinical outcomes such as ICU LOS, ventilation duration, extubation success rate or mortality in mechanically ventilated patients.
Methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Network Meta-Analyses (PRISMA-NMA) [24] (Supplementary Table 1 for the detailed PRISMA-NMA Checklist of this study).
Eligibility criteria
We searched for RCTs in critically ill adult patients with MV, which investigated NMES as a rehabilitation intervention, comparing with other interventions such as physical therapy (PT), NMES combined with PT (NMES+PT) or usual ICU care (CG).
Inclusion criteria for the studies were as follows: (1)Population: Adult patients(≥ 18 years of age) admitted to the ICU who required MV via either an endotracheal tube or tracheotomy; (2) Intervention and comparisons: The primary intervention assessed was NMES, either independently or in combination with PT, with comparisons including PT alone or usual ICU care; (3) Study Design: Only RCTs were included; (4) Outcomes: Studies needed to report on at least one of the following clinical outcomes: ICU LOS, ventilation duration, extubation success rate, and mortality within the ICU or hospital.
Search strategy
Two reviewers (CPX and QMW) independently conducted comprehensive searches of PubMed, Embase, Web of Science, PEDro, and the Cochrane Library databases from their inception to December 24th, 2023, without language or publication type restrictions. Additionally, we examined the reference lists of all pertinent articles and the citations within previously published meta-analyses to identify further potential studies (Supplementary Table 2 for the details of the search strategy).
Studies selection
According to the inclusion criteria, two reviewers (CPX and QMW) independently screened the titles and abstracts of the retrieved studies, and the full text was assessed as necessary, to identify the eligible studies. Any disagreements were resolved by discussing with a third researcher (WG) to reach a consensus.
Data extraction
A standardized data extraction form was utilized to systematically collect data from every study included in the analysis. We extracted details of study information such as the first author’s name, year of publication, the country or region of the study, setting, sample size, duration of the study, and intervention methods. Furthermore, we extracted participant demographics and baseline clinical measurements, including age, the baseline Acute Physiology and Chronic Health Evaluation II (APACHE II) score, and baseline body mass index (BMI). Clinical outcomes were also recorded, encompassing ventilation duration, extubation success rate, ICU LOS, ICU or hospital mortality. The two investigators undertook the data extraction process independently; conflicts were again resolved through consultation with WG. Additionally, supplemental files were reviewed and the authors of the articles were contacted for further details as needed.
Quality assessment
Two reviewers (CPX and QMW) assessed the studies’ risk of bias according to Cochrane risk of bias tool (ROB tool) independently. The tool included seven different items: (1) random sequence generation, (2) allocation concealment, (3) blinding of participants and personnel, (4) blinding of outcome assessment, (5) incomplete outcome data, (6) selective reporting, and (7) other sources of bias. Based on the methods of the trial, each item of the ROB was judged as “high risk”, “low risk”, or “unclear risk”. Additionally, we assessed the quality of evidence contributing to network estimates of the four outcomes with the Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework [25, 26]. Two reviewers (CPX and QMW) made judgments independently, and disagreements were resolved through discussion with a third reviewer (GW) to reach an agreement.
Statistical synthesis and analysis
The statistical analyses were performed using Stata version 14.0 and R 4.3.1. A random-effects model was applied to both pairwise meta-analyses and network meta-analyses. Odds ratios (ORs) with 95% confidence intervals (CIs) were utilized to estimate the effects of dichotomous variables, whereas mean differences (MDs) with 95% CIs were used for continuous variables. The I [2] statistic was calculated to quantify heterogeneity, representing the proportion of total variation attributable to between-study differences. Ranking probabilities for each intervention’s outcomes were calculated and expressed as the surface under the cumulative ranking curve (SUCRA) and visualized using cumulative ranking plots. The SUCRA provides a numerical representation of each intervention’s overall and mean rank, ranging from 0 to 1, with higher values indicating superior rankings.
To assess global inconsistency across the entire analytical network, we employed a design-by-treatment interaction approach. Local inconsistency was appraised using both loop-specific approaches and the node-splitting method. Global heterogeneity was evaluated using the I2 statistic, local heterogeneity was assessed by predictive interval plots, where discrepancies between the confidence intervals of relative treatment effects and their predictive intervals indicated uncertainty due to heterogeneity. Furthermore, a comparison-adjusted funnel plot was utilized to investigate potential publication bias in the included studies. A contribution plot highlighted the influence of each direct comparison on the estimation of each network meta-analytic summary effect. We also conducted a sensitivity analysis by excluding two trials that investigated NMES in patients with prolonged mechanical ventilation to gauge the robustness of the results for the four clinical outcomes examined.
Results
Literature identification and selection
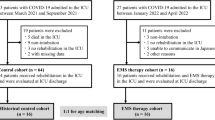
From the initial literature search, we identified a total of 1048 citations (PubMed, n = 146; Embase, n = 265; Cochrane Library, n = 372; Web of Science, n = 214; PEDro, n = 51). Following duplicate removal, 851 citations were screened by titles and abstracts. Subsequently, 757 articles were excluded based on the eligibility criteria. We evaluated the full texts of the remaining 94 articles, with 23 RCTs ultimately meeting the inclusion criteria (A flow chart of the trial selection process is presented in Fig. 1).
Study characteristics
The systematic review included 23 RCTs [2, 16, 27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47], of which 21 were published in English-language journals and two in Chinese-language journals. Publication years ranged from 2012 to 2023, and intervention durations varied from 7 days to 6 months. Twenty trials were two-arm studies, while three were multiple-arm studies. A total of 1163, 1145, 552, and 752 patients contributed to the respective clinical outcomes of ICU LOS, ventilation duration, extubation success rate, and mortality. Analyses were conducted on four interventions: NMES, PT, NMES+PT, and CG. Among the included trials, eight compared NMES with CG, twelve compared NMES+PT with PT, one compared NMES with both PT and NMES+PT, and two compared all four treatments (The network evidence plots for this study are shown in Fig. 2). Overall, 91.3% (21/23) investigated NMES in the early stages of mechanical ventilation, with males comprising 63.9% (838/1312) of participants. The mean age of participants was 53.89 ± 18.85 years (mean ± SD), the baseline mean BMI was 25.16 ± 6.07 kg/m2 (mean ± SD), and the baseline mean APACHE II score was 19.58 ± 7.56 (mean ± SD). Fifteen trials applied NMES to the quadriceps muscle, either alone or in combination with other muscle groups, five applied NMES to the abdominal muscle, either alone or in combination with the diaphragm, and three trails applied NMES to the diaphragm alone. Five trials reported the time from ICU admission to the first NMES intervention session, ranging from 2 hours to 4.6 ± 1.8 days (mean ± SD), with a mean duration of 2.5 ± 1.8 days (mean ± SD). Significant heterogeneity existed within the studies in terms of stimulation parameters. For example, for quadriceps muscles, the stimulation frequency ranged from 30 Hz to 100 Hz, with most trials (8/13) employing 50 Hz; and the pulse width applied varied from 200 μs to 500 μs, with the majority (7/11) using 400 μs. For the diaphragm or abdominal muscles, most trials utilized a frequency of 30 Hz, with only one using 50 Hz, and the pulse duration applied ranging from 300 μs to 400 μs. All studies utilized a stimulation intensity capable of eliciting a visible muscle contraction. Among the included trials, only a few reported a low number of adverse events related to NMES, including discomfort, prickling sensations, and brief, spontaneous reversible episodes of hypertension or tachycardia. No serious NMES-related adverse events were reported (The detailed characteristics of the included trials are provided in Table 1).
Risk of bias assessment
According to the ROB tool, five trials did not adequately describe their randomization methods, and two trials exhibited a high risk of bias within this domain. Furthermore, eleven trials failed to clearly report allocation concealment procedures, and fifteen trails did not achieve blinding of participants. Conversely, fourteen trials demonstrated a low risk of bias concerning blinding of outcome assessment, while eight trails displayed an unclear risk in this area, and the remain one had a high risk of bias in this domain.. 21 trials reported complete outcome data, one trial suffered from incomplete outcome data, and another lacked clarity regarding outcome data completeness. Selective reporting was absent in sixteen studies, and the majority of studies (20 out of 23) presented a low risk of bias in other sources of bias, with only three failing to disclose their funding sources. Ultimately, 15 studies were regarded to have a high risk of bias, whereas only 5 were assessed as having a low risk (The risk of bias assessment is provided in Fig. 3 and Supplementary Table 3).
Results of pairwise meta-analysis and network meta-analysis
The pairwise meta-analysis revealed no significant differences among the four treatments concerning ICU LOS, ventilation duration, and mortality rates. NMES was associated with a significant increase of extubation success rate when compared with CG, with an OR of 1.85 (95% CI: 1.11, 3.08), while NMES was slightly less effective than NMES+PT, as indicated by an OR of 0.23 (95% CI: 0.06, 0.83). The network meta-analysis further established NMES and NMES+PT as superior to CG for extubation success rate, with ORs of 1.85 (95% CI: 1.11, 3.08) and 5.89 (95% CI: 1.77, 19.65), respectively. Consistent with the pairwise meta-analyses, the network meta-analysis also shown a slight decrease in extubation success rate when NMES was compared with NMES+PT, with OR of 0.31 (95% CI: 0.11, 0.93). There were no significant differences among the treatments for ICU LOS, ventilation duration, and mortality according to the network meta-analysis (The results of pairwise meta-analysis and network meta-analysis are shown in Figs. 4, 5, 6, and 7).
Forest plot of pairwise meta-analysis, network meta-analysis and predictive interval for ICU LOS. Both the pairwise meta-analysis and the network meta-analysis revealed no significant differences among the four treatments for ICU LOS. Predictive interval plots suggested no significant heterogeneity in the network meta-analysis among the comparisons for ICU LOS
Forest plot of pairwise meta-analysis, network meta-analysis and predictive interval for ventilation duration. Both the pairwise meta-analysis and the network meta-analysis revealed no significant differences among the four treatments for ventilation duration. Predictive interval plots suggested no significant heterogeneity in the network meta-analysis among the comparisons for ventilation duration
Forest plot of pairwise meta-analysis, network meta-analysis and predictive interval for extubation success rate. The pairwise meta-analysis illustrated significant improvement in extubation success rate with NMES compared to CG. However, the combination of NMES and Physical Therapy (NMES+PT) displayed a slightly higher success rate than NMES alone. The network meta-analysis further confirmed the superiority of both NMES and NMES+PT over CG in terms of the extubation success rate. The predictive interval plots revealed significant heterogeneity in the network meta-analysis when comparing NMES with CG and NMES+PT with CG regarding the extubation success rate
Forest plot of pairwise meta-analysis, network meta-analysis and predictive interval for mortality. Both the pairwise meta-analysis and the network meta-analysis revealed no significant differences among the four treatments for mortality. Predictive interval plots suggested no significant heterogeneity in the network meta-analysis among the comparisons for mortality
Examination of the network contribution plots (Supplementary Fig. 1a-1d) revealed that NMES versus NMES+PT and NMES+PT versus CG had the most substantial influence on the network for ICU LOS, with contributions of 21.7 and 20.9%, respectively. Similarly, PT versus CG and NMES+PT versus CG were predominant for ventilation duration, contributing to 23.2 and 22.2% of the network, respectively. In the context of extubation success rate, the largest impact was seen in NMES versus CG and NMES versus PT comparisons, with contributions of 30.6 and 25.5%, whereas the comparison between PT and NMES+PT, and NMES versus CG presented the most significant contributions of 28.8 and 26.6% for mortality.
Transitivity, inconsistency and heterogeneity
No significant global inconsistency was detected by the design-by-treatment interaction model for all the four outcomes (P = 0.9844 for ICU LOS, p = 0.8107 for ventilation duration, p = 0.3692 for extubation success rate and p = 0.7168 for mortality, respectively). Local inconsistency tests corroborated these findings, indicating consistency in ICU LOS, ventilation duration, extubation success, and mortality, as evidenced by 95% CIs encompassing 0 in the inconsistency plots (Inconsistency assessment shown in Supplementary Fig. 2a-2d). The node-splitting model further supported the absence of significant differences in comparisons across all four outcomes, with P-values ranging from 0.205 to 0.989 (Supplementary Fig. 3a-3d). Nevertheless, predictive interval plots suggested significant heterogeneity in the network meta-analysis (NMA) when comparing NMES with CG and NMES with NMES+PT regarding the extubation success rate (Predictive interval plots shown in Figs. 4, 5, 6, and 7). The funnel plots for ICU LOS, ventilation duration and mortality were relatively symmetrical and did not suggest significant risk of publication bias among the included studies. In contrast, the publication bias was statistically significant for extubation success rate according to the funnel plot (Comparison-adjusted funnel plots shown in Supplementary Fig. 4a-4d).
SUCRA and ranking of all interventions
The SUCRA indicates that NMES was ranked third in effectiveness for ICU LOS, ventilation duration, extubation success rate, and mortality, with respective probabilities of 44.5, 55.6, 80.1, and 59%. PT was ranked second for each of these outcomes, with probabilities of 51.3, 58.3, 77.6, and 57.2%. NMES+PT emerged as the most effective intervention across all four outcomes, exhibiting probabilities of 92, 98.2, 94.7, and 68.1%. In contrast, CG ranked lowest for all outcomes with corresponding probabilities of 64, 86.4, 96.3, and 81.5% (Plots of cumulative ranking probability by SUCRA are depicted in Fig. 8).
GRADE evaluation on quality of evidence
According to the GRADE framework, the quality of evidence was deemed ‘very low’ across all comparative outcomes. The overall ranking of interventions for mortality was assessed as ‘low’ in quality, whereas, for the remaining three outcomes, it was marked as ‘very low’ (Supplementary Table 4a-4d).
Sensitivity analyses and subgroup analyses
Sensitivity analyses (Supplementary Fig. 5a-5d) was conducted by excluding two trials that investigated NMES in patients undergoing prolonged MV. The results were largely consistent with the results of the network meta-analysis across the four outcomes, affirming their stability. The application of NMES to various muscle groups across the included trials could have influenced its efficacy. However, a subgroup analysis concerning different muscle groups could not be undertaken due to insufficient data.
Discussion
To our knowledge, this is the first network meta-analysis examining the efficacy of NMES in critically ill, mechanically ventilated adult patients. We incorporated data from 23 RCTs involving 1312 patients in the quantitative analysis. The study revealed that NMES, both alone and in combination with physical therapy, increased the success rate of extubation when compared to standard ICU care. A combination of NMES and physical therapy showed a higher success rate than NMES used independently. However, no significant improvements in ICU LOS, ventilation duration, or mortality rates were observed when NMES was compared with physical therapy or usual care.
NMES is widely recognized as a rehabilitation tool to restore muscle mass and function in individuals with prolonged immobilization or limited activity, including those with spinal cord injuries, stroke, chronic heart failure, and severe chronic obstructive pulmonary disease (COPD) [48]. Owing to its ability to function without patient cooperation and its utilization of automated equipment, NMES presents as a promising option for critically ill patients. The seminal randomized study by Christina Routsi in 2010 revealed that 55-minute daily sessions of NMES could prevent critical illness polyneuropathy and reduce mechanical ventilation duration compared to routine ICU care [49]. Following this, numerous trials have adopted NMES in ICU settings, particularly in mechanically ventilated patients. Evidence indicated that NMES enhanced muscle strength in COPD patients receiving mechanical ventilation, decreased the incidence of ICU-acquired weakness, and shortened both mechanical ventilation duration and ICU stays [39]. Although NMES may benefits ventilated patients, its impact on clinical outcomes remains contentious, and it is unclear whether NMES is a viable substitute for physical rehabilitation in this population. Our study found that NMES alone was only associated with improved extubation success rate compared with usual ICU care, with no notable advancements in ICU length of stay, mechanical ventilation duration, or mortality compared to physical therapy. Furthermore, physical therapy surpassed NMES in improving these outcomes as it showed better hierarchy rankings. Our finding is consistent with another network meta-analysis which included 43 RCTs and investigated all types of rehabilitation interventions in adult critically ill patients and found greater benefits from individualized physical therapy over NMES in reducing ventilation time and ICU stays [50]. It appears that NMES alone is insufficient for enhancing outcomes in ventilated patients and should not replace physical rehabilitation. Evidence-based recommendations propose that NMES be applied particularly in the initial rehabilitation phase when voluntary muscle contractions are not feasible [10].
Although our analysis indicated that NMES combined with physical therapy ranked best for positively affecting all four measured outcomes, neither combination therapy nor NMES alone demonstrated a positive treatment effects on ICU stay, mechanical ventilation duration, or mortality. These findings are consistent with Guillaume Fossat [51], who noted no improvements in muscle strength or ventilation duration when electrical stimulation was combined with early rehabilitation in a sizable ICU study. This lack of outcomes improvement may be attributable to inadequate intervention durations in the included trials, most of which spanned approximately 2 weeks, with the shortest being 7 days. It has been demonstrated that substantial rehabilitation benefits accrue in patients with prolonged ICU stays who receive sufficient intervention dosages. Shorter interventions cannot be compensated for by increased frequency, early initiation, or a higher daily dose of exercise [11].In a prospective RCT trail, Gondin et al. demonstrated that NMES could elicit morphological changes in the muscle, but only for programs longer than 4 weeks in healthy man [52].For optimized outcomes, longer rehabilitation interventions may be necessary for ventilated patients.
Currently, physical rehabilitation remains the only intervention with proven benefits for critically ill patients [53]. The superior ranking of NMES+PT in our study suggests that combining NMES with physical rehabilitation could be a more effective rehabilitative approach for ventilated patients. Future studies should investigate the impact of this combined therapy.
Notably, the included studies in our analysis applied NMES to various muscle groups using different stimulation parameters (frequency, pulse width, intensity), and there is no consensus on optimal settings. With reference to the available data, it is suggested that NMES be executed for durations ranging from 25 to 60 minutes daily. The advised approach prescribes the utilization of a wide pulse and high frequency; specifically for the quadriceps muscle, a frequency of 45 Hz combined with a pulse width of 375 μs is recommended. The stimulation intensity should cause visible muscular contractions, ideally set at a minimum intensity of 50 mA but should not surpass 100 mA [4, 54, 55]. In our study, the majority of the trials featured stimulation parameters that were closely aligned with these recommendations, predominantly opting for a frequency of 50 Hz and a pulse width of 400 μs to induce visible muscular contractions. Preliminary evidence suggests that the parameters applied by most trials were adequate to elicit an enhancement in muscular strength. However, the determination of superior parameters is still unresolved, highlighting the need for further investigation to identify the optimal NMES settings for this specific patient demographic.
Regarding safety, included studies deemed NMES a well-tolerated and safe intervention, with no reports of severe or life-threatening adverse events and only minor complications such as prickling sensations [29]. Most intervention sessions were completed, with only a few stopped prematurely due to NMES intervention.
Limitation
This study has several limitations. Firstly, as a network meta-analysis, it incorporates a relatively small number of studies, with many of these being single-center trials characterized by limited sample sizes. Such constraints may have resulted in insufficient statistical power to detect differences in intervention effects on clinical outcomes. Secondly, this study lacks outcome parameters for assessing muscle quantity and quality, such as muscle thickness, Medical Research Council Sum Score (MRCs), and functional outcomes. This is due to the high degree of heterogeneity in the methods used to measure these parameters, and the available data were inadequate for a network analysis. Thirdly, the majority of the included studies exhibited a medium to high risk of bias; consequently, the quality of the evidence for all comparisons across the four outcomes was considered very low, as evaluated using the GRADE approach. This underscores the need for further well-controlled trials.
Conclusion
In conclusion, NMES presents as a feasible and safe intervention for critically ill patients undergoing mechanical ventilation. Both standalone NMES and NMES combined with physical therapy have demonstrated improvements in extubation success rate compared with usual ICU care. Moreover, the incorporation of NMES with physical therapy has demonstrated an enhanced extubation success rate, distinctly superior to NMES used alone. Furthermore, the combination of NMES with physiotherapy showed a better ranking over PT or NMES alone in improving clinical outcomes such as ICU LOS, ventilation duration, extubation success rate, and mortality in this population. However, the quality of evidence remains low to very low, due to concerns of bias and imprecision. Therefore, future RCTs with larger sample sizes and more rigorous methodological designs are necessary.
Availability of data and materials
All data generated or analysed during this study are included in this published article (and its supplementary files).
Abbreviations
- ICU:
-
Intensive care unit
- MV:
-
Mechanical ventilation
- LOS:
-
Length of stay
- NMES:
-
Neuromuscular electrical stimulation
- PT:
-
Physical therapy
- NMES+PT:
-
NMES combined with PT
- CG:
-
Usual
- ICU:
-
Care
- APACHE II:
-
Acute Physiology and Chronic Health Evaluation II
- BMI:
-
Body mass index
- COPD:
-
Chronic obstructive pulmonary disease
- SUCRA:
-
Surface under the cumulative ranking curve
- PRISMA-NMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Network Meta-Analyses
- ORs:
-
Odds ratios
- CIs:
-
Confidence intervals
- MDs:
-
Mean differences
- SD:
-
Standard deviation
- GRADE:
-
Grading of Recommendations Assessment, Development and Evaluation
References
Gerovasili V, Pitsolis T, Tzannis G, et al. Neuromuscular electrical stimulation in critically ill patients induces a beneficial effect on muscle histology; 2013. p. 187.
Koutsioumpa E, Makris D, Theochari A, et al. Effect of transcutaneous electrical neuromuscular stimulation on myopathy in intensive care patients. Am J Crit Care. 2018;27(6):495–503.
Stevens RD, Dowdy DW, Michaels RK, Mendez-Tellez PA, Pronovost PJ, Needham DM. Neuromuscular dysfunction acquired in critical illness: a systematic review. Intensive Care Med. 2007;33(11):1876–91.
Vanderthommen M, Duchateau J. Electrical stimulation as a modality to improve performance of the neuromuscular system. Exerc Sport Sci Rev. 2007;35(4):180–5.
Eggmann S, Verra ML, Luder G, Takala J, Jakob SM. Effects of early, combined endurance and resistance training in mechanically ventilated, critically ill patients: a study protocol for a randomised controlled trial. Trials. 2016;17:403.
Castro-Avila AC, Seron P, Fan E, Gaete M, Mickan S. Effect of early rehabilitation during intensive care unit stay on functional status: systematic review and Meta-analysis. PLoS One. 2015;10(7):e130722.
Hu MH, Hsu SS, Yip PK, Jeng JS, Wang YH. Early and intensive rehabilitation predicts good functional outcomes in patients admitted to the stroke intensive care unit. Disabil Rehabil. 2010;15:32.
Wu R, Yeh H, Chang K, Tsai M. Effects of different types and frequencies of early rehabilitation on ventilator weaning among patients in intensive care units: a systematic review and meta-analysis. PLoS One. 2023;18(4):e284923.
Chunyan Z, Bao L, Tianjun Y, Qing M, Aijun P, Dongsheng Z. Effect of early rehabilitation physiotherapy on muscle quality and function in critically ill patients. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2018;30(6):569–72.
Sommers J, Engelbert RH, Dettling-Ihnenfeldt D, et al. Physiotherapy in the intensive care unit: an evidence-based, expert driven, practical statement and rehabilitation recommendations. Clin Rehabil. 2015;29(11):1051–63.
Gosselink R, Bott J, Johnson M, et al. Physiotherapy for adult patients with critical illness: recommendations of the European Respiratory Society and European Society of Intensive Care Medicine Task Force on physiotherapy for critically ill patients. Intensive Care Med. 2008;34(7):1188–99.
Sibilla A, Nydahl P, Greco N, et al. Mobilization of mechanically ventilated patients in Switzerland. J Intensive Care Med. 2020;35(1):55–62.
Currier DP, Mann R. Muscular strength development by electrical stimulation in healthy individuals. Phys Ther. 1983;63(6):915–21.
Rodriguez PO, Setten M, Maskin LP, et al. Muscle weakness in septic patients requiring mechanical ventilation: protective effect of transcutaneous neuromuscular electrical stimulation. J Crit Care. 2012;27(3):311–9.
Gerovasili V, Stefanidis K, Vitzilaios K, et al. Electrical muscle stimulation preserves the muscle mass of critically ill patients: a randomized study. Crit Care. 2009;13(5):R161.
Nakanishi N, Oto J, Tsutsumi R, et al. Effect of electrical muscle stimulation on upper and lower limb muscles in critically ill patients: a two-center randomized controlled trial. Crit Care Med. 2020;48(11):e997–e1003.
Gutiérrez-Arias RE, Zapata-Quiroz CC, Prenafeta-Pedemonte BO, Nasar-Lillo NA, Gallardo-Zamorano DI. Effect of neuromuscular electrical stimulation on the duration of mechanical ventilation. Respir Care. 2021;66(4):679–85.
Wageck B, Nunes GS, Silva FL, Damasceno MCP, de Noronha M. Application and effects of neuromuscular electrical stimulation in critically ill patients: systematic review. Med Int. 2014;38(7):444–54.
Williams N, Flynn M. A review of the efficacy of neuromuscular electrical stimulation in critically ill patients. Physiother Theory Pract. 2013;30(1):6–11.
Li Y, Hou L, Zhu J, Liu L, Li D. Effect of neuromuscular electrical stimulation on muscle strength in patients with mechanical ventilation in intensive care unit: cumulative Meta-analysis and trial sequential analysis. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2022;34(4):416–20.
Zayed Y, Kheiri B, Barbarawi M, et al. Effects of neuromuscular electrical stimulation in critically ill patients: a systematic review and meta-analysis of randomised controlled trials. Australian critical care : official journal of the Confederation of Australian Critical Care Nurses. 2020;33(2):203–10.
Burke D, Gorman E, Stokes D, Lennon O. An evaluation of neuromuscular electrical stimulation in critical care using the ICF framework: a systematic review and meta-analysis. Clin Respir J. 2016;10(4):407–20.
Jie C, Jiajia K, Rui W, et al. Meta-analysis of effects of neuromuscular electrical stimulation of lower limbs on patients with mechanical ventilation in intensive care unit. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2021;33(10):1243–8.
Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84.
Huguet A, Hayden JA, Stinson J, et al. Judging the quality of evidence in reviews of prognostic factor research: adapting the GRADE framework. Syst Rev. 2013;2:71.
Mahlknecht P, Glechner A, Gartlehner G. Guideline development: Going from evidence to recommendations. Challenges and opportunities--a methodologist's view. Z Evid Fortbild Qual Gesundhwes. 2015;109(4–5):319–29.
McCaughey EJ, Jonkman AH, Boswell-Ruys CL, et al. Abdominal functional electrical stimulation to assist ventilator weaning in critical illness: a double-blinded, randomised, sham-controlled pilot study. Critical care (London, England). 2019;23(1):261.
Jonkman AH, Frenzel T, McCaughey EJ, et al. Breath-synchronized electrical stimulation of the expiratory muscles in mechanically ventilated patients: a randomized controlled feasibility study and pooled analysis. Crit Care. 2020;24(1)
Abu-Khaber HA, Abouelela AMZ, Abdelkarim EM. Effect of electrical muscle stimulation on prevention of ICU acquired muscle weakness and facilitating weaning from mechanical ventilation. Alex J Med. 2013;49(4):309–15.
Hsin YF, Chen SH, Yu TJ, Huang CC, Chen YH. Effects of transcutaneous electrical diaphragmatic stimulation on respiratory function in patients with prolonged mechanical ventilation. Ann Thorac Med. 2022;17(1):14–20.
Chen YH, Hsiao HF, Li LF, Chen NH, Huang CC. Effects of electrical muscle stimulation in subjects undergoing prolonged mechanical ventilation. Respir Care. 2019;64(3):262–71.
Shen SY, Lee CH, Lin RL, Cheng KH. Electric muscle stimulation for weaning from mechanical ventilation in elder patients with severe Sepsis and acute respiratory failure – a pilot study. Int J Gerontol. 2017;11(1):41–5.
Dall' Acqua AM, Sachetti A, Santos LJ, et al. Use of neuromuscular electrical stimulation to preserve the thickness of abdominal and chest muscles of critically ill patients: a randomized clinical trial. J Rehabil Med. 2017;49(1):40–8.
Kho ME, Truong AD, Zanni JM, et al. Neuromuscular electrical stimulation in mechanically ventilated patients: a randomized, sham-controlled pilot trial with blinded outcome assessment. J Crit Care. 2015;30(1):32–9.
Dos Santos FV, Cipriano G, Vieira L, et al. Neuromuscular electrical stimulation combined with exercise decreases duration of mechanical ventilation in ICU patients: a randomized controlled trial. Physiother Theory Pract. 2020;36(5):580–8.
Silva PE, De Cássia MR, Livino-De-Carvalho K, et al. Neuromuscular electrical stimulation in critically ill traumatic brain injury patients attenuates muscle atrophy, neurophysiological disorders, and weakness: a randomized controlled trial. J Intensive Care. 2019;7(1)
Mahran GSK, Mehany MM, Abbas MS, et al. Short-term outcomes of neuromuscular electrical stimulation in critically ill patients. Crit Care Nurs Q. 2023;46(2):126–35.
Leite MA, Osaku EF, Albert J, et al. Effects of Neuromuscular Electrical Stimulation of the Quadriceps and Diaphragm in Critically Ill Patients: a Pilot Study. Critical care research and practice. 2018;2018:4298583.
Chen S, Jiang Y, Yu B, et al. Effect of transcutaneous neuromuscular electrical stimulation on prevention of intensive care unit-acquired weakness in chronic obstructive pulmonary disease patients with mechanical ventilation. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2019;31(6):709–13.
Peng L, Chao LI, Cuixia SHANG, et al. Effect of electrical stimulation combined with pulmonary rehabilitation on patients with mechanical ventilation. Journal of Xi'an Jiaotong University (Medical Sciences). 2022;43(05):737–43.
Verceles AC, Serra M, Davis D, et al. Combining exercise, protein supplementation and electric stimulation to mitigate muscle wasting and improve outcomes for survivors of critical illness—the ExPrES study. Heart Lung. 2023;58:229–35.
Medrinal C, Machefert M, Lamia B, et al. Transcutaneous electrical diaphragmatic stimulation in mechanically ventilated patients: a randomised study. Crit Care. 2023;27(1):338.
Liu Y, Gong Y, Zhang C, et al. Effect of neuromuscular electrical stimulation combined with early rehabilitation therapy on mechanically ventilated patients: a prospective randomized controlled study. BMC Pulm Med. 2023;23(1):272.
Campos DR, Bueno T, Anjos J, et al. Early neuromuscular electrical stimulation in addition to early mobilization improves functional status and decreases hospitalization days of critically ill patients. Crit Care Med. 2022;50(7):1116–26.
Othman SY, Elbiaa MA, Mansour ER, El-Menshawy AM, Elsayed SM. Effect of neuromuscular electrical stimulation and early physical activity on ICU-acquired weakness in mechanically ventilated patients: a randomized controlled trial. Nurs Crit Care. 2023;
Olimpio JH, Camilo GB, Marques JA, Xavier RS, Santos CE, Lopes AJ. Effects of transcutaneous electrical diaphragmatic stimulation in critically ill elderly patients: a randomized controlled trial. Physiother Theory Pract. 2023:1–10.
Vieira L, Silva PE, de Melo PF, et al. Early neuromuscular electrical stimulation preserves muscle size and quality and maintains systemic levels of signaling mediators of muscle growth and inflammation in patients with traumatic brain injury: a randomized clinical trial. Crit Care Res Pract. 2023;2023:9335379.
Maffiuletti NA. Physiological and methodological considerations for the use of neuromuscular electrical stimulation. Eur J Appl Physiol. 2010;110(2):223–34.
Routsi C, Gerovasili V, Vasileiadis I, et al. Electrical muscle stimulation prevents critical illness polyneuromyopathy: a randomized parallel intervention trial. Crit Care. 2010;14(2)
Waldauf P, Jiroutková K, Krajčová A, Puthucheary Z, Duška F. Effects of rehabilitation interventions on clinical outcomes in critically ill patients: systematic review and Meta-analysis of randomized controlled trials. Crit Care Med. 2020:1055–65.
Fossat G, Baudin F, Courtes L, et al. Effect of in-bed leg cycling and electrical stimulation of the quadriceps on global muscle strength in critically ill adults: a randomized clinical trial. JAMA. 2018;320(4):368–78.
Gondin J, Guette M, Ballay Y, Martin A. Electromyostimulation training effects on neural drive and muscle architecture. Med Sci Sports Exerc. 2005;37(8):1291–9.
Calvo-Ayala E, Khan BA, Farber MO, Ely EW, Boustani MA. Interventions to improve the physical function of ICU survivors: a systematic review. Chest. 2013;144(5):1469–80.
Balke M, Teschler M, Schäfer H, Pape P, Mooren FC, Schmitz B. Therapeutic potential of Electromyostimulation (EMS) in critically ill patients—a Systematic Review. Front Physiol. 2022;13
Zarzeczny R, Nawrat-Szołtysik A, Polak A. Effects of 12 weeks of neuromuscular electrical stimulation of the quadriceps muscles on the function and physio-biochemical traits in functionally fit female nursing-home residents aged 75 + years: a pilot study. Eur J Appl Physiol. 2023;
Acknowledgments
We would like thank all the people who participated in primary studies.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
C.X. and W.G. conceived and designed the study. C.X. and F.Y. contributed to the literature search, and participated in data collection and statistical analyses. C.X. and Q.W. performed the interpretation and C.X. wrote the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Cuiping Xu is first author.
Supplementary Information
Additional file 1:.
Supplementary Tables and Figures
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, C., Yang, F., Wang, Q. et al. Effect of neuromuscular electrical stimulation in critically ill adults with mechanical ventilation: a systematic review and network meta-analysis. BMC Pulm Med 24, 56 (2024). https://doi.org/10.1186/s12890-024-02854-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-02854-9