Abstract
Background
Workers in pulp and paper factories are continuously exposed to paper dust. Excessive exposure to paper dust can cause respiratory disease. Information about the prevalence of chronic respiratory symptoms and dust exposure levels among workers in pulp and paper factories is not available in Ethiopia. The aim of this study was, therefore, to assess personal total dust exposure levels, the prevalence of chronic respiratory symptoms and their associated risk factors among workers in Ethiopian pulp and paper factories.
Methods
A comparative cross-sectional study was conducted. A total of 40 dust measurements were carried out on 20 randomly selected workers. To assess chronic respiratory symptoms and associated factors, 434 workers from two paper factories and controls were interviewed using a standard questionnaire adapted from the American Thoracic Society (ATS). Gravimetric analyses of the filters were undertaken using a standard microbalance. Poisson regression was performed for comparing the prevalence of symptoms and risk factors for the two groups. Multivariable analyses were conducted to identify factors associated with chronic respiratory symptoms.
Result
The arithmetic mean (AM) and geometric mean (GM) of dust exposure levels among the paper factories workers were 11.3 (± 7.7) and 10.2 (± 1.4) mg/m3 respectively. This exposure level exceeded the threshold limit value recommended for total dust (10 mg/m3). The prevalence of having at least one chronic respiratory symptom was about 51% among the workers in paper factories. The prevalence ratio of having chronic respiratory symptoms among paper factory workers was 5.6 times higher (PR = 6, 95% CI 3.5–10.3) than in the controls. Chronic respiratory symptoms were significantly associated with factors such as an educational status of less than grade 9, being employed in the work sections of the factories, having work experience of 5 years and above, working more than 8 h per day and having a past history of occupation and respiratory illnesses.
Conclusion
The dust concentration in the paper factories exceeded the acceptable recommended limit value of 10 mg/m3. The prevalence of chronic respiratory symptoms among paper factory workers was higher than among controls. The main determining factors for chronic respiratory symptoms among the workers were the specific work section such as production section, low income, having past history of respiratory illnesses, the number of years of working and low educational status. This finding indicated the need for improving the working conditions in paper factories in Ethiopia.
Similar content being viewed by others
Background
Papermaking mainly uses tree trunks, which pass through the processes of cutting, debarking, chipping and pulping. Currently, recycled paper accounts for an increasing proportion of paper production. Dust is generated at each stage of the paper-making process [1,2,3,4,5,6].
Workers in paper factories are often exposed to paper dust. Many studies have shown that the level of dust exposure in paper factories has been above recommended occupational exposure limits (OEL) of 10 mg/m3 [7,8,9,10]. However, some studies conducted in paper factories also indicated low levels of dust exposure [11,12,13,14].
Exposure to paper dust in excess of 10 mg/m3 over a period of many years can cause obstructive and restrictive respiratory diseases such as chronic obstructive lung disease, asthma and reduced lung function (mainly decreased forced expiratory volume by one second (FEV1) and forced vital capacity (FVC)) [7, 9, 12, 14,15,16]. Another study indicated that excessive exposure to paper dust (> 5 mg/m3) was associated with decreased lung function and increased prevalence of different forms of respiratory symptoms [12]. The development of occupational asthma or asthma-like symptoms is probably a significant occupational health hazard in pulp mills [7, 12]. Generally, the health effects vary depending on the types of dust, the duration of the exposure, and the concentration and size of dust in the breathing zone [17].
The effect is higher in those factories that use waste paper as their raw material because this production process generates a huge amount of dust [7]. In addition, dust exposure levels are higher in factories that have old machines. This can increase the impact on respiratory health [15]. By comparison, there was no correlation between exposure to paper dust and impairment of lung function in two studies of lower exposure levels (≤ 5 mg/m3) [18, 19]. This suggests that respiratory problem is associated with the amount of dust exposure.
Occupational respiratory symptoms and diseases are a major burden in low and middle-income countries [20]. This is a result of poor working practice and environments, and the use of outdated machines that can create excessive dust [20]. Workers in the paper industry will be likely to increase in Africa particularly in Ethiopia due to economic growth [21].
Several studies have been performed in Sweden [11,12,13,14,15,16, 19, 22,23,24], Germany [8, 9], and Poland [25] concerning paper dust. However, to the best of our knowledge there is no published scientific study on the level of worker exposure to paper dust in Africa particularly in Ethiopia. In addition, the paper factories in Ethiopia have long service years, more than 60 years, and were established in the 1960s. So, it seemed likely to involve high levels of dust exposure that might lead to different respiratory health problems among the paper factories workers here. Therefore, the aim of this study was to assess personal total dust exposure level, the prevalence of chronic respiratory symptoms, and their associated factors among workers in paper factories in Ethiopia.
Methods
Study area, period and design
The study was conducted in two paper factories in Ethiopia (factories A, and B). The study focused on paper factories that use the material pulp, and recycled old paper as their input and which produced rolled and finished paper [26, 27]. A comparative cross-sectional study was conducted from September 2020 to October 2020 to assess personal dust exposure level, the prevalence of chronic respiratory symptoms, and their associated factors among workers of paper and water bottling factories in Ethiopia. In this study, water bottling factories were used as a control, assuming that there is less (insignificant) amount of dust generation in such factories [28].
Source and study population
All paper factory workers and all water-bottling factories found in Ethiopia were the source population. The study populations included workers selected from these factories.
Selection criteria
Workers who were directly engaged in the production activities in the factories for at least one year or more were included in this study. Those workers less than 18 years of age were excluded from the study.
Sample size determination
The sample size for personal dust exposure assessment was calculated based on the Rappaport et al. 2008 recommendation that 5–10 randomly selected individuals in a similar exposure group (SEG) with repeated measurements are sufficient to predict the group dust exposure level [29]. A SEG is a group of workers working on the same type of activities in a similar work area for the same duration of time. With the above assumptions, 4 SEGs were identified from two selected factories. In factory A there were raw material preparation workers (bell machine compactor and loader, and pulp and recycle paper cutting and milling) as well as production room workers (roll paper, carton and paper production) and in factory B, there were Cone production workers and production room workers (roll paper, carton and paper). Five workers were randomly selected from each SEG. This makes a total of 40 dust measurements on 20 randomly chosen paper factory workers with each a repeated measurement.
The sample size for respiratory symptoms was calculated using a double population proportion formula considering the prevalence of coughs among exposed 36.6% and controls 18.4% [10]. An 80% statistical power was considered sufficient to detect the difference in coughing between the two groups at a significance level of 0.05. To maximize the sample size with an odds ratio of 2.56, we recalculated by taking an odds ratio of 2 on Epi info. After adding 10% for non-response, we determined that 434 participants were needed (i.e., 217 from paper factories and 217 from water bottling).
Sampling technique
The calculated sample size was proportionally assigned to the size of the two selected factories. By using worker registrations as a sampling frame, a simple random sampling method was used to select study subjects from each department.
Data collection procedure
Total dust measurements
Personal total dust was sampled using pre-weighed polyvinyl chloride (PVC) filter membranes with a pore size of 5.0 μm inserted on a Millipore plastic closed face 37 mm filter cassette (CFC) attached to an SKC sidekick pump through which air was pumped by a rechargeable battery-powered motor at a constant flow rate of 2.0 l/min. The sampling cassettes were situated on shoulder straps as close to the breathing zone as possible. Full-shift exposure measurements were conducted on randomly chosen days and repeated sampling was conducted the next day. Data collection took 4 days in each factory. While dust sampling, observation checklists and data sheets were used to record relevant data.
Interviews
The chronic respiratory symptoms among participants were assessed with face-to-face interviews using a standardized structured questionnaire adapted from the American Thoracic Society (ATS) [30]. The standardized questionnaire includes characteristics of participants’ factors, duration of exposure, previous occupational history, smoking habits, as well as respiratory symptoms such as cough, phlegm, wheezing, shortness of breath, and nose irritations, particularly those associated with the risk of respiratory morbidity.
Observational checklist
An observational checklist was used to assess the working condition (including housing conditions, ventilation, type of machine, personal protective equipment (PPE) used and general working conditions).
Data analysis
The result of the dust concentration was described using descriptive statistics such as the measure of central tendency (GM) and the measure of dispersion (GSD). The exposed filter membrane was weighed quantitatively by gravimetric analysis using a standard Mettler Toledo XPE105 micro balance scale with a detection limit of 0.01 mg at the Environmental and Occupational Health laboratory of the College of Health Sciences, Addis Ababa University. The net concentration was calculated by weighing the sampling filter before and after sampling.
The average dust concentration was compared with the threshold limit values (TLV) for total dust (also denoted as nuisance dust or Particles Not Otherwise Specified (PNOS), recommended by the Control of Substances Hazardous to Health Regulations 2002 (COSHH) for an 8-h exposure (10 mg/m3) [31]. Poisson regression models with a Robust estimator were used to estimate the prevalence ratio of different respiratory symptoms among both the workers in paper factories and controls.
Logistic regressions were used to identify factors associated with chronic respiratory symptoms. In the model chronic respiratory symptoms was used as the dependent variable and characteristics of participants, work-place, and behavioral characteristics were used as the independent variable. Only variables with P-value < 0.2 in the binary logistic analysis were transferred to multivariate analysis. The final model contained only variables with P-value ≤ 0.05. The analysis was done using the statistical software SPSS version 22.
Data quality assurance
For dust sampling, the airflow rate in the sampling pumps was measured/checked and recorded before and after each sampling event using a Rota-meter (i.e., flow rates more than ± 10% different from the target flow rate of 2.0 lit/min were dropped). Each series of sampling was controlled and corrected towards one field blank sample daily. The sample head position was mounted based on the person’s working position. At the end of sampling, the filter cassettes were covered and carefully placed in a labeled container to prevent damage. They were then transported to the lab for analysis.
A standardized questionnaire modified from ATS was used to assure data quality. Before data collection, two days of training was given to the data collectors and supervisors in order to ensure that the questionnaires were completed appropriately and to reduce bias. In addition, the questionnaire was translated from English to Amharic and back to English to check its consistency. Each day, the supervisor checked each questionnaire for completeness and consistency. In addition, pre-tests were carried out a week before the actual data collection to check the competency of the data collectors, as well as the reliability and validity of the data collection tools.
Variable measurements
Outcome variables
Chronic respiratory symptoms: cough, cough with sputum, breathlessness, wheezing, or a chest illness that lasts at least three months in one year [32].
Exposure variables
Paper dust: refers to dust coming from finely milled or otherwise processed paper and pulp products [13].
Characteristics of participants: age, sex, marital status, religion, educational status, income level and past history of respiratory illness (is a chronic respiratory diagnoses that occurred before paper dust exposure).
Family and behavioral factors: cigarette smoking, utilization of personal protective equipment (PPE), and energy source used at home for food preparation.
Work-place (environment) characteristics: ventilation, dustiness of working department, duration of employment, length of working hours/day, length of working days/week, past history of dust exposure, and type of machine.
Organizational factors: PPE provision, Occupational Health and Safety (OHS) training (formal short-term training that a worker shall have while he/she is on job) and OHS supervision (is the act of overseeing something or somebody’s activities or guide (correct) the employees if he/she is doing wrong.)
Results
Characteristics of participants
A total of 411 workers in paper factory and control groups participated in the study resulting in a response rate of 94.7%. Of the 411 respondents, 221 (53.8%) were male. The majority of the participants were younger than 25 with the mean (± SD) age being 28.8 (± 7.1) years. Almost half 200 (48.7%) of the study participants were married and 195 (47.5%) of the respondents had attended secondary school. The mean (± SD) monthly incomes of respondents were 3704 (± 2388) Ethiopian birr which is much below the national mean monthly income, 5090 Ethiopian birr. Fifty (12.2%) had a past history of a respiratory diseases that was confirmed by physician. In general, the distribution of sex, age, marital status, educational status, monthly incomes and past history of respiratory illnesses of the two comparative groups of paper and controls were significantly different (Table 1).
Work-related and behavioral characteristics
Out of the 411 respondents, 290 (70.6%) had less than five years of work experience and the majority 224 (54.5%) of the study participants worked above eight hours per day. Three hundred ninety-nine (97.1%) of the respondents had worked more than five days per week and 43 (10.5%) of workers had exposure in previous employments in dusty areas. More than half (56.2%) of the respondents was used bio-fuel (charcoal, wood and gas) as the primary energy source for cooking at home. Only 12 (2.9%) of the participants smoked cigarettes (Table 2).
Only 16 (7.8%) workers involved in this study used personal protective equipment (PPE). Whereas the remaining were not use PPE the main reasons mentioned by 175 (97.6%) of the participants were not provided by the institution and the remaining 5 (2.4%) thinks as dust is not harmful. Seventy nine (38.4%) paper factory workers and 139 (67.8%) water bottling factory workers had training on occupational health and safety (OHS) (Table 2).
Personal dust exposure of paper factories workers
The overall arithmetic mean (± SD) and geometric mean (± GSD) of the dust concentration were 11.3 (± 7.7) and 10.2 (± 1.4) mg/m3 respectively, ranging from 6.8 to 55.8 mg/m3. Out of 40 dust measurements 15 (37.5%) exceeded the acceptable recommended limit value of 10 mg/m3 of total dust of COSHH (Table 3).
Observational findings of paper factories
Observational findings of the study revealed that dust had accumulated on the walls, ceilings, floors, and machines of the different working environments. Particularly high dust levels had accumulated in places where the paper-cutting task takes place, such as the bell machine compactor and cone production. Both factories had a dust absorber in the machine (local exhaust system) that pulled excess dust and paper waste away from the process a so-called trim waste system. The employees were wearing medical (surgical) masks; however, these masks were designed to prevent the transmission of Coronavirus, and not for protecting the workers from paper dust exposure. In one paper factory, the machine was very old established more than 60 years. This might increase dust concentration in that work-place. There was no natural or mechanical ventilation. The design and age of the machinery involved, and the absence of natural or mechanical ventilation increased the dust exposure level in these work-places (Additional file 1).
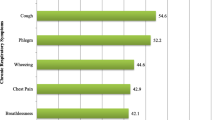
Prevalence of chronic respiratory symptoms in workers
The prevalence of chronic respiratory symptoms in workers in the paper factories and the controls varied from 17 to 33% and 4–8% respectively. The prevalence of at least one chronic respiratory symptom at a work-place was 51.9% and 9.3% respectively for paper factories and controls. The prevalence ratio of any chronic respiratory symptoms of paper factories was significantly higher than controls after adjusting for sex, age, educational status, monthly income, work experience, working hours per day, working day per week, exposure in previous employments, past history of respiratory illnesses, biofuel energy use, use of PPE, OHS training and OHS supervision (Table 4).
Factors associated with chronic respiratory symptoms among paper factory workers
Among the different characteristics of participants factors considered, educational status was found to be the greatest risk factor to chronic respiratory symptoms. In this study respondents who had not completed secondary school had 4 times (AOR = 3.8, 95% CI 1.5–10.0) higher odds of having chronic respiratory symptoms than those who had completed secondary school (Table 5).
Comparing the different work sections respondents involved in the belling (compactor) and loader section had 47 times (AOR = 46.6, 95% CI 6.2–353) high risk and those in the roll paper production, 44 times (AOR = 43.5, 95% CI 7.3–257), higher risk of having chronic respiratory symptom compared with the control group. The number of years of work in the factory was also significantly associated to the chronic respiratory symptoms. The odds of having chronic respiratory symptom after 5–9 years was 2.7 times higher (AOR = 2.7, 95% CI 1.2–6.4) and for those who had worked more than 10 years, it was 3 times (AOR = 3.1, 95% CI 1.0–9.4) higher compared to workers who had work experience of less than 5 years. The remaining other variables considered were not significantly associated with an increased risk of having chronic respiratory symptoms (Table 5).
Discussion
This study found that the arithmetic mean (AM (± SD)) and geometric mean (GM (± GSD)) of total dust concentration were 11.3 (± 7.7) and 10.2 (± 1.4) mg/m3 respectively, which was above the acceptable recommended limit value of COSHH [31]. The prevalence ratio of all chronic respiratory symptoms among paper factories workers was significantly higher than controls after adjusting for sex, age, religion, educational status, monthly income, work experience, working hours per day, working day per weak, exposure in previous employments, past history of respiratory illnesses, biofuel energy use, use of PPE, and OHS training and supervision. Within the group of paper factory workers a number of factors were significantly associated to at least one chronic respiratory symptom. These included only attaining an educational status below secondary school; working in nearly all work sections of the paper factories; having work experience from 5 to 9 years as well as greater than or equal to 10 years; working more than 8 h/day; and having a past history of occupation and respiratory illnesses.
In the present study, the personal total dust exposure of paper factory workers GM (± GSD)) 10.2 (± 1.4) was consistent with that of two previous studies conducted in Germany, which reported levels of GM (± GSD) 10.3 (± 15.5) and 12.4 mg/m3 [8, 9]. The AM of personal dust exposure level in this study was also similar to two studies conducted in Sweden of 9.9 mg/m3 and 10.8 mg/m3 as well as to a study from Turkey with 9.7 mg/m3 [7, 10, 12]. The qualitative findings of our study also support and strengthen this result. Dust levels in the work-place were seen in the accumulations of high amounts dust on the walls, ceiling, floor and machines of the different working environments. In addition, the absence of natural and mechanical ventilation and the presence of very old machines increases dust concentrations [15].
Our study found significantly higher prevalence levels for all chronic respiratory symptoms among the paper factory workers compared to controls. This was similar to a study done in Croatia, where the prevalence of chronic respiratory symptoms such as coughing (36.6% vs. 18.4%) and phlegm (34.7% vs. 16.1%) among workers in paper recycling factories and controls respectively [33]. A similar study conducted in Turkey indicated a prevalence of coughing (31.2% vs. 9%) and wheezing (43.1% vs. 10.3%) among workers in paper factories and controls respectively [10]. As stated previously, these differences might be due to both higher dust exposure levels and low levels of proper PPE use.
The prevalence of chronic respiratory symptoms in this study among paper factory participants (51.9%) was lower than those found in a previous study done in Sweden, (61.5%) [7]. The reason for the difference might be due to the age of the workers in both studies and the sample size difference in the previous study. The Swedish sample size was small and older people were involved. In addition, the difference might be due to the difference in smoking status. In our study, the number of smokers was few.
This study found that demographic characteristics such as educational status and monthly income were significantly associated to the chronic respiratory symptoms among paper factory workers. This study was consistent with a study conducted in Finland, among low socio-economic status, which found that workers with less than secondary school education (AOR = 1.8, 95% CI 1.2–2.6) and having a low income (AOR = 1.4, 95% CI 1.0–1.9) developed more chronic respiratory symptoms compared with those with higher education levels and high-income respectively [34].
Our study found that there was a statistically significant association between chronic respiratory symptoms and duration of employment. Workers with work experience greater than five years had higher chronic respiratory symptoms. This was similar to a study done in Germany, in which the duration of employment for more than 15 had 3 times more symptoms of coughing (AOR = 3.3, 95% CL; 1.4–8.8) compared to less than 15 years duration of employment [8]. This might be directly related to the duration of dust exposure. In other words, longer employment duration means more exposure to dust at the work-place.
Strength and limitation of the study
This is the first study to assess chronic respiratory symptoms and determine dust exposure levels among paper factory workers in Ethiopia. This study also used control groups to ensure the internal validity of the study.
Generally, the total dust sampling Millipore Plastic Closed-Face Filter Cassette (CFC) significantly underestimated the number of coarse particles in the inhalable paper dust level. There can be lost due to the adherence of dust to the interior part of the cassette walls, which may result in lower values thus underestimating the actual dust concentration.
As this study used interviews to assess chronic respiratory symptoms there might be respondents recall bias and this might have influenced the results. In addition, the cross-sectional study design is not appropriate to show a cause and effect relationship between risk factors and outcomes. It is also important to note that there may be other variables present, that we have not identified. We would therefore recommend a longitudinal study that assesses the effect of PPE, ventilation, work-place cleaning, and new machinery on the development of respiratory symptoms. Moreover, the outcomes could also be underestimated due to the healthy worker’s effect.
Conclusion
Findings from this study indicate that the AM (± SD) and GM (± GSD) of the concentration of dust workers in the paper factories were 11.3 (± 7.7) and 10.2 (± 1.4) mg/m3 respectively. Fifteen (37.5%) dust measurements exceeded OEL value of 10 mg/m3 given by COSHH. The prevalence of chronic respiratory symptoms among the paper factory workers was higher than among controls. The main determining factors for chronic respiratory symptoms among the workers were the specific work section such as production sections, the number of years of working, working hours per day and low educational status. We conclude that there should be an effort to reduce dust exposure level in paper factories in Ethiopia to reduce the occupational hazard of workers having chronic respiratory symptoms.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to study participant privacy/consent agreements but are available from the corresponding author on reasonable request.
Abbreviations
- AM:
-
Arithmetic mean
- AOR:
-
Adjusted odds ratio
- ATS:
-
American thoracic society
- COR:
-
Crude odds ratio
- COSHH:
-
Control of substances hazardous to health
- CI:
-
Confidence interval
- GM:
-
Geometric mean
- GSD:
-
Geometric standard deviation
- OR:
-
Odds ratio
- OEL:
-
Occupational exposure limit
- OHS:
-
Occupational health and safety
- PPE:
-
Personal protective equipment
References
United States Environmental Protection Agency. Available and emerging technologies for reducing greenhouse gas emissions from the pulp and paper manufacturing industry. U.S.A: Office of Air and Radiation; 2010.
Environmental Protection Agency. Universal industrial sectors integrated solutions model for the pulp and paper manufacturing industry USA: Universal ISIS, 2014.
Environmental protection agency. Pulping and bleaching system NESHAP for the pulp and paper industry USA: environmental protection agency; 2001 [cited 2019 12]. Available from: http://www.epa.gov/ttn/atw/pulp/guidance.pdf.
Pratima B. Green chemistry and sustainability in pulp and paper industry. Swezerland: Springer; 2015.
Peter W. Hart, Rudie AW. The bleaching of pulp. 5th Edition ed. United States of America: TAPPI Press; 2012.
International labour organization. Pulp and paper industry: In encyclopaedia of occupational health and safety 2011 Available from: https://www.iloencyclopaedia.org/part-x-96841/paper-and-pulp-industry.
Jarvholm B, Thoren K, Brolin I, Ericsson J, Morgan U, Tylen U, et al. Lung function in workers exposed to soft paper dust. Am J Ind Med. 1988;14(4):457–64.
Kraus T, Pfahlberg A, Gefeller O, Raithel HJ. Respiratory symptoms and diseases among workers in the soft tissue producing industry. Occup Environ Med. 2002;59(12):830–5.
Kraus T, Pfahlberg A, Zobelein P, Gefeller O, Raithel HJ. Lung function among workers in the soft tissue paper-producing industry. Chest. 2004;125(2):731–6.
Lutfi C, Ahmet U, Fuat K, Nilay C, Toros S, Tayfun E, et al. Lung health in workers exposed to reed dust. Respir Med. 2005;99:421–8.
Andersson E, Sallsten G, Lohman S, Neitzel R, Toren K. Lung function and paper dust exposure among workers in a soft tissue paper mill. Int Archiv Occup Environ Health. 2019;93(1):105–10.
Ericsson J, Jarvholm B, Norin F. Respiratory symptoms and lung function following exposure in workers exposed to soft paper tissue dust. Int Arch Occup Environ Health. 1988;60(5):341–5.
Toren K, Balder B, Brisman J, Lindholm N, Lowhagen O, Palmqvist M, et al. The risk of asthma in relation to occupational exposures: a case-control study from a Swedish city. Eur Respir J. 1999;13(3):496–501.
Dahlqvist M. Lung function and exposure to paper dust in bookbinders–a pilot study. Upsala J Med Sci. 1992;97(1):49–54.
Thoren K, Jarvholm B, Morgan U. Mortality from asthma and chronic obstructive pulmonary disease among workers in a soft paper mill: a case-referent study. Br J Ind Med. 1989;46(3):192–5.
Toren K, Hagberg S, Westberg H. Health effects of working in pulp and paper mills: exposure, obstructive airways diseases, hypersensitivity reactions, and cardiovascular diseases. Am J Ind Med. 1996;29(2):111–22.
Dilnessa F, Tewodros G, Elias M, Wondu RD. Effect of occupational wood dust on pulmonary function among woodworkers in Jimma Town, Southwest Ethiopia, a comparative cross sectional study. EC Pulmonol Respir Med. 2019;8(8):587–93.
Heederik D, Burdorf L, Boleij J, Willems H, van Bilsen J. Pulmonary function and intradermal tests in workers exposed to soft-paper dust. Am J Ind Med. 1987;11(6):637–45.
Thoren K, Sallsten G, Bake B, Drake U, Jarvholm B, Sahle W. Lung function and respiratory symptoms among workers in a soft paper mill. Int Arch Occup Environ Health. 1989;61(7):467–71.
World Health Organization. Global status report on non communicable diseases 2010. 2011 [1 Sept 2019]. Available from: https://www.who.int/nmh/publications/ncd_report2010/en/.
Driscoll T, Nelson DI, Steenland K, Leigh J, Concha-Barrientos M, Fingerhut M, et al. The global burden of non-malignant respiratory disease due to occupational airborne exposures. Am J Ind Med. 2005;48(6):432–45.
Holm M, Dahlman-Hoglund A, Toren K. Respiratory health effects and exposure to superabsorbent polymer and paper dust - an epidemiological study. BMC Public Health. 2011;11:557.
Holm M, Torén K, Andersson E. Incidence of chronic bronchitis: a prospective study in a large general population. Int J Turberc Lung Dis. 2014;18:870–5.
Torén K, Neitzel R, Sallsten G, Andersson E. Occupational exposure to soft paper dust and mortality. BMG Occup Environ Med. 2020;77:549–54.
Prazmo Z, Dutkiewicz J, Skorska C, Sitkowska J, Cholewa G. Exposure to airborne Gram-negative bacteria, dust and endotoxin in paper factories. Annal Agricul Environ Med AAEM. 2003;10(1):93–100.
Ethiopian business review. The paper conundrum Ethiopia: Ethiopian business review; 2017 [cited 2019 2]. 6th Year [Available from: https://ethiopianbusinessreview.net/investment/item/562-the-paper-conundrum.
Industrial ministry. Comnication with diroctarate about packaging, pulp and paper 2019.
Wakuma S, Bråtveit M, Deressa W, Kumie A, Bente E. Personal dust exposure and its determinants among workers in primary coffee processing in Ethiopia. Annal Work Exposures Health. 2018;62(9):1–9.
Rappaport SM, Kupper LL. Quantitative exposure assessment El Cerrito, CA: Stephen Rappaport 2008.
Ferris BG. Epidemiology standardization project. II. Recommended respiratory disease questionnaires for use with adults and children in epidemiological research. Am Rev Respir Disease 1978;21(40): 118:7–57.
Health topic. Health topics - dust on the control of substances hazardous to health regulations 2002 (COSHH): BETA; 2002. Available from: http://www.hse.gov.uk/paper/dust.htm.
Ghosh T, Gangopadhyay S, Das B. Prevalence of respiratory symptoms and disorders among rice mill workers in India. Environ Health Prev Med. 2014;19:226–33.
Zuskin E, Mustajbegovic J, Makan B, Makan J, Vurkes V, Vitale K. Respiratory function and allergic reaction in paper recycling workers. Arh Hig Rada Toksikol. 1998;49(2):165–77.
Kanervisto M, Vasankari T, Laitinen T, Heliövaara M, Jousilahti P, Saarelainen S. Low socioeconomic status is associated with chronic obstructive airway diseases. Respir Med. 2011;105(8):1140–6.
Acknowledgements
I am extremely thankful for the opportunity and financial help from Addis Ababa University and the Norwegian Agency for Development Cooperation (NORAD). In addition, I would like to thank the supervisors, data collectors and research participants for their cooperation and help. Finally, I would like to thank the factory owners and management teams for their permission to undertake the study, as well as the employees for participating.
Funding
BMN has received financial support from Addis Ababa University and the Norwegian Agency for Development Cooperation (NORAD) for data collection. The funder had no role in the study design, data collection, and analysis, decision to publish, or preparation of the manuscript. There was no additional external funding received for this study.
Author information
Authors and Affiliations
Contributions
BMN planned the study idea and refined it with SWA. BMN, SWA, and TA worked on the designing of the study and approved the proposal. BMN, HBN, TTG, TT, and GKK worked on the data collection, entry, cleaning, and analysis. SWA, TA, AKT, and WTM reviewed and approved the data analysis. All of the authors drafted, reviewed, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance and approval were obtained from the ethical review committee of Addis Ababa University, College of Health Sciences, School of Public Health. Permission to conduct the study was obtained from the factory managers and owners. The purpose and method of the study and importance of their participation were clearly explained to the participants. Informed consent was obtained from all the participants. Our study protocol ensured that issues of rights, privacy and confidentiality were protected during the data collection period. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable for this section.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary material regarding on observational checklist, chronic respiratory symptoms and past history of respiratory illnesses.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Negash, B.M., Abaya, S.W., Abegaz, T. et al. Assessment of paper dust exposure and chronic respiratory symptoms among paper factory workers in, Ethiopia; a comparative cross-sectional study. BMC Pulm Med 23, 48 (2023). https://doi.org/10.1186/s12890-023-02338-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-023-02338-2